Abstract
Recent anatomical and biomechanical studies on the anterolateral ligament (ALL) of the knee have shown that this structure has an important function in relation to joint stability, especially when associated with anterior cruciate ligament (ACL) injury. However, the criteria for its reconstruction have not yet been fully established and the surgical techniques that have been described present variations regarding anatomical points and fixation materials. This study presents a reproducible technique for ALL and ACL reconstruction using hamstring tendons, in which three interference screws are used for fixation.
Keywords: Anterior cruciate ligament reconstruction, Anterolateral ligament, Orthopedic procedures
Resumo
Os recentes estudos anatômicos e biomecânicos sobre o ligamento anterolateral (LAL) do joelho evidenciam que essa estrutura apresenta função relevante para a estabilidade articular principalmente quando associada à lesão do ligamento cruzado anterior (LCA). No entanto, os critérios para sua reconstrução ainda não estão totalmente estabelecidos, assim como as técnicas cirúrgicas descritas apresentam variações sobre os pontos anatômicos e materiais de fixação. O estudo apresenta uma técnica reprodutível para a reconstrução do LAL e LCA com os tendões flexores que usa três parafusos de interferência para as fixações.
Palavras-chave: Reconstrução do ligamento cruzado anterior, Ligamento anterolateral, Procedimentos ortopédicos
Introduction
The treatment of anterior knee instability through reconstruction of the anterior cruciate ligament (ACL) presents good clinical results. However, the failure rate for this operation is estimated to range from 1.8% to 14%.1, 2 The persistence of anterolateral instability assessed by the pivot-shift test postoperatively is described as one of those factors.2, 3
After the anatomical “rediscovery” and biomechanical studies of the anterolateral ligament (ALL) demostrated that this structure is important in anterolateral knee stability, it was observed that insufficiency of this ligament may contribute to the functional failure of isolated ACL reconstructions.4
This study aimed to present a reproducible technique of anatomical ACL and ALL reconstruction with the hamstring tendons, using three interference screws.
Surgical technique
Fifteen adult patients (19–38 years), 12 men and three women, underwent ACL and ALL reconstruction by the technique described below, with a mean follow-up of 10 months (6–15 months). All patients returned, without complaints, to activities of daily living and/or to sports and recreational activities that they practiced prior to injury.
Indication
After spinal anesthesia, a clinical examination was performed to estimate ALL sufficiency.
The anterior asymmetry of the lateral plateau with internal rotation of the tibia in flexion of 30–60°5 relative to the contralateral knee, and increased positivity of the pivot-shift maneuver can be a clinical sign of failure of the ALL.4
The study used the classification for the pivot-shift maneuver determined by the International Knee Documentation Committee6 (IKDC) 2000, which describes four grades: 0 – normal, 1 – glide, 2 – clunk, 3 – gross shift.
The criteria used for ALL reconstruction associated with ACL injuries were:
-
1.
Injury in the ALL substance identified at a magnetic resonance imaging (MRI), termed Segond-like injury;
-
2.
Segond fracture7;
-
3.
Pivot-shift classified as grade II/III;
-
4.
ACL reconstruction review in which patients had residual pivot-shift during the postoperative period and evolved with graft injury;
-
5.
Asymmetrical anterior lateral plateau visible with knee internal rotation in flexion between 30° and 60°.
-
6.
Lateral femoral notch sign.8
Graft preparation and surgical technique
The excision of the semitendinosus tendon (ST) and gracilis tendon (GR) is made through a 4-cm anteromedial incision in the tibia over the pes anserinus.
During the arthroscopic procedure for the anteromedial and anterolateral portals, the joint is assessed and the intercondyle is cleaned, while tendons are handled at the instrumentation table. All grafts are prepared with EthibondR n° 2 (Ethicon, Somerville, NJ).
The GR used to rebuild the ALL is prepared to form a double graft. Each end is sutured with Krackow stitches.
One end of the GR is passed as a “handle” during the preparation of the triple ST graft, which will be used for ACL reconstruction, so that the double GR graft has the same size in its two parts and the triple ST graft has a Krackow suture in one end and the other end is anchored in the GR (Fig. 1A–C).
Fig. 1.
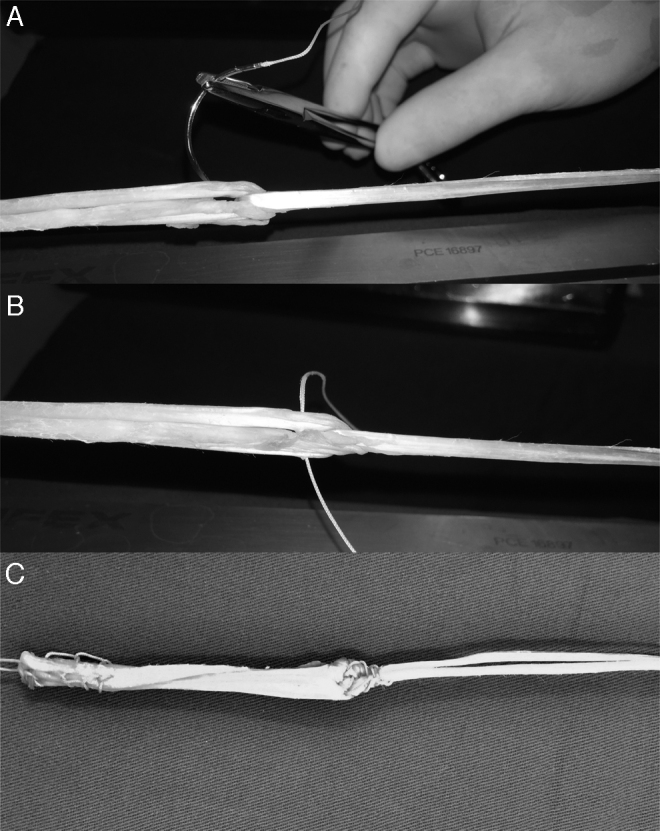
(A) Tensioned triple semitendinosus graft and double gracilis graft; intertwined, ready for suturing. (B) Triple semitendinosus graft (LCA) and double gracilis graft (LAL), started suturing. (C) Finished grafts.
After preparation and measurement of graft diameters (usually 8 mm for the triple ST graft and 5 mm for the double GR), the femoral and tibial tunnels are prepared.
The femoral tunnel, common to the ACL and ALL, is made using the outside-in technique. A tibial ACL guide is placed so that its joint position overlaps the footprint of the anatomical insertion of the ACL in the intercondylar wall. A 65° opening is applied to minimize the “killer turn” of the graft.
After the ACL guide is positioned and the site where the guide wire will be introduced is assessed, the guidewire is removed, and a 4-cm longitudinal incision in the skin and iliotibial tract is performed on the lateral side of the knee.
The lateral epicondyle is identified by palpation; the guidewire is introduced 8 mm (about one digital tip) posterosuperiorly9, 10 in the lateral femoral cortex to mark the entry site.
The ACL guide is then reattached and coupled to the guidewire, followed by the drilling of the path for the ACL footprint. Sequentially, one drill of the same diameter as the graft is used to make the tunnel, which is generally 35-mm long.
The tibial tunnel is prepared with the same guide and similarly, but with an angle of 55° on the tibial ACL footprint.
After creating the tunnels for the ACL, a suture is passed with the guidewire through four outside-in holes through the femoral tunnel and withdrawn with a grasper tool through the tibial tunnel, so as to pass over the joint and allow for the passage of the graft.
Sutures at the loosen edge of the ST graft (ACL) are looped in the transacetabular wire and the graft is passed outside-in from the femur to the tibia, remaining in its final position (Fig. 2A and B). An interference screw of the same diameter as the drilled tunnel, with 30–35 mm length, is used for femoral fixation.
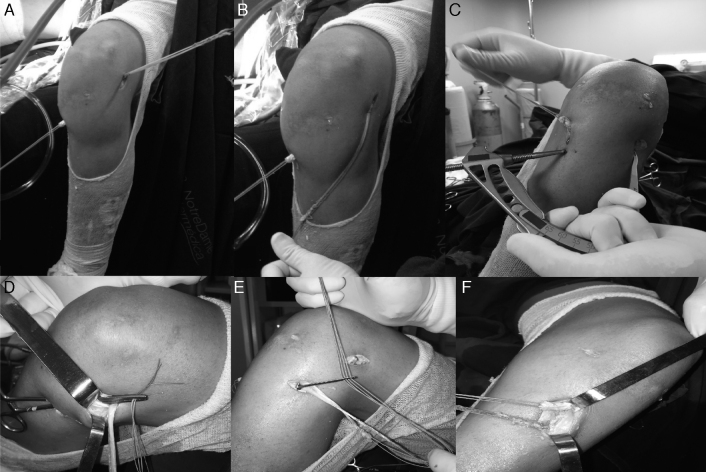
Fig. 2.
(A) ACL graft positioned in the femoral and tibial tunnels and ALL graft fixed in the femoral point; (B) double GR graft length to rebuild the ALL on the path it must follow; (C) positioning of the ACL guide at 65° and exit point halfway between Gerdy's tubercle and the fibular head, 13 mm from the surface of the lateral tibial plateau; (D) clamp passed deep into the iliotibial tract to drive the ALL graft into the tibial tunnel; (E) passage of the ALL graft through the tibial tunnel; (F) ACL and ALL grafts ready to be fixed with interference screw through the same incision.
For the reconstruction and attachment of the ALL in the tibia, the ACL guide is positioned at 65°, so that the guidewire can be inserted 2 cm distal to the tibial tunnel through the same incision made for ACL graft removal. It exits halfway between Gerdy's tubercle and the head of the fibula, 9–13 mm distal to the surface of the lateral tibial plateau, the anatomical ALL point.9
A 3-cm anterolateral skin and iliotibial tract incision is made (Fig. 2C) and the tunnel is drilled with a 6-mm bit.
A long forceps is introduced through the ALL tibial incision deep into the iliotibial tract until its output in the femoral ACL tunnel incision, where the GR graft is pulled and passed through the tibial ALL tunnel (Fig. 2D–F).
The knee is then placed at 30° flexion for ACL fixation and at 45–60° for ALL fixation5 with interference screws that are 2 mm larger than the drilled tunnels, both through the same anteromedial incision. The suture grafts can be tied to reinforce the fixation.
Postoperative rehabilitation follows the protocol for ACL reconstruction with hamstrings.
Discussion
The “rediscovery” of the ALL and its role in anterolateral knee stability is currently presented as one of the trends in knee ligament reconstructions.11
The facts that the ALL is not a structure routinely described in MRI reports and that the reconstruction criteria are not fully established contribute to the missdiagnosis and undertreatment of this injury.
Helito et al.12 showed that the ALL is fully visualized in 71.7% of the MRIs. In turn, Taneja et al.13 have identified the full ALL view in 11%.
Spencer et al.4 showed that the anterolateral knee instability is accentuated when the ACL and the ALL are torn, emphasizing the pivot-shift maneuver.
Sonnery-Cottet et al.11 recommend ALL reconstruction in Segond fractures, chronic ACL injuries, grade III pivot-shift, high-level athletes or those who practice sports that require rotation of the knee, and in the presence of lateral femoral notch sign.8 However, the present authors do not consider chronicity and the patient's activities as criteria for empirical ALL reconstruction if the physical examination shows no evidence of its failure.
Regarding the described techniques for ACL and ALL reconstruction, Helito et al.14 used a quadruple graft (triple ST and one GR) for ACL and one GR for ALL; tibial fixation was conducted with anchors. Sonnery-Cottet et al.11 used triple ST graft for ACL and double GR graft for ALL, with two tibial holes to rebuild the ALL.
In the present technique, the method used for graft preparation creates a suspension effect similar to the Endobutton, added to the suture to reinforce this union, which also includes an interference screw. This allows the end of the ST graft to remain close to the articular femoral point, and there is no need to occupy the entire tunnel, which will be completed by the GR graft, thus facilitating the procedure in case of short grafts.
Studies have shown differences in the ALL femoral anatomical point. Caterine et al.10 and Kennedy et al.9 demonstrated that its origin is on average 3 mm posterior and proximal to the lateral epicondyle; this point was used in the present technique. In turn, Helito et al.15 and Claes et al.16 demonstrated that the origin of the ALL is anterior to the lateral epicondyle.
The option adopted in the present technique was to make the tunnel posterosuperior to the lateral epicondyle, in order to reduce the intraarticular “killer turn” of the graft; this point approaches the isometrics described by Kurosawa et al.17 for lateral tenodesis of the iliotibial tract.
For the tibial point, Sonnery-Cottet et al.11 used two tunnels, which does not appear necessary, since the ALL anatomical insertion has about 9 mm in the tibia.9
Conclusion
ACL and ALL reconstruction using the technique described for the anterolateral instability of the knee was satisfactory in these patients; it uses materials, guides, and incisions that are familiar to any surgeon, which facilitates its reproduction.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Study conducted at the Hospital Renascença, Departamento de Cirurgia de Joelho, Osasco, SP, Brazil.
References
- 1.Mariscalco M.W., Flanigan D.C., Mitchell J., Pedroza A.D., Jones M.H., Andrish J.T. The influence of hamstring autograft size on patient-reported outcomes and risk of revision after anterior cruciate ligament reconstruction: a Multicenter Orthopaedic Outcomes Network (MOON) Cohort Study. Arthroscopy. 2013;29(12):1948–1953. doi: 10.1016/j.arthro.2013.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prodromos C.C., Joyce B.T., Shi K., Keller B.L. A meta-analysis of stability after anterior cruciate ligament reconstruction as a function of hamstring versus patellar tendon graft and fixation type. Arthroscopy. 2005;21(10):1202. doi: 10.1016/j.arthro.2005.08.036. [DOI] [PubMed] [Google Scholar]
- 3.Mohtadi N.G., Chan D.S., Dainty K.N., Whelan D.B. Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev. 2011;(9):CD005960. doi: 10.1002/14651858.CD005960.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Spencer L., Burkhart T.A., Tran M.N., Rezansoff A.J., Deo S., Caterine S. Biomechanical analysis of simulated clinical testing and reconstruction of the anterolateral ligament of the knee. Am J Sports Med. 2015;43(9):2189–2197. doi: 10.1177/0363546515589166. [DOI] [PubMed] [Google Scholar]
- 5.Parsons E.M., Gee A.O., Spiekerman C., Cavanagh P.R. The biomechanical function of the anterolateral ligament of the knee. Am J Sports Med. 2015;43(3):669–674. doi: 10.1177/0363546514562751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Irrgang J.J., Ho H., Harner C.D., Fu F.H. Use of the International Knee Documentation Committee guidelines to assess outcome following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 1998;6(2):107–114. doi: 10.1007/s001670050082. [DOI] [PubMed] [Google Scholar]
- 7.Claes S., Luyckx T., Vereecke E., Bellemans J. The Segond fracture: a bony injury of the anterolateral ligament of the knee. Arthroscopy. 2014;30(11):1475–1482. doi: 10.1016/j.arthro.2014.05.039. [DOI] [PubMed] [Google Scholar]
- 8.Herbst E., Hoser C., Tecklenburg K., Filipovic M., Dallapozza C., Herbort M. The lateral femoral notch sign following ACL injury: frequency, morphology, and relation to meniscal injury and sports activity. Knee Surg Sports Traumatol Arthrosc. 2015;23(8):2250–2258. doi: 10.1007/s00167-014-3022-5. [DOI] [PubMed] [Google Scholar]
- 9.Kennedy M.I., Claes S., Fuso F.A., Williams B.T., Goldsmith M.T., Turnbull T.L. The anterolateral ligament: an anatomic, radiographic, and biomechanical analysis. Am J Sports Med. 2015;43(7):1606–1615. doi: 10.1177/0363546515578253. [DOI] [PubMed] [Google Scholar]
- 10.Caterine S., Litchfield R., Johnson M., Chronik B., Getgood A. A cadaveric study of the anterolateral ligament: re-introducing the lateral capsular ligament. Knee Surg Sports Traumatol Arthrosc. 2015;23(11):3186–3195. doi: 10.1007/s00167-014-3117-z. [DOI] [PubMed] [Google Scholar]
- 11.Sonnery-Cottet B., Thaunat M., Freychet B., Pupim B.H., Murphy C.G., Claes S. Outcome of a combined anterior cruciate ligament and anterolateral ligament reconstruction technique with a minimum 2-year follow-up. Am J Sports Med. 2015;43(7):1598–1605. doi: 10.1177/0363546515571571. [DOI] [PubMed] [Google Scholar]
- 12.Helito C.P., Helito P.V., Costa H.P., Bordalo-Rodrigues M., Pecora J.R., Camanho G.L. MRI evaluation of the anterolateral ligament of the knee: assessment in routine 1.5-T scans. Skeletal Radiol. 2014;43(10):1421–1427. doi: 10.1007/s00256-014-1966-7. [DOI] [PubMed] [Google Scholar]
- 13.Taneja A.K., Miranda F.C., Braga C.A., Gill C.M., Hartmann L.G., Santos D.C. MRI features of the anterolateral ligament of the knee. Skeletal Radiol. 2015;44(3):411. doi: 10.1007/s00256-014-2052-x. [DOI] [PubMed] [Google Scholar]
- 14.Helito C.P., Bonadio M.B., Gobbi R.G., da Mota E., Albuquerque R.F., Pécora J.R. Combined intra- and extra-articular reconstruction of the anterior cruciate ligament: the reconstruction of the knee anterolateral ligament. Arthrosc Tech. 2015;4(3):e239–e244. doi: 10.1016/j.eats.2015.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Helito C.P., Demange M.K., Bonadio M.B., Tirico L.E., Gobbi R.G., Pecora J.R. Radiographic landmarks for locating the femoral origin and tibial insertion of the knee anterolateral ligament. Am J Sports Med. 2014;42(10):2356–2362. doi: 10.1177/0363546514543770. [DOI] [PubMed] [Google Scholar]
- 16.Claes S., Vereecke E., Maes M., Victor J., Verdonk P., Bellemans J. Anatomy of the anterolateral ligament of the knee. J Anat. 2013;223(4):321–328. doi: 10.1111/joa.12087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kurosawa H., Yasuda K., Yamakoshi K., Kamiya A., Kaneda K. An experimental evaluation of isometric placement for extraarticular reconstructions of the anterior cruciate ligament. Am J Sports Med. 1991;19(4):384–388. doi: 10.1177/036354659101900411. [DOI] [PubMed] [Google Scholar]