Abstract
Objectives
Cervical imaging practices are poorly understood in young children with Traumatic Brain Injury (TBI). We therefore sought to: identify child-level and hospital-level factors associated with performance of cervical imaging of children with TBI from falls and abusive head trauma (AHT); and describe across-hospital variation in cervical imaging performance. We hypothesized that imaging decisions would be influenced by hospital volume of young injured children.
Methods
We performed a retrospective study of children younger than 2 years of age with TBI from 2009-2013 in the Premier Perspective Database. After adjustment for observed patient characteristics, we evaluated variation in advanced cervical imaging (computed tomography or magnetic resonance imaging) in children with AHT and TBI from falls.
Results
Of 2,347 children with TBI, 18.7% were from abuse, and 57.1% were from falls. Fifteen percent of children with TBI underwent advanced cervical imaging. Moderate or severe head injuries were associated with increased odds of cervical imaging in AHT (OR 7.10; 95% CI 2.75, 18.35) and falls (OR 2.25; 95% CI 1.19, 4.27). There was no association between annual hospital volume of injured children and cervical imaging performance. The adjusted probability of imaging across hospitals ranged from 4.3 to 84.3% in AHT and 3.1 to 39.0% in TBI from falls (P < 0.001).
Conclusions
These results highlight variation across hospitals in adjusted probability of cervical imaging in AHT (nearly twenty-fold) and TBI from falls (over ten-fold) not explained by observed patient characteristics. This variation suggests opportunities for further research to inform imaging practices.
Keywords: Traumatic Brain Injury, Child Abuse, Spinal Injuries, Accidental Falls
Introduction
Traumatic brain injury (TBI), a leading cause of death in children,1 can co-occur with injuries to the cervical spine.2-4 Recent evidence suggests that cervical spine injuries occur more commonly than previously recognized in certain subpopulations of children with TBI, specifically in young children with abusive head trauma (AHT).5-7 Imaging decisions therefore need to be tailored to the individual child's age and mechanism of trauma. Further understanding of current practices and indications for cervical imaging specifically in young victims of TBI less than 2 years of age is needed due to the distinct mechanisms of TBI in young children,8 anatomic differences of the young developing spine,3,9 and the diagnostic challenges posed by this young and often preverbal population.10
Health services research can help to better describe current imaging practices for young children with TBI and to motivate and potentially guide improvement efforts by examining excessive variation in imaging practices across hospitals (meaning variation above and beyond that due to differences due to patient characteristics) and by testing whether certain types of hospitals, or hospitals that care for different volumes of patients, systematically image these children differently. Regarding variation in practice, we know that performance of cervical computed tomography (CT) among children with TBI younger than 18 years ranges from 0.9 to 59.4% across select children's hospitals.11 We do not know what this range is for young children with TBI, especially after adjustment for patient characteristics. Regarding differences across types of hospitals, in prior work describing cervical imaging of children younger than 3 years presenting with blunt trauma, Level 1 adult trauma centers and pediatric trauma centers in adult hospitals were more likely to obtain cervical CT than Level 1 pediatric trauma centers in children's hospitals.10 Given that non-children's hospitals care for 89% of pediatric trauma victims with intracranial injuries,12 examining care provided in these institutions is important. Regarding hospital volume, these differences suggest that hospitals that care for larger volumes of injured children may image less. Indeed, a study of 14 hospitals found increased pediatric volume was associated with decreased performance of cervical CTs in injured children.13
Accordingly, the purpose of this study was to describe and analyze the use of advanced cervical imaging by TBI mechanism in children younger than 2 years of age. Our objectives were to: identify child-level and hospital-level factors associated with decision to obtain advanced cervical imaging in young children evaluated for the most common mechanisms of TBI (falls and AHT); describe variation in imaging practices across hospitals after accounting for differences in patient characteristics; and evaluate the association of hospital volume of young injured patients with the odds of obtaining advanced cervical imaging. We hypothesized that hospitals treating a higher volume of young injured children may have more experience examining young children and therefore perform less cervical imaging in children with TBI from falls. Because hospitals that care for more injured children may be more familiar with possible abuse-related injuries, we hypothesized that they would obtain more cervical imaging in cases of AHT.
Methods
Data Source
We utilized the Premier Perspective Database (PPD; Premier Inc., Charlotte, NC) for this study. The PPD is an all-payer administrative database that captures approximately 20% of U.S. hospitalizations and 5.5 million annual discharges from more than 500 hospitals.14-16 The PPD provides detailed information on imaging performed during each encounter, in addition to patient demographics, diagnosis and procedure codes, and hospital characteristics. Imaging results are not available in the PPD. This study of de-identified data did not meet the definition of human subject research and did not require Institutional Review Board approval.
Cohort
We selected children less than 2 years of age discharged between 2009 and 2013 from an emergency department (ED) visit, observational stay, or inpatient unit with an International Classification of Diseases, 9th revision, Clinical Modification (ICD-9-CM) diagnosis of TBI. For our analyses, we stratified the cohort by mechanism of injury: falls, motor vehicle crashes (MVCs), and AHT. For our definition of AHT, we adapted the Centers for Disease Control (CDC) AHT algorithm17 by removing ICD-9-CM codes that did not explicitly reference head injury in order to focus our sample on children with AHT and definitive intracranial injuries. To capture the initial presentation of an injury, we included the first TBI encounter for each patient in the study time period. Children transferred to other institutions within 3 days and all children transferred from outside facilities were excluded because imaging could have been performed before or after transport and lead to underestimates of imaging. Hospitalizations related to birth and children and children discharged to rehabilitation facilities or hospice within 3 days were excluded. To facilitate valid hospital volume comparisons, we included only hospitals that reported both ED and inpatient data.
Outcome
Our primary outcome of interest was a binary indictor for advanced cervical imaging. To ensure inclusion of all possible advanced cervical imaging, this outcome was defined as performance of a CT or MRI of the cervical spine, full spine, or spine without specified location. Some hospitals relied exclusively on CT for cervical imaging of children with TBI and others used a combination of CT or MRI. We therefore elected to use this combined outcome because selection of modality was likely influenced by availability and hospital norms in addition to concerns for specific injuries.
The focus of this work was not the use of cervical radiographs because their role as the sole imaging modality to rule out injury in young trauma victims with a decreased Glasgow Coma Scale or with unreliable clinical exams is unclear.18 We do, however, describe the percentage of children who underwent cervical plain radiographs defined as a radiograph of the cervical spine, whole spine, or unspecified spinal region. Skeletal surveys were not included in this definition.
Covariates
Patient-level covariates included age, race (White, African-American, Hispanic, or Other), sex, insurance status (public, private, or other), and discharge year. Each patient's injury severity was measured with the Maximum Abbreviated Injury Scale (MAIS) severity score of the head.19 The MAIS is an ordinal scale of injury severity ranging from minor injury (1) to maximal/untreatable injury (6) for discrete body regions. Each ICD-9-CM code associated with the encounter was mapped to the 1998 version of the Abbreviated Injury Scale (AIS) codes using the ICDMAP-90 software.20 To ensure use of current severity scores, these codes were then manually re-mapped to the most recent AIS 2005/2008 versions and the ICD-9-CM injury descriptions.19-21 A MAIS score of 0 indicated an injury too nonspecific to categorize. MAIS scores of the head outside the ICD-9-CM range of the MAIS, such as 995.55 (Shaken Baby Syndrome), could not be calculated. The final MAIS score of the head was dichotomized for our analyses as minor TBI (scores < 3 including zero and incalculable scores) and moderate/severe TBI (scores ≥ 3).
Hospital-level covariates included hospital location (urban or rural), teaching status (teaching or nonteaching), geographic region (South, Midwest, Northeast, or West), and hospital all-type injury volume. Hospital all-type injury volume was calculated from the annual volume of children < 2 years who were discharged from each hospital's emergency department or inpatient unit with an ICD-9-CM code for any injury (ICD-9-CM codes 800-959). This continuous hospital-specific variable was log-transformed (base 2) in all analyses.22 We defined hospitals whose patient population included at least 75% children less than 18 years as pediatric centers.
Statistical Analysis
We described unadjusted patient and hospital factors associated with each mechanism of TBI using frequencies and proportions in our entire cohort (“Overall TBI Cohort”). We then used multivariable logistic regression models to estimate the association of these patient-level and hospital-level factors with the odds of advanced cervical imaging in cases of AHT and TBI from falls (“AHT and Falls Cohorts”). The primary exposure of interest was hospital all-type injury volume. Separate models were fit for children with AHT and falls. A robust variance estimator was used to adjust confidence intervals (CIs) for the correlation due to clustering of patients within hospitals. All analyses were conducted in Stata 13.1 (College Station, TX).
We used mixed-effects logistic regression models with hospital-specific random intercepts to calculate the hospital-level adjusted percent probability of advanced cervical imaging, adjusting for differences in patient characteristics (age, sex, race, insurance type, head injury severity, discharge year) across hospitals. We then graphically explored the association between all-type injury volume and this adjusted percent probability of imaging by hospital. In order to explore hospital-level variation, we adjusted for solely the above-mentioned patient-level covariates. The unadjusted proportion of patients imaged at each hospital was adjusted by a ratio of the observed to expected probability of imaging to produce each hospital's final adjusted percent probability of imaging.23 For these analyses, we limited our population to hospitals that cared for at least 5 children with TBI from the specific mechanism of injury of each model (“Larger Hospital Volume AHT and Falls Cohorts”).
Sensitivity Analyses
To evaluate whether our findings were impacted by the combined outcome of CT or MRI, we also performed a sensitivity analysis with cervical CT as the outcome. MRI was too rare to model separately. To evaluate whether our variation results were impacted by the exclusion of transfers, we performed a sensitivity analysis including transfers to and from the hospital. To evaluate whether the small numbers of AHT and TBI from falls at some hospitals were driving our variation analyses, we graphically reported adjusted percent probabilities of advanced cervical imaging by the total hospital volume of AHT and TBI from falls over the study period.
Results
Study Population
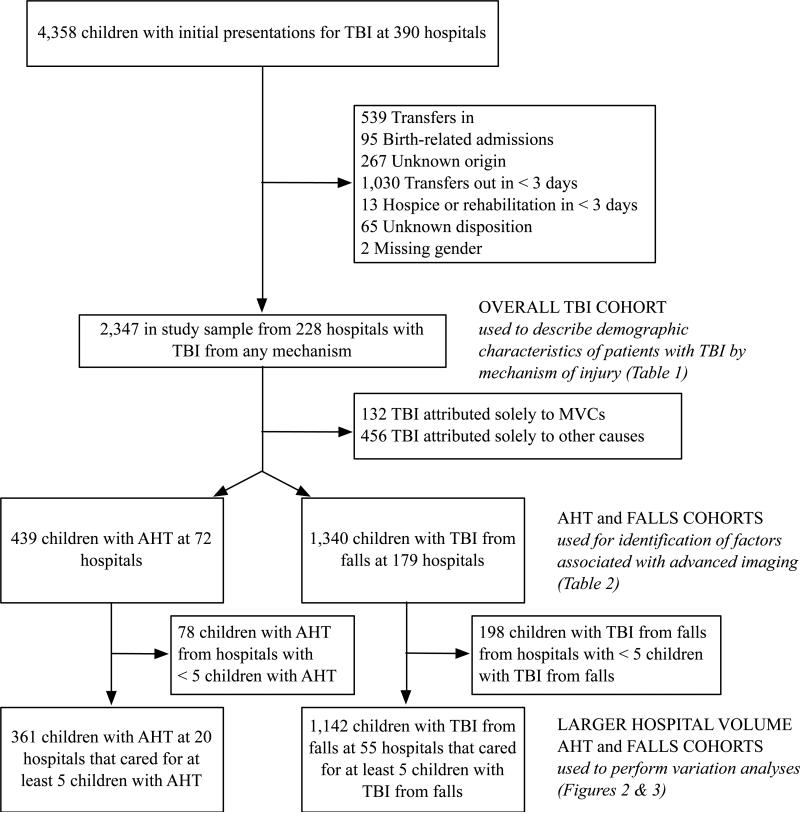
Of 4,191,406 individual children less than 2 years presenting to 456 hospitals during the 5-year study period, we identified 4,358 children (0.10%) from 390 hospitals whose first encounters for TBI were evaluated in the emergency department, inpatient setting, or during an observational stay. Of the 2,347 children who comprised our Overall TBI Cohort (Figure 1), 1,340 (57.1%) were due to falls, 439 (18.7%) were due to AHT, and 140 (6.0%) were from MVCs (Table 1). The remaining 456 (19.4%) of “other” TBI cases were predominantly attributed to accidental or unspecified mechanisms of injury. Children with AHT and TBI from falls were predominantly male, white, and publically insured. A majority of children with AHT and children with TBI from falls had a head injury severity ≥ 3. Our TBI cohort was derived from 228 hospitals, only 3 of which met our definition of a pediatric center. These 3 pediatric centers represented 16.3% of our total TBI cohort, 13.3% of children with falls, and 22.6% of children with AHT.
FIGURE 1.
Flow diagram of children in study and construction of cohorts.
TABLE 1.
Cohort Characteristics of Children with < 2 years with TBI
| All TBI 2347 (100) N (%) |
Falls* 1340 (57.1) N (%) |
AHT* 439 (18.7) N (%) |
MVCs* 140 (6.0) N (%) |
Other 456 (19.4) N (%) |
|
|---|---|---|---|---|---|
| Age (years) | |||||
| 0 | 1666 (71.0) | 943 (70.4) | 364 (82.9) | 68 (48.6) | 312 (68.4) |
| 1 | 681 (29.0) | 397 (29.6) | 75 (17.1) | 72 (51.4) | 144 (31.6) |
| Sex | |||||
| Male | 1363 (58.1) | 767 (57.2) | 260 (59.2) | 72 (51.4) | 280 (61.4) |
| Female | 984 (41.9) | 573 (42.8) | 179 (40.8) | 68 (48.6) | 176 (38.6) |
| Race | |||||
| White | 1262 (53.8) | 759 (56.6) | 220 (50.1) | 52 (37.1) | 244 (53.5) |
| African-American | 413 (17.6) | 210 (15.7) | 84 (19.1) | 41 (29.3) | 84 (18.4) |
| Hispanic | 151 (6.4) | 89 (6.6) | 31 (7.1) | 12 (8.6) | 22 (4.8) |
| Other | 521 (22.2) | 282 (21.0) | 104 (23.7) | 35 (25.0) | 106 (23.3) |
| Insurance | |||||
| Public | 1419 (60.5) | 748 (55.8) | 336 (76.5) | 67 (47.9) | 286 (62.7) |
| Private | 715 (30.5) | 481 (35.9) | 76 (17.3) | 32 (22.9) | 133 (29.2) |
| Other | 213 (9.1) | 111 (8.3) | 27 (6.2) | 41 (29.3) | 37 (8.1) |
| MAIS Score of the Head | |||||
| 0 | 161 (6.9) | 117 (8.7) | 6 (1.4) | 4 (2.9) | 36 (7.9) |
| 1 | 303 (12.9) | 235 (17.5) | 1 (0.2) | 4 (2.9) | 64 (14.0) |
| 2 | 160 (6.8) | 105 (7.8) | 11 (2.5) | 18 (12.9) | 27 (5.9) |
| 3 | 1633 (69.6) | 868 (64.8) | 363 (82.7) | 106 (75.7) | 318 (69.7) |
| 4 | 20 (0.9) | 4 (0.3) | 3 (0.7) | 6 (4.3) | 7 (1.5) |
| 5 | 15 (0.6) | 11 (0.8) | 1 (0.2) | 1 (0.7) | 3 (0.7) |
| 6 | 1 (0.04) | — | — | — | 1 (0.2) |
| Incalculable | 54 (2.3) | — | 54 (12.3) | 1 (0.7) | — |
| Cervical Imaging | |||||
| XR | 183 (7.8) | 88 (6.6) | 40 (9.1) | 35 (25.0) | 23 (5.0) |
| CT | 312 (13.3) | 108 (8.1) | 78 (17.8) | 83 (59.3) | 52 (11.4) |
| MRI | 85 (3.6) | 12 (0.9) | 44 (10.0) | 25 (17.9) | 6 (1.3) |
| CT or MRI | 353 (15.0) | 116 (8.7) | 108 (24.6) | 85 (60.7) | 54 (11.8) |
| Teaching Hospital§ | 1223 (52.1) | 655 (48.9) | 239 (54.4) | 88 (62.9) | 262 (57.5) |
| Urban Hospital§ | 2181 (92.3) | 1234 (92.1) | 420 (95.7) | 132 (94.3) | 421 (92.3) |
| Pediatric Center§ | 383 (16.3) | 178 (13.3) | 99 (22.6) | 31 (22.1) | 82 (18.0) |
Falls, AHT (Abusive Head Trauma), and MVCs (Motor Vehicle Crashes) were not mutually exclusive mechanisms of TBI (Traumatic Brain Injury); 2 children with AHT and 6 children with falls were also coded as having MVCs; 20 children were coded as having both AHT and falls. Column percentages my not add up to 100% due to rounding.
A total of 64 Teaching Hospitals, 180 Urban Hospitals, and 3 Pediatric Centers are represented in this sample.
Advanced cervical imaging
Of the 2,347 children with TBI in the Overall TBI Cohort, 353 (15.0%) underwent a cervical CT or MRI (Table 1). A total of 116 (8.7%) of the 1,340 children with falls and 108 (24.6%) of the 439 children with AHT underwent advanced cervical imaging. Eighty-five (60.7%) of the 140 children with TBI from MVCs and 54 (11.8%) of 456 of children with “other” mechanisms of TBI underwent advanced cervical imaging. CT was the most common type of advanced cervical imaging across groups. Only 3.6% of the overall cohort underwent MRI compared to the 13.3% who underwent CT. One child with TBI from an MVC underwent an unspecified spinal MRI. No children underwent whole spine CT or MRI or an unspecified spinal CT. Only 7.8% of the cohort received cervical plain radiography.
Patient and Hospital-Level Factors Associated with Imaging
Both age and head injury severity were statistically associated with imaging in both the AHT and Falls Cohorts (Table 2). Specifically, children with AHT had higher odds of imaging if they were 1 year of age (vs. < 1 year), of Hispanic ethnicity (vs. Caucasian), had moderate/severe head injury severity (vs. minor), or were discharged in 2013 (vs. 2009). For children with falls, age 1 year (vs. < 1 year) and moderate/severe head injury severity (vs. minor) were similarly associated with increased odds of imaging. Notably, increasing hospital all-type injury volume was not associated with increased odds of imaging in either children with AHT or TBI from falls.
TABLE 2.
Factors Associated with Advanced Cervical Imaging of Children with TBI from AHT and Falls.
| AHT* |
TBI from Falls |
|||
|---|---|---|---|---|
| OR (95% CI) | P-value | OR (95% CI) | P-value | |
| Patient-Level Factors | ||||
| Age 1 year (vs. Age < 1) | 4.43 (2.53, 7.76) | <0.001 | 2.15 (1.41, 3.27) | <0.001 |
| Female (vs. Male) | 0.76 (0.48, 1.20) | 0.24 | 1.07 (0.72, 1.58) | 0.74 |
| Race | 0.04 | 0.22 | ||
| White | Ref. | Ref. | ||
| African-American | 0.99 (0.53, 1.87) | 1.53 (0.98, 2.41) | ||
| Hispanic | 3.15 (1.33, 7.50) | 1.39 (0.80, 2.42) | ||
| Other | 1.97 (0.95, 4.08) | 1.21 (0.62, 2.37) | ||
| Insurance | 0.27 | 0.64 | ||
| Public | Ref. | Ref. | ||
| Private | 1.10 (0.54, 2.21) | 0.86 (0.51, 1.43) | ||
| Other | 1.70 (0.89, 3.26) | 1.30 (0.66, 2.54) | ||
| Moderate/Severe Head Injury (vs. Minor) | 7.10 (2.75, 18.35) | <0.001 | 2.25 (1.19, 4.27) | 0.01 |
| Discharge Year | <0.001 | 0.51 | ||
| 2009 | Ref. | Ref. | ||
| 2010 | 0.54 (0.26, 1.10) | 0.80 (0.46, 1.41) | ||
| 2011 | 0.68 (0.32, 1.44) | 0.60 (0.30, 1.19) | ||
| 2012 | 1.16 (0.57, 2.34) | 0.99 (0.56, 1.74) | ||
| 2013 | 2.08 (1.03, 4.17) | 0.91 (0.49, 1.67) | ||
| Hospital-Level Factors | ||||
| Increasing Hospital All-Type Injury Volume (Log Base 2 Scale) | 0.98 (0.72, 1.35) | 0.92 | 1.19 (0.93, 1.51) | 0.17 |
| Teaching Hospital (vs. Non-Teaching) | 1.70 (0.61, 4.78) | 0.31 | 1.22 (0.56, 2.66) | 0.61 |
| Urban Location (vs. Rural) | 0.63 (0.14, 2.81) | 0.54 | 0.58 (0.24, 1.42) | 0.24 |
| Region | 0.23 | 0.13 | ||
| South | Ref. | Ref. | ||
| Midwest | 0.59 (0.22, 1.63) | 0.39 (0.17, 0.90) | ||
| Northeast | 0.07 (0.004, 1.13) | 0.92 (0.35, 2.43) | ||
| West | 0.95 (0.40, 2.28) | 1.02 (0.42, 2.47) | ||
AHT: Abusive Head Trauma
Variation in Advanced Cervical Imaging
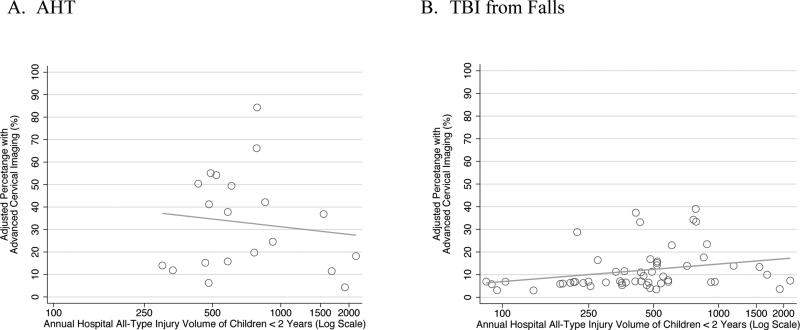
After limiting our sample to only those hospitals with 5 patients with AHT or TBI from falls, 361 children with AHT from 20 hospitals and 1,142 children with TBI from falls from 55 hospitals remained in our Larger Hospital Volume AHT and Falls Cohorts (Figure 1). The unadjusted percentage of children undergoing cervical MRI ranged from 0 to 54.5% for AHT and 0 to 16.7% for falls across hospitals. The unadjusted percentage of children who received cervical CT was 0 to 63.6% for AHT and 0 to 50% for falls. The unadjusted percentage of children undergoing advanced cervical imaging (either CT or MRI) at each hospital ranged from 0 to 75.0% for AHT and 0 to 50.0% for falls. After adjustment for patient characteristics, there was statistically significant variation (P <0.001) in the adjusted probability of advanced cervical imaging across hospitals in cases of AHT and falls. The adjusted probability of advanced cervical imaging across hospitals ranged from 4.3 to 84.3% in children with AHT (Figure 2A) and 3.1 to 39.0% in children with falls (Figure 2B). Figure 2 graphically demonstrates the lack of clear association between hospital all-type injury volume and the hospital-level adjusted probability of advanced cervical imaging.
FIGURE 2.
Relationship between hospital all-type injury volume and adjusted percentage of children undergoing cervical imaging with AHT (A) and TBI from falls (B). Each point represents the adjusted percentage undergoing imaging at a hospital calculated from a mixed-effects model with hospital-specific random intercepts and adjusted for age, gender, race, insurance, head injury severity, and year.
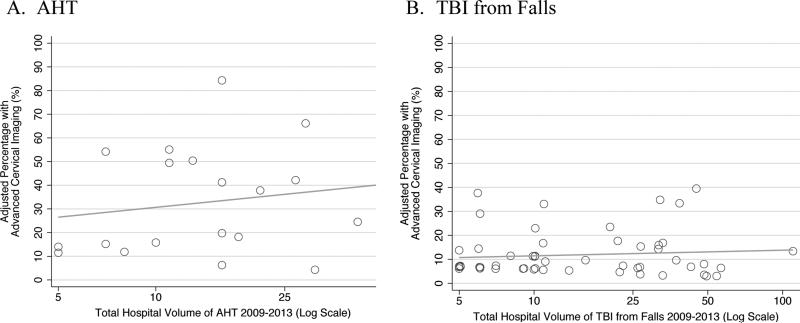
Sensitivity analyses
Restricting the outcome to CT (with or without MRI) did not alter the direction or statistical significance of factors previously identified as being associated with advanced cervical imaging. After limiting our outcome to CT, significant (P <0.001) adjusted hospital variation in cervical imaging remained among cases of AHT (6.3 to 51.9%) and falls (2.8 to 38.4%). After including transfers, the adjusted percentage undergoing advanced cervical imaging remained significant and ranged from 6.2 to 78.2% in AHT and 4.8 to 25.1% in TBI from falls. There was an even spread of low and high adjusted probabilities of imaging across all total hospital volumes of AHT (Figure 3A) and TBI from falls (Figure 3B).
FIGURE 3.
Inter-hospital variation in advanced cervical imaging of children with AHT ordered by total hospital volume of AHT (A) and TBI from falls (B). Adjusted hospital-level percentages were calculated from mixed-effects models with hospital-specific random intercepts and adjusted for age, gender, race, insurance, head injury severity, and year.
Discussion
Our results demonstrate nearly 20-fold inter-hospital variation in the use of advanced cervical imaging in children with AHT and over 10-fold inter-hospital variation in imaging in children with TBI from falls despite adjustment for observed differences in patient populations across hospitals. We found that decisions to image were influenced by both head injury severity and age, but were not influenced by annual hospital volume of injured children. While hospital variation was statistically significant for both children with AHT and TBI from falls, the notable variation in AHT highlights a population in need of further study.
This study sought to illuminate the need for evidence-based practices to improve the quality of care that young children with TBI receive and to motivate research to define optimal use of advanced cervical imaging. While this study cannot define optimal cervical imaging strategies, our finding of excessive practice variation across hospitals, persisting despite thorough adjustment for observed patient characteristics—with nearly 20-fold variation across hospitals among children with AHT and over 10-fold variation across hospitals among children with TBI from falls—provides strong evidence that we need to clarify optimal use of advanced cervical imaging to prevent over or under imaging.
Our Overall TBI Cohort was similar in composition to national estimates of the percentages of children with TBI presenting to children's and non-children's hospitals. Past work has shown that only 11% of children with TBI present to children's hospitals.12 Similarly, we found that 16.3% of our entire cohort and 13.3% of children with TBI from falls received care at pediatric centers. While 22.6% of children ultimately diagnosed with AHT presented to pediatric centers, this finding may be reflective of children's hospitals being more likely to diagnose abuse in infants than general hospitals.24
Only 15.0% of children in our cohort underwent advanced cervical imaging (CT or MRI), with 13.3% of our cohort undergoing CT and 3.6% undergoing MRI. In contrast, 30.6% of children < 3 years presenting between 1995 and 2005 following blunt trauma underwent cervical CT in a prior study.10 This discrepancy may be due to differences in injury severity and risk of cervical injury between study populations or differences in study time period. Efforts to reduce pediatric radiation exposure in children, such as the Image Gently® campaign25 that launched in 2007, may have played a role in the relatively lower use of CT in our contemporary cohort. However, cervical CT use increased in children < 18 years with TBI between 2001 and 2011 at select children's hospitals, though the rate of rise appears to have slowed in the mid 2000s.11
Our study is not without limitations. Due to our use of an administrative dataset, our case definitions of children with TBI and the subcohorts of falls, AHT, and MVCs rely on ICD-9-CM codes and are subject to misclassification from errors in coding and clinical errors in diagnosis. ICD-9-CM codes have been shown to have greater than 90% sensitivity and specificity for identification of AHT at a tertiary children's hospital among children evaluated for possible AHT by the child protection team.26 A study of 4 children's hospitals demonstrated that abuse ICD-9-CM codes among children with TBI who underwent evaluation by a child abuse pediatrician had a sensitivity of 85.0% and specificity of 92.1% in correctly identifying abused children.27 The use of ICD-9-CM codes to identify children with AHT at non-children's hospitals and hospitals without abuse specialists, however, has not been validated. Use of ICD-9-CM codes to calculate the incidence of AHT in children less than 1 year of age using nationally weighted administrative data of pediatric admissions (not limited to children's hospitals) produced comparable incidence estimates to those derived from a study using a prospective AHT surveillance strategy of all hospitals in North Carolina.28,29 This finding may suggest that use of ICD-9-CM codes at non-children's hospitals is a reasonable strategy for AHT incidence estimation and, perhaps, AHT identification. However, the validity of AHT cases identified through ICD-9-CM codes at non-children's hospitals remains unknown.
Our study is also limited by the lack of pre-imaging clinical exam findings and imaging results and by the small sample size at some hospitals. Specific clinical findings that we were unable to capture may be critical to imaging decisions (such as posterior midline cervical spine tenderness). We also elected to control for head injury severity only rather than global injury severity, which may result in incomplete severity adjustment. Use of a global measure of injury severity would, however, include cervical injuries. As children with cervical injuries would have by definition undergone cervical imaging (our primary outcome), use of total injury severity would have introduced circular reasoning into our models. In addition, the ICD-9-CM codes used to calculate head injury severity scores reflect all injuries known at the time of discharge with the benefit of hindsight and not necessarily those injuries known at the time of decisions about cervical imaging. Despite this major limitation, children with more severe head injuries were more likely to undergo cervical imaging in our models, lending face validity to our severity adjustment. Finally, our variation analyses are limited by the small sample size of some hospitals. However, as total hospital volume of AHT or TBI from falls increased, there was no clear decrease in the spread of adjusted probabilities of imaging. This suggests that hospitals with low volumes of AHT and TBI from falls were not disproportionately driving our findings.
Current cervical imaging guidelines of children less than 2 years with suspected abuse recommend cervical radiographs as part of a complete skeletal survey, but these guidelines do not specifically address advanced cervical imaging.30,31 Young children with AHT may be particularly at risk for ligamentous injuries that are often not apparent on plain radiography or CT but detectable on MRI. When MRI is performed, ligamentous injuries are detected in up to 78% of cases of AHT, compared to 46% of children with accidental trauma (not necessarily TBI) and 1% of children without trauma.6 These findings raise the question of whether MRI could have forensic utility to distinguish between traumatic and non-traumatic etiologies to aid in accurate determinations of abuse. Future studies are needed to inform the use of advanced cervical imaging to clarify whether the injuries revealed are of clinical or forensic significance. Understanding which patients benefit most from imaging is important because imaging is not without risk and cost: MRI carries risks associated with sedation while CT exposes young children to radiation. Key outcomes such as confidence of abuse diagnoses, clinical significance of injuries, cost, and adverse events (e.g., from sedation) should be explored prospectively at hospitals that frequently image these children.
Our results highlight variation in performance of advanced cervical imaging in young children with TBI from AHT and falls. This variation was not explained by observed differences in patient populations across hospitals or the annual volume of young injured children treated at each hospital. Further understanding of risk factors for cervical injuries and indications for specific types of cervical imaging are needed to improve the quality of care this young population receives.
What's New.
Statistically significant variation in cervical imaging of children < 2 years with traumatic brain injury from falls and abuse exists across hospitals. This study highlights opportunities for further research to inform the role of cervical imaging in this young population.
Acknowledgements
We thank Kristina B. Metzger, PhD, MPH for her assistance in calculating head injury severity scores for our analyses.
Funding Source: This study was supported by internal funds.
Salary support was provided by the NIH/NICHD institutional training grant 5T32H060550-05 (Dr. Henry) and NIH/NICHD Career Development Awards 1K23HD071967-04 (Dr. Wood) and K08HD073241 (Dr. Zonfrillo). The Children's Hospital of Philadelphia has received payment for Dr. Wood's expert testimony following subpoenas in cases for suspected child abuse. This project was supported by grant number F32HS024194 from the Agency for Healthcare Research and Quality.
Abbreviations
- AHT
Abusive Head Trauma
- AIS
Abbreviated Injury Scale
- CDC
Centers for Disease Control
- CI
Confidence Interval
- CT
Computed Tomography
- ICD-9-CM
International Classification of Diseases, 9th revision, Clinical Modification
- MAIS
Maximum Abbreviated Injury Scale
- MRI
Magnetic Resonance Imaging
- MVCs
Motor Vehicle Crashes
- OR
Odds Ratio
- PPD
Premier Perspective Database
- TBI
Traumatic Brain Injury
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial Disclosure Statement: The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality. The above grants did not play a role in study design, data collection, writing of the report, or the decision to submit the article for publication.
Conflict of Interest: None
References
- 1.Keenan HT, Bratton SL. Epidemiology and outcomes of pediatric traumatic brain injury. Dev Neurosci. 2006;28(4-5):256–263. doi: 10.1159/000094152. [DOI] [PubMed] [Google Scholar]
- 2.Brown RL, Brunn MA, Garcia VF. Cervical spine injuries in children: a review of 103 patients treated consecutively at a level 1 pediatric trauma center. Journal of pediatric surgery. 2001;36(8):1107–1114. doi: 10.1053/jpsu.2001.25665. [DOI] [PubMed] [Google Scholar]
- 3.Cirak B, Ziegfeld S, Knight VM, et al. Spinal injuries in children. J Pediatr Surg. 2004;39(4):607–612. doi: 10.1016/j.jpedsurg.2003.12.011. [DOI] [PubMed] [Google Scholar]
- 4.Givens TG, Polley KA, Smith GF, Hardin WD., Jr. Pediatric cervical spine injury: a three-year experience. J Trauma. 1996;41(2):310–314. doi: 10.1097/00005373-199608000-00019. [DOI] [PubMed] [Google Scholar]
- 5.Kadom N, Khademian Z, Vezina G, et al. Usefulness of MRI detection of cervical spine and brain injuries in the evaluation of abusive head trauma. Pediatr Radiol. 2014;44(7):839–848. doi: 10.1007/s00247-014-2874-7. [DOI] [PubMed] [Google Scholar]
- 6.Choudhary AK, Ishak R, Zacharia TT, Dias MS. Imaging of spinal injury in abusive head trauma: a retrospective study. Pediatr Radiol. 2014;44(9):1130–1140. doi: 10.1007/s00247-014-2959-3. [DOI] [PubMed] [Google Scholar]
- 7.Brennan LK, Rubin D, Christian CW, et al. Neck injuries in young pediatric homicide victims. J Neurosurg Pediatr. 2009;3(3):232–239. doi: 10.3171/2008.11.PEDS0835. [DOI] [PubMed] [Google Scholar]
- 8.Percent Distributions of TBI-related Hospitalizations by Age Group and Injury Mechanism - United States, 2006-2010. Centers for Disease Control and Prevention; [March 13, 2015]. website. http://www.cdc.gov/traumaticbraininjury/data/dist_hosp.html. Updated February 34, 2014. [Google Scholar]
- 9.Fesmire FM, Luten RC. The pediatric cervical spine: developmental anatomy and clinical aspects. J Emerg Med. 1989;7(2):133–142. doi: 10.1016/0736-4679(89)90258-8. [DOI] [PubMed] [Google Scholar]
- 10.Pieretti-Vanmarcke R, Velmahos GC, Nance ML, et al. Clinical clearance of the cervical spine in blunt trauma patients younger than 3 years: a multi-center study of the american association for the surgery of trauma. J Trauma. 2009;67(3):543–549. doi: 10.1097/TA.0b013e3181b57aa1. discussion 549-550. [DOI] [PubMed] [Google Scholar]
- 11.Bennett TD, Bratton SL, Riva-Cambrin J, et al. Cervical Spine Imaging in Hospitalized Children With Traumatic Brain Injury. Pediatr Emerg Care. 2015;31(4):243–249. doi: 10.1097/PEC.0000000000000395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Densmore JC, Lim HJ, Oldham KT, Guice KS. Outcomes and delivery of care in pediatric injury. J Pediatr Surg. 2006;41(1):92–98. doi: 10.1016/j.jpedsurg.2005.10.013. discussion 92-98. [DOI] [PubMed] [Google Scholar]
- 13.Marin JR, Wang L, Winger DG, Mannix RC. Variation in Computed Tomography Imaging for Pediatric Injury-Related Emergency Visits. J Pediatr. 2015;167(4):897–904. doi: 10.1016/j.jpeds.2015.06.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Oderda GM, Gan TJ, Johnson BH, Robinson SB. Effect of opioid-related adverse events on outcomes in selected surgical patients. J Pain Palliat Care Pharmacother. 2013;27(1):62–70. doi: 10.3109/15360288.2012.751956. [DOI] [PubMed] [Google Scholar]
- 15.Fisher BT, Lindenauer PK, Feudtner C. In-Hospital Dabases. In: Strom BL, Kimmel SE, Hennessy S, editors. Pharmacoepidemiology. 5th ed. Hoboken Wiley-Blackwell; Chichester, West Sussex, UK: 2012. pp. 244–258. [Google Scholar]
- 16.Robinson SB, Ernst FR, Lipkin C, Huang X. Patient Outcomes on Day 4 of Intravenous Antibiotic Therapy in Non-Intensive Care Unit Hospitalized Adults With Community- Acquired Bacterial Pneumonia. Infect Dis Clin Pract. 2014;22(6):320–325. doi: 10.1097/IPC.0000000000000143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Parks SE, Annest JL, Hill HA, Karch DL. Pediatric Abusive Head Trauma: Recommended Definitions for Public Health Surveillance and Research. Centers for Disease Control and Prevention; Atlanta: 2012. [Google Scholar]
- 18.Chung S, Mikrogianakis A, Wales PW, et al. Trauma association of Canada Pediatric Subcommittee National Pediatric Cervical Spine Evaluation Pathway: consensus guidelines. J Trauma. 2011;70(4):873–884. doi: 10.1097/TA.0b013e3182108823. [DOI] [PubMed] [Google Scholar]
- 19.The Association for the Advancement of Automotive Medicine . Abbreviated Injury Scale (AIS) 2005 - Update 2008. The Association for the Advancement of Automotive Medicine; Barrington, IL: 2008. [PMC free article] [PubMed] [Google Scholar]
- 20.MacKenzie EJ, Steinwachs DM, Shankar B. Classifying trauma severity based on hospital discharge diagnoses. Validation of an ICD-9CM to AIS-85 conversion table. Med Care. 1989;27(4):412–422. doi: 10.1097/00005650-198904000-00008. [DOI] [PubMed] [Google Scholar]
- 21.Durbin DR, Localio AR, MacKenzie EJ. Validation of the ICD/AIS MAP for pediatric use. Inj Prev. 2001;7(2):96–99. doi: 10.1136/ip.7.2.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.French B, Farjah F, Flum DR, Heagerty PJ. A general framework for estimating volume- outcome associations from longitudinal data. Stat Med. 2012;31(4):366–382. doi: 10.1002/sim.4410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Normand ST, Shahian DM. Statistical and Clinical Aspects of Hospital Outcomes Profiling. Stat Sci. 2007;22(2):206–226. [Google Scholar]
- 24.Trokel M, Waddimba A, Griffith J, Sege R. Variation in the diagnosis of child abuse in severely injured infants. Pediatrics. 2006;117(3):722–728. doi: 10.1542/peds.2004-2731. [DOI] [PubMed] [Google Scholar]
- 25.The Alliance for Radiation in Pediatric Imaging. Campaign Overview. [October 5, 2015];Image Gently. website. http://www.imagegently.org/FAQs-More/Campaign-Overview.
- 26.Berger RP, Parks S, Fromkin J, et al. Assessing the accuracy of the International Classification of Diseases codes to identify abusive head trauma: a feasibility study. Inj Prev. 2015;21(e1):e133–137. doi: 10.1136/injuryprev-2013-040924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hooft AM, Asnes AG, Livingston N, et al. The Accuracy of ICD Codes: Identifying Physical Abuse in 4 Children's Hospitals. Acad Pediatr. 2015;15(4):444–450. doi: 10.1016/j.acap.2015.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ellingson KD, Leventhal JM, Weiss HB. Using Hospital Discharge Data to Track Inflicted Traumatic Brain Injury. Am J Prev Medicine. 2008;34(4):S157–S162. doi: 10.1016/j.amepre.2007.12.021. [DOI] [PubMed] [Google Scholar]
- 29.Keenan HT, Runyan DK, Marshall SW, et al. A population-based study of inflicted traumatic brain injury in young children. JAMA. 2003;290(5):621–626. doi: 10.1001/jama.290.5.621. [DOI] [PubMed] [Google Scholar]
- 30.The American College of Radiology ACR-SPR Practice Parameter for Skeletal Surveys in Children. [December 18, 2014];American College of Radiology. website. http://www.acr.org/~/media/9bdcdbee99b84e87baac2b1695bc07b6.pdf. Published 1997. Amended 2014.
- 31.The American Academy of Pediatrics Section on Radiology Diagnostic imaging of child abuse. Pediatrics. 2009;123(5):1430–1435. doi: 10.1542/peds.2009-0558. [DOI] [PubMed] [Google Scholar]