Abstract
Smartphone-based interventions are increasingly used to support self-monitoring, self-management, and treatment and medication compliance in order to improve overall functioning and well-being. In attempting to develop a smartphone application (S-Health) that assists heroin-dependent patients in recovery, a series of focus groups (72 patients, 22 providers) were conducted in China, Taiwan, and the USA to obtain their perspectives on its acceptance and potential adoption. Data were analyzed according to the Diffusion of Innovation (DOI) theory of characteristics important to the adoption of innovation. Important to Relative Advantage, USA participants cited S-Health’s potential ability to overcome logistical barriers, while those in China and Taiwan valued its potential to supplement currently limited services. In terms of Compatibility, participants across sites reported recovery needs and goals that such an application could be helpful in supporting; however, its utility during strong craving was questioned in China and Taiwan. Important factors relevant to Complexity included concerns about smartphone access and familiarity, individualization of content, and particularly in China and Taiwan, participants wanted assurance of privacy and security. The study results suggest a general acceptance, but also indicate cultural variations in access to therapeutic and other social support systems, legal repercussions of substance use, societal perceptions of addiction, and the role of family and other social support in recovery. Taking these factors into consideration is likely to increase diffusion as well as effectiveness of these smartphone-based interventions.
Keywords: Smartphone application, Recovery from heroin addiction, Diffusion of innovation theory, S-Health
Introduction
Opiate addiction is a growing global health problem. A recent review of worldwide dependence rates and burden of disease due to dependence found a remarkable increase over the past few decades (Degenhardt et al. 2014). Worldwide estimates indicate that approximately 16.5 million people age 15 and older had used heroin or opium (United Nations Office on Drug and Crime 2013), with just under a quarter likely to develop dependence (NIDA, 2014). When examined regionally, Asia is estimated to suffer greatly in terms of absolute numbers of users and gross annual mortality rate (Degenhardt et al. 2014; Narcotics Control Bureau of the Ministry of Public Security P. R. China 2014). The chronic relapsing condition of heroin addiction requires long-term care and management (Hser et al. 2015). Although North America has greater resources and access to care in comparison to much of the world, it continues to demonstrate some of the highest prevalence rates (Degenhardt et al. 2014). As a result, addressing the health risks and consequences associated with heroin use, particularly injection drug use, and the long-term treatment needs of individuals with heroin use disorder are of great concern in both the eastern and western world.
Globally, 60–80 % of IDUs are HCV positive (Nelson et al. 2011) and approximately 3 million IDUs are living with HIV (WHO, 2015), often the result of engaging in high risk behaviors such as risky sexual behaviors, sharing of injection equipment, and poor sterilization procedures (Duan et al. 2013; Magiorkinis et al. 2013; Ng et al. 2013; Quaglio et al. 2003). With a large proportion of risk due to injection drug practices, both Taiwan and China experienced a major surge in the number of reported HIV cases among IDUs beginning in the early 2000s (Lan et al. 2008; Chen et al. 2006; Chen and Kuo 2007). Although HIV prevalence rates are declining in these regions, it remains a major public health problem. And in the USA, HCV is now the most common blood-borne viral infection; it is estimated that of the approximately 5.2 million living with HCV, 80 % will develop chronic HCV (Klevens et al. 2012; Chak et al. 2011). Among all regions, co-infection of HCV and HIV is not uncommon among injection drug users and untreated chronic HCV infection is associated with increased risk for cirrhosis and liver cancer, both of which are costly and life-threatening (Lewden et al. 2005; Rosen 2011; Weber et al. 2006). Thus, it is imperative that drug treatment incorporate education and behavioral skills training related to preventing further transmission of these illnesses as well as managing personal health needs resulting from infection.
Treatment for Heroin Addiction in China, Taiwan, and the USA
Methadone maintenance treatment (MMT) is a medication for the treatment of opiate dependence which has proven useful in reducing drug use and cravings as well as risk for HIV and HCV infection (DAunno et al. 2014; Des Jarlais and Semaan 2008; Nolan et al. 2014; Mattick et al. 2009). MMT has been used in the USA for the treatment of heroin addiction since 1965 (Dole and Nyswander 1965; Kleber 2008) and there are currently about 1200 methadone programs throughout the country (SAMHSA 2013). In China and Taiwan, both governments began introducing and rapidly scaling up MMT programs around the mid-2000s in response to the growing numbers of IDUs and HIV infection rates (Chen and Kuo 2007; Huang et al. 2011, Sullivan and Wu 2007). By the end of 2014, China and Taiwan estimated approximately 767 and 122 clinics respectively (WHO, World Health Organization 2014; Taiwan Ministry of Health and Welfare 2015).
Although China has witnessed an increase in public assistance and a more patient-oriented perception of addiction, heroin users are still highly stigmatized and marginalized in their communities and by their families (Gao and Pan 2014). The proliferation of MMT clinics has allowed for greater access to this treatment, especially in certain regions such as Shanghai, but resources are limited in most other parts of the country. Thus, cost of travel makes accessing MMT too expensive for some (Wu et al. 2012). Moreover, behavioral psychotherapeutic treatment options are even more scant; although there has been an increase in social workers providing some services through community rehabilitation programs, few are well-trained and few are outside of Shanghai (Li 2013). Similarly, MMT providers lack training in counseling and optimal methadone dosing in China—factors likely contributing to high drop-out rates and continued heroin use while enrolled in MMT (Yin et al. 2010).
Starting in 2009, Taiwan began training MMTstaff in family and community-based interventions; these services were then linked with their existing social worker system in order to implement the Taiwan Department of Health harm reduction policy (Lyu et al. 2012; Chou et al. 2013). Most MMT and other addiction-related services are on demand and require the patient to pay associated fees, the exception being full coverage granted to HIV-positive patients (Chou et al. 2013). Similar to China, addiction has a very strong criminal stigma. Its uncommon for MMT treatment to offer psychosocial services and few staff has formal psychosocial therapeutic training (Lee et al. 2011). Oftentimes family services are poorly attended due to the strained or broken relationship (Lee et al. 2011). Neither China nor Taiwan allow for take-home policy in MMT.
In the USA, MMT is offered through either public or private methadone clinics and can be found in all states except for North Dakota and Wyoming (SAMSHA, 2015). Methadone dosing is viewed as only a piece of a larger treatment and recovery plan; clinics require participation in group and/or individual therapy sessions (SAMHSA, 2015). Behavioral psychotherapy for patients receiving methadone focuses on teaching cognitive behavioral strategies (McHugh et al. 2010) and providing motivational enhancement tools (McCann et al. 1994; Miller and Rollnick 1991) that help bolster relapse prevention skills beyond the medication’s suppression of physical cravings (McCann et al. 1994). The therapeutic process aims to give patients skills for identifying triggers for use through understanding previous relapses or moments of intense craving and giving them skills for coping with the emotional and physical distress. Additionally, long-term recovery plans in the USA promote the identification and use of social support networks through such groups as Alcoholics Anonymous (AA) and Narcotics Anonymous (NA). The groups help to lessen isolation and shame and to promote accountability through peer support (Kelly 2003). For some MMT patients, however, certain AA/ NA groups may cause additional shame due to the group’s traditional perception that methadone is a drug and not a medication (Vigilant 2004; White 2011). Although heroin addiction continues to be stigmatized in the USA, there is a general belief that counseling is a vital component of recovery (Dutra et al. 2008; Olsen and Sharfstein 2014; White 2009).
Adoption of Smartphone Application as a Recovery Tool
With over 2 billion smartphone users estimated worldwide in 2016 (eMarketer 2014), smartphone applications can help provide behavioral tools at low-cost to hard-to-reach populations who may not otherwise have access to traditional psychoeducational or psychotherapeutic services (Gibbons et al. 2011). Investigation of behavioral intervention strategies for substance use disorder (Johnson et al. 2011; Marsch 2012; Moore et al. 2011) and HIV prevention (see Noar and Willoughby 2012 for review) within a technology-based format have recently begun to yield promising results. Supportive and educational text messages have been shown to increase positive health behaviors and abstinence (Fjeldsoe et al. 2009; Reback et al. 2012). In particular, studies examining interventions delivered via mobile phones have demonstrated positive outcomes in terms of reducing relapse episodes (Chih et al. 2014) and increasing HIV medication adherence (Ingersoll et al. 2015) among substance using populations. While mobile health interventions have demonstrated good compliance and perceived credibility among participants overall, non-tailored content and timing are less favorably received (Heron and Smyth 2010). A-CHESS, a smartphone application designed to provide monitoring, information, communication, and support to alcohol dependent patients leaving residential treatment, has demonstrated positive results; those receiving the smartphone application had significantly fewer risky drinking days and a higher likelihood of abstinence than those receiving treatment as usual (Gustafson et al. 2014). Thus, technology-based recovery and health management interventions appear to be a useful tool in promoting abstinence and positive health behaviors.
Simply constructing smartphone applications, however, is not enough. The best designed applications are of little use if not adopted by the target population. Diffusion of Innovation (DOI) theory describes the process by which an innovation (i.e., new idea, product, or behavior) is adopted by a specific population as dependent on the communication channels within that social system (Rogers 2002). Adoption and diffusion occur over time, with an innovation’s rate of adoption determined by five main perceived characteristics of the innovation: (1) Relative Advantage is the degree to which an innovation is seen as better than the idea, program, or product it replaces; (2) Compatibility describes how consistent the innovation is with the values, experiences, and needs of the potential adopters; (3) Complexity is how difficult the innovation is to understand and/or use; (4) Triability is the extent to which the innovation can be tested or experimented with before a commitment to adopt is made; (5) Observability describes the extent to which the innovation provides tangible results. Thus, innovations perceived not to be better than what is currently available, inconsistent with social norms and values, require the acquisition of new skills or knowledge, and that do not allow potential adopters trial test or view the results of others will be adopted more slowly or possibly not at all. Examining these factors during the development phase of a new product can therefore help to increase the likelihood it is accepted and used by the target population.
Current Study
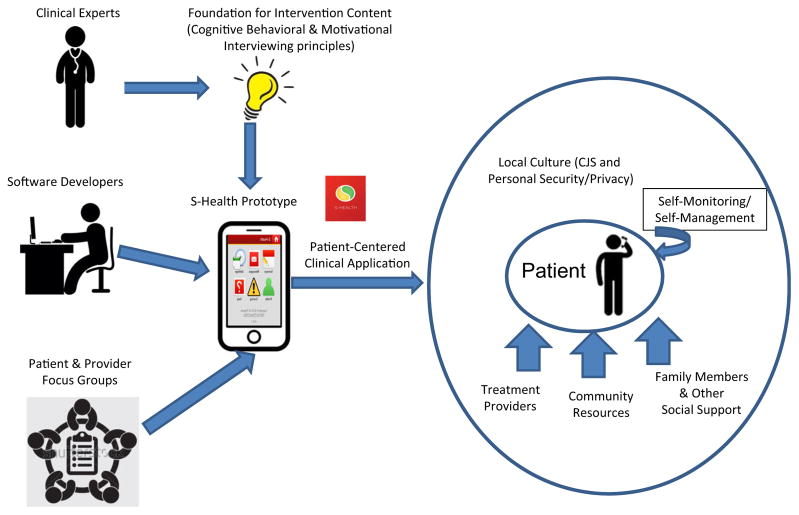
In attempting to develop a smartphone application (S-Health) that supports self-monitoring, self-management, and treatment and medication compliance to improve overall functioning and well-being among opioid-dependent patients, a series of processes and activities are involved. As illustrated in Fig. 1, clinical experts in addiction develop the text content based on cognitive behavioral and motivational interviewing principles. Software developers help identify potential security and data collection issues, program the application, and produce the prototype. S-Health is designed to provide opioid-dependent patients the ability to better identify triggers (e.g., emotions, places, people) and practice in-the-moment coping for relapse prevention. To support a patient-centered approach, the clinical application of S-Health should take advantage or involve family members and other social support, treatment providers, and other community resources. Therefore, grounded in DOI theory, we adopted a qualitative approach to solicit input regarding the application’s design and functionality in a series of patient and provider focus groups conducted in China, Taiwan, and the USA during the developmental phase with special focus on cross-cultural factors influencing variation in acceptance and implementation of S-Health.
Fig. 1.
Conceptualization and development of S-Health
This article reports findings based on participant feedback regarding the first three factors impacting the likelihood and rate of adoption of S-Health. Triability and Observability were not included as primary categories because the purpose of the focus groups were to collect information about the acceptability and utility of S-Health within a research study; these factors were deemed irrelevant for this context since participants would not be allowed to use the application prior to study enrollment nor would they be able to view the results of others. Triability and Observability would be, however, useful in assessing the adoption of diffusion of S-Health among substance abusing populations after it has been formally tested and readily available to non-research participants. We hypothesize that the social and legal systems within each of the countries, particularly as it relates to access to MMT and behavioral psychotherapeutic services, will impact DOI innovation factors.
Methods
Participants
Table 1 presents the demographic characteristics of study participants. In total, 72 patients participated: 14 were from Taiwan, 18 from China, and 40 from the USA. Provider groups consisted of 5, 7, and 10 participants from each of the respective regions. Participants were required to own a smartphone in order to participate in the focus groups. Across groups, approximately 55 % were female. The majority of participants were middle age.
Table 1.
Demographics summary
| USA | China | Taiwan | ||||
|---|---|---|---|---|---|---|
| Patients | n = 40 | n = 18 | n = 14 | |||
| Race/ethnicity (n, %) | ||||||
| Hispanic | 12 | 30.0 % | 0 | 0 % | 0 | 0 % |
| Asian | 0 | 0 % | 18 | 100.0 % | 14 | 100.0 % |
| Black | 15 | 37.5 % | 0 | 0 % | 0 | 0 % |
| Other | 4 | 10.0 % | 0 | 0 % | 0 | 0 % |
| Caucasian/White | 8 | 20.0 % | 0 | 0 % | 0 | 0 % |
| Multiracial | 1 | 2.5 % | 0 | 0 % | 0 | 0 % |
| Age (range) | (23–68) | (32–60) | (35–53) | |||
| Female (n, %) | 26 | 65.0 % | 7 | 38.9 % | 5 | 35.7 % |
| Education (n, %) | ||||||
| Less than High School | 5 | 12.5 % | 7 | 38.9 % | 5 | 35.7 % |
| High School Diploma or Equivalent | 12 | 30.0 % | 8 | 44.4 % | 9 | 64.3 % |
| Some College (no degree) | 9 | 22.5 % | 2 | 11.1 % | 0 | 0 % |
| 2 Year College | 6 | 15.0 % | 1 | 5.6 % | 0 | 0 % |
| 4 Year College | 2 | 5.0 % | 0 | 72.2 % | 0 | 0 % |
| Trade/Technical Training | 4 | 10.0 % | 0 | 0 % | 0 | 0 % |
| Master’s Degree | 0 | 0 % | 0 | 0 % | 0 | 0 % |
| Employment (n, %) | ||||||
| Employed Full-Time | 2 | 5.0 % | 5 | 27.8 % | 6 | 42.9 % |
| Employed Part-Time | 10 | 25.0 % | 0 | 0 % | 2 | 14.3 % |
| Unemployed | 28 | 70.0 % | 13 | 72.2 % | 6 | 42.9 % |
| Providers | n = 10 | n = 7 | n = 5 | |||
| Race/ethnicity (n, %) | ||||||
| Hispanic | 0 | 0 % | 0 | 0 % | 0 | 0 % |
| Asian | 1 | 10.0 % | 7 | 100.0 % | 5 | 100 % |
| Black | 2 | 20.0 % | 0 | 0 % | 0 | 0 % |
| Other | 1 | 10.0 % | 0 | 0 % | 0 | 0 % |
| Caucasian/White | 4 | 40.0 % | 0 | 0 % | 0 | 0 % |
| Multiracial | 2 | 20.0 % | 0 | 0 % | 0 | 0 % |
| Age (range) | (25–70) | (28–56) | 31–38 | |||
| Female (n, %) | 6 | 60.0 % | 4 | 57.1 % | 4 | 80.0 % |
| Education (n, %) | ||||||
| Less than High School | 0 | 0 % | 0 | 0 % | 0 | 0 % |
| High School Diploma or Equivalent | 0 | 0 % | 2 | 28.6 % | 1 | 20.0 % |
| Some College (no degree) | 1 | 10.0 % | 0 | 0 % | 0 | 0 % |
| 2 Year College | 0 | 0 % | 2 | 28.6 % | 0 | 0 % |
| 4 Year College | 3 | 30.0 % | 2 | 28.6 % | 4 | 80.0 % |
| Trade/Technical Training | 0 | 0 % | 0 | 0 % | 0 | 0 % |
| Master’s Degree | 6 | 60.0 % | 1 | 14.3 % | 0 | 0 % |
| Employment (n, %) | ||||||
| Employed Full-Time | 7 | 70.0 % | 7 | 100.0 % | 5 | 100 % |
| Employed Part-Time | 2 | 20.0 % | 0 | 0 % | 0 | 0 % |
| Unemployed | 1 | 10.0 % | 0 | 0 % | 0 | 0 % |
Procedures
A total of 12 focus groups were conducted with MMT patients (2 in Taiwan, 3 in China, 4 in the USA) and service providers (1 in Taiwan, 1 in China, and 1 in the USA). Each focus group contained between 5 and 11 participants. In Taiwan, the focus groups were convened in two cities, Taichung and Taoyuan. In China, the groups were conducted in three Shanghai districts, Xuhui, Hongkou, and Yangpu. Focus groups in the USA met in Los Angeles, California.
Service providers and patients were invited via recruitment flyers posted in areas of the MMT clinics. All service providers invited to the meeting were persons who worked in MMT clinics and all patients were current or former patients of MMT clinics. Procedures were approved by the Institutional Review Board in University of California Los Angeles, Shanghai Mental Health Center, and China Medical University, Taiwan.
The same semi-structured discussion guide was applied to focus groups at all sites. Group discussion topics focused on participants’ current treatment options, recovery needs, triggers and coping strategies, and expectations regarding the utility and safety of S-Health as a relapse prevention tool. All focus groups were conducted in private rooms to ensure privacy and confidentiality and were approximately 1–2 h at length. Transcripts of group discussions were used for all patient and provider groups except for two patient groups in China; discussion notes were used in lieu of transcripts since transcripts were unavailable for these groups.
Analysis
Content analysis was used to analyze the focus group data. One bilingual graduate researcher developed initial code lists first. Open coding was completed to break each sentence into codes, using gerunds to understand, examine, and compare data with data. Gerunds are noun forms of verbs and are often used in the initial coding process of the grounded theory approach (Charmaz 2014). They allow for the coding of action and elucidate important processes (Charmaz 2012). In this paper, data is analyzed in the content analysis approach with grounded theory techniques (such as using gerunds for initial codes). Focus coding, developed by grouping similar initial coding together, was then used to identify categories and themes under the context of the first three factors of DOI theory: Relative Advantage, Compatibility, and Complexity. The code lists were then validated by another bilingual researcher. ATLAS.ti 7.5 is used for the analysis.
Results
Relative Advantage: S-Health Compared to Current Regional Treatment Options
Access to and acceptance of MMT, treatment center counseling services, and self-help support groups emerged as factors in the potential adoption of S-Health.
Access to Counseling Services and Support Groups
A common theme regarding the utility of and access to treatment counselors and support groups emerged within the groups. Patients in the USA appreciated the emotional support and advice they received from peers within the context of group counseling and AA/NA groups. All participants in the USA received MMT and group or individual services within their MMT clinic. They viewed groups as safe places in which participants could share their experiences, learn the science behind addiction, and relate to others. Providers in the USA stated that attending group sessions was a “learning experience” and they wished their clients could attend the group “around the clock.” Patients reported that they could avoid “isolation” and did not feel like an “outcast.”
“It’s a very low environment. Some are literally going under the bridge or under cardboard boxes. (Some) are going into a violent environment or just a using environment. Some of our patients live in dope galleries. They don’t have a choice in the matter. This is their only refuge that they—when they come here.” (USA provider)
Group counseling and self-help groups are not available for patients in China and Taiwan. Additionally, patients in both China and Taiwan reported negative perceptions towards behavioral interventions and group counseling. They generally perceived these as useless; they did not want to talk to strangers about their personal experiences. Patients in Taiwan said that they would avoid each other after the focus group, because they considered interacting with other patients as a major trigger.
“After most group therapies, or some classes, most of them will have fun together sometimes…After those classes, I will leave as quickly as possible, because I want to avoid meeting other users.”(Taiwan patient)
MMT Access and Treatment Concerns
Regional differences across sites were also observed regarding access to and perceptions of MMT. Patients from the USA did not voice concern regarding access to MMT; some perceived MMT as a natural part of their daily activities. For others, however, they reported concern about the consequences of long-term use of methadone and were interested in eventually stopping. USA providers indicated that family members did not understand and support MMT.
“We need for them to get stable because each individual – it takes ‘em a different length of time for a person to be stable on this type of medication. The family doesn’t see it that way. ‘You’ve been on it 2 weeks. You should be –Time to go. Get – coming off of this.’” (USA Provider)
Conversely, several issues were raised by patients in China and Taiwan. They expressed great concern about the side effects of MMT, their dependence on MMT, and the barriers they faced to accessing MMT. In Taiwan, patients complained that they could not go to MMT clinics in another city. As a result, they avoided traveling, or in some instances, used heroin to evade withdrawal symptoms if they left the city.
Providers in China cited several problems related to MMT utilization and treatment retention. They reported that most patients in MMT clinics were not highly motivated to stop using, with lack of money being the primary reason for receiving MMT. Further, they noted that heroin users were often hesitant to seek MMT because they feared they would be identified and registered by the public security sector. And for heroin users that did begin MMT, incarceration was cited as a common reason for discontinuation of methadone treatment.
“The MMT clinic is too far away. I have lots of work at home. I may not have the time, you know. My parents can be sick. I have got kids. Both my husband and I are taking methadone. If he was arrested, I had to take care of all the people at home. It is too far. I cannot take methadone every single day.” (China Patient)
“So many clients are not willing to participate in MMT, or just want to use MMT for transition. They want to stop methadone. If they enroll in MMT, they will be arrested when they check in a hotel (if they had a positive urine test). Their driving license will also be revoked. Many long-term MMT patients also want to stop MMT because of a lot of inconvenience in their lives.” (China Provider)
Despite these concerns surrounding MMT in China and Taiwan, patients generally perceived MMT as the most effective treatment method for heroin addiction.
S-Health Application as a Recovery Tool
Focus group participants across sites agreed that S-Health would be a useful tool for patients in treatment. It was not tied to the negative perceptions that patients in China and Taiwan associated with traditional therapy or support groups and felt that its focus on facilitating self-management was appealing.
“I think we should at least have a try. It should work. I think we should try as much as possible.” (Taiwan patient)
“I will definitely do it. I will try things which are helpful.” (China patient)
Compatibility: S-Health and Patient Experiences, Values, and Recovery Needs
Patients and providers across sites discussed the difficulty in avoiding relapse and the want for something to bolster their recovery efforts. Patients in China and Taiwan expressed greater concern over coping with physical cravings than patients in the USA, and noted they would not adopt the application if physical cravings were too high. All patients and providers, however, felt that S-Health had the potential to combat psychological cravings through enhancing their motivation for abstinence and providing relevant recovery and health information.
Work and Family are Important Motivating Factors in Recovery
Patients across sites reported a range of reasons for recovery, including avoiding withdrawal symptoms, improved quality of life, personal reputation, financial stability, positive family and social relationships, religion, and being “done” with the lifestyle associated with addiction. Motivation for becoming and staying abstinent, however, were highly individualized. Still, family and employment appeared to be the exception and resonated with patients across sites and at varying stages of recovery.
Patients and providers in all countries stated that securing regular employment was a top priority. Patients stated that working gave their lives structure; however, patients across sites reported facing a great deal of difficulty in finding a job. In China and Taiwan, patients reported receiving assistance from social workers and the government in job searches, but some were concerned that health problems would prevent them from being eligible for many positions. Providers in Taiwan complained that their patients were often fired if the employer learned of their status as a drug user.
When we talked with clients, we found that people usually relapsed when they did not have a job, or when they lost a job suddenly, or when they had a period of time waiting for the next assignment though they had a stable employment.”(Taiwan provider)
Patients and providers at all sites also agreed that family plays an important role in recovery. Patients reported that healthy family relationships served as a support and a significant motivator for staying abstinent. Conversely, negative relationships were often a factor in relapse. Providers in China and Taiwan stated they attempt to involve family, rebuild the relationships between patients and their family, and educate family members.
“My son was studying abroad when I was using at home. My wife called my son, saying that your Dad was still using in Shanghai and we were short of money. My son was studying in the US then. He did not continue his program and came back to Shanghai immediately. My son is very good. I will ruin him if I continue using, right? He came back, and I promised to him that I would never use again.” (China Patient)
“I would just say a lot of our recent admissions have been in the 25 or younger range. I’d say the family component, particularly from what I’ve seen of people in that age range, and especially when family members are providing some or all of the funds to pay for the treatment, that family component is crucial. …I’ve seen people make gains when we start addressing family issues that they were real stuck before.” (USA provider)
Triggers and Coping Methods
Patients stated that even when they are motivated to stay abstinent, they face many triggers for returning to use. Patients and providers at all sites agreed that associating with “old friends” that are still using is a primary trigger for relapse. Additionally, holidays, boredom, emotional strain, alcohol use, and physical cravings were also considered by patients and providers as major triggers at all sites.
“Family stress and alcohol make people start using again. A lot of our patients think they can drink socially but then it gets out of control.” (Provider Group, U.S.)
“I met one of my patients several days ago. He said he didn’t use heroin for more than 3 years and kept using methadone in MMT. But he met the old friends (they got to know in the compulsory rehabilitation center). Now they get together and relapse.” (China Provider)
In contrast to the three sites reporting similar triggers, patients and providers in China, the USA, and Taiwan identified different primary methods for coping with urges to use. Patients in the USA reported using prayer and going to an AA/NA meeting or calling a sponsor as key coping tools. Providers in China and Taiwan reported that they encouraged their patients to seek help from social workers and other healthcare providers. Providers in China stated they would text or call their patients, something not mentioned by patients and providers in the other sites. Additional coping methods that were identified across sites included alternative behaviors such as reading, sleeping, and talking with a non-using friend or family member.
“Meetings are good because you know you’re not the only one and you can hear other people’s stories. It’s about not isolating yourself. You have to get out in the community with the right people.” (USA Patient)
“We encourage our clients to talk to doctors during out-patient visits, if they have a bad mood. I said that we are all psychiatrists.” (Taiwan Provider)
Desired Features and Functions of S-Health
Patients and providers across sites were generally positive about the potential utility of a smartphone-based tool. They thought S-Health could provide a distraction from mild cravings or thoughts of using and could be a useful tool for self-monitoring progress and keeping appointments. Patients at all sites felt that individualized feedback was important and were very interested in receiving health information, especially related to MMT, HCV, HIV, and the impact and interaction of various medications with methadone. Patients in the USA were interested in being provided with information regarding AA/NA meeting locations and free mental health services, as well as using S-Health to connect directly to other patients or providers.
“Maybe the App can provide us more information on methadone, such as how it will affect our body if we use it long term. What’s the negative influence on our body? Does it damage our brain?” (Taiwan Patient)
“We are Hepatitis C patients, it can tell us what is better to eat and to do. Family affection (messages) also works. (China Patient)
“It would be good if triggered that the text went to a live therapist who could text back immediately. Then they could see what you needed and give more information.” (USA Patient)
“So many of our clients have such a difficult time for various reasons making appointments and remembering appointments and stuff like that…I didn’t know if there would be any benefit at all in having a treatment-specific scheduling thing, a remindering thing.” (USA Provider)
Complexity: Facilitators and Barriers to Adopting S-Health
Perceptions about the ease of incorporating S-Health into patient lives were influenced by variations in smartphone access and familiarity as well as differences in culture and policy of our three study sites.
Availability and Familiarity of Smartphone
The issue of smartphone familiarity received minimal discussion with patients and providers in the USA. In general, patients seemed to indicate they would be comfortable using S-Health and could do so with ease. Some patients in the USA described already using group texts as a way to connect with others in recovery and motivate one another to stay abstinent.
“There were a bunch of guys that we had come from the jail—anyway, a pretty tight peer group and a few of ‘em had taken to—there’s a bunch of recovery messages like—‘Easy does it.’ Little picture messages, basically and they would circulate a lot of ‘em around. They’d send ‘em to me and I’d send ‘em off to ten people and shoot ‘em off. They would circulate around and it was actually sort of cool. I mean it sounds a little cheesy, but it was a little bit inspiring to get those and say, ‘Oh, such-and-such, he’s still clean.’” (USA Patient)
Conversely, patients and providers in China and Taiwan expressed some concerns about patients’ access to smartphones. Providers in China stated that many patients did not have smartphones, and those that did, tended to be younger with greater financial security. Additionally, providers in both China and Taiwan were concerned about the low education level of patients and felt that patients would only be able to adopt S-Health if given appropriate training. Further, they indicated that survey and message content should be kept simple to account for low reading level.
“When I do health education for my clients, I always use kindergarten ways of teaching to ensure that they can understand.” (Taiwan Provider)
“I want to say that young people may accept this kind of thing (S-Health). Many old guys cannot even use the cellphone. They cannot read or text a message. How can they do this?” (China Patient)
Motivation and Feared Consequences for Adopting S-Health
Patients suggested financial incentives as initial motivation for using the application, but reported that they would be personally motivated to adopt S-Health if they perceived it to be easy, attractive, interesting, and useful. They also noted that they would be more likely to interact with the application if they were not at work or around family members because of limited knowledge regarding issues surrounding privacy and confidentiality.
“When I am with my family, I will not answer honestly or will not answer at all… I am afraid that my family will suspect me, because they love me but they have no confidence.” (Taiwan patient)
“It would be best if there is a reward for us. … It is only an encouragement. I know that you cannot give us a TV, a cellphone, right? But that little gift will motivate me to spend five minutes every day before I go to bed.” (Taiwan patient)
“When I open the App, if I really like it, I will not need a gift.” (Taiwan patient)
Although drug use is illegal and stigmatized in all three countries, patients and providers in the USA expressed far less concern about potential legal ramifications due to using S-Health. Patients in China and Taiwan, however, wanted assurance of privacy and confidentiality. Patients stated they would be willing to use S-Health, but having trust in the researchers was essential. Participants feared data breaches and subsequent arrest due to substance use information shared via the application. Chinese and Taiwanese patients needed to first understand issues of data security before adoption.
“I have to emphasize one problem that I just mentioned. Some patients will be comfortable (with sharing information), but not many. Most patients will feel that they are watched (if their information is shared). They had a nick name for the public security sector (gonganju), ‘laogong (husband).’ If you talk (about sharing information), they will be sensitive about this.” (China provider)
“Many clients often run away from the police, when they are wanted. They will not use their cellphone to avoid being tracked by the police.” (Taiwan provider)
Discussion
This qualitative study of patient and provider perspectives collected data via focus groups conducted in MMT clinics located in China, Taiwan, and the USA in order to determine how three factors contributing to adoption of innovation within the DOI theory (Relative Advantage, Compatibility, Complexity) may be influenced by the socio-cultural differences of the three sites. Rogers’ theory (Rogers 2002) argues that the social systems in which adopters reside greatly influence perceptions regarding the key elements of adoption. As such, we anticipated that social and legal variations across countries would impact patient and provider views about the acceptability and utility of S-Health.
Relative Advantage
Group and individual counseling services, self-help groups, and methadone treatment are the current existing services available to potential S-Health adopters. According to DOI, satisfaction and convenience influence adopters’ perceptions about the relative advantage of an innovation. Given the USA patients’ comfort and satisfaction with current group support and behavioral interventions, adopting S-Health would appear to not be relatively advantageous for these patients. Their enthusiasm for skill acquisition and motivational support from the application, however, appears to indicate that they would be highly likely to accept S-Health as part of their recovery program. In fact, they suggested integration of S-Health within their existing networks and treatment programs, through such functions as connecting them to peers and providing easily accessible information regarding local AA/NA meetings, would make the application more desirable and useful.
Conversely, counseling services and self-help groups are not available in many areas in China and Taiwan; and for the services that do exist, providers oftentimes lack adequate training (Li 2013; Yin et al. 2010). This lack of familiarity with behavioral interventions elicited negative perceptions regarding the utility of therapy among Chinese and Taiwanese patients in the current study. Patients seemed to be ashamed at the prospect of sharing personal information with others in a group format, and were concerned that hearing or talking about the past may trigger cravings. Because S-health would not require face-to-face interactions with a therapist or other group members, it may be more likely accepted as a useful adjunct to MMT than traditional group counseling for patients in these regions.
In addition, Chinese and Taiwanese participants also reported more barriers in accessing MMT, more concerns about the side effects of methadone, and stronger motivation to stop using methadone. Moreover, patients’ desire to quit methadone in China and Taiwan seems to be a risk for relapse at these sites. S-Health can serve as a platform for heroin users to learn more about MMT, combat negative attitudes toward MMT, and self-manage MMT progress. Although both countries increased MMT clinics in recent years (Chen and Kuo 2007; Huang et al. 2011; Sullivan and Wu 2007), patients and providers both report notable difficulties in receiving needed services. Thus, mobile behavioral health interventions may be a natural way to fill this gap in care by providing a portable and non-medicinal recovery tool.
Compatibility
Patients and providers across sites report a large but similar range of reasons for patients’ recovery. Of upmost importance was finding employment and building positive family relationships. Family was considered an important motivator for abstinence in all regions, yet strained relationships were also cited as a primary reason for relapse. In general, interpersonal relationships, including those with therapists and “old friends” along with family members, play a key role in the recovery process. USA patients wanted S-Health to actively connect them to others in recovery or provide information about time and location of local self-help groups. Integration of positive social supports appears to be a necessary part of aligning the function of S-Health with existing values across cultures.
Patients in China and Taiwan voiced their concern specifically about the impact physical cravings have on the potential for relapse. Although the cause of a greater report in physical cravings is beyond the scope of this study, possibly due to regional variations in dosing (Yin et al. 2010) and access to MMT (Wu et al. 2012), this factor could result in a slower adoption of S-Health. While the interactive nature of a smartphone application could help to reduce psychological cravings through self-monitoring and self-regulation, more intense physical cravings may need to be addressed separately (e.g., take-home options, access to methadone during traveling). Cross-culturally, patients and providers reported the need for coping tools during times of high risk, the delivery of relevant knowledge regarding MMT, HIV, HCV, and overall health, and assistance in monitoring personal progress and keeping appointments.
Complexity
While it seems possible to create an application that is in alignment with the values and social norms of each site, adoption may face the greatest barrier in terms of Complexity. Smartphones among USA patients were common, but providers and patients in China and Taiwan voiced concerns regarding accessibility to smartphones and familiarity with applications, particularly for older patients. The development of new skills hinders the likelihood and rate of adoption of an innovation (Rogers 2002). Thus, additional trainings from staff may be required in China and Taiwan for patients to accept and integrate S-Health as a recovery tool.
Visual appeal and perceived usefulness are important factors for motivating patients to adopt and regularly use S-Health, but more importantly, patients must understand how they and the application itself can protect their privacy. Individuals can interface with the application during times of their choosing (i.e., alone rather than around family or at work). Particularly for patients in China and Taiwan, they should be explicitly instructed on how to engage with the application during times when they are not fearful of judgment from family members and the integrity of their responses will not be compromised. Study staff must explain in a clear manner the steps taken to protect their privacy and confidentiality, as well as the limitations of these data-protecting methods. Adequately teaching patients about security is essential for adoption and would assist in diffusion of the application through patients’ assuring one another that S-Health was safe to use.
While incarceration was cited as a common reason for discontinuation of methadone in China and Taiwan, this is also a problem throughout the USA (Deren et al. 2005). On the other hand, many studies have demonstrated that MMT is effective in reducing criminal activities and incarceration. Thus, while a smartphone application can be designed to provide monitoring, information, communication, and support the recovery as suggested by the literature, safeguarding the privacy and confidentiality of use status and other sensitive information should be a high priority.
Limitations
For the current study, DOI theory was applied to the development phase of an innovation rather than an analysis of factors and systems examining why a new idea, behavior, or product has supplanted what is currently in place. The patient sample was limited to MMT clinic patients that were currently receiving services; it cannot describe the acceptability and likelihood of adoption of S-Health among heroin-dependent patients not enrolled in MMT. Interpretation of results is also limited geographically to the regions in which the focus groups were held. In particular, MMT patients in Shanghai are likely to have greater access to resources supportive of recovery relative to other resources limited areas in China. Nevertheless, smartphone applications may not be relevant in those regions with even more limited resources including access to smartphones. Furthermore, for two of the patient groups in China, transcripts for the focus group discussions were not available. Instead, coding for these groups was done with summary notes and therefore cannot provide the detail of transcripts or be coded in the same manner.
Conclusion
In conclusion, social and cultural environment plays a key role in adopting a new technology-based intervention. The success of introducing and effectively implementing S-Health as a supplementary behavioral intervention for heroin users depends on the interplay of several factors. On the one hand, S-Health can fill a major gap in behavioral treatment for drug users and provide services in a way that is individualized, interactive, and interesting. On the other hand, certain cultural and social barriers, such as smartphone accessibility and acceptability, stigma toward drug use and HIV, and potential for criminal justice threat, may prevent S-Health from being successfully received and used cross-culturally. As illustrated in Fig. 1, a patient-centered clinical application of S-Health can be enhanced to support the self-monitoring and self-management practices by involving treatment providers, community resources, and social supports, grounded within the specific local culture.
Future research endeavors need to focus on 1) developing a smartphone application that successfully addresses these potential barriers; 2) exploring similar topics in other localities in the USA, China, Taiwan, as well as other countries; and 3) incorporating functions and materials identified and desired by the the target population to effectively assist heroin users in recovery.
Acknowledgments
Funding This study was funded by the National Institute on Drug Abuse (P30DA016383, R21DA033285, & R13 DA035084; PI:Hser).
Footnotes
Conflict of Interest All authors declare no conflict of interest.
Compliance with Ethical Standards
Ethical approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent Informed consent was obtained from all individual participants included in the study.
References
- Chak E, Talal AH, Sherman KE, Schiff ER, Saab S. Hepatitis C virus infection in USA: An estimate of true prevalence. Liver Int. 2011;31(8):1090–1101. doi: 10.1111/j.1478-3231.2011.02494.x. [DOI] [PubMed] [Google Scholar]
- Charmaz K. The power and potential of grounded theory. Medical Sociology Online. 2012;6(3):2–15. [Google Scholar]
- Charmaz K. Constructing grounded theory. Sage; 2014. [Google Scholar]
- Chen, Kuo HIV-1 in Taiwan. Lancet. 2007;369:623–625. doi: 10.1016/S0140-6736(07)60291-8. [DOI] [PubMed] [Google Scholar]
- Chen AYM, Lan YC, Lai SF, Yang JY, Tsai SF, Kuo SHS. HIV-1 CRF07_BC infections, injecting drug users, Taiwan. Emerg Infect Dis. 2006;12(4):703–705. doi: 10.3201/eid1204.050762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chih MY, Patton T, McTavish FM, Isham AJ, Judkins-Fisher CL, Atwood AK, DHG Predictive modeling of addiction lapses in a mobile health application. J Subst Abus Treat. 2014;46(1):29–35. doi: 10.1016/j.jsat.2013.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou YC, Shih SF, Tsai WD, Li CS, Xu K, Lee TS. Improvement of quality of life in methadone treatment patients in northern Taiwan: a follow-up study. BMC Psychiatry. 2013;13:190. doi: 10.1186/1471-244X-13-190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Aunno T, Pollack HA, Frimpong JA, Wuchiett D. Evidence-based treatment for opiod disorders: a 23-year national study of methadone dose levels. J Subst Abus Treat. 2014;47(4):245–250. doi: 10.1016/j.jsat.2014.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L, Charlson F, Mathers B, Hall WD, Flaxman AD, Johns N, Vos T. The global epidemiology and burden of opioid dependence: Results from the global burden of disease 2010 study. Addiction. 2014;109(8):1320–1333. doi: 10.1111/add.12551. [DOI] [PubMed] [Google Scholar]
- Deren S, Goldstein MF, Des Jarlais DC, Richman BL, Kang S, Flom PL. Drug use, HIV-related risk behaviors and dropout status of new admissions and re-admissions to methadone treatment. J Subst Abuse Treat 2001 Mar. 2005;20(2):185–189. doi: 10.1016/s0740-5472(00)00153-7. [DOI] [PubMed] [Google Scholar]
- Des Jarlais DC, Semaan S. HIV prevention for injecting drug users: the first 25 years and counting. Psychosom Med. 2008;70(5):606–611. doi: 10.1097/PSY.0b013e3181772157. [DOI] [PubMed] [Google Scholar]
- Dole VP, Nyswander M. A medical treatment for diacetylmorphine (heroin) addiction. A clinical trial with methadone hydrochloride. J Am Med Assoc. 1965;193:646–650. doi: 10.1001/jama.1965.03090080008002. [DOI] [PubMed] [Google Scholar]
- Duan S, Han J, Tang RH, Yang YC, Xiang LF, Ye RH, Yang SS, Yang YB, Long YC, Li GQ, Yin MS, Pang L, Rou KM, Wu ZY, He N. Study on the incidence and risk factors of HCV infection among heroin addicts who were on methadone maintenance treatment in Dehong prefecture, Yunnan province. Zhonghua Liu Xing Bing Xue Za Zhi. 2013;34(6):552–556. [PubMed] [Google Scholar]
- Dutra L, Stathopoulou G, Basden SL, et al. A meta-analytic review of psychosocial interventions for substance use disorders. Am J Psychiatry. 2008;165(2):179–187. doi: 10.1176/appi.ajp.2007.06111851. [DOI] [PubMed] [Google Scholar]
- eMarketer. 2 Billion consumers Worldwide to get Smart(Phones) by 2016. 2014 http://www.emarketer.com/Article/2-Billion-Consumers-Worldwide-Smartphones-by-2016/1011694#sthash.DZVjChdO.dpuf http://www.emarketer.com/Article/2-Billion-Consumers-Worldwide-Smartphones-by-2016/1011694.
- Fjeldsoe BS, Marshall AL, Miller YD. Behavior change interventions delivered by mobile telephone short-message service. Am J Prev Med. 2009;36(2):165–173. doi: 10.1016/j.amepre.2008.09.040. [DOI] [PubMed] [Google Scholar]
- Gao P, Pan S. Permanent mechanism for community-based drug addiction treatment. Journal of Shanxi Normal University (Social Science Edition) 2014;41(3):59–64. [Google Scholar]
- Gibbons MC, Fleisher L, Slamon RE, Bass S, Kandadai V, Beck JR. Exploring the potential of Web 2.0 to address health disparities. J Health Commun. 2011;16(Suppl 1):77–89. doi: 10.1080/10810730.2011.596916. [DOI] [PubMed] [Google Scholar]
- Gustafson DH, McTavish FM, Chih MY, et al. A Smartphone Application to Support Recovery From Alcoholism. JAMA Psych. 2014;71(5):566–572. doi: 10.1001/jamapsychiatry.2013.4642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heron KE, Smyth JM. Ecological momentary interventions: Incorporating mobile technology into psychosocial and health behavior treatments. Brit J H Psych. 2010;15(1):1–39. doi: 10.1348/135910709X466063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hser YI, Evans E, Grella C, Ling W, Anglin D. Long-term course of opioid addiction. Harv Rev Psychiatry. 2015;23(2):76–89. doi: 10.1097/HRP.0000000000000052. [DOI] [PubMed] [Google Scholar]
- Huang YF, Kuo HS, Lew-Ting CY, Tian F, Yang CH, Tsai TI, Gange SJ, Nelson KE. Mortality among a corhort of drug users after their release from prison: an evaluation of the effectiveness of a harm reduction program in Taiwan. Addiction. 2011;106(8):1437–1445. doi: 10.1111/j.1360-0443.2011.03443.x. [DOI] [PubMed] [Google Scholar]
- Ingersoll KS, Dillingham RA, Hettema JE, Conaway M, Freeman J, Reynolds G, Hosseinbor S. Pilot RCT of bidirectional text messaging for ART adherence among nonurban substance users with HIV. Health Psychol. 2015;34(Suppl):1305–1315. doi: 10.1037/hea0000295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson K, Isham A, Shah DV, Gustafson DH. Potential roles for new communication technologies in treatment of addiction. Curr Psychiatry Rep. 2011;13(5):390–397. doi: 10.1007/s11920-011-0218-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF. Self-help for substance abuse disorders: History, effectiveness, knowledge gaps and research opportunities. Clin Psychol Rev. 2003;23:639–663. doi: 10.1016/s0272-7358(03)00053-9. [DOI] [PubMed] [Google Scholar]
- Kleber HD. Methadone maintenance 4 decades later: thousands of lives saved but still controversial. J Am Med Assoc. 2008;300(19):2303–2305. doi: 10.1001/jama.2008.648. [DOI] [PubMed] [Google Scholar]
- Klevens RM, Hu DJ, Jiles R, Holmberg SD. Evolving epidemiology of hepatitis C virus in the United States. Clin Infect Dis. 2012;55:S3–S9. doi: 10.1093/cid/cis393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lan YC, Elbeik T, Dileanis J, Ng V, Chen YJ, Leu HS, Cheng SH, Wong JC, Wong WW, Chen YM. Molecular epidemiology of HIV-1 subtypes and drug resistant strains in Taiwan. J Med Virol. 2008;80:183–191. doi: 10.1002/jmv.21065. [DOI] [PubMed] [Google Scholar]
- Lee TS, Shen HC, Wu WH, Huang CW, Yen MY, Wang BE, Chuang P, Shih CY, Chou YC, Liu YL. Clinical characteristics and risk behavior as a function of HIV status among heroin users enrolled in methadone treatment in northern Taiwan. Subst Abuse Treat Prev Policy. 2011;6:6. doi: 10.1186/1747-597X-6-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewden C, Salmon D, Morlat P, Bevilacqua S, Jougla E, Bonnet F, Heripret L, Costagliola D, May T, Chene G. Causes of death among human immunodeficiency virus (HIV)-infected adults in the era of potent antiretroviral therapy: emerging role of hepatitis and cancers, persistent role of AIDS. Int J Epidemiol. 2005;34:121–130. doi: 10.1093/ije/dyh307. [DOI] [PubMed] [Google Scholar]
- Li ES. The new drug detoxification system in China: a misused tool for drug rehabilitation. E Asia L Rev. 2013;9:168–212. [Google Scholar]
- Lyu SY, Su LW, Chen YM. Effects of education on harm-reduction programmes. Lancet. 2012;379(9814):e28–e30. doi: 10.1016/S0140-6736(11)60786-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magiorkinis G, Sypsa V, Magiorkinis E, Paraskevis D, Katsoulidou A, Belshaw R, Fraser C, Pybus OG, Hatzakis A. Integrating phylodynamics and epidemiology to estimate transmission diversity in viral epidemics. PLoS Comput Biol. 2013;9(1):e1002876. doi: 10.1371/journal.pcbi.1002876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsch LA. Leveraging technology to enhance addiction treatment and recovery. J Addict Dis. 2012;31(3):313–318. doi: 10.1080/10550887.2012.694606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattick RP, Breen C, Kimber J, Davoli M. Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database Syst Rev. 2009;3:CD002209. doi: 10.1002/14651858.CD002209. [DOI] [PubMed] [Google Scholar]
- McCann MJ, Rawson RA, Obert JL, Hasson A. Treatment of opiate addiction using methadone: a counselor manual. Center for Substance Abuse Treatment; Rockville: 1994. [Google Scholar]
- McHugh RK, Hearon BA, Otto MW. Cognitive-behavioral therapy for substance use disorders. Psychiat Clin North Am. 2010;33(3):511–525. doi: 10.1016/j.psc.2010.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: preparing people to change addictive behavior. J Community Appl Soc Psychol. 1991;2:299–300. [Google Scholar]
- Moore BA, Fazzino T, Garnet B, Cutter CJ, Barry DT. Computer-based interventions for drug use disorders: a systematic review. J Subst Abus Treat. 2011;40(3):215–223. doi: 10.1016/j.jsat.2010.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narcotics Control Bureau of the Ministry of Public Security P. R. China. [Accessed 10 Sept 2015];Annual report on drug control in China. 2014 http://www.bjjdzx.org/157/2014-07-15/60020.htm http://www.bjjdzx.org/157/2014-07-15/60020.htm.
- National Institute on Drug Abuse. [Accessed 13 Sept 2015];Drug facts: Heroin. 2014 http://www.drugabuse.gov/publications/drugfacts/heroin.
- Nelson PK, Mathers BM, Cowie B, Hagan H, Des Jarlais D, Horyniak D, Degenhardt L. Global epidemiology of hepatitis B and hepatitis C in people who inject drugs: results of systematic reviews. Lancet. 2011;378(9791):571–583. doi: 10.1016/S0140-6736(11)61097-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng MH, Chou JY, Chang TJ, Lee PC, Shao WC, Lin TY, Chen VC, Gossop M. High prevalence but low awareness of hepatitis C virus infection among heroin users who received methadone maintenance therapy in Taiwan. Addict Behav. 2013;38(4):2089–2093. doi: 10.1016/j.addbeh.2013.01.010. [DOI] [PubMed] [Google Scholar]
- Noar SM, Willoughby JF. eHealth interventions for HIV prevention. AIDS Care. 2012;24(8):945–952. doi: 10.1080/09540121.2012.668167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolan S, Dias Lima V, Fairbairn N, Kerr T, Montaner J, Grebely J, Wood E. The impact of methadone maintenance therapy on hepatitis C incidence among illicit drug users. Addiction. 2014;109(12):2053–2059. doi: 10.1111/add.12682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsen Y, Sharfstein JM. Confronting the Stigma of Opioid Use Disorder—and Its Treatment. J Am Med Assoc. 2014;311(14):1393–1394. doi: 10.1001/jama.2014.2147. [DOI] [PubMed] [Google Scholar]
- Quaglio G, Lugoboni F, Pajusco B, Sarti M, Talamini G, Lechi A, Mezzelani P, Des Jarlais DC. Factors associated with hepatitis C virus infection in injection and noninjection drug users in Italy. Clin Infect Dis. 2003;37(1):33–40. doi: 10.1086/375566. [DOI] [PubMed] [Google Scholar]
- Reback CJ, Grant DL, Fletcher JB, Branson BM, Shoptaw S, Rhode Bowers J, Charania M, Mansergh G. Text messaging reduces HIV risk behaviors among methamphetamine-using men who have sex with men. Aids and Beh. 2012;16(7):1993–2002. doi: 10.1007/s10461-012-0200-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers EM. Diffusion of preventive innovations. Addict Behav. 2002;27(6):989–993. doi: 10.1016/s0306-4603(02)00300-3. [DOI] [PubMed] [Google Scholar]
- Rosen HR. Clinical practice. Chronic hepatitis C infection. N Engl J Med. 2011;364(25):2429–2438. doi: 10.1056/NEJMcp1006613. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. [Accessed 10 Dec 2015];National Survey of Substance Abuse Treatment Services Report: Trends in the Use of Methadone and Buprenorphine at Substance Abuse Treatment Facilities: 2003 to 2011. 2013 http://www.samhsa.gov/data/sites/default/files/N-SSATS%20Rprt%20Trnds%20Use%20Methadone%20&%20Buprenorphine%20at%20SA%20Trmt%20Facs%20%2003-11/N-SSATS%20Rprt%20Trnds%20Use%20Methadone%20&%20Buprenorphine%20at%20SA%20Trmt%20Facs%20%2003-11/sr107-NSSATS-Buprenorph.htm. [PubMed]
- Substance Abuse and Mental Health Services Administration. [Accessed 10 Dec 2015s];Behavioral Health Treatment Services Locator. 2015 https://findtreatment.samhsa.gov/
- Sullivan SG, Wu Z. Rapid scale up of harm reduction in China. Int J Drug Policy. 2007;18(2):118–128. doi: 10.1016/j.drugpo.2006.11.014. [DOI] [PubMed] [Google Scholar]
- Taiwan Ministry of Health and Welfare. [Accessed 13 Dec 2015];2014 Anti-drug report. 2015 http://www.moj.gov.tw/public/Attachment/410291426435.pdf.
- United Nations Office on Drug and Crime. World Drug Refport. Vienna: UNODC; 2013. [Google Scholar]
- Vigilant LG. The stigma paradox in methadone maintenance: Naïve and positive consequences of a “treatment punishment” approach to opiate addiction. Humanit Soc. 2004;28(4):403–418. [Google Scholar]
- Weber R, Sabin CA, Friis-Moller N, Reiss P, El-Sadr WM, Kirk O, Dabis F, Law MG, Pradier C, De Wit S, et al. Liver-related deaths in persons infected with the human immunodeficiency virus: the D:A: D study. Arch Intern Med. 2006;166:1632–1641. doi: 10.1001/archinte.166.15.1632. [DOI] [PubMed] [Google Scholar]
- White W. Long-term strategies to reduce the stigma attached to addiction, treatment, and recovery within the City of Philadelphia (with particular reference to medication-assisted treatment/recovery) Philadelphia, PA: Department of Behavioral Health and Intellectual Disability Services; 2009. [15 September 2015]. http://dbhids.org/technical-papers-on-recoverytransformation/ [Google Scholar]
- White WL. Narcotics Anonymous and the pharmacotherapeutic treatment of opioid addiction. Great Lakes Addiction Technology Transfer Center and Philadelphia Department of Behavioral Health and Intellectual Disability Services; Chicago: 2011. [Google Scholar]
- World Health Organization. Reducing harm, preventing HIV, saving lives: China’s vast methadone maintenance treatment program marks successes even as it addresses key challenges ahead. [September 2015];2014 http://www.wpro.who.int/china/mediacentre/releases/2014/2014112702/en/.13.
- World Health Organization. [14 September 2015];Injecting drug use: HIV/AIDS. 2015 http://www.who.int/hiv/topics/idu/about/en/
- Wu F, Peng CY, Jiang H, Zhang R, Zhao M, Li J, Hser YI. Methadone maintenance treatment in China: perceived challenges from the perspectives of service providers and patients. J Public Health. 2012;35(2):206–212. doi: 10.1093/pubmed/fds079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin W, Hao Y, Sun X, Gong X, Li F, Li J, Wu Z. Scaling up the national methadone maintenance treatment program in China: achievements and challenges. Int J Epidemiol. 2010;39(Suppl 2):ii29–ii37. doi: 10.1093/ije/dyq210. [DOI] [PMC free article] [PubMed] [Google Scholar]