Key Clinical Message
Adenoid cystic carcinoma (ACC) is a rare malignant tumor of the salivary glands, with higher frequency in the submandibular gland, a prolonged clinical course, and poor long‐term survival. It tends to metastasize to lungs, bone, liver, brain, and rarely to skin. Comprehensive skin examination and appropriate follow‐up is recommended, since cutaneous metastasis represents disease progression, requiring management and prognosis adjustment.
Keywords: Adenoid cystic carcinoma, cutaneous metastases
Introduction
Adenoid cystic carcinoma (ACC) is a rare malignant tumor of the salivary glands, with higher frequency in the submandibular gland, a prolonged clinical course, and poor long‐term survival. Adenoid cystic carcinoma tends to metastasize to lungs, bone, liver, and brain. Cutaneous metastases are rare and usually represent an advanced stage of disseminated disease.
Case Description
A 52‐year‐old man underwent excision of a 2.5 cm right submandibular gland mass in 2003. Specimen revealed ACC (Fig. 1) with extensive perineural invasion (Fig. 2), involving the periglandular fat and the resection margins. The patient received postoperative radiotherapy. Nine years later, the patient complained of severe headaches and ear pain. Image studies showed recurrent deeply infiltrative tumor, occupying the masticator and submandibular spaces, extending superiorly to the C1 arch. Bone erosion involving the posterior mandibular cortex was seen, compatible with tumor invasion. A right submandibular area fine needle aspiration confirmed the diagnosis of recurrent ACC. The patient had right partial segmental mandibulectomy, infratemporal fossa dissection, parotidectomy, and carotid arterial system dissection. An 8‐cm well‐defined, rubbery white‐tan mass was identified, surrounding the posterior/inferior aspect of the mandible, extending into the adjacent parotid gland, masseter muscle and margins, but not into the adjacent skin or bone. Microscopic examination showed a moderately differentiated predominantly cribriform pattern ACC with perineural invasion, encasing the carotid artery and invading the parotid gland. No lymphovascular invasion was identified and none of the 36 examined lymph nodes was involved. The patient received five sessions of stereotactic radiotherapy and had a free flap reconstruction with a PEG tube.
Figure 1.
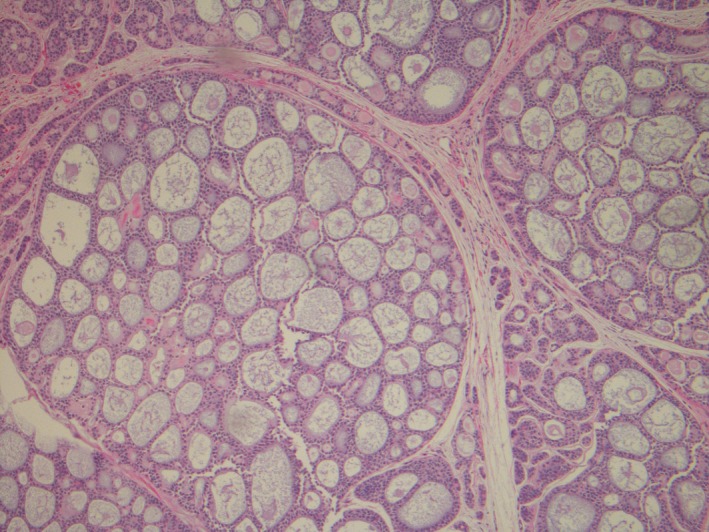
Histopathology of the right submandibular gland mass, showing nodular proliferation of uniform basaloid cells in a cribriform pattern, consistent with adenoid cystic carcinoma.
Figure 2.
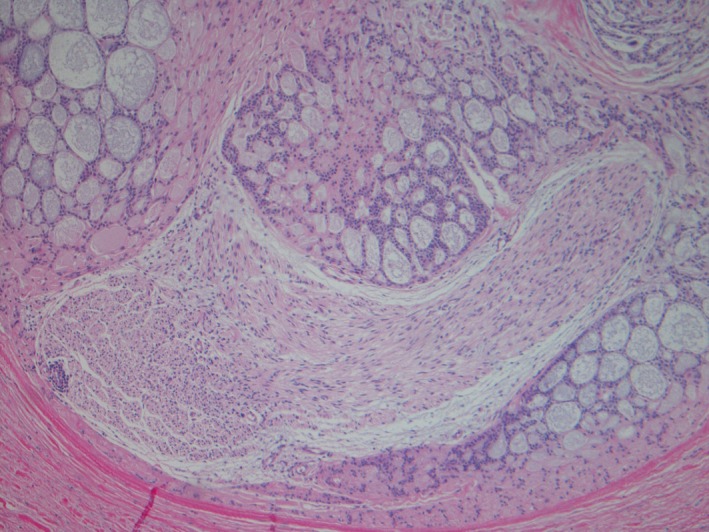
Histopathology of adenoid cystic carcinoma showing perineural invasion.
In 2013, 10 years after the original diagnosis, a PET‐CT scan showed a new hypermetabolic 3.4‐cm lung mass, multiple bilateral pulmonary nodules, and indeterminate hypermetabolism in the left lateral tongue and base of the tongue. Subsequently, the patient received chemotherapy for 1 year: Cisplatin/5Fluorouracil/Erbitux for 3 months followed by Taxotere for 9 months. The disease was stable for 6 months. A small increase of the lung nodules prompted Sunitinib administration, but the patient developed an allergic reaction and the treatment was discontinued. In November 2015, 12 years after the initial submandibular gland ACC diagnosis, the patient presented with new painful poorly circumscribed lesions on his right toes (Fig. 3). Skin biopsy (Figs. 4 and 5) confirmed ACC metastasis and the tumor was sent for genetic analysis. The patient was started on radiotherapy with an initial good response; however, the disease recurred and continues to progress with additional nodules on his right toes and shin (Fig. 6).
Figure 3.

Right toes nodules, 12 years after the original ACC diagnosis.
Figure 4.
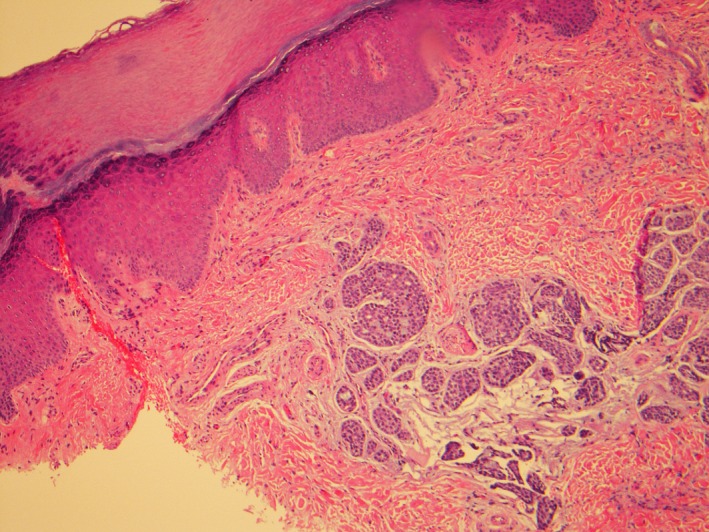
Histopathology of the skin biopsy, showing infiltrating nodular proliferation of uniform basaloid cells in a cribriform pattern, similar to the primary ACC (low power).
Figure 5.
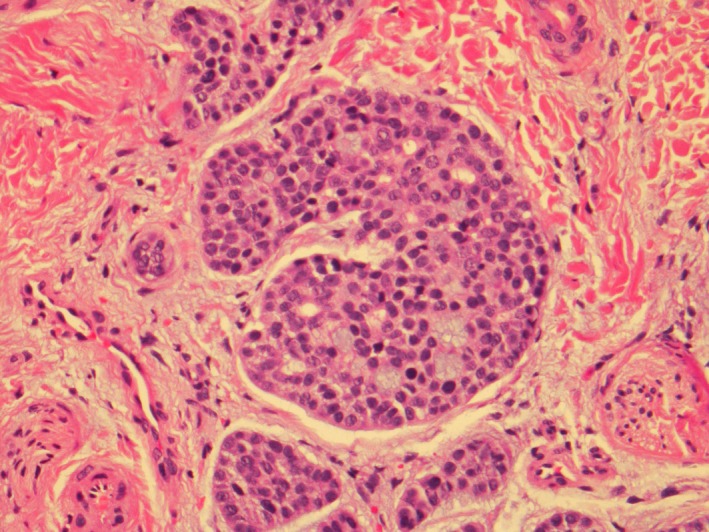
Histopathology of the skin biopsy, showing infiltrating nodular proliferation of uniform basaloid cells in a cribriform pattern, similar to the primary ACC (high power).
Figure 6.

Poorly circumscribed right toes nodules, 13 years after the original ACC diagnosis.
Discussion
Ten to fifteen percent of salivary gland neoplasms are malignant 1. ACC occurs with a higher frequency in the submandibular gland and is a rare malignancy, with a protracted clinical course and poor survival. Patients are 54 years old on average, when first diagnosed with salivary gland ACC 2. There are three ACC morphologic patterns, often mixed: tubular, cribriform, and solid, with the last one having a more aggressive clinical course.
Skin metastases of ACC are extremely rare; ACCs were previously reported as metastatic to skin, presenting as nodules on the neck, abdomen, shoulder, elbow, mental region, plantar surface, and digit nodules 3. To the best of our knowledge, there is only one case of metastatic ACC of the submandibular gland to toes previously described in the literature; the patient in that case expired 10 months after the reported toe metastasis and 7 years after the initial diagnosis, with extensive metastatic disease 4.
Since morphology and immunohistochemistry cannot differentiate between a primary cutaneous ACC and a metastasis to skin, prior history is vital to reach the correct diagnosis 5.
Adenoid cystic carcinoma commonly metastasizes to the lung, bone, and viscera, even with adequate locoregional control 6. Metastases to skin represent disease progression 7 and can determine prognosis and further management. Direct extension from adjacent structures (especially in cutaneous lesions overlying salivary glands, perioral or periorbital areas) and iatrogenic dissemination from prior surgical approach should be excluded as well 8.
Prior studies showed that about 37 months, on average, passed between the primary diagnosis and the metastatic ACC and approximately 21 months passed between other than the lungs metastases and death 2. Additionally, it was reported that 11% of patients die within 1 year and one‐third die within 3 years from the metastases diagnosis 9. Our patient is alive 3 years since detection of lung ACC metastasis and 6 months after the cutaneous metastatic disease detection.
Treatment of disseminated ACC is challenging; there is currently no consensus about the optimal therapeutic approach. There is debate even on the role of surgery, since it might not necessarily increase survival 6. Often ACC is unresponsive to chemotherapy; however, palliative chemotherapy might be used in symptomatic patients, with various responses, which might not necessarily be attributed to chemotherapy itself but rather to the indolent clinical evolution of ACC 6.
Although no improvement in survival is reported, the use of adjuvant radiotherapy appears to improve locoregional control and disease‐free survival 1, 10. Despite receiving adjuvant radiotherapy, our patient showed disease progression.
Other treatment approaches of distant metastasis were attempted, such as chemoembolization and radiofrequency ablation, with insufficient data to support any of them 11.
There are no known targetable genetic alterations in ACC. KIT, a transmembrane receptor tyrosine kinase, is over‐expressed in ACC and can be detected immunohistochemically. In some patients with unresectable metastatic ACCs that overexpress CD117 treatment with imatinib mesylate, a tyrosine kinase inhibitor targeting KIT, was attempted; however, responses have been disappointing 12. When there are only isolated metastases, surgery can be attempted for disease control, but the usefulness of metastatectomy for the overall survival is controversial 1, 5, 6.
Studies have demonstrated that most cases of ACC harbor a t(6;9) chromosomal translocation, involving the gene encoding the transcription factor MYB 13, 14, 15. More recently, MYBL1–NFIB gene fusions, MYBL1 gene rearrangements, and MYBL1 overexpression were reported in ACCs without t(6;9) translocations, as well as 5′‐NFIB gene fusions in a subset of MYB‐NFIB‐negative ACCs with t(6;9) translocations 16.
Various trials of targeted therapy have not yet yielded an adequate response with any agents; therefore, a standardized therapeutic approach with adequate results for advanced ACC is not available at present.
Tumor tissue from our patient was sent for genetic analysis. Three main genomic alterations were identified: BCOR, EP300, and TERT; however, there are currently no FDA‐approved therapies and no potential clinical trials specific to the reported genomic alterations. Although TERT promoter mutations have not been described in the context of ACC, a variety of therapeutic approaches for targeting tumors with TERT mutations are under development, including immunotherapies utilizing TERT as a tumor‐associated antigen, antisense oligonucleotide‐ or peptide‐based therapies, and TERT promoter‐directed cytotoxic molecules.
Adenoid cystic carcinoma is neurotropic, has a protracted course and spreads relentlessly to adjacent and distant structures via hematogenous and lymphatic routes 1. It carries a high mortality rate and most patients die 5–10 years after the initial treatment. Our patient is still alive after 13 years, with extensive metastatic disease.
Skin metastases in ACC are very rare. A recent study suggested that an integrin signature of tumor secreted exosomes may determine the pattern of distant metastasis 17.
This case underscores the importance of performing a comprehensive skin examination in patients with ACC history. Appropriate judicious follow‐up is recommended in ACC and skin metastasis should be considered when cutaneous nodules appear, since this might represent a crucial step in disease progression, requiring management and prognosis adjustment.
Conflict of Interest
None declared.
References
- 1. Harish, K. , and Gouri S. R. M.. Adenoid cystic carcinoma of the parotid metastasizing to liver: case report. Available at http://bmccancer.biomedcentral.com/articles/10.1186/1471-2407-4-41 (Accessed: January, 2016). [DOI] [PMC free article] [PubMed]
- 2. VanderWal, J. E. , Becking A. G., Snow G. B., and VanderWaal I.. 2002. Distant metastases of adenoid cystic carcinoma of the salivary glands and the value of diagnostic examinations during followup. Head Neck 24:779–783. [DOI] [PubMed] [Google Scholar]
- 3. Saco, M. , Howe N., Jukic D. M., and Muro‐Cacho C.. Adenoid cystic carcinoma of the base of the tongue metastasizing to the scalp. Dermatol. Online J. 20:6 Available at http://escholarship.org/uc/item/6141j293 (Accessed: January, 2016). [PubMed] [Google Scholar]
- 4. Weitzner, S. 1975. Adenoid cystic carcinoma of submaxillary gland metastatic to great toe. Am. Surg. 41:655–658. [PubMed] [Google Scholar]
- 5. Da Cruz Perez, D. E. , Magrin J., Paes de Almeida O., and Kowalski L. P.. 2007. Multiple cutaneous metastases from a parotid adenoid cystic carcinoma. Pathol. Oncol. Res. 13:167–169. [DOI] [PubMed] [Google Scholar]
- 6. Coupland, A. , Sewpaul A., Darne A., and White S.. 2014. Adenoid cystic carcinoma of the submandibular gland, locoregional recurrence, and a solitary liver metastasis more than 30 years since primary diagnosis . Article ID 581823. Available at http://www.hindawi.com/journals/cris/2014/581823/ (Accessed: January, 2016). [DOI] [PMC free article] [PubMed]
- 7. Gualdi, G. , Monari P., Calzavara‐Pinton P., Farisoglio C., Ginani A., and Catrani S.. 2014. Early cutaneous metastasis of adenoid cystic carcinoma of the salivary gland. Cutis 93:E16–E18. [PubMed] [Google Scholar]
- 8. Jedrych, J. , and Galan A.. 2013. Multiple cutaneous metastases: a rare and late sequelae of lacrimal gland adenoid cystic carcinoma. J. Cutan. Pathol. 40:341–345. [DOI] [PubMed] [Google Scholar]
- 9. Sung, M. W. , Kim K. H., Kim J. W., Min Y. G., Seong W.J., Roh J. L., et al. 2003. Clinicopathologic predictors and impact of distant metastasis from adenoid cystic carcinoma of the head and neck. Arch. Otolaryngol. Head Neck Surg. 129:1193–1197. [DOI] [PubMed] [Google Scholar]
- 10. Nascimento, A. G. , Amaral A. L. P., Prado L. A. F., Kligerman J., and Silveira T. R. P.. 1986. Adenoid cystic carcinoma of salivary glands: a study of 61 cases with clinicopathologic correlation. Cancer 57:312–319. [DOI] [PubMed] [Google Scholar]
- 11. Karatzas, A. , Katsanos K., Maroulis I., Kalogeropoulou C., Tzorakoleftherakis E., and Karnabatidis D.. 2011. Multi‐modality curative treatment of salivary gland cancer livermetastases with drug‐eluting bead chemoembolization, radiofrequency ablation, and surgical resection: a case report. J. Med. Case Rep. 5:416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dillon, P. M. , Chakraborty S., Moskaluk C. A., Joshi P. J., and Thomas C. Y.. 2015. Adenoid cystic carcinoma: a review of recent advances, molecular targets, and clinical trials. Head Neck . Wiley Online Library (wileyonlinelibrary.com). DOI 10.1002/hed.23925 (Accessed: April, 2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Di Palma, S. , Fehr A., Danford M., Smith C., and Stenman G.. 2014. Primary sinonasal adenoid cystic carcinoma presenting with skin metastases – genomic profile and expression of the MYB–NFIB fusion biomarker. Histopathology 64:453–455. [DOI] [PubMed] [Google Scholar]
- 14. Nordkvist, A. , Mark J., Gustafsson H., Bang G., and Stenman G.. 1994. Non‐random chromosome rearrangements in adenoid cystic carcinoma of the salivary glands. Genes Chromosomes Cancer 10:115–121. [DOI] [PubMed] [Google Scholar]
- 15. Hudson, J. B. , and Collins B. T.. 2014. MYB Gene abnormalities t(6;9) in adenoid cystic carcinoma fine‐needle aspiration biopsy using fluorescence in situ hybridization. Arch. Pathol. Lab. Med. 138:403–409. [DOI] [PubMed] [Google Scholar]
- 16. Mitani, Y. , Liu B., Rao P. H., Borra V. J., Zafereo M., Weber R. S., et al. 2015. Novel MYBL1 gene rearrangements with recurrent MYBL1–NFIB fusions in salivary adenoid cystic carcinomas lacking t(6;9) translocations. Clin. Cancer Res. 22:725–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hoshino, A. , Costa‐Silva B., Shen T.‐L., Rodrigues G., Hashimoto A., Mark M. T., et al. 2015. Tumour exosome integrins determine organotropic metastasis. Nature 19:329–335. [DOI] [PMC free article] [PubMed] [Google Scholar]


