Abstract
The West Africa Ebola virus (EBOV) outbreak has highlighted the need for effective disinfectants capable of reducing viral load in a range of sample types, equipment and settings. Although chlorine-based products are widely used, they can also be damaging to equipment or apparatus that needs continuous use such as aircraft use for transportation of infected people. Two aircraft cleaning solutions were assessed alongside two common laboratory disinfectants in a contact kill assay with EBOV on two aircraft relevant materials representative of a porous and non-porous surface. A decimal log reduction of viral titre of 4 is required for a disinfectant to be deemed effective and two of the disinfectants fulfilled this criteria under the conditions tested. One product, Ardrox 6092, was found to perform similarly to sodium hypochlorite, but as it does not have the corrosive properties of sodium hypochlorite, it could be an alternative disinfectant solution to be used for decontamination of EBOV on sensitive apparatus.
Keywords: Ebola virus, disinfection, decontamination, inactivation, sodium hypochlorite, safety
1. Introduction
The worst outbreak of Ebola virus disease (EVD) started in Guinea, West Africa [1] in December 2013, and over two years later sporadic cases were still occurring. The outbreak spread to multiple countries with Guinea, Sierra Leone and Liberia being particularly affected. As of January, over 28,600 cases and more than 11,300 deaths have been reported by the World Health Organization (WHO) [2]. In addition to cases in West Africa, infected personnel have been evacuated out of Africa, and facilities in Europe and the United States have treated Ebola virus (EBOV)-infected patients. An unprecedented international response led to volunteers from all over the world travelling to West Africa to work in laboratories, hospitals, treatment centres, holding centres or in the local communities to provide diagnostics, treatment and care and advice to try and halt the spread of the disease. Often working in temporary or adapted buildings with re-purposed equipment, personnel were reliant on personal protective equipment and disinfection for effective infection control.
EBOV, along with the other filoviruses, is a lipid enveloped virus, often considered fragile, that can be inactivated by the use of both physical and chemical methods [3]. Until recently there was limited data on efficacy of disinfectants against EBOV. The Center for Disease Control (CDC), advises “Suitable disinfectant solutions include 0.5% sodium hypochlorite (10% aqueous solution of household bleach), as well as fresh, correctly prepared solutions of glutaraldehyde (2% or as recommended by the manufacturer) and phenolic disinfectants (0.5%–3%)” [4]. The use of sodium hypochlorite solutions is widely advised in further CDC guidance on managing suspected viral hemorrhagic fever [5] and by the WHO in their guidelines on laboratory diagnosis of EVD [6]. Many chlorine-based products, however, are corrosive and may damage fragile equipment or apparatus that needs to be re-used [7]. Chlorine-based products may compromise performance on vehicles used for transport of infected patients, including military aircraft, which were used for evacuation of infected personnel to Europe and the United States. Therefore, alternative disinfectants that are effective against EBOV need to be identified and tested.
Two commonly used military detergents (Calla 1452 and Ardrox 6092) were assessed in a contact kill assay for efficacy against a single EBOV strain in comparison with sodium hypochlorite, and the commercially available disinfectant Desintex. Efficacy was tested on two representative military-relevant surfaces: painted aluminium as a hard, non-porous material, and pilot seat-belt strapping material as a soft porous material. British standard requirements for virucidal activity state a product should “demonstrate at least a decimal log reduction of 4 in virus titre” when tested in accordance with various parameters [8].
2. Materials and Methods
2.1. Test Materials
Tissue culture media (TCM) used throughout was Dulbecco’s minimum essential media supplemented with 2% foetal calf serum, 1% l-glutamine and 1% penicillin/streptomycin (all Sigma, Gillingham, Dorset, UK). The fifty percent tissue culture infectious dose (TCID50) amount was calculated using the method of Reed and Muench [9].
EBOV H.sapiens-tc/COD/1976/Yambuku-Ecran, hereafter referred to as EBOV-Ecran was used in all studies. This virus, previously known as EBOV “E718” was supplied by Public Health England [10]. Passage 5 material was used to infect Vero C1008 cells (ECACC Cat. No. 85020206) maintained in TCM. Virus was harvested on day 5 post-inoculation and titrated to produce a working stock at 1 × 107 TCID50/mL. EBOV-Ecran was titrated in 96-well plates using the endpoint TCID50 assay as previously described [11], although modified with removal of the staining and fixing steps so that all plates were scored for cytopathic effects upon microscopic examination on day 7.
Four disinfectants were assessed for efficacy against EBOV-Ecran (Table 1). Calla 1452 (Zip-chem products, Morgan Hill, CA, USA) was prepared by dilution in tap water (1:32) to give an approximate starting concentration of 3%, as recommended by Air Movements Navy Command Headquarters. Desintex (Laboratoires Rochex, Ville La Grand, France) was prepared by dilution in tap water to a starting concentration of 5% v/v. Ardrox 6092 (Chemetall Plc, Bletchley, Milton Keynes, UK Defence Standard 79-17/2) required no preparation as this was used as a neat solution, and sodium hypochlorite (SyChem, UK) was prepared by dilution in tap water to a starting concentration of 1.5% v/v.
Table 1.
Summary of disinfectants assessed for efficacy against Ebola virus (EBOV)-Ecran.
| Name | Supplier | Active Components (%) | Preparation | Final % Tested (v/v) | Volume Tested (µL) | Contact Time (Mins at RT) |
|---|---|---|---|---|---|---|
| Ardrox 6092 | Chemetall, UK | 3-Butoxypropan-2-ol, propylene glycol monobutyl ether (3–5); Disodium metasilicate (1–2.5); Alcohol ethoxylate (1–2.5) | Used neat | 50.0 | 50 | 10 |
| Calla 1452 | Zip-chem products, CA, US | Alkyl Dimethyl benzylammonium Chloride (1.1); Di(octyl-decyl) dimethyl ammonium Chloride (1.6); Ethanol (0.3) | 1:32 dilution in tap water | 1.5 | 50 | 10 |
| Desintex | Laboratoires Rochex, France | Alkylamine (8.7); PolyHexaMethyleneBiguanide (2.1); Quaternary ammonium (3.1) | 1:20 dilution in tap water | 2.5 | 50 | 10 |
| Sodium Hypochlorite | SyChem, UK | Sodium hypochlorite (14–15); Potassium permanganate (<1) | 1:10 dilution in tap water | 0.75 | 50 | 10 |
Aircraft relevant materials were supplied directly by 1710 Naval Air Squadron as pre-cut coupons and were not pre-conditioned in any way. The coupons assessed were painted aluminium and pilot seat-belt strapping material in 1 cm2 discs.
All growth and manipulation of EBOV-Ecran was performed within a Class III microbiological safety cabinet within a dedicated containment level 4 laboratory at Defence Science and Technology Laboratory (Dstl), Porton Down [12].
2.2. Recovery Testing
To optimise recovery of EBOV-Ecran from different materials, virus was deposited onto coupons of aluminium or strapping in 50 µL droplets at room temperature. Samples were then placed into TCM sufficient to be submerged (2 mL), and vortexed for 10 s before being enumerated by standard TCID50 assay. Recovery of EBOV-Ecran from sterile 6-well cell culture plates served as a positive control and recovery of TCM only from aluminium and strapping was used as a negative control. All recovery testing was performed in triplicate. In an attempt to optimise recovery, vortex times were increased or samples were vortexed multiple times.
2.3. Toxicity Testing
To test the toxicity of disinfectants against the Vero C1008 cell line, each disinfectant was added to a contact plate and incubated at room temperature for 10 min. Samples were then washed by centrifugation at 10,000 rpm for 5 min in a Microcentaur MSE centrifuge allowing the formation of a pellet which was re-suspended in TCM and enumerated using the TCID50 assay. Cells were observed for signs of toxicity. EBOV-Ecran only (no disinfectant) was used as a positive control, and TCM without virus was used as a negative control. All testing was performed in triplicate. To reduce toxicity, the number of washes was increased as necessary.
2.4. Efficacy of Different Disinfectants by Virus Enumeration
Coupon assessments were made with a single contact time of 10 min at room temperature (Table 1). In triplicate, 50 µL of disinfectant (or TCM as a positive control) was added to 50 µL EBOV-Ecran on aluminium or strapping coupons, or directly to a sterile 6-well cell culture plate. Additionally, disinfectant was added to 50 µL TCM only as a negative control. After 10 min contact time, virus was recovered by vortexing for 10 s followed by washing by centrifugation with TCM up to three times, sufficient to reduce toxicity to Vero C1008 cells. TCID50 enumeration was performed on all samples. Test samples were evaluated against the control samples with a 4-log10 reduction in viral titre being the standard minimum for a disinfectant to be considered effective.
2.5. Efficacy of Different Disinfectants by Cell Passage
Samples were also qualitatively assessed for inactivation by serial passage [13]. Washed samples generated as above were used to infect flasks of Vero C1008 cells (5 mL total volume) and incubated at 37 °C/5% CO2 for 7 days. After this time, flasks were observed for signs of infection (cytopathic effects, CPE) and the flasks were passaged in to a larger volume (10 mL) of fresh TCM and incubated for a further 7 days. After observation for CPE, flasks were passaged a third and final time into 20 mL TCM and incubated for another 7 days. If no signs of infection (no CPE) were observed after 3 passages, samples were considered to be free of viable virus.
2.6. Statistical Analysis
GraphPad Prism (version 6.02, La Jolla, CA, USA) was used to analyse the efficacy data. Two-way ANOVA with Bonferroni’s multiple comparison test was used for each coupon type to compare the mean log reduction in titre from control of each disinfectant to the log reduction when no disinfectant was used (0) at the 95% confidence level. Additionally, identical 2-way ANOVA analysis was used for each disinfectant to compare the mean log reduction in titre of the different coupon types.
3. Results
3.1. Recovery of EBOV-Ecran from Test Surfaces and Toxicity of Disinfectants to Cells
In triplicate, samples of EBOV-Ecran were deposited on two test surfaces, aluminium and pilot strapping material. Results are shown in Figure 1. The mean titre of EBOV-Ecran recovered from a sterile cell culture plate (no coupon) was 1.3 × 106 TCID50/mL. The mean titre recovered from aluminium coupons was 5.9 × 105 TCID50/mL, representing a 45% recovery efficiency and a high enough titre to determine a 4-log10 reduction. No further attempts were made to optimise recovery from aluminium coupons. The mean titre recovered from strapping was 4.1 × 103 TCID50/mL. This represents a recovery efficiency of only 0.32%. The limit of quantification of the TCID50 assay is 10 TCID50/mL, therefore a starting titre of at least 1 × 105 TCID50/mL is required to demonstrate a 4-log10 reduction. Attempts to improve recovery from strapping were not successful (results not shown). Therefore, in addition to reduction in viral titre, strapping samples were subjected to serial passage in Vero C1008 cells to confirm inactivation.
Figure 1.
Recovery of Ebola virus (EBOV)-Ecran from different test surfaces. EBOV-Ecran or tissue culture media (TCM) was deposited onto 2 different coupon types, or directly onto a sterile 6-well cell culture plate (no coupon), before being recovered into 2 mL TCM by vortexing for 10 s. Samples were washed up to three times prior to enumeration. The titre of EBOV-Ecran (in TCID50/mL) recovered from 3 replicate tests is shown (±SEM). All TCM samples were negative for viable EBOV-Ecran. TCID50: 50% tissue culture infectious dose.
Four disinfectants (see Table 1) were tested for toxicity in cells in triplicate. Calla 1452, Ardrox 6092 and sodium hypochlorite were rendered non-toxic to cells after one wash in TCM (results not shown). Desintex required three washes to remove toxic components (results not shown).
3.2. Coupon Disinfectant Assays
Four disinfectants (see Table 1) were tested for the ability to reduce the viral titre of EBOV-Ecran on different coupon types. All samples were tested by enumeration in TCID50/mL after a 10 min contact time at room temperature (Table 2). The limit of quantification (LoQ) of the TCID50 assay is 10 TCID50/mL. This equates to 50% (4/8 well in a 96-well plate format) of neat sample being observed to have CPE in the TCID50 assay. However, <50% of the inoculated wells may be positive for CPE (e.g., 1, 2 or 3 of 8 positive wells in the neat dilution), indicating viable virus is present but is <10 TCID50/mL. This number cannot truly be enumerated by the method of Reed and Muench [9].
Table 2.
Recovery of EBOV-Ecran recovered from different test surfaces after treatment with four disinfectants.
| Sample Type | Mean Titre of EBOV-Ecran Recovered (TCID50/mL) | ||
|---|---|---|---|
| Aluminium (n = 3) | Strapping (n = 3) | No Coupon (n = 6) | |
| EBOV-Ecran + TCM | 1.5 × 105 | 2.2 × 103 | 1.1 × 105 |
| EBOV-Ecran + Ardrox 6092 | 0 * | 0 * | 0 * |
| EBOV-Ecran + Calla 1452 | 7.0 × 102 | 2.3 × 102 | 7.0 ** |
| EBOV-Ecran + sodium hypochlorite | 0 * | 0 * | 0 * |
| EBOV-Ecran + Desintex | 1.6 × 10 1 | 0 * | 2.4 ** |
TCID50/mL: 50% tissue culture infectious dose per mL; * No viable virus observed in TCID50 assay; ** Extrapolated, virus observed but below limit of quantification (LoQ) (10 TCID50).
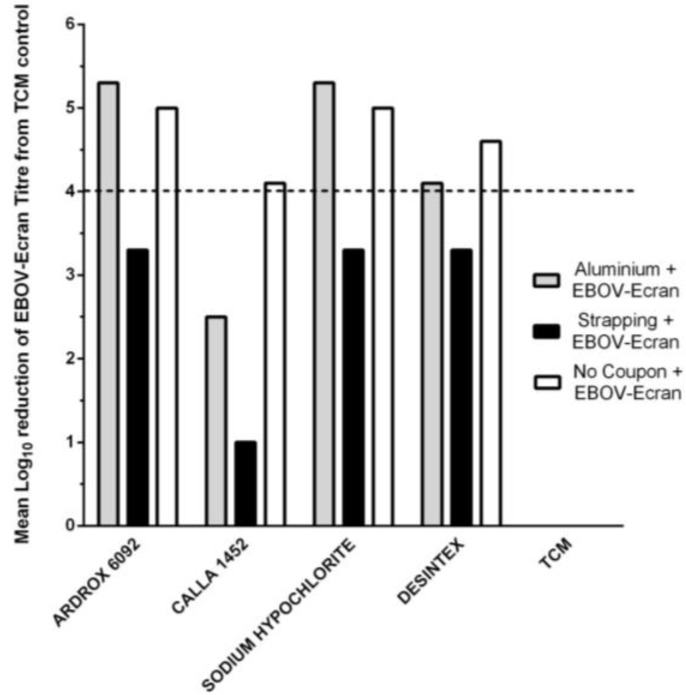
Efficacy of the four disinfectants was determined by comparing the mean log reduction in EBOV-Ecran with the positive control (EBOV-Ecran + TCM; Table 2, Figure 2). The British standards require a 4-log10 reduction of virus for a disinfectant to be classed as effective [8].
Figure 2.
Reduction in EBOV-Ecran titre on different test surfaces after contact with four different disinfectants. EBOV-Ecran was deposited onto three surfaces and an equal volume of disinfectant or TCM was added for a contact time of 10 min (n = 3). When TCM was added to virus in place of disinfectant, high titres of EBOV-Ecran were recovered (Table 2; 1.5 × 105 TCID50/mL from aluminium; 2.2 × 103 TCID50/mL from strapping and 1.1 × 105 TCID50/mL from no coupon) and these values served as the positive control against which disinfectants were assessed. The reduction in log10 titre was determined as the difference between the mean log10-titre with no disinfection (TCM only) and the mean log10-titre for each disinfectant on aluminium coupons (grey bars), strapping coupons (black bars) or directly onto a sterile 6-well cell culture plate (no coupon, white bars). The British standard minimum requirement is a 4-log10 reduction (dashed line).
3.2.1. Efficacy of Four Disinfectants against EBOV-Ecran on Aluminium Coupons
For the aluminium coupons, under the parameters tested, the mean titre of EBOV-Ecran recovered from the coupon was ~1.5 × 105 TCID50/mL. Addition of sodium hypochlorite or Ardrox 6092 resulted in no detectable virus in the TCID50 assay (Table 2). There was also no detectable EBOV-Ecran when Ardrox 6092 and sodium hypochlorite were added to virus on a sterile cell culture plate (no coupon; Table 2). When Calla 1452 was added to EBOV-Ecran on aluminium coupons 7 × 102 TCID50/mL of EBOV-Ecran was recovered from the sample and when Calla 1452 and EBOV-Ecran were mixed on a sterile cell culture plate, viable virus was also seen (Table 2). Low levels of EBOV-Ecran were detected when Desintex was added to aluminium coupons and viable virus was also observed, albeit below the LoQ of the assay, when Desintex and EBOV-Ecran were tested on a sterile cell culture plate only (Table 2).
For the aluminium coupons, a greater than 4-log10 drop in EBOV-Ecran titre was observed with Ardrox 6092 and sodium hypochlorite (Figure 2). Based on mean counts, a 4-log10 drop in EBOV-Ecran titre was also observed with Desintex on aluminium, although viable virus was recovered (Table 2). When no coupon was present, a 4-log10 drop in EBOV-Ecran titre was observed for all four disinfectants (Figure 2).
3.2.2. Efficacy of Four Disinfectants against EBOV-Ecran on Strapping Coupons
Poor recovery was observed for pilot strapping (Figure 1), with a mean titre of 2 × 103 TCID50/mL. A 4-log10 reduction in titre therefore fell below the LoQ of the assay. Samples were still processed in the TCID50 assay despite the inability to observe the necessary reduction in order to identify a degree of activity prior to serial cell passage. As with the aluminium coupons, no viable virus could be detected on strapping coupons treated with Ardrox 6092 or sodium hypochlorite in the TCID50 assay (Table 2). When Calla 1452 was added to EBOV-Ecran on strapping, 2.3 × 102 TCID50/mL of EBOV-Ecran was recovered and when Desintex and EBOV-Ecran were tested on strapping coupons no viable virus was detected (Table 2). The use of TCM in place of EBOV-Ecran as a negative control was conclusive for all samples types as no viable virus was detected (results not shown). Due to poor recovery, a 4-log10 reduction in titre was not achieved with any disinfectant on the strapping coupons (Figure 2).
Additional qualitative testing of disinfectants on strapping coupons was performed by serial passage. All samples from strapping coupons treated with disinfectant or media only were subject to three passages in cells to allow for amplification of low numbers of viable virus to detectable limits. After three passages, no viable virus was observed in replicate Ardrox 6092- or sodium hypochlorite-treated samples suggesting there had been complete inactivation of EBOV-Ecran on the strapping coupons when treated with these disinfectants. Desintex-treated strapping coupons were also all negative for viable virus after three passages, with the exception of one of the Desintex-treated EBOV-Ecran samples from a sterile cell culture plate (no coupon) after the second passage. This suggests that this concentration of Desintex does not consistently provide complete inactivation. Calla 1452-treated samples were positive for viable virus after the first passage (when recovered from strapping coupons and after the second passage when recovered from a sterile cell culture plate (no coupon).
Two-way ANOVA analysis with Bonferroni’s multiple comparison test indicated that the difference in log reduction for each disinfectant compared to the log reduction with no disinfectant (TCM only, 0, no reduction) was significant for Ardrox 6092, sodium hypochlorite and Desintex on all three surface types (p ≤ 0.01 for aluminium and for when no coupon was used and p ≤ 0.05 for strapping). Calla 1452 produced a significant log reduction from control only when no coupon was present (p ≤ 0.01). For each disinfectant, there was no significant difference in log reduction between the three different surface types.
4. Discussion and Conclusions
The worst outbreak of EVD in history has highlighted the need for effective disinfectants [1,2,4,5,6]. Although efficacy is the primary objective, the disinfectants also need to be appropriate for their intended use. Disinfectants may be required for use on the skin and body parts, complex surfaces, delicate instruments and textiles and on small or large areas. Whilst chlorine-based products are widely recommended for use against EBOV, and used internationally in hospitals, laboratories and in the community, they can also be damaging. Equipment or apparatus that is damaged may lose integrity, utility or reduce safe operation, therefore alternative effective disinfectants are needed. Three disinfectants for which there is no published data available were tested for activity against EBOV-Ecran alongside sodium hypochlorite as a control disinfectant on two representative aircraft relevant surfaces. The surfaces, painted aluminium and pilot seat-belt strapping, were also representative of other porous or non-porous surfaces that may be encountered on transport vehicles, buildings or other settings.
As perhaps expected, sodium hypochlorite performed well in our assessments in that no viable virus was recovered from either aluminium or strapping coupons, or when no coupon was present. Different chlorine-based products will have different properties and will react differently with different material. A single concentration of sodium hypochlorite (SyChem) was tested here, but 0.75% sodium hypochlorite met the minimum British standards under the conditions tested. The efficacy of sodium hypochlorite against a different EBOV has already been investigated by others using similar methods to our work [14]. In this work, 0.5% and 1.0% sodium hypochlorite gave complete reduction in viral titre after 5 min contact time whereas concentrations of 0.1% and 0.01% were not effective in reducing viral titre over 10 min contact time [14]. Our data is consistent with these results and provides evidence of a further concentration of sodium hypochlorite (0.75%) demonstrating efficacy against EBOV-Ecran. For General Healthcare Settings in West Africa the CDC recommends 0.5% as strong for disinfecting ‘surfaces, objects, medical equipment, and gloved hands’ and a milder 0.05% for hand washing etc. [15]. The lower concentration may not be effective but higher concentrations have been reported to affect equipment [7] and personnel [16] and were shown to be damaging to aircraft surfaces [17]. An alternative to liquid chlorine based products for general disinfection is the use of gaseous chlorine dioxide which has been used to decontaminate hospitals and large areas previously [18,19]. However, surrogate testing suggests this method should not be relied on solely to be effective against EBOV [20] and further efficacy testing and assessment for corrosiveness and potential damage from this form of disinfection is required. Likewise, other forms of gaseous disinfection (e.g., hydrogen peroxide) or other methods of inactivation (such as UV light) could be considered. However, in an outbreak environment where there may be limited infrastructure, training or there may not be the appropriate personal protective equipment to work with more novel disinfection methods, simpler methods are likely to be more advantageous.
The active components of Desintex are alkylamine and quarternary ammonium compounds. Our results demonstrated good efficacy of 2.5% Desintex although not complete inactivation. A reduction in titre of EBOV-Ecran by over 3-log10 was observed on both coupon types as well as on sterile cell culture plates. However, viable virus was detected when Desintex was added to EBOV-Ecran on aluminium coupons and when no coupon was present. EBOV-Ecran was not detected on strapping coupons although recovery levels were low from this coupon type, and when samples were serially passaged there was no detectable virus-induced CPE. Although under the conditions tested Desintex meets the British Standard requirements, this is a minimum requirement and the fact that viable virus remained should be noted. EBOV strains have been shown to be infectious at low levels, and to remain infectious in different matrices [21,22,23,24]. Desintex has also been shown to be damaging to aircraft surfaces [17] so may not be a suitable alternative to sodium hypochlorite for use on aircraft. It is also important to note that Dstl routinely uses Desintex at a final concentration of 5% v/v, twice the concentration tested in these studies.
Ardrox 6092 is a water-based alkaline (pH > 11) cleaner designated as suitable for cleaning civil and military fixed wing aircraft and helicopters. Calla products contain ethanol, alkyl dimethyl benzyl- and di(octyl-decyl)-ammonium chloride and are also sold as aircraft cleaners. Calla 1452 has been included in the cleaning supplies on aircraft used to move EBOV-infected patients [25] as it is specifically a hard surface, interior aircraft disinfectant. Both Ardrox 6092 and Calla 1452 are commonly used by the UK military for routine cleaning of aircraft and do not damage the airframes [17] but their efficacy against EBOV had not been determined. Our results show that Calla 1452 is not effective against EBOV-Ecran on the two coupons tested; under the conditions described Calla 1452 showed minimal reduction in viral load falling below the level required to meet British disinfection standards [8]. However, the efficacy of Calla 1452 may be improved with increased contact times or different concentrations. The results generated in this study would suggest that is it not currently advisable to use Calla 1452 to disinfect aircraft surfaces that may be contaminated with EBOV.
Ardrox 6092 was demonstrated to show efficacy against EBOV-Ecran under the conditions tested and therefore further efficacy characterisation should be pursued for example different contact times, disinfectant concentrations or volumes or different matrices. Ardrox 6092 is known to be non-corrosive to aircraft [17] but the effect of high pH on virus activity had not been determined. Viable virus was not recovered from aluminium or strapping coupons when Ardrox 6092 was applied although it was not possible to determine a 4-log10 reduction for the strapping coupons (a 3-log10 reduction was achieved). Recovery from strapping was poor; despite numerous attempts to increase recovery, and success with other porous material, it was not possible to improve efficiency from strapping. Poor recovery from airline carpet material had been previously observed [26] whilst a recent study using providone-iodine hand wash solutions against EBOV described an alternative method of large volume plating to verify efficacy and increased sensitivity when low titres of stock EBOV were harvested from culture [27]. Utilising this method may have improved sensitivity when assaying strapping samples but we did not have the capability to do this or to produce a higher titre starting stock. The promising efficacy of Ardrox 6092 against EBOV-Ecran necessitates inclusion in future studies and for further assessment against other viruses, surfaces and matrices.
Further assessments of disinfectant action on strapping material were made by serial cell passage in order to amplify any low levels of virus that may have been present in the sample and therefore increased the sensitivity of the testing. Previously it has been shown that 0.1 TCID50 can be amplified by passage in tissue culture flasks [13], therefore the results using Ardrox 6092 and the detection limit of the flask passage under the conditions tested in these experiments, indicated that Ardrox 6092 is likely to meet the minimum standards required. However, improved recovery efficiency or an alternative method of analysis would be required to determine this.
Our studies were limited to testing EBOV-Ecran only in TCM which is not representative of the type of matrix that may be encountered in the field, where EBOV will be present in bodily fluids including but not limited to, blood, vomit and faeces [26]. The survival of different isolates of EBOV in blood [14,21,22,24,26] and in other bodily fluids or specimens [24,26] has been reported. The organic matter in more complex matrices such as bodily fluids may initiate a reaction with the disinfectant or may provide protection to the virus, affecting the mode of action of disinfectant. Complications may also arise from potential sample toxicity and recovery of virus thereby rendering results more difficult to interpret. TCM is a representative matrix encountered in the laboratory and provides an initial starting point in the assessment of disinfectant efficacy against pathogenic viruses. Disinfectants that show efficacy in TCM can be taken forward for further study in more complex matrices, whilst disinfectants that do not work in TCM are un-likely to be efficacious in more complex media although further testing in alternative matrices is recommended.
Additionally, we did not use the EBOV strain responsible for the West Africa outbreak (EBOV-Makona) due to availability at the time, lack of characterisation and low titre during initial experiments. However, initial phylogenetic analysis of isolates from West Africa shows they are a distinct clade but still have high homology with early EBOV strains [1,28]. The protocols performed in these studies may be considered a ‘worse-case scenario’ as there was no mixing of virus and disinfectant, and equal volumes were used. There are multiple factors and conditions that contribute to a disinfectant’s effectiveness and it was not in the scope of this study to investigate all parameters. Further work is required to fully characterize the efficacy of these and other disinfectants for use against highly pathogenic viruses.
The need to find further disinfectants that are effective against EBOV that can be used in a range of scenarios remains. Under the conditions tested in this study, Calla 1452 has limited efficacy against EBOV-Ecran, but aircraft cleaner Ardrox 6092 may be an effective alternative to corrosive sodium hypochlorite for aircraft relevant materials and other vulnerable surfaces.
Acknowledgments
This work was funded by Naval Air Squadron, HM Naval Base, Portsmouth, UK. The authors acknowledge the help of Jackie Steward with experimental work.
Author Contributions
Amanda Phelps, Mark S Lever and Andrew Dutch secured the funding; Sophie Smither, Amanda Phelps and Mark S Lever conceived and designed the experiments; Sophie Smither, Amanda Phelps, Lin Eastaugh, Sarah Ngugi and Lyn O’Brien made substantial contributions to performing the experiments; Sophie Smither and Amanda Phelps analysed the data and interpreted the results; Lin Eastaugh and Andrew Dutch contributed reagents and materials; Sophie Smither wrote the paper, Amanda Phelps and Mark S Lever helped in preparation of the manuscript.
Conflicts of Interest
Dstl authors claim no conflict of interest. Andrew Dutch had no role in the collection, analyses, or interpretation of data or in the writing of the manuscript.
References
- 1.Baize S., Pannetier D., Oestereich L., Rieger T., Koivogui L., Magassouba N., Soropogui B., Sow M.S., Keïta S., De Clerck H., et al. Emergence of Zaire Ebola virus disease in Guinea. N. Engl. J. Med. 2014;371:1418–1425. doi: 10.1056/NEJMoa1404505. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization Situation Reports. [(accessed on 31 May 2016)]. Available online: http://www.who.int/csr/disease/ebola/situation-reports/archive/en/
- 3.Mitchell S.W., McCormick J.B. Physicochemical inactivation of Lassa, Ebola, and Marburg viruses and effect on clinical laboratory analyses. J. Clin. Microbiol. 1984;20:486–489. doi: 10.1128/jcm.20.3.486-489.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.CDC Management of Patients with Suspected Viral Hemorrhagic Fever. [(accessed on 21 April 2016)]; Available online: http://www.cdc.gov/mmwr/preview/mmwrhtml/00037085.htm.
- 5.CDC Interim Guidance for Managing Patients with Suspected Viral Hemorrhagic Fever in U.S. Hospitals. [(accessed on 21 April 2016)]; Available online: http://www.cdc.gov/HAI/pdfs/bbp/VHFinterimGuidance05_19_05.pdf.
- 6.WHO Laboratory Diagnosis of Ebola Virus Disease. [(accessed on 21 April 2016)]. Available online: http://apps.who.int/iris/bitstream/10665/134009/1/WHO_EVD_GUIDANCE_LAB_14.1_eng.pdf.
- 7.Johnston A.M., Lewis S.E. Decontaminating Ebola-infected ultrasound probes. Anaesthesia. 2015;70:628–629. doi: 10.1111/anae.13060. [DOI] [PubMed] [Google Scholar]
- 8.British Standards Institution BSEN 14476:2013+A1:2015. Chemical Disinfectants and Antiseptics. Quantitative Suspension Test for the Evaluation of Virucidal Activity in the Medical Area. Test Method and Requirements (Phase 2/Step 1) 2013. [(accessed on 9 July 2015)]. Available online: http://shop.bsigroup.com/ProductDetail/?pid=000000000030318301.
- 9.Reed L.J., Muench H. A simple method of estimating fifty per cent endpoints. Am. J. Hyg. 1938;27:493–497. [Google Scholar]
- 10.Kuhn J.H., Lofts L.L., Kugelman J.R., Smither S.J., Lever M.S., van der Groen G., Johnson K.M., Radoshitzky S.R., Bavari S., Jahrling P.B., et al. Reidentification of Ebola virus E718 and ME as Ebola Virus/H.sapiens-tc/COD/1976/Yambuku-Ecran. Genome Announc. 2014;2:e1178–e1114. doi: 10.1128/genomeA.01178-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smither S.J., Lear-Rooney C., Biggins J., Pettitt J., Lever M.S., Olinger G.G., Jr. Comparison of the plaque assay and 50% tissue culture infectious dose assay as methods for measuring filovirus infectivity. J. Virol. Methods. 2013;193:565–571. doi: 10.1016/j.jviromet.2013.05.015. [DOI] [PubMed] [Google Scholar]
- 12.Smither S.J., Lever M.S. A review of filovirus work and facilities at the Defence Science and Technology Laboratory Porton Down. Viruses. 2012;4:1305–1317. doi: 10.3390/v4081305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smither S.J., Weller S.A., Phelps A., Eastaugh L., Ngugi S., O’Brien L.M., Steward J., Lonsdale S.G., Lever M.S. Buffer AVL alone does not inactivate Ebola virus in a representative clinical sample type. J. Clin. Microbiol. 2015;53:3148–3154. doi: 10.1128/JCM.01449-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cook B.W., Cutts T.A., Nikiforuk A.M., Poliquin P.G., Court D.A., Strong J.E., Theriault S.S. Evaluating environmental persistence and disinfection of the Ebola virus Makona variant. Viruses. 2015;7:1975–1986. doi: 10.3390/v7041975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.CDC For General Healthcare Settings in West Africa: How to Prepare and Use Chlorine Solutions. [(accessed on 31 May 2016)]; Available online: http://www.cdc.gov/vhf/ebola/hcp/mixing-chlorine-solutions.html.
- 16.Carpenter A., Cox A.T., Marion D., Phillips A., Ewington I. A case of a chlorine inhalation injury in an Ebola treatment unit. J. R. Army Med. Corps. 2015;162:229–231. doi: 10.1136/jramc-2015-000501. [DOI] [PubMed] [Google Scholar]
- 17.Andrew Dutch, NAVY 1710NAS-MIG CCHS 2. Personal communication.
- 18.Lowe J.J., Gibbs S.G., Iwen P.C., Smith P.W., Hewlett A.L. Decontamination of a hospital room using gaseous chlorine dioxide: Bacillus anthracis, Francisella tularensis, and Yersinia pestis. J. Occup. Environ. Hyg. 2013;10:533–539. doi: 10.1080/15459624.2013.818241. [DOI] [PubMed] [Google Scholar]
- 19.Doona C.J., Feeherry F.E., Kustin K., Olinger G.G., Setlow P., Malkin A.J., Leighton T. Fighting Ebola with novel spore decontamination technologies for the military. Front. Microbiol. 2015;6:663. doi: 10.3389/fmicb.2015.00663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lowe J.J., Hewlett A.L., Iwen P.C., Smith P.W., Gibbs S.G. Surrogate testing suggests that chlorine dioxide gas exposure would not inactivate Ebola virus contained in environmental blood contamination. J. Occup. Environ. Hyg. 2015;8 doi: 10.1080/15459624.2015.1043058. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 21.Piercy T.J., Smither S.J., Steward J.A., Eastaugh L., Lever M.S. The survival of filoviruses in liquids, on solid substrates and in a dynamic aerosol. J. Appl. Microbiol. 2010;109:1531–1539. doi: 10.1111/j.1365-2672.2010.04778.x. [DOI] [PubMed] [Google Scholar]
- 22.Fischer R., Judson S., Miazgowicz K., Bushmaker T., Prescott J., Munster V.J. Ebola virus stability on surfaces and in fluids in simulated outbreak environments. Emerg. Infect. Dis. 2015;2:1243–1246. doi: 10.3201/eid2107.150253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Judson S., Prescott J., Munster V. Understanding ebola virus transmission. Viruses. 2015;7:511–521. doi: 10.3390/v7020511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Prescott J., Bushmaker T., Fischer R., Miazgowicz K., Judson S., Munster V.J. Postmortem stability of Ebola virus. Emerg. Infect. Dis. 2015;21:856–859. doi: 10.3201/eid2105.150041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Thoms W.E., Wilson W.T., Grimm K., Conger N.G., Gonzales C.G., DeDecker L., Hatzfeld J.J. Long-range transportation of Ebola-exposed patients: An evidence-based protocol. Am. J. Infect. Dis. Microb. 2015;2:19–24. [Google Scholar]
- 26.Schuit M., Miller D.M., Reddick-Elick M.S., Wlazlowski C.B., Filone C.M., Herzog A., Colf L.A., Wahl-Jensen V., Hevey M., Noah J.W. Differences in the comparative stability of Ebola virus Makona-C05 and Yambuku-Mayinga in Blood. PLoS ONE. 2016;11:185. doi: 10.1371/journal.pone.0148476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Eggers M., Eickmann M., Kowalski K., Zorn J., Reimer K. Povidone-iodine hand wash and hand rub products demonstrated excellent in vitro virucidal efficacy against Ebola virus and modified vaccinia virus Ankara, the new European test virus for enveloped viruses. BMC Infect. Dis. 2015;15:375. doi: 10.1186/s12879-015-1111-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gire S.K., Goba A., Andersen K.G., Sealfon R.S., Park D.J., Kanneh L., Jalloh S., Momoh M., Fullah M., Dudas G., et al. Genomic surveillance elucidates Ebola virus origin and transmission during the 2014 outbreak. Science. 2014;345:1369–1372. doi: 10.1126/science.1259657. [DOI] [PMC free article] [PubMed] [Google Scholar]