Abstract
Neuroendocrine carcinoma (NEC) originating from the gastrointestinal hepatobiliary-pancreas is a rare, invasive, and progressive disease, for which the prognosis is extremely poor. The patient was a 72-year-old man referred with complaints of jaundice. He was diagnosed with middle extrahepatic cholangiocarcinoma (cT4N1M0, cStage IV). He underwent a right hepatectomy combined with extrahepatic bile duct and portal vein resection after percutaneous transhepatic portal vein embolization. Microscopic examination showed a large-cell neuroendocrine carcinoma according to the WHO criteria for the clinicopathologic classification of gastroenteropancreatic neuroendocrine tumors. Currently, the patient is receiving combination chemotherapy with cisplatin and etoposide for postoperative multiple liver metastases. Although NEC is difficult to diagnose preoperatively, it should be considered an uncommon alternative diagnosis.
Keywords: Neuroendocrine carcinoma, Extrahepatic bile duct, Neuroendocrine tumor
Core tip: We encountered a resected case of a neuroendocrine carcinoma originating from the extrahepatic bile duct. Although neuroendocrine carcinoma is rare and difficult to diagnose preoperatively, it should be considered an uncommon alternative diagnosis.
INTRODUCTION
Currently, the 2010 World Health Organization (WHO) classification recommends that neuroendocrine tumors (NETs) be classified as NET Grade 1, NET Grade 2, and neuroendocrine carcinoma (NEC) Grade 3[1]. NEC originating from the gastrointestinal hepatobiliary-pancreas is a very rare, invasive, and progressive disease for which the prognosis is extremely poor. We encountered a resected case of NEC originating from the extrahepatic bile duct. Herein, we present the clinicopathological features and clinical course of the patient with NEC of the extrahepatic bile duct and provide a brief review of the literature.
CASE REPORT
The patient was a 72-year-old man referred from a local hospital with complaints of jaundice. Laboratory data on admission showed elevated total bilirubin (T-bil), 12.2 mg/dL (normal range, 0.2-1.2 mg/dL); lactic acid dehydrogenase, 237 U/L (124-232 U/L); alkaline phosphatase, 1070 U/L (120-320 U/L); and γ-glutamyl transpeptidase, 899 U/L (5-55 U/L). The tumor markers tested were within normal limits; specifically, carcinoembryonic antigen (CEA), 2.8 ng/mL (normal range, < 5.0 ng/mL), and carbohydrate antigen 19-9, 916.8 U/mL (< 37 U/mL). Magnetic response cholangiopancreatography (MRCP) and endoscopic retrograde cholangiopancreatography (ERCP) demonstrated the presence of severe stenosis of the middle part of the common bile duct (CBD) (Figure 1). The patient underwent endoscopic nasobiliary drainage (ENBD) with the aim of reducing jaundice. Abdominal computed tomography (CT) showed a tumor in the middle portion of the CBD and dilatation of the CBD and the intrahepatic bile ducts bilaterally (Figure 2). The tumor was suspected to have invaded the right hepatic artery and the portal vein. According to the Union Internationale Contre le Cancer (UICC) guidelines, the patient was diagnosed with middle extrahepatic cholangiocarcinoma (cT4N1M0, cStage IV)[2]. On the 3D reconstructed CT image, we confirmed the patient’s condition and simulated the operative procedure (Figure 3). A right hepatectomy combined with extrahepatic bile duct and portal vein resection after percutaneous transhepatic portal vein embolization was planned. The operation was successfully performed. Peritoneal lavage cytology demonstrated no cancer cells in the abdominal cavity. No microscopic invasion of the resected bile duct stump was observed in an intraoperative frozen specimen. The patient underwent a curative resection.
Figure 1.
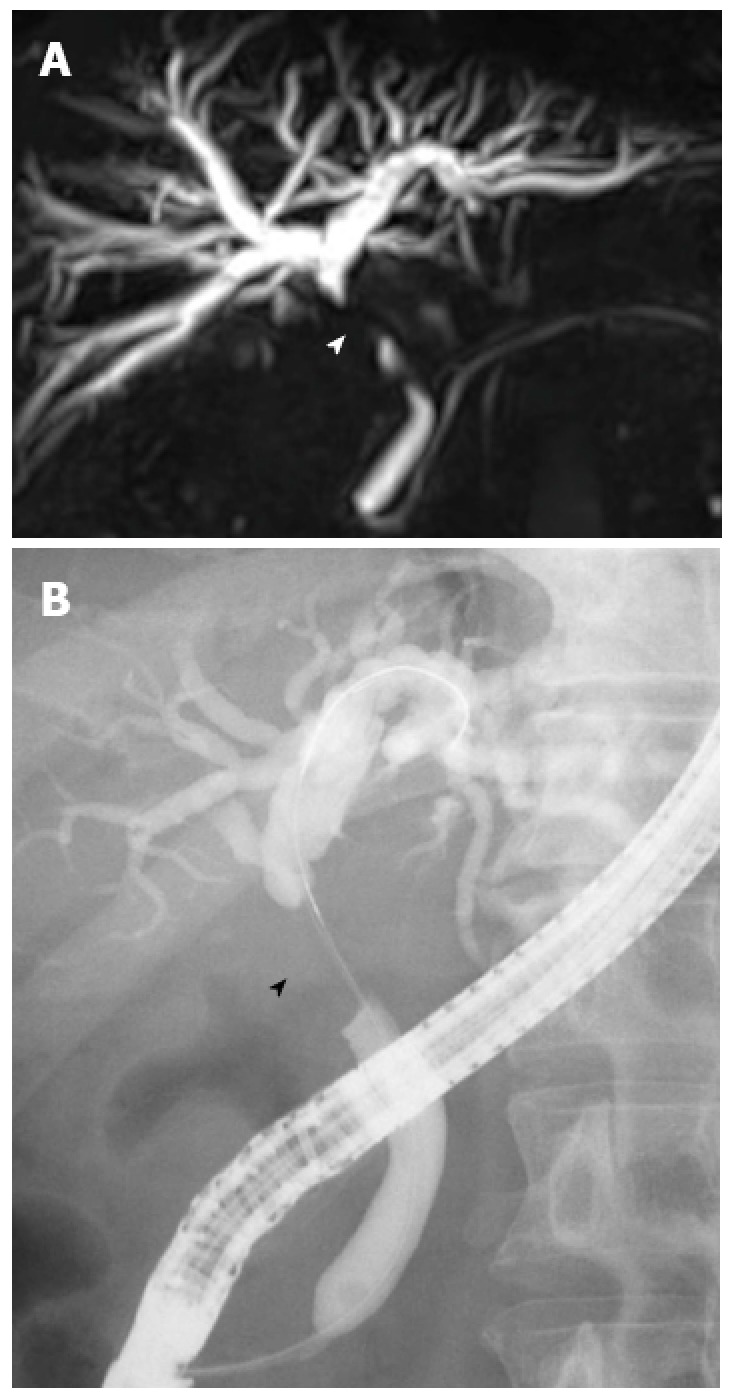
Magnetic resonance cholangiopancreatography (A) and endoscopic retrograde cholangiopancreatography (B) of the bile duct. Severe stenosis of the middle common bile duct was observed (arrowhead).
Figure 2.
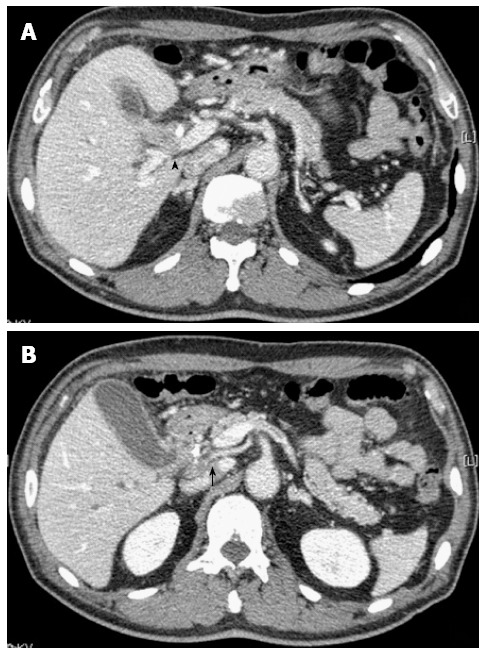
Abdominal computed tomography images at two different levels are shown. A: Computed tomography (CT) showed a low-density mass measuring 18 mm in diameter located in the middle bile duct adjacent to the portal vein (arrowhead). An endoscopic nasobiliary drainage tube was observed in the bile duct; B: CT showed a low-density mass involving the right hepatic artery from the superior mesenteric artery in the middle bile duct (arrow).
Figure 3.
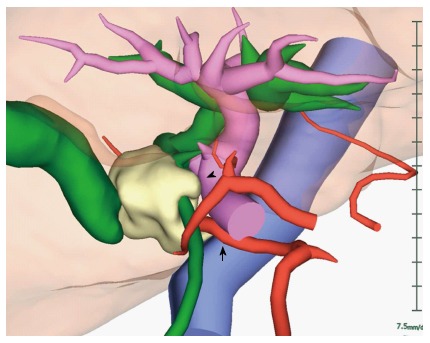
3D reconstructed computed tomography fused with an magnetic resonance cholangiopancreatography image. The tumor was located in the middle bile duct. The tumor was suspected to have invaded the portal vein (arrowhead) and the right hepatic artery from the superior mesenteric artery (arrow).
Pathologic findings
Macroscopically, a white, solid tumor measuring 30 mm × 30 mm × 25 mm was located in the middle portion of the CBD and cystic duct. On microscopic examination, tumor cells were detected in the middle CBD (Figure 4). The tumor cells were round or oval, hyperchromatic, and had an increased nucleus-to-cytoplasm ratio. Mitotic figures were quite frequent and were observed in 55 cells per 10 high-power fields. Immunohistochemically, the tumor cells were diffusely positive for CD56, a membrane protein usually present in neuroendocrine cells. Tumor cells were positive for synaptophysin, which is typically expressed on the surface of neurons or endothelial cells. The Ki-67 labeling index was 56.2%. These findings were consistent with large-cell neuroendocrine carcinoma according to the WHO criteria for the clinicopathologic classification of gastroenteropancreatic NETs[1]. According to the UICC guidelines, the final classification of the tumor was T3aN1M0 Stage IIB.
Figure 4.
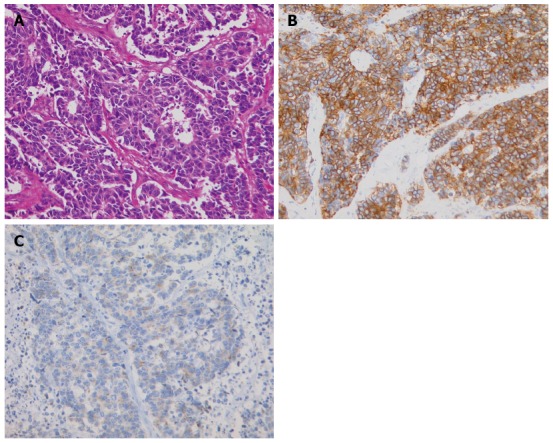
Histopathologic appearance of the neuroendocrine carcinoma. A: The cells were round or oval, hyperchromatic, and had an increased nucleus-to-cytoplasm ratio (hematoxylin-eosin staining, magnification × 200); B: Immunohistochemically, tumor cells were diffusely positive for CD56, a membrane protein usually present in neuroendocrine cells; C: Immunohistochemically, tumor cells were positive for synaptophysin, which is typically expressed on the surface of neurons or endothelial cells.
Although the patient developed postoperative liver failure, he recovered and was discharged on postoperative day 51 in good condition. However, multiple liver metastases appeared 3 mo after the surgery. Currently, the patient is receiving combination chemotherapy with cisplatin and etoposide. He is now alive 7 mo after surgery.
DISCUSSION
Most extrahepatic bile duct tumors are adenocarcinomas, while other types of tumors are rare[3]. Biliary neuroendocrine carcinoma represents 0.19% of extrahepatic bile duct tumors[4]. Furthermore, NEC arising from the biliary tract is rare. NECs were previously classified as small-cell carcinomas (SCCs)[5]. We conducted a systematic literature search using PubMed (1985-2015) with the following keywords: “neuroendocrine carcinoma,” “small cell carcinoma,” and “biliary tract” and found only 24 reported cases of NEC of the extrahepatic biliary tracts, excluding the intrahepatic bile duct, the gallbladder, and the ampulla of Vater[5]. In some reports, NEC of the extrahepatic biliary tracts was primarily located in the middle to distal bile ducts. Patients underwent surgery in all of the 15 reported cases. The operative procedures were pancreaticoduodenectomy in 13 cases and extra bile duct resection in the remaining 2 cases.
Extrahepatic biliary SCCs have been categorized into two histological types: the pure and mixed types[6]. According to the 2010 WHO classification of NET, mixed adenoneuroendocrine carcinoma (MANEC) was also categorized in the same line as NEC. Previously, NETs have been considered to originate from enterochromaffin or Kulchitsky cells in the crypts of Lieberkühn, which are now believed to be of endodermal origin[7,8]. The biliary tract has a very small number of Kulchitsky cells, which explains the rarity of NETs at this site.
A preoperative diagnosis of NEC of the biliary tract is considered very difficult. In a Japanese report, a regimen of preoperative chemoradiation therapy, curative resection and adjuvant chemotherapy was very effective based on the preoperative pathological diagnosis of NEC of the distal bile duct[9]. However, to our knowledge, such cases are rare. Iwasa et al[10] retrospectively examined the clinical data of twenty-one patients with unresectable or recurrent poorly differentiated NEC arising from the hepatobiliary tract and pancreas and who received combination chemotherapy with cisplatin and etoposide as the first-line treatment. Although no complete responses were obtained, three patients had partial responses, resulting in an overall response rate of 14%. The median progression-free survival was 1.8 mo, and the median overall survival (OS) was 5.8 mo. The prognosis of NEC arising from the hepatobiliary tract remains very poor even with the recent therapeutic approaches.
Patients with biliary NETs have extremely different clinical outcomes according to histopathologic subtypes based on the WHO 2010 classification. In particular, as noted above, the prognosis of biliary NEC has been reported to be very poor. Kim et al[11] reported 20 patients with biliary NET based on a curative resection. Seven of the 20 patients had NEC, and the other seven were diagnosed with MANEC. Six of 7 cases of NEC and all 7 cases of MANEC experienced recurrence, with a median OS of 9.6 and 12.2 mo, respectively. Based on data from the National Cancer Institute’s Surveillance, Epidemiology, and End Results program (1973-2005), Albores-Saavedra et al[4] analyzed the demographics and 10-year relative survival rates of carcinoids and SCCs of the gallbladder and EHBD according to histologic type and stage. There were 31 carcinoid tumors and 17 SCCs of the EHBD. The 10-year survival rate was 80% for carcinoid tumors of the EHBD and 0% for SCC of the EHBD. Almost all patients with SCC in the biliary system died within 1 year after the diagnosis.
In conclusion, NEC arising from the extrahepatic biliary tracts is rare and has a very high malignant potential with a poor prognosis. NEC is difficult to diagnose preoperatively, but it should be considered an uncommon alternative diagnosis. Although treatment strategies have not yet been established, a multidisciplinary approach may improve the prognosis of this highly malignant neoplasm.
COMMENTS
Case characteristics
The patient was a 72-year-old man referred with complaints of jaundice.
Clinical diagnosis
Physical examination showed jaundice.
Differential diagnosis
Primary adenocarcinoma of the extrahepatic bile duct.
Laboratory diagnosis
Laboratory data showed elevated total bilirubin, lactic acid dehydrogenase, alkaline phosphatase,γ-glutamyl transpeptidase, and carbohydrate antigen 19-9.
Imaging diagnosis
Computed tomography showed a tumor in the middle portion of the common bile duct, and the tumor was suspected to have invaded the right hepatic artery and the portal vein.
Treatment
A right hepatectomy combined with extrahepatic bile duct and portal vein resection was performed after percutaneous transhepatic portal vein embolization.
Related reports
The authors found 24 reported cases of neuroendocrine carcinoma (NEC) of the extrahepatic biliary tracts in a PubMed systematic literature search (1985-2015) using the keywords “neuroendocrine carcinoma,” “small cell carcinoma,” and “biliary tract”.
Term explanation
Most extrahepatic bile duct tumors are adenocarcinomas, and biliary neuroendocrine carcinomas represent 0.19% of extrahepatic bile duct tumors.
Experiences and lessons
Although NEC is rare and difficult to diagnose preoperatively, it should be considered an uncommon alternative diagnosis.
Peer-review
The paper provides state-of-the art imaging and methodology and addresses the importance of interdisciplinary approaches.
Footnotes
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
Institutional review board statement: The University of Tsukuba Hospital Institutional Review Board does not require approval for case reports.
Informed consent statement: The patient involved in this case report authorized the disclosure of his protected health information for academic purposes.
Conflict-of-interest statement: All authors indicate that they have no financial interests or potential conflicts of interest to declare.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: March 31, 2016
First decision: May 12, 2016
Article in press: June 13, 2016
P- Reviewer: Boy C, Yoshihiro H S- Editor: Yu J L- Editor: A E- Editor: Wang CH
References
- 1.Bosman FT, Carneiro F, Hruban RH, Theise ND. 4th ed. Lyon: The International Agency for Research on Cancer; 2010. WHO classification of tumours of the digestive system. [Google Scholar]
- 2.Union internationale Contre le cancer. 7th ed. New York, NY: Wiley-Liss; 2009. TNM classification of malignant tumours. [Google Scholar]
- 3.Yasuda T, Imai G, Takemoto M, Yamasaki M, Ishikawa H, Kitano M, Nakai T, Takeyama Y. Carcinoid tumor of the extrahepatic bile duct: report of a case. Clin J Gastroenterol. 2013;6:177–187. doi: 10.1007/s12328-013-0373-2. [DOI] [PubMed] [Google Scholar]
- 4.Albores-Saavedra J, Batich K, Hossain S, Henson DE, Schwartz AM. Carcinoid tumors and small-cell carcinomas of the gallbladder and extrahepatic bile ducts: a comparative study based on 221 cases from the Surveillance, Epidemiology, and End Results Program. Ann Diagn Pathol. 2009;13:378–383. doi: 10.1016/j.anndiagpath.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 5.Kihara Y, Yokomizo H, Urata T, Nagamine M, Hirata T. A case report of primary neuroendocrine carcinoma of the perihilar bile duct. BMC Surg. 2015;15:125. doi: 10.1186/s12893-015-0116-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ikegami T, Kayashima H, Sadanaga N, Morizono S, Nakashima A, Matsuura H, Shirabe K, Maehara Y. Composite small cell and mucinous carcinoma originating from the intrahepatic bile duct: report of a case. Surg Today. 2013;43:194–198. doi: 10.1007/s00595-012-0331-5. [DOI] [PubMed] [Google Scholar]
- 7.Barrón-Rodríguez LP, Manivel JC, Méndez-Sánchez N, Jessurun J. Carcinoid tumor of the common bile duct: evidence for its origin in metaplastic endocrine cells. Am J Gastroenterol. 1991;86:1073–1076. [PubMed] [Google Scholar]
- 8.Takahashi K, Sasaki R, Oshiro Y, Fukunaga K, Oda T, Ohkohchi N. Well-differentiated endocrine carcinoma originating from the bile duct in association with a congenital choledochal cyst. Int Surg. 2012;97:315–320. doi: 10.9738/CC152.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baba M, Furuya K, Koizumi T, Kasai K, Sadaoka K, Sekiya C, Hattori A. [Two cases of neuroendocrine carcinoma in the biliary system with long-term survival] Nihon Shokakibyo Gakkai Zasshi. 2012;109:1598–1607. [PubMed] [Google Scholar]
- 10.Iwasa S, Morizane C, Okusaka T, Ueno H, Ikeda M, Kondo S, Tanaka T, Nakachi K, Mitsunaga S, Kojima Y, et al. Cisplatin and etoposide as first-line chemotherapy for poorly differentiated neuroendocrine carcinoma of the hepatobiliary tract and pancreas. Jpn J Clin Oncol. 2010;40:313–318. doi: 10.1093/jjco/hyp173. [DOI] [PubMed] [Google Scholar]
- 11.Kim J, Lee WJ, Lee SH, Lee KB, Ryu JK, Kim YT, Kim SW, Yoon YB, Hwang JH, Han HS, et al. Clinical features of 20 patients with curatively resected biliary neuroendocrine tumours. Dig Liver Dis. 2011;43:965–970. doi: 10.1016/j.dld.2011.07.010. [DOI] [PubMed] [Google Scholar]


