ePosters – Radiation Therapy
Assessment of interventions to support the first Australian implementation of active patient portal
Alison McSkimming, 1 Deanna Chapman, 1 Natasha Bissell, 1 Deidre Besuijen, 2 David Willis1
1North West Cancer Centre, Tamworth, Australia 2Information Technology, Hunter New England Health, Waratah, Australia
Objectives: Active Patient Portal (APP) gives patients the option of secure on‐line access to their Oncology appointments and personalised healthcare information. Our service implemented APP to provide a unified list of Oncology appointments and to improve access across our large rural catchment area. A subset on Radiation Oncology functionality was piloted to determine an operational approach that fostered patient uptake, while minimising staff workload.
Method: Ongoing monitoring of utilisation rates was conducted using the ARIA Radiation Oncology Information system and APP analytics tools. Patient and staff feedback was thematically analysed. The Vendor and local IT provided support services.
Interventions to improve patient uptake and/or minimise staffing burdens were instituted in response to issues such as low uptake rates. These included developing training resources, adjusting workflows, improving accessibility and building awareness.
Results: Each intervention resulted in a spike in utilisation, but typically with an increase in workload.
The greatest uptake rate resulted from face‐to‐face introductory sessions for patients who were already on treatment. This was initially resource intensive. Video training resources reduced introductory sessions from an average 37.5 to 10 min. Departmental signage increased awareness and demand. Postal invitations prior to treatment commencing resulted in low uptake.
Barriers for patients included IT literacy, preferring traditional communication methods and poor internet availability in some rural areas.
Logistics were the primary barrier to offering APP identified by staff. Technical support requirements were minimal.
Conclusion: Patient uptake of this novel application currently requires resourcing, but simple interventions are improving efficiency.
Evaluating bladder size of prostate patients using kilovoltage imaging
Matthew Oliver, Alan Turner, Richard Oates
Peter MacCallum Cancer Centre, Bendigo, Australia
Objectives: In radiotherapy for prostate cancer, consistent bladder filling reduces bladder toxicities and ensures accurate treatment1. Radiation Therapists (RTs) routinely assess kilovoltage (kV) images for patient positioning, with cone‐beam CT (CBCT) or ultrasound usually required to assess bladder filling, potentially increasing patient radiation exposure. This study assessed the ability of RTs to reliably evaluate bladder filling using kV imaging for patients receiving radiotherapy for prostate cancer.
Methods: Ten RTs reviewed ten anterior kV projections taken from previous patients. Each participant attempted to outline the bladder and rated their ability to visualise the bladder for each image. Participant contours were qualitatively compared to post‐treatment CBCT bladder contours acquired on the same treatment fraction as the kV projections.
Results: Of the 100 image assessments:
47 were assessed as ‘Easy’, and closely matched the CBCT bladder contour.
46 were assessed as ‘Difficult’, and poorly matched the CBCT bladder contour.
Seven were assessed as ‘Unable to visualise’.
The presence of bowel gas and contrast against bony anatomy were described as the main obstacles to accurately visualise the bladder on the kV image.
Conclusion: Kilovoltage imaging cannot replace established methods of pre‐treatment bladder volume measurement. CBCT and ultrasound bladder scanning may enable a more accurate measurement but at a cost of greater time. As kV imaging is part of the daily localisation routine in radiotherapy for prostate cancer, this small study concludes that daily kV imaging could be used for rapid bladder preparation assessment where both radiation therapists are in agreement on the bladder outline.
Reference
1. Jain S, Loblaw DA, Morton GC, Danjoux C, Szumacher E, Chu W, et al. The effect of radiation technique and bladder filling on the acute toxicity of pelvic radiotherapy for localized high risk prostate cancer. Radiotherapy and Oncology 2012; 105: 193–7.
Focal brachytherapy for prostate cancer: a case study
Bing Wei, Andrew See, Yen Tran, Emma Fitzgerald
Epworth Radiation Oncology, East Melbourne, Australia
Purpose: Low Dose Rate (LDR) prostate brachytherapy encompasses the whole gland, where it may be associated with erectile dysfunction, incontinence and rectal toxicity.1 Recently, LDR brachytherapy has been considered for use in a focused manner. This has become feasible owing to more thorough pre‐treatment radiological and pathological assessment that may more aptly identify the dominant lesion.2 The purpose of this case study is to share our experience in the management of the first focal prostate brachytherapy in our department.
Methods: A volume study was performed on a 76‐year‐old gentleman with a recent diagnosis of intermediate risk prostate cancer. A hemi‐gland prostate brachytherapy was performed on an MRI defined nodule to 200 Gy and remaining anterior gland to 145 Gy. A total of 44 seeds were implanted via the transperineal route intraoperatively.
Result: At 2 months the patient is doing clinically well with an early PSA response. The anticipation is that virtually no clinically meaningful dose to both rectum and neurovascular bundle with obviate both rectal toxicity and minimise erectile dysfunction. Other clinical endpoints such as disease control and PSA response remain under active assessment and will be reported in due course.
Conclusion: The aim of focal brachytherapy is to provide effective cancer control for low‐risk disease with reduced genitourinary and rectal side effects. Long term follow up is required to assess late rectal and urethral toxicities. We have successfully managed our first patient on a pilot protocol and will further this initiative in a formalised phase II environment.
References
1. Sylvester JE, Grimm PD, Wong J, Galbreath RW, Merrick G, Blasko JC. Fifteen‐year biochemical relapse‐free survival, cause‐specifi c survival, and overall survival following I(125) prostate brachytherapy in clinically localized prostate cancer: Seattle experience. Int J Radiat Oncol Biol Phys 2011; 81: 376–81.
2. Jain AK, Ennis RD. Focal therapy, differential therapy, and radiation treatment for prostate cancer. Adv Urol. 2012; 2012: 573193.
A regional experience to implement and promote deep inspiration breath hold (DIBH) radiotherapy for the left‐sided breast cancer patients
Kenneth Wan, Jonathan Tomaszewski
Ballarat Austin Radiation Oncology Centre, Austin Health, North Ballarat, Australia
Objectives: Deep inspiration breath hold (DIBH) is an advanced radiotherapy technique to reduce heart and lung toxicity for left‐sided breast cancer treatment but has not been widely available in Australia, particularly in regional areas. The Ballarat‐Austin Radiation Oncology Centre (BAROC) was the first regional site in Victoria to implement DIBH. The goals of the multidisciplinary BAROC DIBH team were: (1) To implement a safe and high quality DIBH program thus reducing cardiac dose for our left‐sided breast cancer patients. (2) To minimise the need for patients to travel out of the region to access cardiac‐sparing radiotherapy.
Methods: A project group was established in early 2014 to systematically develop, implement and evaluate DIBH. Funding was sought to support the project. Public relations strategic planning was undertaken to engage all the key stakeholders for education and promotion of referrals.
Results: DIBH was successfully implemented in April 2015. Since April 2015, 32 patients have been accessed for DIBH suitability. Twenty‐five (78%) patients proceeded to DIBH treatment due to an anticipated reduction in cardiac dose; 20 patients have completed DIBH treatment, and 5 patients are currently receiving treatment or in the planning stage. On average, the mean heart dose has been reduced by over 50%, whilst maintaining equivalent or better target coverage. The left‐ sided breast cancer referrals have increased by 77% since DIBH implementation.
Conclusion: BAROC has established a comprehensive, evidence‐based DIBH program for our patients.
Development and evaluation of psychosocial guidelines for HPV‐positive oropharyngeal cancer patients
Alisha Wintour
Princess Alexandra Hospital, Brisbane, Australia
Objectives: The purpose of this study was to develop evidence‐based guidelines to help this unique subset of patients cope with the dual diagnosis of oropharyngeal cancer along with a sexually transmitted infection.
Methods: A literature search was conducted across a variety of databases, including Science Direct, PubMed and Google Scholar. Keywords used included psychosocial issues, human papilloma virus (HPV), oropharyngeal cancer and HPV positive.
Results: The articles reviewed acknowledged the psychosocial issues that these patients suffer from however they note the lack of research within this area. Initial evidence was gained from literature regarding guidelines used for female HPV‐positive cervical cancer patients to formulate a questionnaire and brochure for males suffering with psychosocial issues upon diagnosis. Clinically it was noted that there was a lack of psychosocial assessment and support available for these patients and that the resources developed would be highly beneficial.
Conclusion: Due to the increased prevalence of this disease it is increasingly important that these psychosocial issues are addressed. This study provides practitioners with the tools and resources to assess and support these patients suffering from the psychosocial issues that are associated with sexually transmitted infections and cancer.
Retrospective analysis of one arm‐up versus two arms‐up for radiotherapy to the breast using variations in couch and gantry positions
Christine Kenny, Livia Chan, Sabeena Beveridge
Ballarat‐Austin Radiation Oncology Centre, Ballarat, Australia
Objectives: To determine whether the two arms‐up set up and the change in breast‐board(BB) gives a more reliable and stable set up resulting in smaller half‐half shifts1.
The one arm‐up technique for treating breast cancer was utilised due to the narrow bore of the CT scanner. In 2012 a wide bore CT scanner became available and the two arms‐up technique was adopted. In 2013 the BB1 was replaced with a new BB2.
Method: The treatment database was interrogated for patients receiving external beam radiotherapy (EBRT) to one side only, from November 2011 to June 2014. Information of the couch long, lateral and vertical and the lateral treatment angle of each daily treatment were extracted and daily differences were calculated.
Results: Analysis of variations from the planned couch and gantry parameters produced a mean and range for each of the three arms of the study (one arm‐up with the old BB, two arms‐up with the old BB and two arms‐up with the new BB).
Table 1: Mean and range of daily couch and gantry variations from those planned for each of the three arms of the study.

Conclusion: The change to two arms‐up and to the new BB has resulted in reduction in the size of the half‐half shift2 adjustments performed when treating breast EBRT. The increase in the couch long variations, however, raises questions about the board indexation.
References
1. PosiboardTM ‐2 Breastboard. Available from: http://www.civco.com/ro/breast‐positioning/breastboards/posiboard2‐breastboard‐109030.htm#productOptions.
2. C‐QualTM Breastboard. Available from: http://www.civco.com/ro/breast‐positioning/breastboards/cqual‐breastboard‐B1.htm#productOptions.
Residual setup error in prostate radiotherapy
Anita Harriman, Timothy Deegan, Scott Jones, Carole Brady, Cathy Hargrave
Radiation Oncology Mater Centre, South Brisbane
Introduction: Accurate delivery of radiotherapy to the prostate is impacted by setup uncertainties including organ motion.1 Image‐guidance can correct for these uncertainties, but residual setup errors (RSE) remain.2 Margins, that include healthy tissue, are used to account for RSE.2,3 Evaluating the sources of RSE is essential when considering the viability of margin reduction.2
Objectives: To determine the magnitude of RSE in prostate cancer patients treated at ROMC. Secondary aims were to correlate RSE to image‐matching time, and to quantify couch motion error as a contributing factor to RSE.
Methods: Data from 38 patients treated for prostate cancer between January 2010 and March 2011 was included in this retrospective study. RSE was calculated by comparing prostate fiducial marker alignment on pre and post‐couch shift orthogonal x‐ray images. Daily phantom‐based quality assurance records from this period were also reviewed to isolate couch based errors.
Results: RSE for the 917 treatment fractions that required couch movements was −0.2 ± 1.27 mm Superior‐Inferior (SI), 0.0 ± 0.74 mm Left‐Right (LR), and −0.3 ± 1.2 mm Anterior‐Posterior (AP). The image‐guidance process became more efficient over time, but the magnitude of RSE did not correlate with image‐matching time. Couch movement errors of 0.0 ± 0.5 mm SI, 0.1 ± 0.6 mm LR and −0.7 ± 0.6 mm AP were recorded during daily quality assurance.
Conclusion: While couch movement and intrafraction motion both contribute to RSE, intrafraction motion showed greater variation. Potential reduction of RSE by real‐time correction for intrafraction motion, and increased mechanical accuracy may enable reduction of margins in the future.
References
1. Létourneau D, Martinez AA, Lockman D, Yan D, Vargas C, Ivaldi G, et al. Assessment Of Residual Error For Online Cone‐Beam CT‐Guided Treatment Of Prostate Cancer Patients. Int J Radiat Oncol Biol Phys. 2005; 62: 1239–46. doi:10.1016/J.Ijrobp.2005.03.035.
2. Poulsen PR, Muren LP, Høyer M. Residual Set‐Up Errors And Margins In On‐Line Image‐Guided Prostate Localization In Radiotherapy. Radiother Oncol. 2007; 85: 201–6. doi:10.1016/J.Radonc.2007.08.006.
3. Mayyas E, Chetty IJ, Chetvertkov M, Wen N, Neicu T, Nurushev T, et al. Evaluation Of Multiple Image‐Based Modalities For Image‐Guided Radiation Therapy (IGRT) Of Prostate Carcinoma: A Prospective Study. Med Phys. 2013; 40: 041707–1 – 041707–9. doi:10.1118/1.4794502.
Woah! What is that?! A case study on an asymptomatic, grossly distended bladder in a prostate cancer patient
Hana Grigg, Kylie Robbie
Townsville Cancer Centre, Townville, Australia
At the Townsville Cancer Centre (TCC), approximately 100 prostate cancer patients are treated per year. Emphasis is placed on consistency and reproducibility throughout radiation treatment, with a full bladder, empty rectum protocol used to facilitate this during External Beam Radiation Therapy (EBRT).
This case study investigates the presentation of a prostate cancer patient with an asymptomatic distended bladder, discovered at radiation therapy simulation. The bladder volume noted on planning scan was over 9000 mL. The patient described recent sensation of abdominal distension since hormone treatment but no discomfort. Urinary habits were unremarkable; stream was acceptable with nil urgency or hesitancy and normal volumes being passed. The patient did experience some nocturia‐ approximately 4–5 times a night, but this was neither unusual nor distressing.
The patient's Estimated Glomerular Filtration Rate (eGFR), which measures kidney function, was at Stage 4, pending Stage 5 potentially resulting in kidney failure.1 Within less than 24 h the patient was catheterised and 11,070 mL of urine was drained from the bladder. Based on a literature search, this was the largest bladder size to date.
One month follow‐up has shown improved eGFR, creatine levels and successful management of the catheter. EBRT has been delayed until the bladder size is managed, with prostate cancer controlled by hormones. The patient will be re‐simulated for normal bladder parameters.
Radiation therapy has seen more and more image‐guided processes emerging to improve accuracy and treatment procedures. Considerations of these image‐guided technologies, particularly bladder scanning, may have been valuable in this case.
Reference
1. The National Kidney Foundation. Glomerular Filtration Rate (GFR) [Internet]. 2015 [cited 7 September 2015]. Available from: https://www.kidney.org/atoz/content/gfr.
A case study utilising the clinical practice improvement methodology to reduce simulation cancellations for breast patients
Vanathy Manivasahan
Crown Princess Mary Cancer Centre, North Rocks, Australia
In NSW, the Clinical Excellence Commission provides Clinical Practice Improvement (CPI) training to frontline healthcare workers with the intentions of improving quality of care and patient outcomes. The CPI methodology provides a framework which incorporates a diagnostic phase to identify the problem that is causing inefficiencies and design a solution to improve the outcome. This poster will highlight how the CPI methodology was utilised at the Crown Princess Mary Cancer Centre, Westmead hospital to reduce the number of cancellations for simulation appointments for breast cancer patients. The current cancellation rate ranged from 10% to 22% each month leading to a wastage of health care resources and creating unnecessary inconvenience and anxiety to the patient and carer.
A multidisciplinary team was established to undertake the project. The aim statement, developed in the diagnostic phase of the model was to reduce the cancellation rate of Breast cancer simulation appointments by 50% from the previous 12 months over a 6 month period. Various quality improvement tools and techniques were used to establish the causes and potential solutions to the problem. The Pareto principal which states that ‘80% of the trouble comes from 20% of the problem’, was utilised to identify communication to be the process that needed improvement in order to achieve the project aim. A potential solution was implemented in an attempt to improve the communication process. Preliminary results will be presented in this poster to show if the CPI was found to be effective in reaching the project aim.
Initial experiences of hippocampal avoidance whole brain radiation therapy (HA‐WBRT) at an Australian cancer care centre.
Rhys Fitzgerald, Melissa Tonks, Josh Runham, Peter Gorayski
Radiation Oncology Centres, Springfield, Australia
Objectives: Hippocampal avoidance whole brain radiation therapy (HA‐WBRT) is a novel radiation therapy delivery technique used to mitigate neurocognitive impairment for those patients receiving whole brain radiation therapy. To help improve the quality of life for patients following treatment, this technique was investigated for implementation in our institution.
Methods: Doses to planning target volume (PTV) and organ at risk were adopted from the Radiation Therapy Oncology Group (RTOG) protocol 0933. A literature search identified that for linear accelerator based treatments, either intensity modulated radiation therapy (IMRT) or volumetric modulated arc therapy (VMAT) is essential to achieve the dose gradients required to achieve hippocampal avoidance.1,2 Due to treatment time reductions associated with VMAT, IMRT was removed from the investigation.
Results: A two full arc technique which had specifically designed fixed jaws, allowing preferential hippocampal sparing best adhered to the RTOG protocol objectives.
Conclusions: HA‐WBRT safely and effectively implemented in our institution adhering to RTOG 0933 guidelines.
References
1. Shen, J., et al., An efficient Volumetric Arc Therapy treatment planning approach for hippocampal‐avoidance whole‐brain radiation therapy (HA‐WBRT). Medical Dosimetry, 2015; 40: 205–9.
2. Lee, K., N. Lenards, and J. Holson, Whole‐brain hippocampal sparing radiation therapy: Volume‐modulated arc therapy vs intensity‐modulated radiation therapy case study. Medical Dosimetry.
Intraoperative radiotherapy devices comparison
Sarah Schmeider
Peter MacCallum Cancer Centre, Elwood, Australia
Objective: Intra Operative Radiation Therapy (IORT) is becoming utilised more for breast radiotherapy based on the publication of recent randomised trials demonstrating its efficacy. It is a convenient form of partial breast radiotherapy as treatments can be delivered in 1 (or few) treatments, in some cases at the time of the primary breast surgery. In addition, IORT's concentrated dose has been reported in some cases to result in less toxicities which increases their QoL. The objective of this poster is to compare the IORT devices available for clinical use, how their capabilities differ and the supporting evidence.
Methods: With the use of technical data, machine capabilities and journal articles a comparison table of the range of IORT machines has been constructed. Aspects such as the treatment time, the size and ease of access of the machine, the shielding requirements, treatment sites capabilities, energys, applicator sizes, reusable/disposable applicators have been included in the analysis. Supporting clinical evidence for each device has been included.
Results: The devices included in this analysis are Intrabeam, Xoft, Novac & Mobetron (both Linac electrons) Mammosite (Iridium‐92). Comparison of devices and the clinical trials involved, including the pros and cons for the use of this device, quick overview of the trials and their outcomes.
Conclusion: This analysis provides clinicians with an overview of the range of IORT devices available, the pros and cons of each one. This information would aid selection of the most appropriate device for the specific needs of any radiation oncology department.
Is Rectum/Bladder ‐ PTV overlap a predictive factor in achieving VMAT prostate dose constraints?
Menglei Chao, Natalie Coburn, Rachael Beldham‐Collins, Kevin Van Tilburg
Nepean Cancer Care Centre, Kingswood, Australia
Objective: Generic dose‐volume constraints of the Rectum/Bladder (R/B) are used in planning to reduce doses to these organs in prostate cancer. A retrospective study was undertaken to assess possible correlations between the overlap of the R/B with the Planning Target Volume (PTV) and the dose received during planning to these Organs At Risk (OAR). We also aim to establish a predictive model to identify the cases that might exceed R/B dose limits prior to optimization.
Method: The data for 65 prostate cancer patients who had VMAT treatment to the intact prostate and proximal seminal vesicles at Nepean Cancer Care Centre from 2012 to 2014 were analysed. R/B volume, R/B‐PTV overlapping volume, percentage overlapping volume and R/B VMAT planning objectives were collected. An identical prescription of 78 Gy/39# was delivered. Statistical methods were undertaken to assess the significance of the collated data.
Results: The percentage overlap between R/B and the PTV were highly correlated to dose constraints of relevant critical organs, with R2 = 0.62 for rectum V75 Gy and R2 = 0.9 for bladder V70 Gy. The predictive cutoff value for RV75 Gy > 10% and BV70 Gy > 15% were 10.14% (sensitivity 83%, specificity 84%) and 7.95% (sensitivity 96%, specificity 93%) respectively.
Conclusions: R/B‐PTV percentage overlap has a high reliability in estimating sparing of R/B. This prediction model can be used to improve planning efficiency and assess the need of extra organ‐sparing interventions.
Modified Styro‐former: An improvement in quality assurance check and accuracy of electron plaques
Sok Yee Phang, Wan Wei Tan, Allan Lingan Santos
National Cancer Center Singapore, 11 Hospital Drive, Singapore
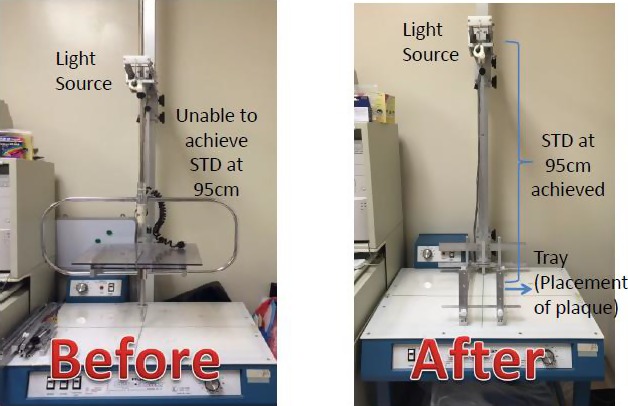
Purpose/Objective: Improve the quality assurance process and verification method of the electron plaque using modified styro‐former device. It aims to increase the accuracy of electron treatment by detecting human error and improve the current workflow.
Materials and Methods: 50 of irregular shapes of electron plaques of 3D electron cases were fabricated. These electron plaques consisted different applicator sizes from the range of 6 × 6 to 15 × 15. All fabricated electron plaques were verified using both the modified innovated styro‐former device and LINAC. Differences were all recorded and analysed using Eclipse planning system and verified by Radiation Oncologist.
Results: 24 electron plaques were found to be no difference from plan; 18 electron plaques were less than or equal to 2 mm translational shift; 2 electron plaques were less than 1.3 degree rotational shifts; and 6 electron plaques were less than 2 degree of rotational shifts with translational shift of less than 2 mm. The differences were compared to the original treatment plan, dose coverage was adequate without compromising to the PTV(Planning Target Volume). The P‐value of the conformity index (CI) was insignificant.
Conclusions: The results of this study concluded that the modified styro‐former device (figure 1) is able to ensure good quality assurance of the electron plaques, detect errors and minimize radiation incidents, and improve workflow efficiency.
Figure 1. Modified Styfrofoam Cutter E‐PLAQUE QA DEVICE
An overview of patient specific heart constraints for the optimisation of Simultaneous Integrated Breast Boost plans
Rachel Ward, Drew Latty, Dan Jia, Kirsty Stuart
Crown Princess Mary Cancer Centre, Westmead, Australia
Objectives: Simultaneously integrated boosts (SIB) have shown to be as effective as traditional boosting methods in breast cancer radiation therapy. With the greater complexity of SIB plans it becomes more difficult to assess the contribution of dose to the heart from non‐tangential fields. In July 2014, CPMCC introduced patient specific heart tolerances based on the lowest achievable mean heart dose from tangential fields. This study will analyse the plan characteristics of SIB plans generated from standard dosimetric constraints and from patient specific heart constraints (PSHC).
Methods: 267 breast cancer patients planned with SIB, treated between July 2013‐June 2015 were audited. Planning constraints; beam arrangement; heart, lung and left anterior descending coronary artery doses; RTOG conformity index and homogeneity index were evaluated.
Results: All evaluated planning characteristics were comparable excluding mean heart dose. For patients planned using standard dosimetric constraints, the average mean heart dose was 3.9 Gy for left‐sided patients and 1.1 Gy for right sided patient, of which 28.5% and 48% of the dose could be attributed to the SIB fields respectively. For patients planned using PSHC, the average mean heart dose was 2.6 Gy for left‐sided patients and 0.7 Gy for right sided patients, of which 10% and 16% of the dose could be attributed to the SIB fields respectively.
Conclusion: Patient specific heart tolerances show promise in assisting the optimisation of simultaneously integrated breast boost plans, further prospective evaluation of PSHC and beam arrangements could assist in the transition between traditional planning methods and knowledge based planning.
The implementation of soft tissue matching for photon boosts to the breast
Nicola Holt, Kathryn Clarke
Genesis Cancer Care, Crows Nest, Australia
Objectives: The addition of a boost treating the tumour bed following radiotherapy to the whole breast is a widely accepted treatment regime.1 Although electrons are the most common method for treating boosts, the location and depth of the tumour bed may require the use of a photon technique2. Changes in anatomy suggest that soft tissue matching to the breast contour is the preferred image matching technique.3 The introduction of this technique at Genesis Cancer Care's Mater department has required additional training for staff. An in‐house investigation was conducted to determine the difference between soft tissue and bony matching for breast boosts and the effect they have on isocentre placement.
Methods: 10 patients receiving photon boosts to their tumour bed were included in the investigation. Treatment staff first performed a bony match, followed by a soft tissue match, and recorded the discrepancy between the matches. An average of the patient's daily corrective moves was calculated and the data analysed.
Results: The data collected suggested that there can be significant differences in breast size and contour between initial simulation and boost treatments. In these cases there were significant discrepancies between the bony and soft tissue matches.
Conclusion: For most patients there were few inconsistencies between bony and soft tissue matching. However, for patients who demonstrated significant changes in breast size or contour, the isocentre placement could be dramatically affected if staff incorrectly matched to the bone. This outlined the importance of staff training to ensure the tumour bed received the prescribed dose.
References
1. Sainsbury, J., Anderson, T. and Morgan, D. Breast Cancer‐ ABC of Breast Disease. (2000) The British Medical Journal 325 (745)
2. Poortmans, P., Bartelink, H. & Pierart, M. The influence of the boost technique on local control in breast conserving treatment in the EORTC ‘boost versus no boost’ randomised trial. (2004) Radiotherapy and Oncology 72 (1) pp 25‐33
3. Benda, R., Yasuda, G., Sethi, A., Gabram, S., Hinerman, R. & Mendenhall, N. (2003) Breast Boost: Are we missing the target? Oncology and Radiotherapy 97 (4) pp905‐909.
Deep inspiration breath hold versus free breathing in left breast radiotherapy
Reuben Patrick Estoesta, Lani Fingleton, Diana Naehrig, Elizabeth Claridge‐Mackonis, Darren Martin, Melissa Pham, Joanne Toohey, Susan Carroll
Chris O'Brien's Lifehouse, Camperdown, Australia
Objectives: Radiotherapy for left‐sided breast cancer can result in significant dose to heart and left anterior descending artery (LAD). There is a dose‐response relationship between the risk of cardiac toxicities and radiation dose. This study compares the dosimetry of a newly introduced deep inspiration breath hold (DIBH) technique and the standard free breathing (FB) technique.
Methods: Twenty patients with left‐sided breast cancer underwent computed tomography (CT) simulation in FB and DIBH. The FB scan was analysed to see if the patient would benefit from the DIBH by assessing the heart's location in terms of the posterior edge of the PTV. A dosimetric comparison was made between the two techniques and treatment set‐up was verified using electronic portal imaging device (EPID) images.
Results: Compared with FB, DIBH resulted in statistically significant reduction in heart mean dose (1.63 Gy vs. 3.62 Gy), maximum dose (33.61 Gy vs. 45.76 Gy), V30 (0.24% vs. 3.67%) and V20 (0.46% vs. 4.88%). These results were reflected in the LAD mean dose (5.92 Gy vs. 20.63 Gy), maximum dose (22.46 Gy vs. 41.54 Gy) and V30 (1.66% vs. 38.16%). The left lung volume was larger in the DIBH sample (1845.52 cc vs. 1156.33 cc). EPID verification showed a variation of 1 mm from the planned position.
Conclusion: Overall the results of these measurements indicate that DIBH is an effective technique at reducing the dose to the cardiac structures compared to FB and based on EPID imaging DIBH was reproducible on treatment. Further research is required to determine the accuracy and reproducibility of using this DIBH technique during treatment.
Patient education video on radiotherapy headrest and shell fabrication
Wan Wei Tan, Sze Yarn Sin, Estella Au, Sok Yee Phang, Allan Santos, Abdul Shahid Zakaria
National Cancer Centre Singapore, Singapore, Singapore
Purpose:
To alleviate the anxiety of patients by improving their understanding in the headrest and shell fabrication procedure
To reduce the briefing time by the radiation therapist
Methodology: 40 patients who underwent headrest and shell fabrication procedure were selected and categorized into 2 groups: (1) 20 patients who received video briefing; (2) 20 patients who received verbal briefing. These patients were given a survey form at the end of the procedure to provide a feedback on the anxiety level and understanding towards the procedure. The data was then collated and analyzed.
Results: 50% of the patients who underwent video briefing reported decrease in anxiety after watching the video. 90% of them found the video very helpful while the remaining found it moderately helpful in understanding the procedure. As for the patients who underwent verbal briefing, 80% of them reported that there was no difference with the briefing in helping with their anxiety. The briefing time, however, on average increased by 1 minute.
Conclusion: Patients generally preferred video briefing as it improved their understanding towards the headrest and shell fabrication procedure despite the longer briefing time. Hence, it helped to reduce their anxiety level on an unfamiliar process.
Evaluating bladder filling protocols at Townsville Cancer Centre (TCC)
Amanda Patterson, Matthew Fairbairn
Townsville Health and Hospital Service, Townsville, Australia
Objectives: A consistent, reproducible bladder volume is paramount in radiotherapy treatment of prostate cancer. Bladder filling protocols aim to reproduce bladder volumes. This retrospective study evaluated daily treatment images to determine if the current bladder filling protocol at Townsville Cancer Centre (TCC) results in consistent bladder volumes in prostate cancer patients.
Methods: We evaluated two groups of prostate cancer patients: Group 1 (n = 20) received treatment prior to bladder protocol implementation; and Group 2 (n = 20) received treatment after implementation. Bladder volumes were contoured on all available (4–8) conebeam CT (CBCT) images for group 1 and 10 randomly selected images from each patient's treatment course for group 2. These contours were audited prior to comparison with the planning CT bladder volumes. Independent samples t‐test was performed to compare the mean bladder volume differences in cubic centimetres (cc) between group 1 and 2 using the statistical package SPSS.
Results: The mean bladder volume differences (+/− cc) were 30.41 and 23.29 for group 1 and 2 respectively, which were not significantly different (P = 0.154). However, Group 2 demonstrated a lower standard deviation (SD) in absolute bladder volume (SD = 67.5 cc) compared to group 1 (SD = 118.8 cc).
Conclusion: The data does not show statistical significance between the groups, but the differences in standard deviation are clinically relevant. Patients consuming the standardised volume of water had less variation between planning and treatment volumes, favouring the current bladder filling protocol. This will lead to further investigation into existing and emerging technologies such as bladder scanners.
ePosters – Medical Imaging
Effectiveness of core clinical skills training in first year Medical Imaging Students
Therese Gunn, Kelly Wilson‐Stewart, Vicki Braithwaite
QUT, Brisbane, Australia
Introduction: Teaching clinical skills to preclinical healthcare students effectively can be challenging, and the transition from the university setting to the clinical environment can be stressful1.
To enhance preclinical skills training, Queensland University of Technology (QUT) provides multiple blended learning options to work in synchronicity with more traditional theoretical components.
Objectives: To evaluate the perceived usefulness of the preclinical blended learning techniques offered to students prior to prepare them for their first clinical placement.
Methods: Students were surveyed following their first two week clinical block to assess the usefulness of each of the educational tools offered. The usefulness of the following teaching methods were assessed;Interactive tutorialsX‐raying disarticulated phantoms in the simulation laboratoryRoleplay in the simulation laboratoryVirtual positioning softwareSelf‐directed learning/reflection
Students were also asked to indicate their confidence of topics covered in the interactive tutorials such as, interpreting request forms, communication skills, familiarity with medical terminology and imaging series.
Results: Predominantly students felt that most of teaching tools available prior to their placement were effective in preparing them for patient contact within a clinical environment. 81% of students (n = 32) indicated that they either agreed or strongly agreed that their prior knowledge of technical skills and competency in communication skills prepared them well for clinical placement
Conclusion: The methods used to teach preclinical skills to Medical Imaging students at QUT have been successful in preparing students for their first clinical placement.
Reference
1. Swamy, M., et al., Role of SimMan in teaching clinical skills to preclinical medical students. BMC Medical Education, 2013. 13: 20–20.
Radiation regulatory compliance and accreditation
Vivien Munoz‐Ferrada
Gammasonics Institute, Drummoyne NSW, Australia
In today's world the regulatory requirements are increasing from both State and Federal Governments and compliance mandatory. State regulators are reducing responsibility with the onus more on the possession licensee. What you need to know and have prepared in the event of an onsite audit by a regulatory body. How the Federal Codes of Practice interface with your Management licence and Use Licence and DIAS Accreditation.
What are the legal implications of non compliance with the mandatory regulations. Most owners of ionising equipment want to comply with the various legislations but often do not know how. It is increasingly difficult to find out how to comply and how to know what is the right advice. The design layout of x‐ray rooms for shielding can be such that lead requirements are minimised without minimising safety. This presentation covers all aspects of regulatory compliance.
CT reverse flash – an alternative for imaging type A aortic Dissections.
Anthony Barnes
Radiology Department Princess Alexandra Hospital, Birkdale, Australia
Objectives: To provide an alternative imaging method to conventional cardiac gating for type A Aortic Dissections using a Siemens Definition Flash Scanner.
Background: Imaging the ascending aorta has historically necessitated the use of cardiac gating and helical acquisition in multiple cardiac phases to minimise motion in this area with significant radiation dose, examination time, difficulty and motion artefact. This technique provides a simpler alternative with reproducible and reliable results.
Methods: Using a Siemens dual source Flash scanner a simplified scan technique has been developed to image the aortic root using Flash mode with bolus tracking on the femoral artery and reversing scan direction to minimise motion artefact around the aortic root whilst maintaining even contrast enhancement throughout the entire scan. Conventional scan direction is superior to inferior. Cardiac motion is minimised by sub second scan acquisition. Radiation dose is also minimised by not requiring helical acquisition of image in various cardiac phases. A limitation of this technique is that the maximum FOV is limited to 330 mm at the maximum pitch.
Results: We have been using this method as a protocol successfully within our department for 2 years on patients who meet the mandatory size criteria.
Conclusion: This robust technique has improved patient throughput for this examination type whilst minimising radiation dose and cardiac motion. It is a very reliable and reproducible scan technique with excellent patient outcomes.
Improving Podiatry students’ clinical reasoning when requesting x‐rays: An interdisciplinary approach using multimedia tools
Kelly Wilson‐Stewart
Queensland University of Technology, Brisbane, Australia
Objectives: Under Medicare, podiatrists are able to request funded plain x‐ray images of the foot and ankle. Within undergraduate podiatry education, students should be made aware of the potential risks associated with the use of ionising radiation, and the importance of adhering to the ALARA (As Low As Reasonably Achievable) principle.
The aim of this study was to assess the effectiveness of using a clinical case study format to improve podiatry students’ clinical reasoning skills when requesting x‐rays. It is envisaged that enhanced clinical judgement of graduates will lead to more appropriate utilisation of diagnostic imaging requests by podiatrists.
Methods: An interactive multimedia story was developed by a Medical Imaging lecturer to highlight the appropriate clinical pathways that students should consider when assessing a patient. The willing third year podiatry students were randomly divided into a test (n = 20) and control group (n = 20). The test group were given access to the branching story tutorial supplementary to the resources available to the control group. A formative quiz was released to both groups to quantitatively determine whether the student understanding in the test group was enhanced. A qualitative survey was also distributed.
Results: The results demonstrate that the group with access to the tutorials performed better on the formative quiz than the control group. All qualitative responses regarding the interactive tutorial were positive.
Conclusion: Both quantitative and qualitative evidence indicates that students demonstrated improved clinical judgement when determining the most appropriate diagnostic imaging requests. This teaching method should be continued in the future.
Dual energy CT and gout
Jessica Williams
Princess Alexander Hospital, Brisbane, Australia
Gout is the most common crystal deposition arthropathy and results from the precipitation of monosodium urate crystals within joints2. The incidence of gout has tripled over recent decades, and in order to successfully meet the challenge of this surge in disease burden, providers are required to correctly diagnose and distinguish gout from other forms of joint disease4. Currently, definitive diagnosis of gout requires identification of monosodium urate crystals in synovial fluid aspirates from the involved joint3,4. Dual‐Energy Computed Tomography (DECT) is a promising new imaging technique which many be clinically relevant in the diagnosis and management of Gout. The aim of this poster is to describe the basic technique of DECT and indentify the role of DECT in diagnosing gout. Case studies in which the diagnosis of gout was made or excluded on the basis of dual‐energy CT will be discussed. These cases studies highlight the utility of dual‐energy CT as a problem solving tool in identifying the presence of monosodium urate crystals and in confirming or excluding gout in clinically challenging cases. In patients with known gout, DECT may be used to provide sensitive and specific volumetric quantification of subclinical tophi and evaluate response to treatment1. A prompt diagnosis of gout could avert associated long‐term complications, thereby reducing disease burden and improving overall quality of life. Therefore, DECT promise to be a unique and clinically relevant modality in the diagnosis and management of gout2.
References
1. Madhura A,Desai et al. (2011). Clinical Utillity of Dual‐Energy CT for Evaluation of Tophaceous Gout. Radiographics. 31 (1), 1365‐1375.
2. Nicolaou, Savvakis et al. (2010). Dual‐Energy CT as a Potential New Diagnostic Tool in the Management of Gout in the Acute Setting. AJR. 194 (1), 1072‐1078
3. Glazebrook, Katrina et al. (2011). Identification of Intraarticular and Periarticular Uric Acid Crystals with Dual‐Energy CT: Initial Evaluation. Radiology. 261 (2), 516‐524.
4. Bongartz, Tim et al. (2014). Dual‐energy CT for the diagnosis of gout and accuracy and diagnostic yield study. ARD. (0), 1‐6.
Rural and remote ‐ a shining opportunity
Judi Klontz, 1 Christopher Dransfield, 2 Delphi Manietta
1Queensland Country Practice, Brisbane, Australia2Medical Imaging ‐ Kempsey Hospital, Kempsey, Australia
The Rural and Remote Practitioners Panel (RRPAP) would like to demonstrate to all radiographers their passion for living outside metropolitan areas. By introducing the panel and its members, the AIR community will have a better understanding of the conditions involved working within rural practice in its many forms throughout the various states of Australia.
The RRPAP is responsible for evaluating applications for various monetary scholarships and will touch on these briefly. These scholarships are available to practitioners within the rural and remote communities.
Is it dislocated? Challenges of rural radiography
Judi Klontz, 1 Amy Brackenrig2
1Queensland Country Practice, Brisbane, Australia2Bundaberg Hospital, Bundaberg, Australia
Often rural and remote locations do not have the luxury of a radiologist to give hot reporting on plain film xray examinations. It is often left to the skill of the radiographer to provide optimal images for the attending physician to provide the best patient care. In many instances, the sole practitioner must rise up and guide an inexperienced junior doctor through the image interpretation process. This case study of a questionable dislocated shoulder emphasizes that plain film imaging done correctly may assist in providing the answers to the doctors query.
TB in the New World
Annette Peters, 1 Raenor Priest2
1Princess Alexandra Hospital, Brisbane, Australia2MIA Radiology, Lilydale, Victoria, Australia
Case Studies of pulmonary tuberculosis and review ‐ A Pictorial Essay: Background: There is a perception that TB is on the increase worldwide, the so called ‘TB epidemic’. In fact, there has been a 47% decline in TB mortality rate since 1990.1 Despite advanced treatment and the fact that nearly all cases can be cured, TB remains one of the World's biggest threats.2
Aetiology: Mycobacterium Tuberculosis ‐ are Parasites of the pulmonary macrophage. TB can also affect other body parts such as brain, bones and kidneys. In most cases the macrophages remain contained at the site of infection, as a result, a primary granulomatous lesion develops. The healing can be seen as scaring and calcium deposits giving the typical appearances seen on a chest X‐ray and forms part of the diagnosis TB.
Aim: The aim is to discuss the radiographic presentation associated with TB. The case studies are collected from Princess Alexandra Hospital in Brisbane, at the TB clinic with cross referencing with Images from ‘IMPAX’. The Images will be chosen from different age groups and genders, and will include images from some high risk groups in order to demonstrate the different appearances of TB on the chest X‐ray. The chest X‐ray is a crucial part of the diagnosis of TB.
References
1. Global tuberculosis Report 2015 20th Edition
World Health Organisation Http://www.who.int/tb/publications/global_report/gtbr15_main_text.pdf?ua=1
2. Tuberculosis management, prevention and control of tuberculosis: Guidelines for health care providers 2002‐2005 http://ideas.health.vic.gov.au/diseases/tuberculosis‐management‐guide.asp
3D printing in cardiovascular disease
Zhonghua Sun, Andrew Squelch
Curtin University, Perth, Australia
Objectives: In recent years, 3D printing technology has been increasingly used in the medical field, with research showing potential in assisting diagnostic evaluation of cardiovascular disease. This study demonstrates the current research applications of 3D printing in cardiovascular disease.
Methods: 3D printed models of two common cardiovascular disease including aortic dissection, and abdominal aortic aneurysms were manufactured based on CT angiographic images. 2D and 3D image processing steps for image post‐processing and segmentation were briefly described. Comparison of dimensional measurements between the 3D printed models and CT data was performed to determine the accuracy of the 3D printed models.
Results: 3D printed models of aortic dissection and aneurysm were successfully generated. The models were evaluated with measurement of certain anatomical structures of the model comparable to the data from CT angiography. Complex anatomical structures such as aortic dissection in relation to the arterial branches, and aortic aneurysm relative to the extent involving aortic branches were clearly visualised and assessed on the 3D printed models.
Conclusion: 3D printing is an emerging and promising technique with clinical applications showing potential in improvement of understanding of complex anatomy in cardiovascular disease, thus achieving the goal of assisting clinicians more accurately manage patients prior to surgical treatment.
Synchrotron tomography imaging of aortic stent graft: an early report of an in vitro phantom study
Zhonghua Sun, Curtise CK Ng
Curtin University, Perth, Australia
Objective: The study objective was to demonstrate the superiority of synchrotron tomography over conventional CT for imaging aortic stent graft structures.
Methods: A human aorta phantom consisting of normal aortic branches, aortic aneurysm and a stent graft with suprarenal component placed in situ was used in the experiment. The synchrotron tomography with a range of monochromatic x‐ray energies ranging from 40 to 100 keV and a beam size of 40 × 45 mm2 was used in scanning the phantom. The phantom was rotated to acquire projection images for tomographic reconstruction with one projection taken every 0.1° for a total sample rotation of 180°, giving 1800 projections per scan (Fig. 1). Images were recorded by detectors with a field of view of 70 × 20 mm2 and 19.88 μm pixel size. The phantom was also scanned by a 64‐slice CT scanner for image comparison.
Fig. 1. Phantom (with stent graft) set up for synchrotron tomography imaging.

Results: The metal wires and suprarenal stent struts of aortic stent graft were clearly visualized in synchrotron tomographic images and fine details were demonstrated. Streaking artifacts arising from the suprarenal stent struts were less apparent when images were acquired with higher keV in comparison to those obtained with lower keV (Fig. 2). The diameter of stent wires was less magnified on synchrotron tomography when compared to conventional CT, which is associated with overestimation of stent wire thickness (Fig. 3).
Fig. 2. Synchrotron tomography imaging of suprarenal stent wires. Streaking artifacts are apparent when scans were performed with 40 and 60 KeV but less obvious with the increase of keV. SMA stands for superior mesenteric artery.

Fig. 3. CT images acquired with 64‐slice CT scanner show suprarenal stent wires crossing the superior mesenteric artery (arrows), with wire thickness much thickness than the actual diameter.

Conclusion: This early report shows the feasibility of high resolution 2D synchrotron tomography for better delineation of stent graft details. Further studies on 3D visualisation of stent graft details would be warranted.
MDCT abdominal imaging under AEC systems: the effects of patient size classification using cross‐sectional area on diagnostic reference levels
Myeongsoo Kim, Kelly Spuur, Xiaoming Zheng
Charles Sturt Univeristy, Wagga Wagga, Australia
Objectives: To investigate potential dose reduction in abdominal MDCT using AEC systems according to different classification metrics of patient sizes; cross‐sectional area (CSA), body mass index (BMI), and body weight.
Methods: Images of 107 patients who underwent abdominal CT examinations at Seoul National University Hospital using a GE Discovery™ 750HD (w/FBP) 64‐slice MDCT scanner were reviewed. The CSA was measured at the level of the common hepatic vein in the liver and was calculated using the average of two dimensions; BMI and body weight were obtained prior to scanning. Assessment was performed by a comparison of a volume CT dose index (CTDIvol) at the 75% and 50% level of dose distribution of collected data in terms of diagnostic reference levels (DRLs).
Results: The minimum and maximum CSA values were 335 cm2 and 921 cm2, and demonstrated a good correlation coefficient of 0.912. The correlation coefficient of BMI and weight were 0.791 and 0.854 (P < 0.01). Reference doses at the 75% level of dose distribution according to CSA and body weight were 11.2 mGy and 11.64 mGy in the average habitus group. The achievable doses at the 50% level were 9.46 mGy and 9.79 mGy. The dose variation from the 75% to 50% level in the CSA showed a CTDIvol decrease of 21% (small habitus) and 4% (large habitus).
Conclusion: CT scanning with AEC systems is fundamentally reliant on the correct classification of patient size for dose minimisation. The CSA classification should be the superior choice for dose reduction in terms of DRLs.
Figure 1: CSA, cross‐sectional area (cm2) measurement: calculated using the horizontal and vertical diameter (mm) at the level of origin of the intrahepatic portal vein.
CT Scanning Techniques of Wrist Joints
Naomi Nugent
Queensland Health, Gympie, Australia
There is a large array of CT scanners currently operational in the public and private sectors. Scanning the entire wrist joint in one axial rotation is preferable, however most scanners in practice will need to scan the joint helically.
When scanning helically, a number of factors must be considered:
Principle of Obliquity
Focal Spot Size
Splay Artifacts
Radiation Dose
1. Principles of Obliquity: Positioning of the wrist in an oblique position across the scan plan to increase the number of slices through the joint, and therefore increasing the sampling data across the joint. This also reduces metal artifacts.
2. Focal Spot Size: Reducing the focal spot to the smallest available setting improves resolution/detail.
3. Splay Artifacts: Occurs when there is a z‐axis sampling error. The severity of the artifact depends on the magnitude of the high contrast transitions. This increases with slice width, pitch and detector rows.
4. Radiation Dose: The radiation dose commonly required for wrist scanning is very low. However, when there is metal fixation present, a small increase in radiation dose will counteract the beam hardening artifacts, thereby improving image quality.
Once the data is obtained, the information should be reconstructed in a minimum of 3 planes (Axial, Coronal and Sagittal).
With the correct settings and knowledge of the equipment, CT scanning of the wrist can be improved while keeping radiation dose to a minimum.
A different kind of rock
Megan Flynn
QLD Health, Brisbane, Australia
Since 1977 when Andreas Gruentzig performed the first percutaneous transluminal coronary angioplasty (PTCA) using a balloon catheter in Zurich many advances in the Cardiac Catheter laboratory have evolved. Initially PTCA was limited to certain disease types however nowadays with technology, equipment and skills advancing more complicated disease can be targeted with significant success rate. One interventional device that makes this possible is The Rotablator.
The Rotablator is a drill powered by compressed air, made out of tiny diamond pieces. This debulking device is used prior to angioplasty allowing for treatment with stents and balloons to be made possible. It provides high‐speed rotational atherectomy on severe and inelastic plaque. It is able to differentiate between hard plaque and healthy tissues so not to damage normal arterial wall. The purpose of the device is to remove calcification in the coronary arteries by breaking it down into microparticles smaller than red blood cells, which can then be removed by the body.
Due to the infrequency of use there is little awareness of this important tool and more education on it is needed. This presentation focuses on the function and indication for rotablation. It provides an overview of the equipment and examples of cases that the device was used.
The production of a department CPD manual
Jasmine Grech, Adam Steward
Western Health, Melbourne, Australia
Continuing professional development (CPD) and its appropriate documentation has been a long‐standing expectation of medical radiation professionals. Medical Imaging Departments are exceedingly aware of these expectations and are often active in seeking ways to assist staff to meet these needs. As an intern radiographer at Western Health, I was charged with the preparation of a department CPD manual and logbook which would direct staff through the process of undertaking and documenting their CPD activities. This presentation describes my project, the final product and its use.
Full moon revisited: does workload increase?
Lesley Halmos1,2
1East Melbourne Radiology MIA, East Melbourne, Australia2St Vincent's Public Hospital Melbourne, Fitzroy, Australia
Background: Over many centuries, there are myths of werewolves, vampires, zombies and other ‘crazy’ beings coming out during full moon. It is common belief among health professionals that when there is a full moon, there is an increase in workload, specifically psychiatric patients. Although an increasing amount of research shows no correlation with the full moon, past studies have supported the link with full moon activity and changes in animal behaviour and human sleep patterns, which can increase the risk of epilepsy and psychosis. The majority of patients presenting to the Emergency Department (ED) at Melbourne's St Vincent's Public Hospital with psychosis or psychiatric symptoms will undergo a CT brain scan to exclude an organic origin.
Objective: To determine if workload increases in the ED in the form of psychiatric presentations, by comparing the number of CT brain scan requests on full moon and non‐full moon days, and business and non‐business hours.
Methods: Retrospective data were extracted from January 2013 to February 2014 comparing the number of CT brain scan requests by St Vincent's Hospital ED. Statistical analysis was conducted using a chi‐square test with statistical significance of P < 0.05.
Results: There was no difference in the number of daily ED CT scans on full moon compared to non‐full moon (9.75 scans/day vs 8.10 scans/day P = 0.306).
Conclusions: There is no difference in ED psychiatric presentations during full moon and non‐full days. A survey of healthcare professionals may shed light on whether the beliefs of the effects of full moon still persist.
Abdominal imaging in an acute setting for non‐ambulant patients should we consider a lateral decubitus radiograph?
Adam Steward, Shezard Arnolda
Western Hospital, Clayton, Australia
Introduction: The initial imaging modality of choice in the suspicion of perforation or bowel obstruction within an emergency department is a supine abdominal radiograph. If bowel dilatation is evident on the supine radiograph an erect abdominal radiograph is acquired to analyse the presence of a Pneumoperitoneum, consistent with a perforation or excessive fluid levels within the bowel, consistent with bowel obstruction.
Objective: The aim of this research is to compare the anatomical coverage and subjective quality of lateral decubitus abdominal radiographs to AP erect abdominal radiographs performed seated in bed.
Method: A retrospective study was performed over a period of 6 months including a sample of 1099 patients receiving abdominal radiographs. The anatomical coverage of lateral decubitus radiographs and AP erect radiographs in bed were compared against corresponding supine abdominal radiographs.
Results: Lateral decubitus radiographs covered 46% (P < 0.05) more anatomy between the iliac crest to the pubic symphysis, than AP erect radiograph in bed. On further analysis by a panel of qualified radiologist they stated that lateral decubitus radiographs had greater subjectivity and diagnostic potential than an AP erect radiograph in bed.
Conclusion: Lateral decubitus radiographs are a more optimal imaging technique than an AP erect radiograph in bed in non‐ambulant patients.


