Abstract
Background and objectives
An environmental trigger has been proposed as an inciting factor in the development of anti-GBM disease. This multicenter, observational study sought to define the national incidence of anti-GBM disease during an 11-year period (2003–2014) in Ireland, investigate clustering of cases in time and space, and assess the effect of spatial variability in incidence on outcome.
Design, setting, participants, & measurements
We ascertained cases by screening immunology laboratories for instances of positivity for anti-GBM antibody and the national renal histopathology registry for biopsy-proven cases. The population at risk was defined from national census data. We used a variable-window scan statistic to detect temporal clustering. A Bayesian spatial model was used to calculate standardized incidence ratios (SIRs) for each of the 26 counties.
Results
Seventy-nine cases were included. National incidence was 1.64 (95% confidence interval [95% CI], 0.82 to 3.35) per million population per year. A temporal cluster (n=10) was identified during a 3-month period; six cases were resident in four rural counties in the southeast. Spatial analysis revealed wide regional variation in SIRs and a cluster (n=7) in the northwest (SIR, 1.71; 95% CI, 1.02 to 3.06). There were 29 deaths and 57 cases of ESRD during a mean follow-up of 2.9 years. Greater distance from diagnosis site to treating center, stratified by median distance traveled, did not significantly affect patient (hazard ratio, 1.80; 95% CI, 0.87 to 3.77) or renal (hazard ratio, 0.76; 95% CI, 0.40 to 1.13) survival.
Conclusions
To our knowledge, this is the first study to report national incidence rates of anti-GBM disease and formally investigate patterns of incidence. Clustering of cases in time and space supports the hypothesis of an environmental trigger for disease onset. The substantial variability in regional incidence highlights the need for comprehensive country-wide studies to improve our understanding of the etiology of anti-GBM disease.
Keywords: anti-glomerular basement membrane disease; epidemiology; cluster analysis; incidence; ANCA; autoantibodies; follow-up studies; humans; kidney; kidney failure, chronic
Introduction
Anti-glomerular basement membrane (anti-GBM) disease is an autoimmune condition that affects the kidney and lung, resulting in rapidly progressive GN and alveolar hemorrhage, respectively. The pathogenesis of anti-GBM disease has been well defined at the molecular level, such that anti-GBM disease is regarded as a prototypic autoimmune disease (1). The factors that initiate the autoimmune process remain unknown. An environmental exposure has long been suspected as an inciting factor, but, largely because of its rarity, no epidemiologic studies have been able to accurately define this.
Efforts to define the incidence of anti-GBM disease have most often arisen from single centers or defined regions within a country. These studies are prone to ascertainment bias and may not be truly representative of the population at risk. There has also been heterogeneity among studies with regard to mode of case ascertainment and inclusion criteria, particularly with respect to ANCA status. These methodologic differences make international comparisons of incidence a challenging task.
Historically, the island of Ireland has experienced little in the way of inward migration and, genetically, has a relatively homogenous population. These factors make Ireland an attractive setting in which to study the epidemiology of a rare disease at a country-wide level. The primary aims of this study were to comprehensively define the national incidence of anti-GBM disease in the Republic of Ireland and to investigate the presence of clustering of cases in time and space. We hypothesized that unidentified environmental factors influence the occurrence of anti-GBM disease and that this may have implications for delivery of the required highly specialized care.
Materials and Methods
Study Population
We included all diagnosed cases of anti-GBM disease across all age groups in the Republic of Ireland between June 1, 2003, and May 31, 2014. The population at risk was calculated from national and regional population figures provided by the Central Statistics Office (available from http://www.cso.ie/en/census/). The Central Statistics Office undertook a national census in 2002, 2006, and 2011. The population for the intervening years was estimated as average increments from these census figures. Only individuals resident in the Republic of Ireland at the time of diagnosis were considered for inclusion in the study. Recruitment to the study was approved by the ethics committee of each center, and the requirement for consent was waived because all study data were anonymized by the local data controller.
Inclusion Criteria
Inclusion criteria were based on the 2012 Chapel Hill consensus nomenclature criteria: “Vasculitis affecting glomerular capillaries, pulmonary capillaries, or both, with GBM deposition of anti-GBM autoantibodies. Lung involvement causes pulmonary hemorrhage, and renal involvement causes glomerulonephritis with necrosis and crescents” (2). Included cases required evidence of GN and/or pulmonary capillaritis. In the absence of kidney biopsy, renal function that declined during a period of days to weeks in the presence of blood and protein on urine dipstick and a positive result on a serum anti-GBM antibody test was accepted as a surrogate for GN. In the absence of overt lung hemorrhage with hemoptysis, the presence of alveolar infiltrates on chest imaging in the presence of an anti-GBM antibody was accepted as a surrogate. Cases of crescentic GN on kidney biopsy with linear staining of IgG on immunofluorescence were included, even if no circulating anti-GBM antibody was identified. Cases of positivity for anti-GBM antibody occurring after transplantation in patients with Alport syndrome were excluded. Cases with a contemporaneous positive ANCA test result were included only if the kidney biopsy demonstrated linear IgG staining on immunofluorescence and/or there were no overt manifestations of an extrarenal vasculitic illness (e.g., mononeuritis multiplex, sinusitis, granulomatous lung disease, or vasculitic skin rash).
Case Ascertainment
Potential cases were initially identified by screening immunology laboratories for instances of positivity for anti-GBM antibody. Each case was investigated further by data extraction from hospital electronic records or chart review at the center where the test was ordered. Data were collected at each site using a standardized data collection form. In addition, the records of the national renal histopathology office were examined to confirm biopsy-proven cases and identify cases of anti-GBM disease without circulating anti-GBM antibody. Because the study was anonymized and carried out across several sites, there was potential for duplication of patients due to interhospital transfer. Duplicate cases were identified using the variables sex, date of birth, and electoral district at the time of diagnosis to ensure that each individual was included only once in the study.
Details of Anti-GBM Antibody Assay
Three types of anti-GBM antibody assay were in use during the study period. In the immunology laboratory at Beaumont Hospital Dublin, the center that encountered most cases, the following assays were in use: from June 2003, the BioDiagnostics ELISA kit (product code 107–007T), with a positive test result defined as exceeding 15 arbitrary units/ml; from December 2006 to August 2008, the Wieslab GBM ELISA kit (product code GP 104X), with a positive test result defined as >20 U/ml; from August 2008 until the end of the study period, the Phadia ELiA assay (product code 14–5514–01; Thermo Fisher Scientific, Vernon Hills, IL), which measures IgG antibody using a human recombinant noncollagenous-1 domain of the α-3 chain of type IV collagen, with >10 IU/ml indicating a positive test result.
Study Outcomes
The primary outcomes were incidence of anti-GBM disease at a national level and the presence of temporal or spatial clustering of incidence. Date of diagnosis was defined as the date of renal biopsy or date of positivity for anti-GBM antibody in the absence of a biopsy. Patient address at the time of diagnosis was documented to the level of electoral district and county. All patients were followed until death or last clinical encounter. The effect of spatial distribution on patient and renal survival was a secondary outcome. We also investigated the effect of dual positivity for ANCA and anti-GBM antibodies on patient and renal survival as an exploratory outcome.
Statistical Analyses
Annual incidence was calculated from June 1 to May 31 for each year of the study period and expressed as per million population (pmp) per year. We used a variable-window scan statistic (3,4) to detect clustering of cases in time. A Bayesian conditional autoregressive spatial model (5) was used to provide robust standardized incidence ratio (SIR) estimates and associated 95% confidence intervals (95% CIs) at the county level. The conditional autoregressive spatial model is appropriate for data arising from nonoverlapping spatial areas, where there is likely to be a similarity in data from areas close together, which may be due to neighborhood or grouping effects. The model is fitted in a Bayesian setting, which allows flexibility in the model specification, and is the framework in which these models are ordinarily fitted. These analyses were conducted using R (6) and the R package CARBayes (7). SIR estimates were further adjusted for deprivation, which allows interpretation of the results having adjusted for confounders related to this. The remainder of the statistical analyses was performed using Stata software, version 13 (StataCorp., College Station, TX). Continuous variables are presented as medians (interquartile range) and were compared using the Wilcoxon rank-sum test. Categorical variables were compared using the chi-squared test or Fisher exact test (when cell frequency was <5). Survival analysis was performed using Kaplan–Meier curves and the log-rank test. All analyses were two-tailed at an α level of 0.05.
Results
Patient Characteristics
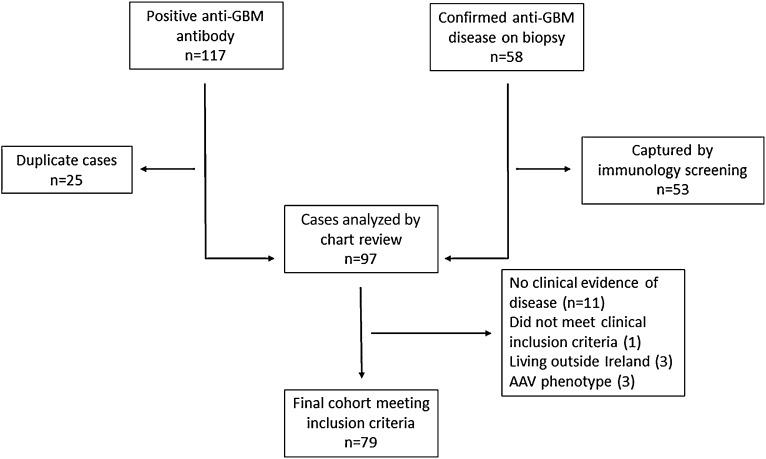
A total of 79 cases of anti-GBM disease met our inclusion criteria (Figure 1). The characteristics of the cohort are shown in Table 1. The median age was 63.4 (range, 48.5–74.5) years, and 56% of individuals were male. Most (77%) presented with kidney involvement alone. Five cases (6.3%) did not have detectable circulating anti-GBM antibody and were diagnosed on kidney biopsy, which was performed in 73% of patients. Fifty-eight cases (73%) required dialysis at presentation. One third of cases (33%) had a contemporaneous positive ANCA test result, with antigen specificity split roughly equally between myeloperoxidase and proteinase 3. Such double-positive cases were substantially older than ANCA-negative cases (median age, 69.7 versus 58.3 years). The mode of induction treatment is summarized in Supplemental Table 1.
Figure 1.
Flowchart of case ascertainment. A total of 97 individuals had either a positive result for anti-glomerular basement membrane (anti-GBM) antibody, or a biopsy-proven diagnosis of anti-GBM disease. Of those excluded from the final analysis, most (n=11) had a modest rise in antibody level with no evidence of clinical disease. Three double-positive cases had symptoms and signs consistent with multisystem ANCA-associated vasculitis (AAV). Three patients did not reside in Ireland at the time of diagnosis. One case had antibody positivity and reduced kidney function but did not meet our inclusion criteria.
Table 1.
Characteristics of patient cohort stratified by the presence or absence of a positive ANCA test result
| Characteristic | Total Cohort (n=79) | ANCA-Positivea (n=26 [33.3%]) | ANCA-Negative (n=52 [66.7%]) | P Valueb |
|---|---|---|---|---|
| Age, yr | 63.4 (48.5–74.5) | 69.7 (58.1–80.6) | 58.3 (44.6–69.7) | <0.01 |
| Women | 35 (44.3) | 13 (50) | 21 (40.4) | 0.42 |
| Systems involved | 0.85 | |||
| Kidney alone | 61 (77.2) | 21 (80.8) | 39 (75) | |
| Lung alone | 1 (1.3) | 0 | 1 (1.9) | |
| Both kidney and lung | 17 (21.5) | 5 (19.2) | 12 (23.1) | |
| Linear IgG on renal biopsy | 58 (73.4) | 19 (73.1) | 38 (73.1) | 1.0 |
| ANCA subtypec | NA | |||
| Anti-PR3 | 10 (12.8) | 10 (40) | NA | |
| Anti-MPO | 12 (15.4) | 12 (48) | NA | |
| Anti-PR3 and anti-MPO | 3 (3.8) | 3 (12) | NA | |
| Anti-GBM antibody level, U/ml | 212 (96–530) | 170 (96–400) | 273 (88–585) | 0.32 |
| Negative anti-GBM antibody result | 5 (6.3) | 2 (7.7) | 3 (5.8) | 1.0 |
| Dialysis at presentation | 58 (73.4) | 18 (69.2) | 40 (76.9) | 0.46 |
| Patient survival (95% CI), % | 0.47 | |||
| 1-yr survival | 73.7 (62.2 to 82.2) | 71.8 (49.6 to 85.5) | 74.2 (59.6 to 84.1) | |
| 5-yr survival | 59.1 (45.1 to 70.6) | 53.3 (28.2 to 73.1) | 61.0 (43.7 to 74.5) |
Numbers are expressed as number (percentage) or median (interquartile range) unless otherwise stipulated. PR3, proteinase 3; NA, not applicable; MPO, myeloperoxidase; 95% CI, 95% confidence interval.
ANCA test was performed in 78 of 79 cases.
For difference between ANCA-positive and ANCA-negative groups.
ELISA was performed in 25 of 26 patients who were ANCA positive by indirect immunofluorescence.
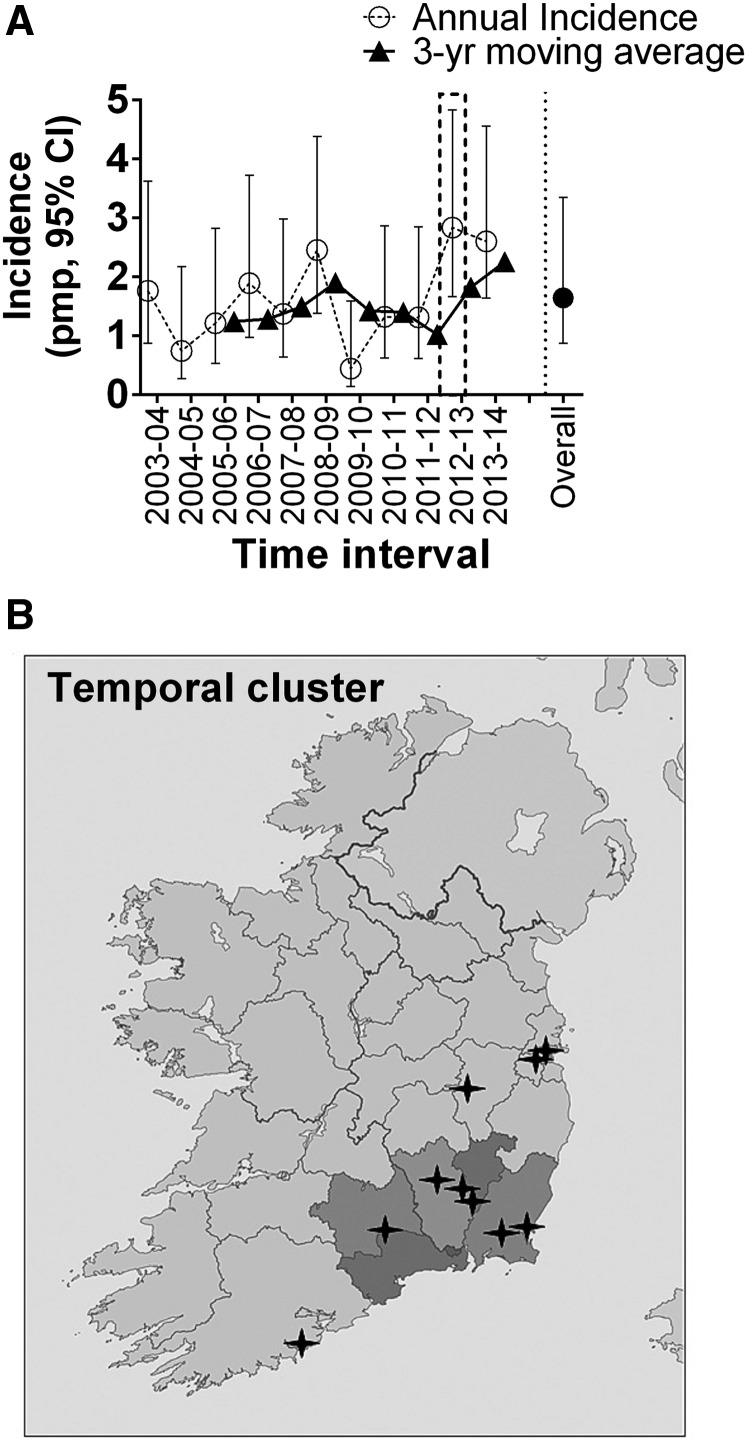
Incidence and Temporal Clustering
Annual incidence ranged from 0.4 to 2.8 pmp per year (Figure 2A, Table 2) and the average incidence over the observation period was 1.64 (95% CI, 0.82 to 3.35) pmp per year (Table 2). A statistically significant cluster of cases was identified beginning on December 10, 2012, and finishing on March 14, 2013 (P=0.05). In this 3-month period, ten cases were identified, 80% of whom were male. The proportion of double-positive cases (30%) and lung involvement at presentation (20%) was similar to that in the rest of the cohort. Because of the rarity of the condition, it was not possible to perform a combined temporal-spatial analysis. However, six of the ten cases (60%) resided in four predominantly rural counties in the southeast of the country at the time of diagnosis (Figure 2B).
Figure 2.
Incidence and temporal clustering. (A) Annual incidence rates (with 95% confidence intervals [95% CIs]) for each year of the study period, expressed as per million population (pmp). (B) The location of cases diagnosed in the temporal cluster (represented by black stars). Six cases were resident in the southeast of the country (area shaded in dark gray).
Table 2.
Annual national incidence of anti-GBM disease and census
| Year | Population, n | Cases, n | Incidence (95% CI), pmp |
|---|---|---|---|
| 2003–2004 | 3,979,803 | 7 | 1.76 (0.87 to 3.62) |
| 2004–2005 | 4,045,103 | 3 | 0.74 (0.27 to 2.17) |
| 2005–2006 | 4,133,703 | 5 | 1.21 (0.53 to 2.82) |
| 2006–2007 | 4,239,838 | 8 | 1.89 (0.97 to 3.72) |
| 2007–2008 | 4,382,748 | 6 | 1.37 (0.64 to 2.98) |
| 2008–2009 | 4,491,948 | 11 | 2.45 (1.38 to 4.38) |
| 2009–2010 | 4,540,248 | 2 | 0.44 (0.14 to 1.59) |
| 2010–2011 | 4,561,648 | 6 | 1.32 (0.62 to 2.86) |
| 2011–2012 | 4,588,252 | 6 | 1.31 (0.61 to 2.85) |
| 2012–2013 | 4,598,752 | 13 | 2.83 (1.66 to 4.83) |
| 2013–2014 | 4,606,452 | 12 | 2.60 (1.64 to 4.55) |
| Overall | 4,378,955 | 79 | 1.64 (0.82 to 3.35) |
Population figures for Ireland, 2003–2014. 95% CI, 95% confidence interval; pmp, per million population.
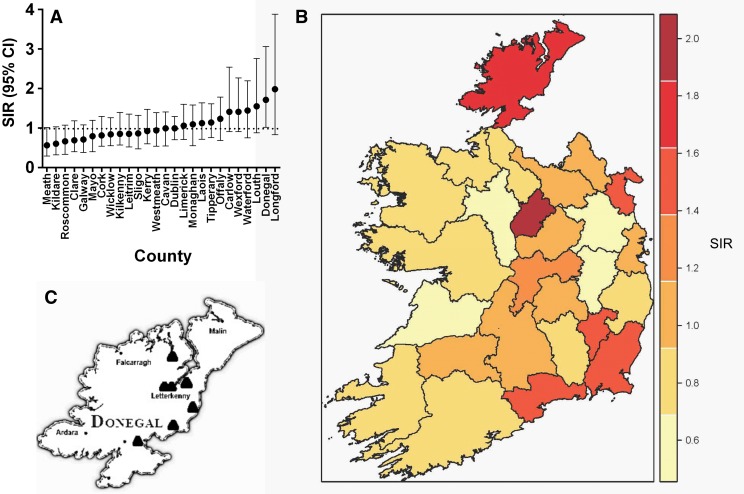
Spatial Analysis
The SIR of anti-GBM disease varied substantially across Irish counties (Figure 3A). For instance, western counties had relatively low SIRs compared with the rest of the country (Figure 3B). A spatial cluster was identified in the northwest of the country in County Donegal (SIR, 1.71; 95% CI, 1.02 to 3.06). During the 11-year observation period, a total of seven cases were diagnosed along the eastern border of Donegal (Figure 3C), a rural county with a population of 161,137 inhabitants (according to the 2011 census). None of these cases were diagnosed during the period of the temporal cluster, none had lung involvement, and five (71%) had a positive ANCA test result. A further concentration of cases was noted in the southeast (Figure 3B), an area that corresponded to the temporal cluster; however, in the spatial cluster analysis, the SIR 95% CI crossed 1 for each of the four counties in question.
Figure 3.
Spatial clustering. Results of spatial analysis showing standardized incidence ratios (SIR) with 95% confidence intervals (95% CIs) for each county (A), a country-wide spatial map of SIR (B), and the location of all seven cases encountered in County Donegal (C).
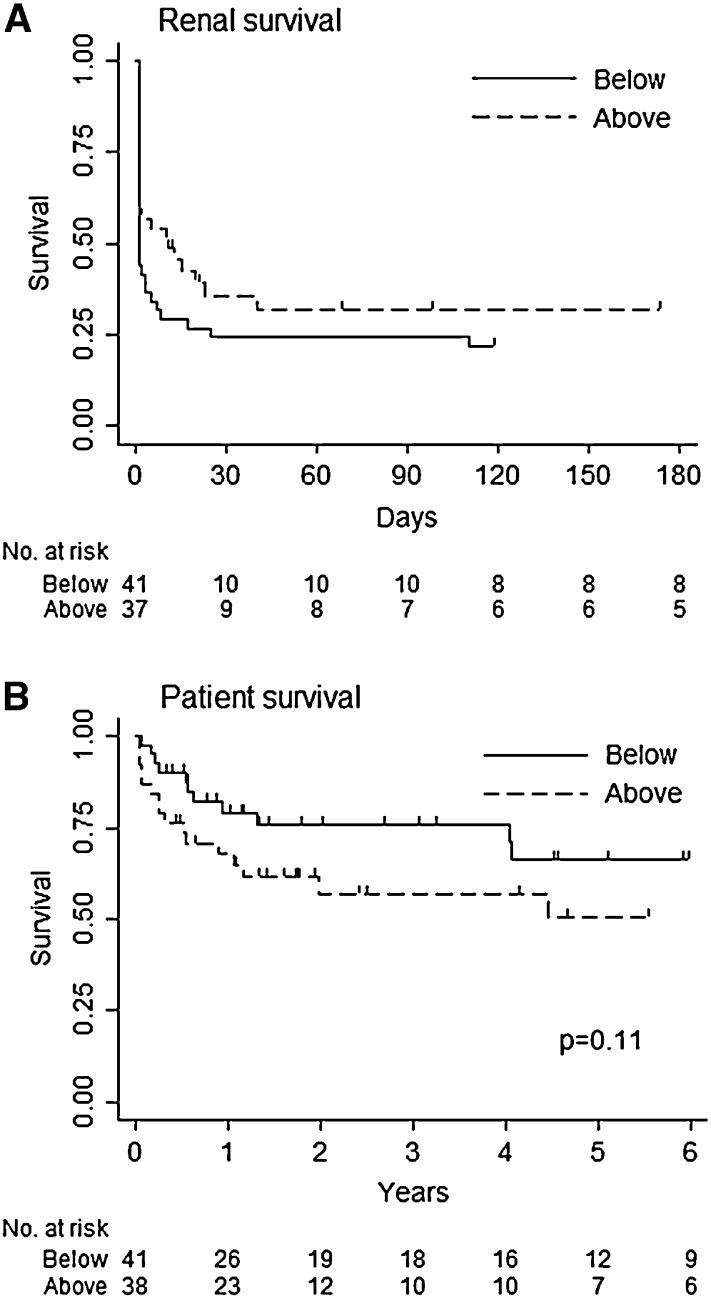
Effect of Clustering and Dual Antibody Positivity on Outcome
We hypothesized that the predominantly rural clustering would influence outcome and have implications for service provision. The median distance from site of diagnosis to treating center was 78 km (range, 11–163 km). With stratification by the median, there was no significant association between distance and renal survival (hazard ratio, 0.76; 95% CI, 0.40 to 1.13) (Figure 4A) or patient survival (hazard ratio, 1.80; 95% CI, 0.87 to 3.77) (Figure 4B). Patients with dual positivity for ANCA and anti-GBM antibodies had a marginally lower risk of ESRD (hazard ratio, 0.68; 95% CI, 0.34 to 0.99) (Supplemental Figure 1A), whereas dual positivity had no effect on risk of death (hazard ratio, 1.32; 95% CI, 0.61 to 2.93) (Supplemental Figure 1C). Age had no effect on risk of ESRD and, as expected, had a strong effect on risk of death (Supplemental Figure 1, B and D).
Figure 4.
Effect of clustering on outcome. Kaplan–Meier curves demonstrating renal survival (A) and patient survival (B) according to distance in kilometers from specialist referral center (above or below the median distance traveled).
Discussion
In this study, we report the national incidence of anti-GBM disease in the Republic of Ireland with a rate of 1.64 pmp per year. To our knowledge, this is the first attempt to accurately define the incidence of anti-GBM disease at a country-wide level using a robust combination of screening of anti-GBM antibody and renal biopsy data, along with national census data, to define the population at risk. We found evidence of temporal clustering and demonstrated substantial geographic variation in SIRs of anti-GBM disease, including a spatial clustering of cases in the northwest of Ireland. We hypothesized that a mismatch between the location of cases and centers providing specialized care would adversely affect outcome. Although patient survival was lower with greater distance from treating center, this was not statistically significant, and renal survival was actually slightly higher in geographically distant locations. Therefore, we conclude that the incidence of anti-GBM disease varies in space and time, supporting an environmental influence, but this does not appear to strongly affect care delivery.
A series of elegant studies over the last 50 years have greatly advanced our understanding of anti-GBM disease at a molecular level. This research endeavor has not been matched by high-quality epidemiologic studies attempting to link biologic processes with clinical experience of the disease. For example, incidence figures from the literature are variable. Table 3 summarizes the results of prior studies that have described the incidence of anti-GBM disease (8–15). Although there may be natural variation in disease rates among the populations studied, obvious differences in study methods may account for the different figures reported. In half of these studies, an incidence rate could not be calculated because the population at risk was not specified (12,13,15) or could only be estimated (11). Studies of renal biopsy registries have reported comparatively lower incidence rates of approximately 0.6 pmp per year (10,14). For a variety of reasons, not all patients with anti-GBM disease have a kidney biopsy performed. For example, the diagnosis was based on serology and clinical phenotype in 27% of the patients in our cohort.
Table 3.
Summary of published studies of anti-GBM disease incidence
| Author (Reference) | Year | Country | Source of Cases | Population at Risk | Duration of Study Period, yr | Cases, n | Rate, pmp/yr |
|---|---|---|---|---|---|---|---|
| Canney et al (current study) | 2016 | Ireland | Nationwide study using serology and biopsy data | 4,378,955 | 11 | 79 | 1.64 |
| Taylor et al (9) | 2011 | New Zealand | Serology and biopsy data from a single regional laboratory | 1,279,188 | 10 | 23 | 1.79 |
| Nakabayashi et al (12) | 2011 | Japan | Retrospective single-center study of renal pathology | NA | 10 | 7 | NAa |
| Hirayama et al (13) | 2008 | Japan | National survey of nephrology units | NA | 12 | 47 | NAb |
| Rutgers et al (10) | 2005 | Netherlands | Regional renal biopsy registry | 720,000 | 25 | 13 | 0.7 |
| Li et al (11) | 2004 | China | Single-center experience | 1,500,000c | 11 | 10 | 0.6 |
| Heaf et al (14) | 1999 | Denmark | National renal biopsy registry | 5,200,000 | 11.7 | NA | 0.6 |
| Andrassy et al (8) | 1991 | Germany | Single-center study of RPGN | 930,000 | 5.7 | 3 | 0.57 |
| McPhaul et al (15) | 1976 | United States | Prospective single-center study of consecutive renal biopsies | NA | 3.5 | 43 | NAa |
pmp, per million population; NA, not available; RPGN, rapidly progressive GN.
Rate expressed as proportion of biopsy-proven GN.
Rate expressed as the proportion of total RPGN cases in the survey.
Estimated catchment area of the hospital.
Previous anecdotal reports have described apparent clustering of anti-GBM disease cases. A mini-epidemic of four cases was described in Connecticut during the winter of 1971–1972, a time period that coincided with an outbreak of influenza A infection (16). A study from the Mersey region of the United Kingdom provided a descriptive report of ten cases that occurred between September 1984 and October 1985, with no obvious geographic clustering (17). Our study represents the first attempt to systematically examine incidence patterns of anti-GBM disease at a country-wide level and investigate spatial and temporal clustering using formal statistical methods. The clinical presentation of anti-GBM disease was different in the two types of clusters we identified. The clinical phenotype in the Donegal cohort was that of an older adult, mostly female, presenting with kidney involvement alone with a high proportion of ANCA positivity. In contrast, the clinical picture of cases in the temporal cluster was more in keeping with the classic description of anti-GBM disease: younger male individuals with pulmonary involvement and a lower proportion of double positivity. It is thus plausible that anti-GBM disease has more than one “face”: that is, that the disease behaves differently in subpopulations. Further comprehensive epidemiologic studies are required to investigate such hypotheses and link these findings back to our understanding of the molecular biology of anti-GBM disease.
The association between anti-GBM disease and simultaneous presence of positive ANCA result has long been recognized (18,19). In this study, we attempted to robustly define anti-GBM disease in the presence of a positive ANCA result with the use of renal biopsy data and the exclusion of cases with clear multisystem involvement beyond a renal or pulmonary renal syndrome. Our approach is reflected in a very low rate of relapse. We encountered a single renal relapse of anti-GBM disease confirmed on kidney biopsy. This was in a native kidney and was not associated with a positive ANCA result. Anti-GBM disease is classically a monophasic illness; although relapses can occur (20), they are often in the context of coexistent ANCA positivity (21,22). As seen in previous studies, we found that double-positive cases tended to be older (10,21,23). A diagnosis of “true” anti-GBM disease can be particularly challenging in this group because older patients may be less likely to undergo renal biopsy. Compared with a previous study in which only 16% of patients age >65 years had a kidney biopsy performed (23), the biopsy rate was high (>70%) among both younger and older patients in our cohort. Additionally, linear IgG staining was confirmed on immunofluorescence in 73% of double-positive cases. In contrast to previous studies, concomitant ANCA positivity was not associated with an increased risk of mortality or ESRD. One possible explanation for this was the approach we undertook for inclusion of double-positive cases, with the aim of excluding cases in which ANCA-associated vasculitis was the principal driver of disease. Nevertheless, further studies will be required to corroborate this finding.
Strengths of our study include the relatively large size of our cohort, the thorough screening process used at a national level to ascertain cases, and the high proportion of cases biopsied. Our study has several limitations. Although we had a comparatively large cohort in the context of a rare disease, the sample size did not facilitate exploration of other potential disease risk factors. It is possible that some findings may have arisen from chance, owing to the absolute number of cases involved and the fact that multiple tests were performed. No explicit adjustment for multiple testing was carried out, but the 95% CIs and actual P values have been reported to allow interpretation of the findings. Our goal was to obtain 100% case ascertainment during the study period. Given the retrospective study design, we could not be absolutely confident of identifying all cases of anti-GBM disease. For example, it is possible that some patients presenting with ESRD had anti-GBM disease but did not undergo any diagnostic test. However, such an occurrence would be highly unusual. The nature of the clinical syndrome (dramatic decline in kidney function, often with lung hemorrhage) is such that cases are managed in a hospital setting, and so it is unlikely that we missed cases remaining in community care. In addition, the antibody test is both sensitive and specific. By combining serology with a thorough review of histopathology records, we are confident that the observed incidence rate reflects the true incidence rate in the country.
In conclusion, we report national incidence rates for anti-GBM disease in the Republic of Ireland and show that these are higher than those in most other countries. We believe this reflects our diligent approach to both case ascertainment and defining the at-risk population. This study advances the existing literature by providing more robust and representative incidence estimates than previously reported, along with a systematic approach to the detection of disease clusters. We discovered a statistically significant clustering of cases in time, which supports the hypothesis of an environmental exposure as the disease-initiating factor for anti-GBM disease. We also demonstrated substantial regional variation in incidence rates. Given this degree of heterogeneity, it is likely that single-center studies are not truly representative of the population at risk. Rather, further epidemiologic studies are required at a country-wide level in other populations to better define incidence patterns of anti-GBM disease and advance our understanding of its etiology.
Disclosures
None.
Supplementary Material
Acknowledgments
We thank Peter Annis, Kevin Hartigan, Dr. Vincent Tormey, Dr. Waleed ElSheikh, Dr. Sami Suleiman, Dr. Anne Marie Moran, and Dr. Yvonne Ryan for their contribution to case ascertainment and data collection.
M.A.L. is supported by Science Foundation Ireland grant 11/Y/B2093.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
See related editorial, “Clustering of Anti-GBM Disease: Clues to an Environmental Trigger?,” on pages 1324–1326.
This article contains supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.13591215/-/DCSupplemental.
References
- 1.Hellmark T, Segelmark M: Diagnosis and classification of Goodpasture’s disease (anti-GBM). J Autoimmun 48-49: 108–112, 2014 [DOI] [PubMed] [Google Scholar]
- 2.Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F, Flores-Suarez LF, Gross WL, Guillevin L, Hagen EC, Hoffman GS, Jayne DR, Kallenberg CG, Lamprecht P, Langford CA, Luqmani RA, Mahr AD, Matteson EL, Merkel PA, Ozen S, Pusey CD, Rasmussen N, Rees AJ, Scott DG, Specks U, Stone JH, Takahashi K, Watts RA: 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum 65: 1–11, 2013 [DOI] [PubMed] [Google Scholar]
- 3.Naus J, Wallenstein S: Temporal surveillance using scan statistics. Stat Med 25: 311–324, 2006 [DOI] [PubMed] [Google Scholar]
- 4.Nagarwalla N: A scan statistic with a variable window. Stat Med 15: 845–850, 1996 [DOI] [PubMed] [Google Scholar]
- 5.Besag J, York J, Mollie A: Bayesian image restoration with two applications in spatial statistics. Ann Inst Stat Math 43: 1–59, 1991 [Google Scholar]
- 6.R Core Team : R: A language and environment for statistical computing, Vienna, Austria, R Foundation for Statistical Computing, 2014 [Google Scholar]
- 7.Lee D: CARBayes: An R package for bayesian spatial modeling with conditional autoregressive priors. J Stat Softw 55: 1–24, 2013 [Google Scholar]
- 8.Andrassy K, Küster S, Waldherr R, Ritz E: Rapidly progressive glomerulonephritis: Analysis of prevalence and clinical course. Nephron 59: 206–212, 1991 [DOI] [PubMed] [Google Scholar]
- 9.Taylor DM, Yehia M, Simpson IJ, Thein H, Chang Y, de Zoysa JR: Anti-glomerular basement membrane disease in Auckland. Intern Med J 42: 672–676, 2012 [DOI] [PubMed] [Google Scholar]
- 10.Rutgers A, Slot M, van Paassen P, van Breda Vriesman P, Heeringa P, Tervaert JW: Coexistence of anti-glomerular basement membrane antibodies and myeloperoxidase-ANCAs in crescentic glomerulonephritis. Am J Kidney Dis 46: 253–262, 2005 [DOI] [PubMed] [Google Scholar]
- 11.Li FK, Tse KC, Lam MF, Yip TP, Lui SL, Chan GS, Chan KW, Chan EY, Choy BY, Lo WK, Chan TM, Lai KN: Incidence and outcome of antiglomerular basement membrane disease in Chinese. Nephrology (Carlton) 9: 100–104, 2004 [DOI] [PubMed] [Google Scholar]
- 12.Nakabayashi K, Fujioka Y, Arimura Y, Fukuoka T, Marumo T, Umino M, Kamiya Y, Okai T, Tsurumaki S, Nagasawa T, Yamada A: Anti-glomerular basement membrane (anti-GBM) disease accompanied by vasculitis that was not positive for antineutrophil cytoplasmic antibodies to myeloperoxidase and proteinase 3: A report of two cases and the incidence of anti-GBM disease at one institution. Clin Exp Nephrol 15: 504–513, 2011 [DOI] [PubMed] [Google Scholar]
- 13.Hirayama K, Yamagata K, Kobayashi M, Koyama A: Anti-glomerular basement membrane antibody disease in Japan: Part of the nationwide rapidly progressive glomerulonephritis survey in Japan. Clin Exp Nephrol 12: 339–347, 2008 [DOI] [PubMed] [Google Scholar]
- 14.Heaf J, Løkkegaard H, Larsen S: The epidemiology and prognosis of glomerulonephritis in Denmark 1985-1997. Nephrol Dial Transplant 14: 1889–1897, 1999 [DOI] [PubMed] [Google Scholar]
- 15.McPhaul JJ Jr, Mullins JD: Glomerulonephritis mediated by antibody to glomerular basement membrane. Immunological, clinical, and histopathological characteristics. J Clin Invest 57: 351–361, 1976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Perez GO, Bjornsson S, Ross AH, Aamato J, Rothfield N: A mini-epidemic of Goodpasture’s syndrome clinical and immunological studies. Nephron 13: 161–173, 1974 [DOI] [PubMed] [Google Scholar]
- 17.Williams PS, Davenport A, McDicken I, Ashby D, Goldsmith HJ, Bone JM: Increased incidence of anti-glomerular basement membrane antibody (anti-GBM) nephritis in the Mersey Region, September 1984-October 1985. Q J Med 68: 727–733, 1988 [PubMed] [Google Scholar]
- 18.O’Donoghue DJ, Short CD, Brenchley PE, Lawler W, Ballardie FW: Sequential development of systemic vasculitis with anti-neutrophil cytoplasmic antibodies complicating anti-glomerular basement membrane disease. Clin Nephrol 32: 251–255, 1989 [PubMed] [Google Scholar]
- 19.Levy JB, Hammad T, Coulthart A, Dougan T, Pusey CD: Clinical features and outcome of patients with both ANCA and anti-GBM antibodies. Kidney Int 66: 1535–1540, 2004 [DOI] [PubMed] [Google Scholar]
- 20.Levy JB, Lachmann RH, Pusey CD: Recurrent Goodpasture’s disease. Am J Kidney Dis 27: 573–578, 1996 [DOI] [PubMed] [Google Scholar]
- 21.Alchi B, Griffiths M, Sivalingam M, Jayne D, Farrington K: Predictors of renal and patient outcomes in anti-GBM disease: clinicopathologic analysis of a two-centre cohort. Nephrol Dial Transplant 30: 814–821, 2015 [DOI] [PubMed]
- 22.Lindic J, Vizjak A, Ferluga D, Kovac D, Ales A, Kveder R, Ponikvar R, Bren A: Clinical outcome of patients with coexistent antineutrophil cytoplasmic antibodies and antibodies against glomerular basement membrane. Ther Apher Dial 13: 278–281, 2009 [DOI] [PubMed] [Google Scholar]
- 23.Cui Z, Zhao J, Jia XY, Zhu SN, Zhao MH: Clinical features and outcomes of anti-glomerular basement membrane disease in older patients. Am J Kidney Dis 57: 575–582, 2011 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.