Abstract
Background:
In the absence of primary care and prevailing associated social stigma, many patients of neural tube defects (NTDs) from remote areas die without getting any treatment. The high number of such untreated cases and unregistered deaths in these areas made us ponders to the fact that tertiary care center-based studies do not represent the true incidence of NTDs.
Materials and Methods:
We did a population-based survey for NTDs births of rural areas from Jaunpur to Ghazipur district in Eastern Uttar Pradesh. These districts are among the least developed areas of Northern India in Uttar Pradesh among other 17.
Results:
The data show an incidence of 7.48 per 1000 live births.
Conclusion:
Besides of unawareness regarding periconceptional folate supplementation, intensive effort is required to design adequately powered studies to search other key factors responsible for high prevalence of NTDs.
Key words: Epidemiology, India, meningomyelocele, neural tube defect
Introduction
Neural tube defects (NTDs) are among the leading noninfectious birth defects with a worldwide prevalence of 1–2 per 1000 live births[1] causing significant infants' morbidity and mortality and known to have multifactorial-polygenic origin for occurrence where both genetic and environmental factors including maternal nutrition are reported to have considerable contributions[2] known to vary with geographical areas, population, and type of study.[3] NTD comprises spina bifida, anencephaly, encephalocele, craniorachischisis, and iniencephaly.
The prevalence of NTDs in India has been reported to vary from 0.5 to 11 per 1000 births.[4,5,6,7,8] However, most of these are hospital-based studies from different cities. The Indian Planning Commission has initiated the Backward Districts Initiative scheme, which aims to identify districts which would benefit from focused development programs to address the problems of low agricultural productivity and unemployment. Two hundred districts have identified the population comprising mostly of marginal farmers and forest dwellers. In many of these districts, poverty has increased despite consistent focus of several poverty eradication programs. In the state of Uttar Pradesh, 17 districts have been identified. Ghazipur and Jaunpur are among them. The criteria for the under development, included the following parameters namely, incidence of poverty, education, health, water supply, transport and communications, and degree of industrialization.
In India, 68.85% of the population resides in rural areas (Census 2011),[9] therefore, it can be assumed that on an average there are almost 2.2 times higher frequency of reproducibly active female in the rural areas. These females often undergo delivery in supervision of untrained dais, and most of defective births die prior to getting treatment. Considering the above facts, it may be suggested that the tertiary care center-based studies for the incidence of the NTDs may not represent the true incidence of NTDs. The present study was, therefore, undertaken, in order to determine the prevailing incidence of NTD in these districts.
Materials and Methods
The study was approved by the ethical committee of Banaras Hindu University, Varanasi. To determine the incidence of NTDs, two districts of Eastern Uttar Pradesh that is Northern part of India were selected which were listed among the most deprived by the Indian Planning Commission. The study was done in Dharmapur block (117 villages) of district Jaunpur and Deokali (226 villages) block in Ghazipur District, Uttar Pradesh, India, between March, 2012, and September, 2014. The study was accomplished by a door-to-door visit in a cluster of 30 villages of Jaunpur and 30 villages of Ghazipur. The total population in Jaunpur (4,494,204) and Ghazipur (3,620,268) was distributed in 21 blocks and 16 blocks, respectively. From which 30 villages of Dharmapur block (Jaunpur) and 30 villages of Deokali block (Ghazipur) were selected, covering a population of 91,195. These villages were selected on random basis. For this study, we adopted the methodology followed by Cherian et al.[10] for population-based study in Balrampur district of Western Uttar Pradesh. In the preliminary step, information about women who had delivered during the preceding year was collected from primary health centers and accredited and social health activist of each village. Three teams of trained fieldworkers having three members in each team were recruited and sent for the door-to-door survey. All the teams were provided photographic album consisting of pictures of various forms of NTDs such as meningocele, meningomyelocele, encephalocele, and anencephaly, and a list of questions about the history of defective pregnancy and previous pregnancy. Verbal informed consent for participation in this study was taken. All mothers, as well as other relative females, were asked about any births similar to those depicted in the album born to them or in the village during this period.
Results
During the study period, 2540 live births were registered. The estimated crude birth rate was 24.85 per 1000 population, which is almost equal to crude birth rate in Uttar Pradesh. Nineteen babies were born with NTDs during the survey [Table 1], of which ten died (5 with myelomeningocele; 4 with meningocele; 1 with anencephaly). This gives an incidence of NTDs of one affected baby per 134 live births, 7.48 per 1000 live births. In this study, we observed myelomeningocele with a relative occurrence of 3.149 per 1000 live births [Table 1] making up 42% of total cases of NTDs seen with anencephaly having the lowest occurrence of 5% [Figure 1]. About 36.84% of total cases had associated malformations such as hydrocephaly, paraplegia, Arnold–Chiari malformation, and talipesequinovarus, [Table 1] and the gender wise distribution (male: female) of various forms of NTDs was highest for meningocele (2:1) followed by myelomeningocele (1.6:1) and encephalocele (1:1) [Figure 2]. The ratio of male affected to that of the female affected was 1.38–1, frequency of spina bifida was higher in proportion compared to anencephaly. In this study, we did not incorporate the cases of miscarriages and stillbirths as no definite information regarding their physical characteristics were available.
Table 1.
Frequency and types of NTDs of cases born during March 2012-September 2014
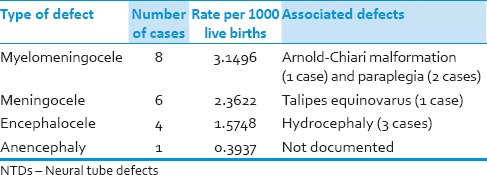
Figure 1.
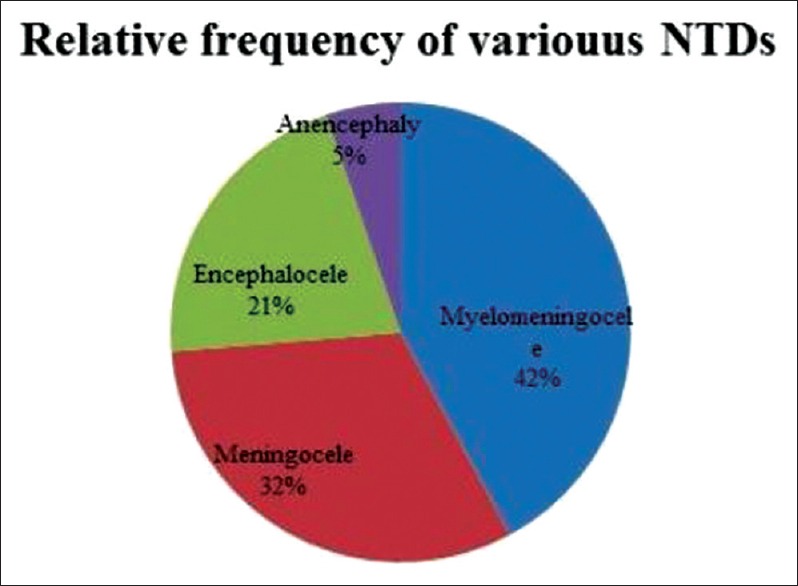
Pie chart showing the relative frequency of various types of neural tube defects. This figure represents the higher frequency myelomeningocele (42%) type of neural tube defect, and least frequency was in anencephaly (5%) of the cases
Figure 2.
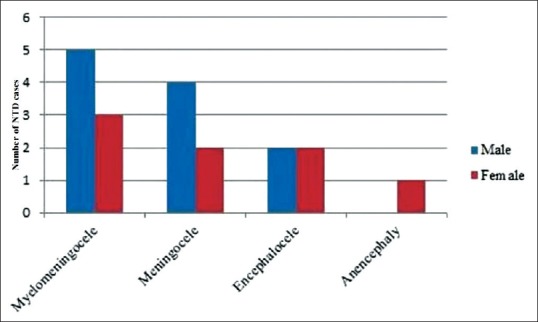
Gender distribution of the neural tube defects illustrated by bar diagram. This figure shows that the numbers of neural tube defect cases including myelomeningocele and meningocele were higher in males than females
Discussion
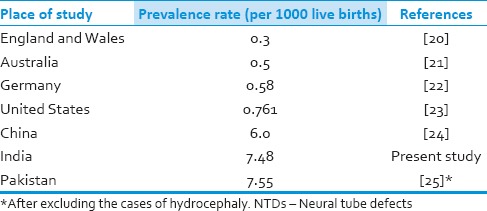
This study reports an incidence of NTDs of 7.48 per 1000 births. When we compare this result to previous studies on the incidence of the NTDs in various parts of India published in the last decade [Table 2], this is slightly lower than another population-based study which showed an incidence rate of 8.21 per 1000 births reported from Balrampur district, in Western Uttar Pradesh;[10] however, rest of the studies in the table were hospital-based and, therefore, cannot be compared to ours. Though not significantly different, the small decrease in the incidence rate could be attributed to the implementation of the national program in the rural areas for folic acid supplementation which is known to prevent NTDs up to 70%.[18,19] On the other hand, as shown in Table 3, the incidence of NTDs in the Indian subcontinent is much higher than seen in the economically developed countries, where prenatal screening is a standard medical protocol, allowing for the early detection of fetuses with NTDs allowing the parents the option of termination. However in India, unplanned pregnancies, unawareness regarding the benefits of periconceptional folate supplementation, and the absence of such prenatal diagnostic tests mean that parents only become aware of their malformed infant after birth. The difference of the incidence of NTDs in our study in comparison to Cherian et al.,[10] in spite of similar random based study protocols may be due to differences in the populations under study and the fact that our study cohort is twice the size of that reported by Cherian et al. and is thus providing a more accurate result. Further, during survey some cases may have been missed like spina bifida occulta. No data about stillbirths or miscarriage were available as the mother, and other close relatives were unable to explain the morphological features of stillborn. A custom exists in these regions of Eastern Uttar Pradesh, if a stillborn or miscarriage fetus has any abnormality, they are discarded immediately without showing them to the mother any family members or villagers, as it is considered a bad omen. The dais, who help in such deliveries, do not keep accurate notes on the occurrence of such births, and thus finding the history of a stillborn or miscarriage with NTD had been very difficult, and we think that we may have missed such cases. Another limitation of this study is the inability to discriminate between syndromic and nonsyndromic NTDs on behalf of information collected from dais and relatives in death cases, although the authors did not find any live child with NTD of syndromic origin. Of the nineteen cases of NTD recorded, the frequencies of a male child affected to that of the female child were more with a ratio of 1.38–1. Many studies revealed that females are more affected than males.[26,27] The frequency of spina bifida was in higher proportion compared to anencephaly. However, many studies have reported equal incidences of these two forms of NTD,[28,29] which may be attributed for not considering miscarriages and stillbirths. NTD is a neglected problem whose etiopathogenesis has been attributed to both genetic and environmental factors. Our study reveals a high incidence in Northern part of India. A much higher incidence might be prevailing in some of the remote villages, where a survey in the near future may unravel many mysteries yet unexplored.
Table 2.
Prevalence of NTDs and types of studies from 1992 to 2014 in different regions of India
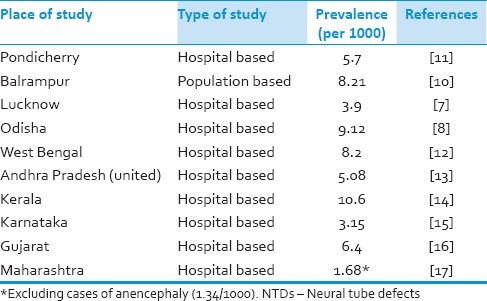
Table 3.
Prevalence of NTDs among developed countries and adjoining Asian countries
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Greene ND, Copp AJ. Development of the vertebrate central nervous system: Formation of the neural tube. Prenat Diagn. 2009;29:303–11. doi: 10.1002/pd.2206. [DOI] [PubMed] [Google Scholar]
- 2.Hall JG, Friedman JM, Kenna BA, Popkin J, Jawanda M, Arnold W. Clinical, genetic and epidemiological factors in neural tube defects. Am J Med Genet. 1988;43:827–37. [PMC free article] [PubMed] [Google Scholar]
- 3.Au KS, Ashley-Koch A, Northrup H. Epidemiologic and genetic aspects of spina bifida and other neural tube defects. Dev Disabil Res Rev. 2010;16:6–15. doi: 10.1002/ddrr.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Verma IC, Mathews AR. Congenital malformations in India. In: Satyavati GV, editor. Peoples of India: Some Genetical Aspects. New Delhi: Indian Council of Medical Research; 1983. p. 70. [Google Scholar]
- 5.Kulkarni ML, Mathew MA, Ramachandran B. High incidence of neural-tube defects in South India. Lancet. 1987;1:1260. doi: 10.1016/s0140-6736(87)92705-x. [DOI] [PubMed] [Google Scholar]
- 6.Sharma JB, Gulati N. Potential relationship between dengue fever and neural tube defects in a northern district of India. Int J Gynaecol Obstet. 1992;39:291–5. doi: 10.1016/0020-7292(92)90260-p. [DOI] [PubMed] [Google Scholar]
- 7.Sharma AK, Upreti M, Kamboj M, Mehra P, Das K, Misra A, et al. Incidence of neural tube defects of Lucknow over a 10 year period from 1982-1991. Indian J Med Res. 1994;99:223–6. [PubMed] [Google Scholar]
- 8.Kumari BS, Panda R, Rath S. Neural tube defect: Epidemiologic and demographic implication. IOSR J Dent Med Sci. 2014;13:1–4. [Google Scholar]
- 9.Census of India. 2011. [Last retrieved on 2015 Aug 07]. Available from: http://www.censusindia.gov.in/2011-prov-results/paper2/data_files/india/Rural_Urban_2011.pdf .
- 10.Cherian A, Seena S, Bullock RK, Antony AC. Incidence of neural tube defects in the least-developed area of India: A population-based study. Lancet. 2005;366:930–1. doi: 10.1016/S0140-6736(05)67319-9. [DOI] [PubMed] [Google Scholar]
- 11.Mahadevan B, Bhat BV. Neural tube defects in Pondicherry. Indian J Pediatr. 2005;72:557–9. doi: 10.1007/BF02724177. [DOI] [PubMed] [Google Scholar]
- 12.Pradhan R, Mondal S, Adhya S. A study of neural tube defects in perinatal autopsy series. Med Legal Updates. 2013;13(1):140–4. [Google Scholar]
- 13.Durgesh V, Vijaylaxmi K, Rao RR. Incidences of myelomeningocele with anencephaly in Vijaynagaram district of north coastal Andhra Pradesh. Int J Basic Appl Med Sci. 2013;3:259–62. [Google Scholar]
- 14.Menasinka SB. A study of neural tube defects. Anat Soc India. 2010;59:162–7. [Google Scholar]
- 15.Suresh MN. Neural tube defects. Anat Karnataka. 2011;5:61–4. [Google Scholar]
- 16.Gupta S, Gupta P, Soni JS. A study on incidences of various systematic congenital malformations and their association with maternal factors. Natl J Med Res. 2012;2:19–21. [Google Scholar]
- 17.Dutta V, Chaturvedi P. Congenital malformations in rural Maharashtra. Indian Pediatr. 2000;37:998–1001. [PubMed] [Google Scholar]
- 18.Prevention of neural tube defects: Results of the Medical Research Council Vitamin Study. MRC Vitamin Study Research Group. Lancet. 1991;338:131–7. [PubMed] [Google Scholar]
- 19.Czeizel AE, Dudás I. Prevention of the first occurrence of neural-tube defects by periconceptional Vitamin supplementation. N Engl J Med. 1992;327:1832–5. doi: 10.1056/NEJM199212243272602. [DOI] [PubMed] [Google Scholar]
- 20.Morris JK, Wald NJ. Prevalence of neural tube defect pregnancies in England and Wales from 1964 to 2004. J Med Screen. 2007;14:55–9. doi: 10.1258/096914107781261945. [DOI] [PubMed] [Google Scholar]
- 21.Abeywardana S, Bower C, Halliday J, Chan A, Sullivan EA. Prevalence of neural tube defects in Australia prior to mandatory fortification of bread-making flour with folic acid. Aust N Z J Public Health. 2010;34:351–5. doi: 10.1111/j.1753-6405.2010.00565.x. [DOI] [PubMed] [Google Scholar]
- 22.Bowles D, Wasiak R, Kissner M, van Nooten F, Engel S, Linder R, et al. Economic burden of neural tube defects in Germany. Public Health. 2014;128:274–81. doi: 10.1016/j.puhe.2013.12.001. [DOI] [PubMed] [Google Scholar]
- 23.Boulet SL, Yang Q, Mai C, Kirby RS, Collins JS, Robbins JM, et al. Trends in the postfortification prevalence of spina bifida and anencephaly in the United States. Birth Defects Res A Clin Mol Teratol. 2008;82:527–32. doi: 10.1002/bdra.20468. [DOI] [PubMed] [Google Scholar]
- 24.Xiao KZ, Zhang ZY, Su YM, Liu FQ, Yan ZZ, Jiang ZQ, et al. Central nervous system congenital malformations, especially neural tube defects in 29 provinces, metropolitan cities and autonomous regions of China: Chinese Birth Defects Monitoring Program. Int J Epidemiol. 1990;19:978–82. doi: 10.1093/ije/19.4.978. [DOI] [PubMed] [Google Scholar]
- 25.Khattak ST, Naheed T, Akhtar S, Jamal T. Incidence and risk factors for neural tube defects in Peshwar. Gomal J Med Sci. 2008;6:1–4. [Google Scholar]
- 26.Little L, Elwood JM. Epidemiology of neural tube defects. In: Kiley M, editor. Reproductive and Perinatal Epidemiology. Boston: CRC Press; 1991. pp. 251–336. [Google Scholar]
- 27.McDonnell RJ, Johnson Z, Delaney V, Dack P. East Ireland 1980-1994: Epidemiology of neural tube defects. J Epidemiol Community Health. 1999;53:782–8. doi: 10.1136/jech.53.12.782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Botto LD, Moore CA, Khoury MJ, Erickson JD. Neural-tube defects. N Engl J Med. 1999;341:1509–19. doi: 10.1056/NEJM199911113412006. [DOI] [PubMed] [Google Scholar]
- 29.Melvin EC, George TM, Worley G, Franklin A, Mackey J, Viles K, et al. Genetic studies in neural tube defects. NTD Collaborative Group. Pediatr Neurosurg. 2000;32:1–9. doi: 10.1159/000028889. [DOI] [PubMed] [Google Scholar]


