Abstract
Background:
Tentorial hematoma is frequently seen in traumatic brain injury (TBI) patients, especially in motorized two-wheeler riders following head injury. However its relevance and prognostic significance are not known.
Objective:
To evaluate patients of TBI with tentorial hematoma using a simple grading system and attempt to correlate this grading with factors like helmet use and neurological outcome.
Materials and Methods:
This prospective study over a 1-year period included patients with TBI who had tentorial hematoma in the initial plain head. Patients were divided into three grades based on the initial CT findings: Grade I: Isolated tentorial hematoma, grade II: tentorial hematoma with midline shift but open cisterns and grade III: Tentorial hematoma with effaced cisterns. Clinical and radiological records of patients including admission GCS and GOS at discharge were assessed in all cases.
Observations:
A total of 1786 patients of TBI were admitted during the study period. Of these, 106 (5.9%) patients had tentorial hematoma. 84.9% (n = 90) were male and 15.1% (n = 16) were female with the mean age being 36.5 years (range 2-66 years). The mean admission GCS was 13, 11 and 8 in patients with grade I, II and III tentorial hematoma respectively. 43.4% (n = 46) of the patients had grade I, 32.1% (n = 34) had grade II and 24.5% (n = 26) patients had grade III tentorial hematoma. Seventy-one patients (84.5%) were riding motorized two wheelers with 63 (89%) wearing helmets. The majority of the patients wearing helmets (58.8%) had grade I hematoma with 35% (n = 22) having grade II hematoma and only 6.3% (n = 4) having grade III hematoma. Overall, there were 20 deaths. 50% (n = 10) of the deaths were in patients with grade III hematoma and 40% (n = 8) of the deaths were in patients with grade II hematoma. There were two (10%) deaths in patients with grade I hematoma (both unrelated to head injury). The mean GOS at the time of discharge was 5, 4.1 and 2.2 in patients with grade I, II and III tentorial hematoma, respectively.
Conclusions:
Tentorial hematomas are very common in two-wheeler riders with TBI and could be a marker for indirect forces such as rotational forces experienced while wearing helmets.
Key words: Head injury, helmet, mortality, outcome, tentorial bleed, tentorial hematoma, traumatic brain injury
Introduction
Motorized two-wheeler riders have a disproportionately higher incidence of traumatic brain injuries (TBI) as compared to other modes of transport. Worldwide, helmets have been shown to be extremely effective in reducing the incidence as well as the severity of TBI in this vulnerable population.[1] This reduction in mortality and morbidity may be due to absorption and deflection of the kinetic forces by the helmet. The redistribution of forces may have new consequences such as formation of tentorial hematoma (s). It is the senior authors observation that tentorial hematoma are very common in helmeted motorized two-wheeler riders who suffer head injury and this hypothesis is made stronger by previous studies which have shown that presence of tentorial hematoma signifies rotational and acceleration-decleration forces experienced around the brainstem.[1]
It may also be argued that sporadically described hematoma of the tentorium cerebelli and its vicinity may also be a predictive factor for outcome in patients after TBI. However, unequivocal radiological diagnostic criteria for tentorial hematoma are lacking and presence of hyperdensity in the region of the tentorial cerebelli on plain CT head following trauma is commonly considered as evidence for tentorial hematoma.[2] In the current study we propose a simple grading system for tentorial hematoma and attempt to correlate this grading system with factors such as helmet use and neurological outcome.
Materials and Methods
This prospective study was conducted from January 2009 to Dec 2009 in patients of TBI who were admitted in the department of Neurosurgery. Only patients who had initial CT scan done within 24 hours of injury were included in the study. The CT scan was evaluated for the presence of tentorial hematoma by two neurosurgeons (DA and PD). Tentorial hematoma was defined as hyperdensity in posterior fossa near tentorium ceribelli with hounsefield unit of 60-90 on plain CT head.
Patients were divided into three groups based on a grading system devised by the authors:
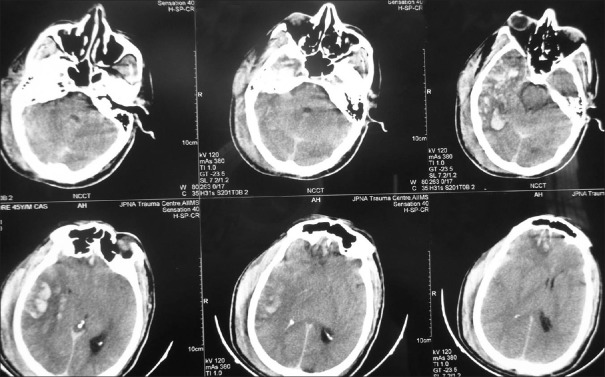
Grade I: Isolated tentorial hematoma [Figure 1]
Figure 1.
(a and b) Plain CT head of a patient with head injury showing isolated tentorial hematoma (grade 1 tentorial hematoma)
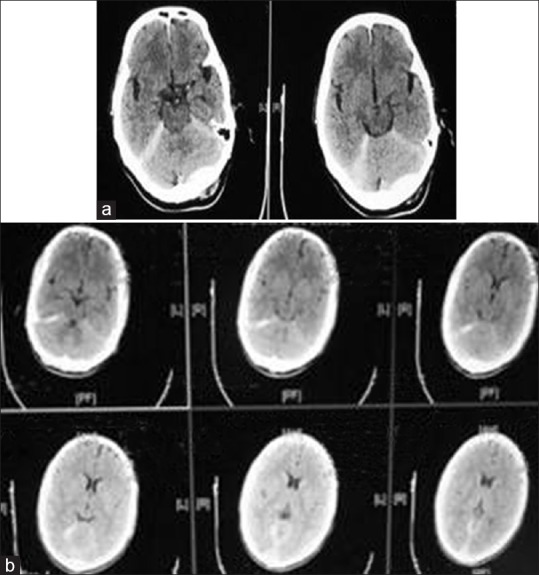
Grade II: Tentorial hematoma with midline shift but open cisterns [Figure 2]
Figure 2.
Plain CT head of a patient with head injury showing tentorial hematoma with midline shift but open cisterns (grade 2 tentorial hematoma)
Grade III: Tentorial hematoma with effaced basal cisterns [Figure 3].
Figure 3.
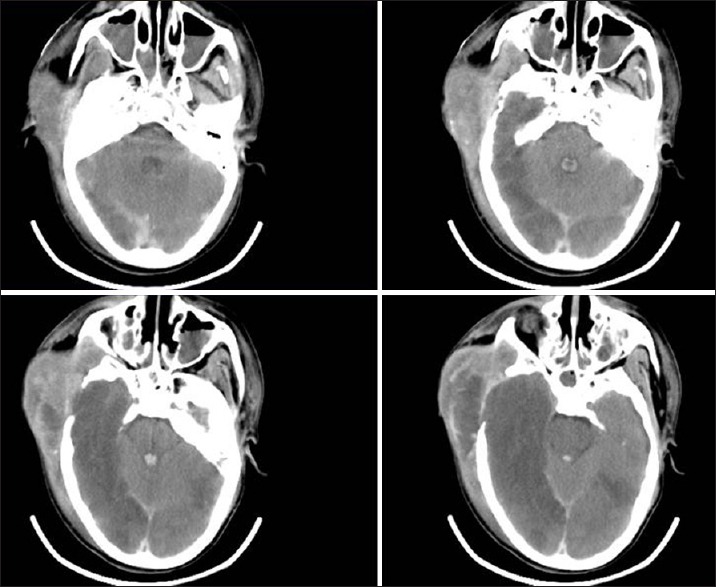
Plain CT head of a patient with head injury showing tentorial hematoma with effaced cisterns (grade 3 tentorial hematoma)
Demographic, clinical and radiological records of patients including admission GCS and GOS at discharge were assessed in all cases
Results
Demographics
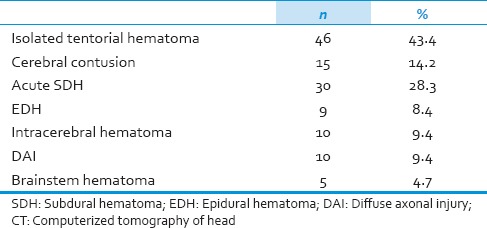
Of the 1,786 patients enrolled during the study period, 106 had tentorial hematoma on the initial CT head. There were 90 male and 16 female patients with mean age of 36.5 years (range 2-66 years). There were 46 patients in Grade 1, 34 in grade 2 and 26 in Grade 3 tentorial hematoma [Tables 1 and 2]. The mean admission GCS was 13, 11 and 8 in patients with grade I, II and III tentorial hematoma, respectively. Road traffic injuries (RTI) were the most common cause of head injury seen in 84 (79.24%) patients, followed by assault in 13 (12.3%). Fall from height accounted for only nine cases (8.4%). Among RTI, 84.5% (n = 71) were motorized two-wheeler injuries (63 wearing helmet) with four-wheeler injuries accounting for the remaining 15.5%.
Table 1.
Admission and discharge variables of patients with tentorial hematoma
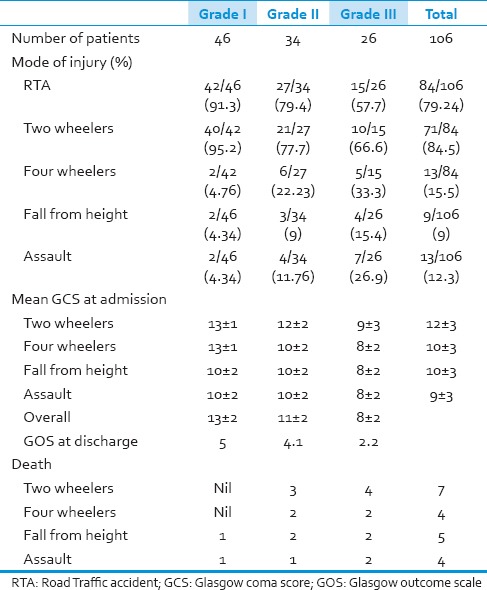
Table 2.
Associated CT findings in patients with tentorial hematoma
Of the 63 helmeted motorized two-wheeler injuries with tentorial hematoma, 37 (58.8%) had grade I hematoma. 22 (35%) had grade II hematoma and only 4 (6.3%) had grade III hematoma.
Management
Grade I tentorial hematoma group (n = 46)
Most patients (65.2%) were managed conservatively. Four patients required decompressive craniectomy following persistently high ICP (>20 mmHg) on ICP monitoring. Two patients died (unrelated to head injury).
Grade II tentorial hematoma group (n = 34)
Surgical intervention was done in 27 patients (six died subsequently) and only five patients were managed conservatively. Two additional patients were hemodynamically unstable and died before any intervention could be done.
Grade III tentorial hematoma group (n = 26)
Surgical intervention was done in 21 patients (5 died subsequently) and five patients were hemodynamically unstable and died before intervention could be undertaken.
Outcome
The mean GOS at the time of discharge was 5, 4.1 and 2.2 in patients with grade I, II and III tentorial hematoma, respectively. There were 20 deaths. Fifty percent (n = 10) of the deaths were in patients with grade III hematoma and 40% (n = 8) of the deaths were in patients with grade II hematoma. There were only two (10%) deaths in patients with grade I hematoma (both unrelated to head injury).
Discussion
The incidence of head injury is steadily increasing in developing countries with urbanization and increasing vehicular population. Road traffic injuries cause the majority of head injuries in civilian life and in our study too RTI was the most common cause of TBI, seen in 84 (79.24%) out of 106 cases. It is well known that two-wheeler riders are more prone for severe head injuries and fatalities.[3,4,5,6] Helmet use has been shown to dramatically decrease the severity of the head injury and most countries have legislations for compulsory use while riding two wheelers.[1,3,4,5,6,7,8,9] However, due to various reasons riders do not wear good quality helmets and even if they wear helmets, do not strap them on properly.[10] This negatives the advantages of a helmet leading to increased incidence and severity of TBI.
It is the senior authors (DA) observation that tentorial hematomas are commonly seen in head-injured patients wearing helmets. This study was undertaken to assess the incidence of tentorial hematoma and to see for possible correlation with helmet use. However, while designing the study, it was realised that an unequivocal definition of haematoma of the tentorium cerebelli in the literature is lacking. Tentorial cerebelli consists of the layers of the dura and has a free and fixed border. The most anteriorly placed fixed part, called the sphenopetrous ligament runs from the posterior clinoid process to the apex of the petrous part of the temporal bone and then runs bilaterally as a double-layered structure along the transverse sinuses ascending along the occipital bone to join the falx cerebri in the midline.[11] Blood may collect under the inferior surface, over the superior surface or between the two dural layers due to tearing of tentorial sinuses or bridging veins.[11,12] As tentorium may be normally slightly hyperdense, small hematomas are difficult to visualize. However, most hematomas appear are clearly seen as hyperdensity along the tentorial surface with a Hounsfield units (HU), typically being between 60 and 90 HU [Figures 1–3]. We therefore devised a simple grading system for tentorial hematomas. The grading system is very simple to apply and is based on the initial plain CT head. Repeat CT scans may not be accurate in grading the tentorial hematoma as in our experience the hematoma resolves quickly over 48-72 hours.
It is pertinent to note that tentorial hemotoma (of any grade) is rare in TBI population (5.9% in our study). The most significant finding of our study was the extremely high association of tentorial hematoma with helmet use (89%). However, as we excluded other forms of two wheelers (like bicycles-where helmet may not be worn as frequently), we are unable to draw conclusions on the incidence and pattern of isolated tentorial hematoma in non-helmeted injuries. Nevertheless, the fact that isolated tentorial hematoma was commonly seen in majority of helmeted patients (59%), suggests that although the helmet is offering protection against direct brain injury, transmission of rotational and indirect forces around the brainstem is still occurring resulting in the tentorial hematoma. A previous study by Richter et al. also showed that helmets decrease direct forces but are not able to sufficiently prevent indirect rotational forces.[1] This is a cause of concern and further changes in helmet design are warranted to decrease these forces.
Clinical outcomes at discharge was limited to GOS and this remains a limitation of this study. There were only two in-hospital mortalities in grade I tentorial hematomas, both these patients (one having history of fall from height and other with assault) had polytrauma and died of causes unrelated to head injury. There were eight deaths in grade II (of which three were two-wheeler riders). Maximum (n = 10) deaths in grade III tentorial hematomas. This suggests that our grading system can be easily applied in neurosurgical practise to predict outcome and for prognostication in these patients.
As we did not include patients without tentorial hematoma, comparisons cannot be made between the groups. However, the objective of this study was to see for any correlation of tentorial hematoma with helmet use and this was achieved in our study. We hope this study will encourage future studies to better elucidate the prognostic and clinical significance of tentorial bleed in head-injured patients.
Conclusions
Tentorial hematomas are extremely common in motorized two-wheeler riders especially in those wearing helmets and could be a marker for indirect forces such as rotational forces experienced while wearing helmets.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Richter M, Otte D, Lehmann U, Chinn B, Schuller E, Doyle D, et al. Head injury mechanisms in helmet-protected motorcyclists: Prospective multicenter study. J Trauma. 2001;51:949–58. doi: 10.1097/00005373-200111000-00021. [DOI] [PubMed] [Google Scholar]
- 2.Vielvoye GJ, Peters AC, Van Dulken H. Acute infratentorial traumatic subdural hematoma associated with a torn tentorium cerebelli in a one-year-old boy. Neuroradiology. 1982;22:259–61. doi: 10.1007/BF00342075. [DOI] [PubMed] [Google Scholar]
- 3.Talving P, Teixeira PG, Barmparas G, Dubose J, Preston C, Inaba K, et al. Motorcycle-related injuries: Effect of age on type and severity of injuries and mortality. J Trauma. 2010;68:441–6. doi: 10.1097/TA.0b013e3181cbf303. [DOI] [PubMed] [Google Scholar]
- 4.Weiss H, Agimi Y, Steiner C. Youth motorcycle-related hospitalizations and traumatic brain injuries in the United States in 2006. Pediatrics. 2010;126:1141–8. doi: 10.1542/peds.2010-0271. [DOI] [PubMed] [Google Scholar]
- 5.Weiss H, Agimi Y, Steiner C. Youth motorcycle-related brain injury by state helmet law type: United States, 2005-2007. Pediatrics. 2010;126:1149–55. doi: 10.1542/peds.2010-0902. [DOI] [PubMed] [Google Scholar]
- 6.Mitka M. Findings on youth injuries bolster case for helmet use by all motorcycle riders. JAMA. 2010;304:2683–4. doi: 10.1001/jama.2010.1811. [DOI] [PubMed] [Google Scholar]
- 7.Adeleye AO. Impact of motorcycle helmets and state laws on society's burden: A national study. Ann Surg. 2010;252:573–4. doi: 10.1097/SLA.0b013e3181f07e39. [DOI] [PubMed] [Google Scholar]
- 8.MacLeod JB, Digiacomo JC, Tinkoff G. An evidence-based review: Helmet efficacy to reduce head injury and mortality in motorcycle crashes: EAST practice management guidelines. J Trauma. 2010;69:1101–11. doi: 10.1097/TA.0b013e3181f8a9cc. [DOI] [PubMed] [Google Scholar]
- 9.Liu BC, Ivers R, Norton R, Boufous S, Blows S, Lo SK. Helmets for preventing injury in motorcycle riders. Cochrane Database of Systematic Reviews. 2008;1:CD004333. doi: 10.1002/14651858.CD004333.pub3. [DOI] [PubMed] [Google Scholar]
- 10.Zamani-Alavijeh F, Niknami S, Mohammadi E, Montazeri A, Ghofranipour F, Ahmadi F, et al. Motorcyclists' reactions to safety helmet law: A qualitative study. BMC Public Health. 2009;9:393. doi: 10.1186/1471-2458-9-393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ueyama T, Al-Mefty O, Tamaki N. Bridging veins on the tentorial surface of the cerebellum: A microsurgical anatomic study and operative considerations. Neurosurgery. 1998;43:1137–45. doi: 10.1097/00006123-199811000-00068. [DOI] [PubMed] [Google Scholar]
- 12.Muthukumar N, Palaniappan P. Tentorial venous sinuses: An anatomic study. Neurosurgery. 1998;42:363–71. doi: 10.1097/00006123-199802000-00097. [DOI] [PubMed] [Google Scholar]