Abstract
Background:
High spinal cord injury (HSCI) is one of the devastating traumatic injuries. 80% of these patients are young male, and 93% will have major neurological disabilities. There is a paucity of literature about prolonged bradycardia in HSCI patients. The aim of this study was to know the prevalence, risk factors, precipitating factors for prolonged bradycardia in the HSCI patients.
Materials and Methods:
All patients who were admitted to the Intensive Care Unit (ICU) of a tertiary hospital, with spinal cord injury above level of dorsal (D4) were enrolled in this study prospectively. Patient's demographic data, mechanism, level and type of spinal injury, associated injuries, injury severity score (ISS), spinal shock, vasopressors used, time of occurrence of bradycardia, treatment for bradycardia, precipitating as well as risk factors and outcome were recorded.
Results:
During the study period, a total of 138 patients were admitted to the ICU with HSCI. Majority of patients were male. The most frequently associated injury in these patients was skeletal fractures (38.4%). Most common complication was pneumonia 56 (41%). Forty-five (33%) of the total patients had prolonged bradycardia; 87% of these patients had pneumonia when bradycardia occurred. 53.4% had cardiac asystole. 29 (21%) patients had bradycardia at the time of endotracheal suctioning, whereas 27 (20%) patients developed bradycardia at the time of positioning. Majority of the patients were managed conservatively. Those HSCI patients who developed prolonged bradycardia, their ISS score was statistically higher, ICU and hospital stay was significantly higher compared with those HSCI patient who did not have prolonged bradycardia. Multivariate analysis revealed that hypotension on admission; pneumonia, and tracheostomy were risk factors for the development of prolonged bradycardia in HSCI patients.
Conclusion:
Prolonged bradycardia was associated with significantly higher incidence of asystole. Endotracheal suctioning and positioning of HSCI patients were significant provocative factors for prolonged bradycardia; hypotension on admission, pneumonia and tracheostomy were the risk factors for the development of prolonged bradycardia in these patients.
Key words: Asystole, atropine, autonomic nervous system, bradycardia, high spinal cord injury
Introduction
High spinal cord injuries (HSCIs) are one of the most serious traumatic injuries that occur to the human body. These injuries are caused by road traffic accidents (RTAs), fall, and fall of a heavy object (FOHO). HSCI has a serious pathological impact due to its involvement of central nervous as well as autonomic nervous system. The spinal cord involvement lead to a major neurological deficit, whereas autonomic nervous system due to sympathetic and parasympathetic imbalance causes life-threatening bradycardia, asystole, hypotension, ventricular and supraventricular tachycardia in initial days and hypertensive crisis in later stages. The combine effect of these both system involvement increases the morbidity and mortality in these patients.
Bradycardia is one of the most common cardiac abnormality in HSCI patients and can last longer than the usual period (>7 days), and it is termed as prolonged bradycardia.[1] It can progress to life threatening cardiac asystole. HSCI is being the spinal cord injury above fourth dorsal vertebra. It cut-off the sympathetic out flow and at the same time intact parasympathetic flow will take the upper hand, leading to parasympathetic dominance; which leads to various cardiac conduction abnormalities. The cardiac involvement can be acute or progress to chronic cardiac abnormalities leading to chronic cardiac disease. The cardiac disease is the most common cause of death in HSCI patients.[2] There is not enough literature about provocative and risk factors as well as management of prolonged bradycardia in HSCI patients.
The aim of this study was to know the prevalence, duration, risk factors, precipitating factors for prolonged bradycardia, and its association with pneumonia, positioning or endotracheal suction in the HSCI patients.
Materials And Methods
All patients who were admitted to the Intensive Care Unit (ICU) of the tertiary hospital with spinal cord injury above level of dorsal vertebra 4 from January 1995 to December 2010 were enrolled prospectively in this study.
Patient's demographic data, mechanism of injury (RTA, FOHO, fall from height, diving injury) and associated injuries (head injury, chest injury, multiple skeletal fractures), level and type of spinal injury, injury severity score (ISS), spinal shock, vasopressors used, time of occurrence of bradycardia, treatment of bradycardia, chest X-ray finding at the time of bradycardia, relation of bradycardia with endotracheal suctioning or patient's position, ICU stay, tracheostomy, and outcome were recorded. Patients with acute myocardial infraction without any history of trauma, traumatic cardiac arrest, and asystole due to other etiological reasons were excluded from this study.
Bradycardia was defined as documented heart rate of <50 beats/min. Hypotension was defined as the systolic blood pressure of <90 mm of Hg. Asystole was an acute event with severe bradycardia, followed by loss of pulse and blood pressure requiring cardiorespiratory resuscitation. Pneumonia was diagnosed as per Centre for Disease Control criteria. Medical therapy for bradycardia included the atropine, adrenaline and aminophylline. Vasopressors used were noradrenaline and dopamine. Any complications occurred during the study such as atrial fibrillation, pneumonia, pneumothorax, septic shock, multiorgan failure, acute renal failure, gastroparasis, paralytic ileus, gastrointestinal bleeding, bed sore, urinary tract infection and hyperthermia were recorded. Ethical approval was obtained for the study from Institutional Research Committee.
Statistical methods
Data were entered in IBM SPSS version 19.0 Statistical Package. Descriptive statistics in the form of frequency and percentages were calculated for categorical variables and mean ± standard deviation were calculated for interval variables. Chi-square tests were performed to see association between prolonged bradycardia versus no prolonged bradycardia for all the categorical variables, whereas Student's t-test and Wilcoxon's rank sum test, wherever applicable, were performed for interval variables. Logistic regression with enter method, taking important variables for prolonged bradycardia has been used to see risk factors and presented with adjusted odds ratios (OR) and 95% confidence interval (CI). Two-tailed P value has been considered for statistical significant level.
Results
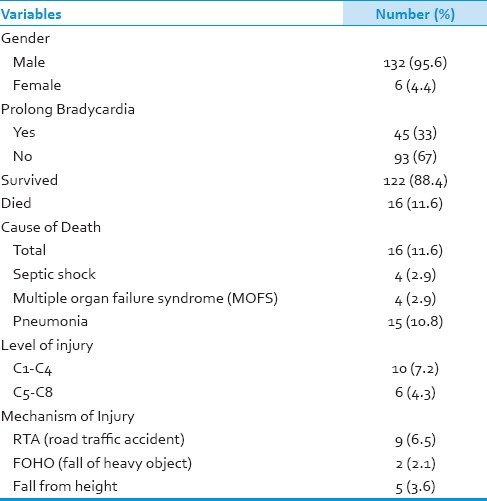
A total of 138 patients were admitted to the ICU with HSCI. Forty-five (33%) of them were having prolonged bradycardia. Majority of patients were males. Average ISS score was 37.4, and average age was 35.62 years. Total 16 (11.6%) patients were died. Majority of them 9 (65%) were involved in RTA, 15 (94%) had developed pneumonia, which lead to septic shock 4 (25%) patients with multiple organ failure, [Table 1].
Table 1.
Demographic characteristics and clinical findings
These HSCI was more common in the local population (22.5%), followed by Indians (19.6%), Nepali (13.8%) and Egyptians [Graph 1]. Most common mechanism for HSCI was RTA (60.9%), fall, FOHOs in 31.2% and 5.8% patients respectively [Figure 1]. The most frequently associated injury in these patients was skeletal fractures (38.4%), head injuries (37.7%) and chest trauma in 26.8% [Figure 1].
Graph 1.
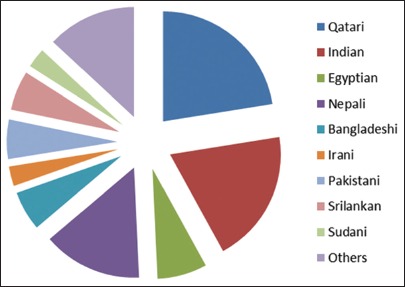
Patients division according to the nationality
Figure 1.
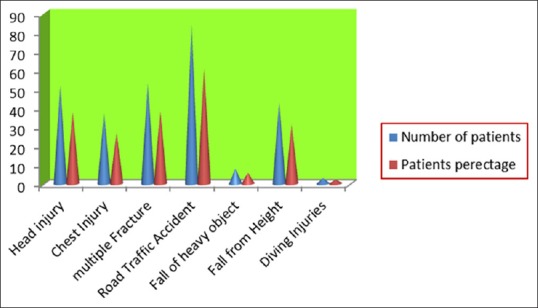
Mechanism and associated injury
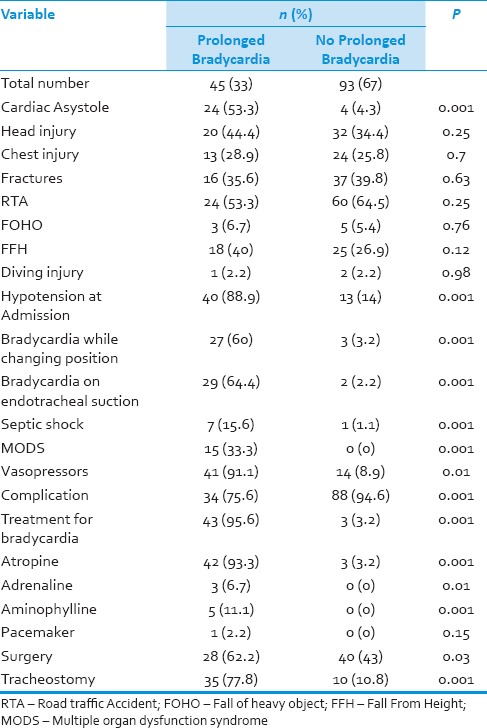
Table 2 shows that prolonged bradycardia patients had significantly higher asystole (53.3% vs. 4.3%, P = 0.001), hypotension (88.9% vs. 14%, P = 0.001). Significantly higher incidence of bradycardia while changing position (60% vs. 3.2%, P = 0.001), and endobronchial/endotracheal suctioning (64.4% vs. 2.2%, P = 0.001). Prolonged bradycardia group of patients required higher vasopressors to support their hemodynamic (91.1% vs. 8.9%, P = 0.001). Patients with prolonged bradycardia had significantly more complications (75.6% vs. 94.6%, P = 0.001). 95.6% patients received medical treatment in bradycardia group whereas; only 3.2% patients were given medical treatment in nonbradycardia group [Table 2].
Table 2.
Mechanism of injury and clinical parameters according to the prolonged bradycardia
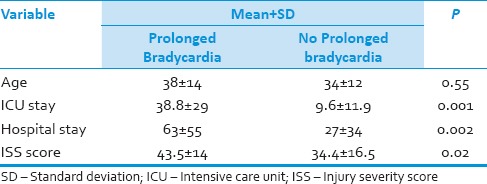
Prolonged bradycardia group patients had significantly higher ISS score (43.5 ± 14 vs. 34.4 ± 16.5, P = 0.02), significantly prolonged ICU (38.8 ± 29 vs. 9.6 ± 11.9, P = 0.001), and hospital stay (63 ± 55 vs. 27 ± 34, P = 0.002) than the nonbradycardia group [Table 3].
Table 3.
Interval characteristic according to prolonged bradycardia
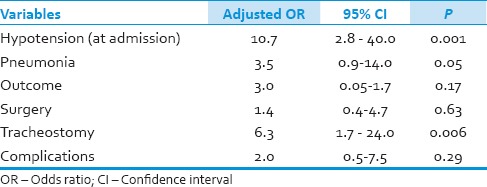
Multivariate analysis after adjusting important variables like pneumonia, outcome, surgery and complications revealed that hypotension (OR = 10.66, 95% CI = 2.8–40.6, P = 0.001), pneumonia (OR = 3.5, 95% CI = 0.9–14.0, P = 0.05) and tracheostomy (OR = 6.3, 95% CI = 1.67–23.5, P = 0.006) were the risk factors for the development of prolonged bradycardia in HSCI patients. Tracheostomy was performed 6 times more in prolonged bradycardia group patients than the nonbradycardia [Table 4].
Table 4.
Multivariate analysis and risk factors for bradycardia
In our study, the most common complication (40.57%) was pneumonia (50 patients), which lead to multi-organ failure (15 patients), septic shock in eight patients, gastrointestinal bleeding in four patients and bedsores in three patients [Figure 2].
Figure 2.
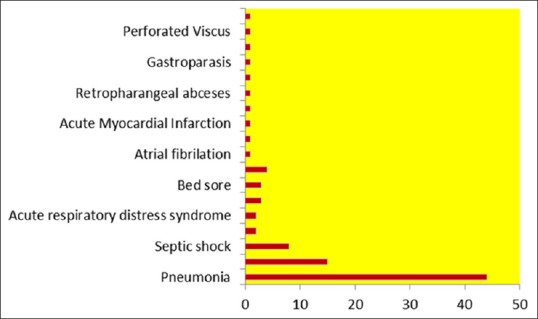
Medical complications
Discussion
High spinal cord injury is one of the major traumatic injuries. Eighty percent of these patients are young males, and 93% of them will have major neurological disabilities [Figure 3]. Hence, these injuries had a great financial impact on patient's family as well as the health care system.[2,3] These HSCI will cut-off the sympathetic nervous supply below the level of the injury; as the thoracolumbar sympathetic outflow occurs at the dorsal 1 (D1) to lumbar2 (L2) spinal level. The parasympathetic control is directly through vagus nerve and the preganglionic fibers synapse with the postganglionic parasympathetic neurons near the myocardium, whereas the sympathetic preganglionic neurons are situated within the lateral horns of D1-L2 in the spinal cord. When HSCI occur the sympathetic supply to the heart is cut, but parasympathetic control to the myocardium is intact. In the normal circumstances, autonomic control to the heart is balanced as sympathetic and parasympathetic supply antagonizes each other, and if one of them is absent other will dominate. It leads to the various cardiovascular abnormalities; these cardiovascular conduction disturbances are bradycardia, life-threatening cardiac arrhythmia, cardiac conduction defects, hypothermia and hypotension.[4] More higher the level of the spinal cord injury, involvement cardiovascular system will be more profound. Cardiovascular complication in HSCI patients are the leading factor for the increased morbidity and mortality.[2]
Figure 3.

X-ray neck with high spinal injury
The most frequent cardiac abnormality associated with HSCI is bradycardia. Initial bradycardia occurs in all patients with HSCI and spinal shock. When a patient recovers from spinal shock, the heart rate increases, commonly in 1-week (7 days) of injury, but in few patients bradycardia can persist up to 6 weeks.
Lehmann et al. found that bradycardia occurs in all patients with cervical spine injuries, and 15% of these patients will have cardiac asystole.[1] Moerman et al. also reported the same percentage of asystole.[5] In our study, 33% of these HSCI had prolonged bradycardia. About 53% of the prolonged bradycardia patients had asystole. The time of onset and duration of bradycardia is variable, and it is not well-standardized in the literature; there is a paucity of literature available about prolonged bradycardia. Piepmeier et al. reported high incidence of bradycardia up to 5 postinjury days and then declines rapidly in HSCI patients.[6] Moerman et al. described mean time of bradycardia 5–7 days and 15% of them had asystole. Franga et al. reported that 16% of their patients had asystole.[7]
Our study reconfirms that the endotracheal suctioning and positioning of HSCI patients is significantly associated with bradycardia and asystole. HSCI patients will have increased bronchial secretions as a result of vagal dominance or bronchial infection hence requiring frequent bronchial suctioning as well as positioning. Normal response to this maneuver is tachycardia, but in HSCI patient parasympathetic dominance leads to bradycardia and cardiac asystole; because of this etiological reseasons; the use of ipatropium bromide may decrease the incidence of bradycardia and asystole.[8] HSCI patients are at an increased risk for the development of pneumonia, and it is the most frequent complication in our study. HSCI or more higher the level of spinal injury, higher will be a risk of pneumonia, as these patients are unable to clear the bronchial secretions; due to weaker cough reflex as a result of weakness or paralysis of the muscles of respiration. Net result of all these is retention of bronchial secretions, thickening of the secretion, atelectasis and development of pneumonia.[9] In our study, pneumonia was the major risk factor for the development of prolonged bradycardia and asystole in HSCI patients. In HSCI patients the normal response to hypoxia is absent due to absent sympathetic flow, so when these patients develops pneumonia and hypoxia as the pulmonary inflation reflex is absent there will be no tachycardia, but dominant parasympathetic flow will cause bradycardia and asystole.[6,10]
Gilgoff et al. reported a case of HSCI, who developed pneumonia and complicated by bradycardia requiring pacemaker and Holter monitoring; and with interrogation of Holter monitoring it revealed that there was seven-fold increased in pace maker activity indicating that the pneumonia causing increased incidence of life-threatening bradycardia and asystole.[11]
Our study demonstrated that the pneumonia was a significant risk factor for prolonged bradycardia and asystole with the odd ratio of 3.48% and 95% CI: (0.88-14.2) [Table 4]. In this study, we also found that initial spinal shock and tracheostomy are also significant risk factors for the development of prolonged bradycardia and cardiac asystole. Spinal shock or hypotension on admission occurs in HSCI patients occurs due to the decreased vascular tone as a consequence of afferent sympathetic pathway disruption, vasodilatation, absence of reflex tachycardia, in combination with direct negative inotropic vagal effect on the myocardium.[7] Spinal cord injury patients will require a tracheostomy to support respiration and ventilation. The need for tracheostomy is significantly higher in patients with HSCI.[12] We found a significant correlation between tracheostomy and occurrence of prolonged bradycardia and asystole. This might be due to the combine effect of high injury level, higher incidence of pneumonia, more bronchial secretion requiring more suctioning as well as positioning of these patients.
Majority of our patients had medical management for bradycardia and asystole, which included atropine sulfate, adrenaline and aminophyline. Only one patient had pace maker insertion, and it has been removed due to infection. Our patients responded well to the medical therapy, but the incidences of asystole were higher, may be related to the medical therapy as well as higher incidence of pneumonia. Recent literature dictates that the pacemaker in HSCI patients to prevent life-threatening bradycardia and asystole.[13] cardiac pace maker insertion is not free from complications, such as death, failure to pace and infection. One has to weight the risk against benefits; Franga et al. found that risk are relatively minimal when compared with benefits in HSCI patient in the prevention of life-threatening bradyarrhythmia and asystole.[7] Overall mortality of HSCI in our study was 11.6%, which is comparable with that described in the literature[13,14] All patients with the worst outcome had prolonged bradycardia and a significant percentage (95.4%) of them had pneumonia; which lead to septic shock and multi-organ failure. In spite of prolonged bradycardia, higher incidence of asystole and pneumonia, the morality was 34%.
Future larger studies are needed with comparison of pace maker and medical therapy, Preventive measures such as, initial use of ipatropium bromide nebulization, kinetic rotation therapy.
Conclusion
High spinal cord injury remains a serious life threatening trauma, as it involves both central nervous system as well as autonomic nervous system. Bradycardia was the most common life-threatening arrhythmia occurring in these patients. It can progress to the cardiac asystole. Significant percentage of HSCI patients can have prolonged bradycardia and asystole after a week of injury. Prolonged bradycardia in HSCI patients is associated with significant higher incident of asystole. Endotracheal suctioning and positioning of HSCI patients were significant provocative factors for prolonged bradycardia. We found that hypotension on admission, pneumonia, and tracheostomy were the significant risk factors for the development of prolonged bradycardia in HSCI patients. Majority of our patients responded well to the medical therapy, with slight higher incidence of asystole; but mortality was comparable. Pneumonia was a significant risk factor for mortality in HSCI patients. In our study in spite of significant prolonged bradycardia and a higher incidence of asystole, the outcome was comparable.
Key points
Road traffic accident was common etiology, and skeletal injury was most frequently associated injury in HSCI patients
Prolonged bradycardia in HSCI patients is associated with significantly increased incidence of asystole
Endotracheal suctioning and positioning of HSCI patients are provocative for bradycardia
Spinal shock, pneumonia and tracheostomy are the significant risk factors for the development of prolonged bradycardia in HSCI patients
Prolonged bradycardia significantly increases the ICU as well as hospital stay of HSCI patients
In spite of the higher incidence of prolonged bradycardia and asystole; medical management was effective.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Lehmann KG, Lane JG, Piepmeier JM, Batsford WP. Cardiovascular abnormalities accompanying acute spinal cord injury in humans: Incidence, time course and severity. J Am Coll Cardiol. 1987;10:46–52. doi: 10.1016/s0735-1097(87)80158-4. [DOI] [PubMed] [Google Scholar]
- 2.Grigorean VT, Sandu AM, Popescu M, Iacobini MA, Stoian R, Neascu C, et al. Cardiac dysfunctions following spinal cord injury. J Med Life. 2009;2:133–45. [PMC free article] [PubMed] [Google Scholar]
- 3.McMahon D, Tutt M, Cook AM. Pharmacological management of hemodynamic complications following spinal cord injury. Orthopedics. 2009;32:331. doi: 10.3928/01477447-20090502-07. [DOI] [PubMed] [Google Scholar]
- 4.Krassioukov AV, Karlsson AK, Wecht JM, Wuermser LA, Mathias CJ, Marino RJ, et al. Assessment of autonomic dysfunction following spinal cord injury: Rationale for additions to International standards for neurological assessment. J Rehabil Res Dev. 2007;44:103–12. doi: 10.1682/jrrd.2005.10.0159. [DOI] [PubMed] [Google Scholar]
- 5.Moerman JR, Christie B, 3rd, Sykes LN, Vogel RL, Nolan TL, Ashley DW. Early cardiac pacemaker placement for life-threatening bradycardia in traumatic spinal cord injury. J Trauma. 2011;70:1485–8. doi: 10.1097/TA.0b013e3182185509. [DOI] [PubMed] [Google Scholar]
- 6.Piepmeier JM, Lehmann KB, Lane JG. Cardiovascular instability following acute cervical spinal cord trauma. Cent Nerv Syst Trauma. 1985;2:153–60. doi: 10.1089/cns.1985.2.153. [DOI] [PubMed] [Google Scholar]
- 7.Franga DL, Hawkins ML, Medeiros RS, Adewumi D. Recurrent asystole resulting from high cervical spinal cord injuries. Am Surg. 2006;72:525–9. [PubMed] [Google Scholar]
- 8.Dicpinigaitis PV, Spungen AM, Bauman WA, Absgarten A, Almenoff PL. Bronchial hyperresponsiveness after cervical spinal cord injury. Chest. 1994;105:1073–6. doi: 10.1378/chest.105.4.1073. [DOI] [PubMed] [Google Scholar]
- 9.Jackson AB, Groomes TE. Incidence of respiratory complications following spinal cord injury. Arch Phys Med Rehabil. 1994;75:270–5. doi: 10.1016/0003-9993(94)90027-2. [DOI] [PubMed] [Google Scholar]
- 10.Sanghvi AV, Chhabra HS, Nigam V, Tandon V, Mascarenhas AA. Permanent cardiac pacemaker for cardiac arrest following cervico-dorsal spinal injury. Eur Spine J. 2009;18(Suppl 2):254–7. doi: 10.1007/s00586-009-0944-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gilgoff IS, Ward SL, Hohn AR. Cardiac pacemaker in high spinal cord injury. Arch Phys Med Rehabil. 1991;72:601–3. [PubMed] [Google Scholar]
- 12.Como JJ, Sutton ER, McCunn M, Dutton RP, Johnson SB, Aarabi B, et al. Characterizing the need for mechanical ventilation following cervical spinal cord injury with neurologic deficit. J Trauma. 2005;59:912–6. doi: 10.1097/01.ta.0000187660.03742.a6. [DOI] [PubMed] [Google Scholar]
- 13.Rangappa P, Jeyadoss J, Flabouris A, Clark JM, Marshall R. Cardiac pacing in patients with a cervical spinal cord injury. Spinal Cord. 2010;48:867–71. doi: 10.1038/sc.2010.48. [DOI] [PubMed] [Google Scholar]
- 14.Bilello JF, Davis JW, Cunningham MA, Groom TF, Lemaster D, Sue LP. Cervical spinal cord injury and the need for cardiovascular intervention. Arch Surg. 2003;138:1127–9. doi: 10.1001/archsurg.138.10.1127. [DOI] [PubMed] [Google Scholar]


