Abstract
Bilateral abducens and facial palsy following head injury are extremely rare. We present a patient with post-traumatic bilateral facial and abducens palsy. There were bitemporal fractures that did not correspond with the facial canal. Despite complete facial palsy with axonal degeneration and > 90% facial muscle degenervation, conservative management helped. This report highlights the importance of conservative management in post-traumatic complete facial palsy especially when the fracture line does not correspond with the facial canal.
Key words: Bilateral abducens palsy, bilateral facial palsy, post-traumatic
Introduction
Involvement of abducens and facial nerve (immediate and delayed) following head injury is not uncommon. However, immediate onset, bilateral abducens, and facial nerve involvement after a relatively minor head injury is extremely rare.[1,2] The usual line of management is surgical especially in the presence of immediate and complete facial palsy.[3] However, we managed a patient conservatively with gratifying results.
Case Details
A 26-year-old man was peeping out of the window of a moving bus when he accidently hit a lamp post. Following a brief period of unconsciousness he came to the hospital walking. He had left ear otorrhoea, double vision, and inability to close his eyes. He was fully alert and oriented. Examination revealed complete bilateral lower motor facial paresis (House-Brackmann grade V) with bilateral abducens palsy [Figure 1a]. Rest of the neurological examination was unremarkable. Computed tomogram (CT) showed an oblique fracture of the left petrous and right longitudinal petrous fracture extending into the temporal squama with pneumocephalus [Figure 2a–c]. MRI ruled out injury to brainstem [Figure 2d–f]. Series of thin slices of CT skull base were studied to rule out other injuries apart from those described [Figure 3]. Pure tone audiometry showed mild conductive hearing loss of the left ear and mild mixed hearing loss on the right side. The fractures were unable to explain the facial paresis. He was given a course of steroids (60 mg of prednisolone/day for 1 week tapered gradually over next 3 weeks) along with oral methycobalamine (1000 microgram everyday for 12 weeks). Facial message was advised. The electroneuronography was performed 6 weeks later that showed axonal degeneration of both facial nerves. Three months later he showed complete recovery of bilateral abducens and partial improvement of left facial nerve [Figure 1b]. Electroneuronography at 3 months post injury showed no improvement in facial nerve conduction. Six months after the injury he had completed the recovery of bilateral facial paresis as well [Figure 1c]. Electrophysiololgical studies were not done at this point of time.
Figure 1.
(a) Immediate post injury shows bilateral abducens palsy with inability to close bilateral eyes due to bilateral facial palsy; (b) After 3 months showing improvement in bilateral abducens but no improvement in bilateral facial palsy; (c) After 6 months showing complete recovery of bilateral facial (ability to smile and close both eyes)
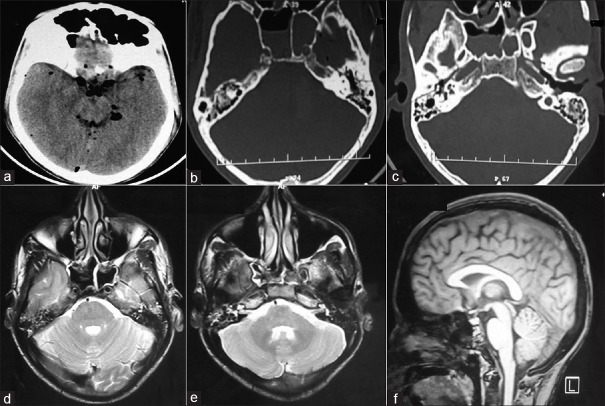
Figure 2.
(a) CT head following injury showing pneumocephalus; (b) Longitudinal fracture along right petrous (bone window axial) and (c) Oblique fracture along left petrous (bone window axial); (d and f) MRI (T2 axial and T1 sagittal) showing normal brain stem
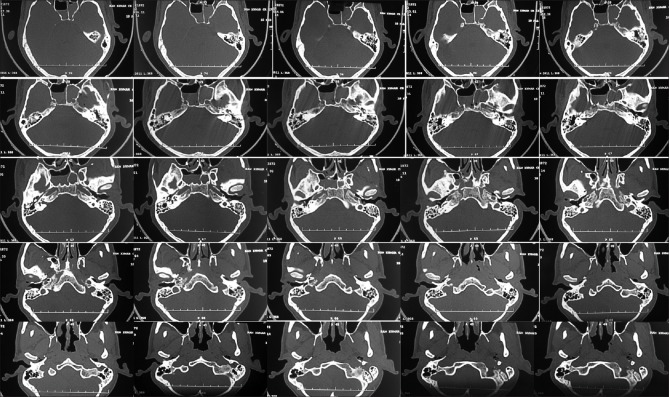
Figure 3.
Thin slices of CT of the skull base
Discussion
Isolated facial or abducens nerve palsy is not uncommon in head injured patients. Incidence of sixth nerve injury is around 2.7% of head trauma patients, 10% of whom have bilateral involvement.[2] The long intracranial course of the nerve along with its rigid intracavernous attachment has been attributed to its vulnerability. The nerve may be impacted against the Gruber's (petrosphenoidal) ligament following an upward thrust or is injured when it impacts against the ridge of the petrous pyramid. Alternatively, the nerve trunk may be contused at its entry point through the dural opening into Dorello's canal.[2]
The facial nerve is the second most commonly damaged cranial nerve, being involved in 1% to 3% of head-injured patients. The common site of injury is within the facial nerve canal. The occurrence of facial nerve paralysis depends upon the type of temporal bone fracture and its incidence is 20% with longitudinal fractures and 50% in transverse fractures.[2] Intraneural hematoma (40-50%), nerve disruption (9-26%), contusion (36%), or impinging bone fragments may cause its dysfunction. Furthermore, the facial nerve is relatively fixed at geniculate ganglion where it is tethered by greater superficial petrosal nerve and may the site of injury. The meatal foramen due to its narrow size in the labyrinthine segment is another potential site of facial nerve compression especially in the presence of edema or hematoma. The mechanism of facial nerve injury in our case cannot be attributed to temporal bone fracture as the fracture line is much higher for facial nerve path.[2]
Combined bilateral facial and abducens palsy is very rare and there is very limited literature available regarding this.[1,2] Lateral crush injuries or contact loading giving rise to bitemporal fractures have been attributed. Occasionally, subarachnoid blood and hematoma around the clivus may give rise to cranial nerve involvement due to vasospasm. Edema or pneumocephalus may be the cause of bilateral 6th and 7th nerve involvement in the index case, though it remains speculative.
The management of traumatic facial nerve injuries is controversial and must be individualized for each patient. The indications and timing of surgical exploration are issues that continue to be debated. Surgical exploration is indicated when within 6 days of onset of paralysis and the denervation of facial muscles is greater than 90%. Surgery is also indicated when the nerve is 100% degenerated when first seen and there is clear fracture of facial canal.[3] Conservative management is indicated for 6-12 months if no fracture is seen on CT.[3] Both the cases described by Kobayashi and Lee were operated upon.[1,2]
We feel that even in case of complete facial palsy with denervation greater than 90% it is better to wait, especially if the temporal fractures do not lie along the facial canal. The usual time for the wallerian degeneration and then the time taken for regeneration is approximately 6 months. In case there is no improvement even after 6 months, the canal may be explored. In case the fracture line lies along with the facial canal, it can be explored earlier especially in case of complete paresis.
Abducent nerve being pure motor and innervating a single muscle usually recover spontaneously.[4] Apart from this the patient being an young individual may behave differently from the older ones.
Conclusion
Bilateral facial and abducens palsy associated with blunt head trauma and without any correlative radiological findings is a rare presentation. In such cases, facial nerve recovery is the major concern, as abducens nerve palsy usually recovers spontaneously. Conservative line of management is a better option in the absence of fracture corresponding with the facial canal, especially in the presence of some clinical improvement even though the electrophysiological studies may not suggest improvement. More credence should be given to clinical improvement than to electrophysiological studies for deciding between surgical and conservative management.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Kobayashi S, Yokota H, Nakazawa S. A case of crushing head injury showing bilateral abducens, facial and acoustic nerve palsies. No Shinkei Geka. 1988;16:869–73. [PubMed] [Google Scholar]
- 2.Lee GY, Halcrow S. Petrous to petrous fracture associated with bilateral abducens and facial nerve palsies: A case report. J Trauma. 2002;53:583–5. doi: 10.1097/00005373-200209000-00034. [DOI] [PubMed] [Google Scholar]
- 3.Darrouzet V, Duclos JY, Liguoro D, Truilhe Y, De Bonfils C, Bebear JP. Management of facial paralysis resulting from temporal bone fractures: Our experience 115 cases. Otolaryngol Head Neck Surg. 2001;125:77–84. doi: 10.1067/mhn.2001.116182. [DOI] [PubMed] [Google Scholar]
- 4.Yanamadala V, Walcott BP, Nahed BV, Coumans JV. Delayed post-traumatic bilateral abducens nerve palsy with complete recovery. J Clin Neurosci. 2012;19:585–6. doi: 10.1016/j.jocn.2011.09.007. [DOI] [PubMed] [Google Scholar]