Abstract
Aging is associated with decreased aerobic fitness and cardiac remodeling leading to increased risk for cardiovascular disease. High-intensity interval training (HIIT) on the treadmill has been reported to be more effective in ameliorating these risk factors compared with moderate-intensity continuous training (MICT) in patients with cardiometabolic disease. In older adults, however, weight-bearing activities are frequently limited due to musculoskeletal and balance problems. The purpose of this study was to examine the feasibility and safety of non-weight-bearing all-extremity HIIT in older adults. In addition, we tested the hypothesis that all-extremity HIIT will be more effective in improving aerobic fitness, cardiac function, and metabolic risk factors compared with all-extremity MICT. Fifty-one healthy sedentary older adults (age: 65±1 years) were randomized to HIIT (n=17), MICT (n=18) or non-exercise control (CONT; n=16). HIIT (4×4 minutes 90% of peak heart rate; HRpeak) and isocaloric MICT (70% of HRpeak) were performed on a non-weight-bearing all-extremity ergometer, 4x/week for 8 weeks under supervision. All-extremity HIIT was feasible in older adults and resulted in no adverse events. Aerobic fitness (peak oxygen consumption; VO2peak) and ejection fraction (echocardiography) improved by 11% (P<0.0001) and 4% (P=0.001) respectively in HIIT, while no changes were observed in MICT and CONT (P≥0.1). Greater improvements in ejection fraction were associated with greater improvements in VO2peak (r=0.57; P<0.0001). Insulin resistance (homeostatic model assessment) decreased only in HIIT by 26% (P=0.016). Diastolic function, body composition, glucose and lipids were unaffected (P≥0.1). In conclusion, all-extremity HIIT is feasible and safe in older adults. HIIT, but not MICT, improved aerobic fitness, ejection fraction, and insulin resistance.
Keywords: High-intensity interval training, moderate-intensity continuous training, aerobic fitness, cardiac function, metabolic risk factors, aging
1. Introduction
Aging induces cardiac remodeling and changes in cardiac function that lead to increased risk of cardiovascular disease (CVD) (Fleg and Strait 2012). Improving aerobic fitness lowers the risk of CVD mortality (Lee et al. 2011), however, the optimal training regimen for improving aerobic fitness in older adults remains undefined. High-intensity interval training (HIIT) has been reported to have superior effects on aerobic fitness, cardiac function, lipids and glucose control compared with moderate-intensity continuous training (MICT) in patients with cardiometabolic disease (Molmen-Hansen et al. 2012; Rognmo et al. 2004; Tjonna et al. 2008; Wisloff et al. 2007). The HIIT protocol in these studies consists of 4-min intervals of high-intensity treadmill walking (usually “uphill”) interspersed with periods of moderate-intensity walking. However, older adults frequently experience balance and musculoskeletal problems (Gheno et al. 2012) which limit the feasibility of weight-bearing exercise and in particular high-intensity treadmill walking. Development of an alternative exercise modality for HIIT that avoids the age-related limitations of treadmill walking is necessary for older adults. The use of a stationary cycle eliminates balance and weight-bearing concerns, and is likely to be more suitable as a long-term exercise routine for older adults. More importantly, use of an all-extremity ergometer increases the active amount of muscle mass during exercise compared to lower extremity exercise, allows compensation for unilateral or bilateral lower extremity weakness or fatigue, and ultimately affords a larger proportion of older individuals to undergo HIIT.
Therefore, we sought to evaluate the feasibility and safety of performing HIIT on a non-weight-bearing all-extremity ergometer in previously sedentary older adults. In addition, we tested the hypothesis that 8 weeks of all-extremity HIIT will be more effective in improving aerobic fitness, cardiac function, and metabolic risk factors compared with all-extremity MICT in healthy sedentary older adults.
2. Methods
2.1. Subjects
Subjects were 55–79 years old, sedentary, non-smokers who were free of cardiovascular and other major clinical disease (e.g., diabetes, liver and renal disease) as assessed by medical history, physical examination, resting blood pressure, ECG and blood analysis (i.e., comprehensive metabolic panel, lipid panel, insulin, and complete blood count with differential). In addition, all subjects demonstrated normal ECG and blood pressure responses to a clinically-supervised diagnostic graded exercise treadmill test. Prior to study enrollment, subjects were weight stable (<5% change in body weight) for at least 6 months, were not on hormone replacement therapy (e.g., estrogen, progesterone or testosterone) for at least 2 years, and female subjects were postmenopausal for at least 2 years. Subjects who were on a stable drug regimen for lipid and blood pressure control were enrolled in the intervention, but were required not to change their use of medication during study participation.
The study was approved by the Institutional Review Board of the University of Florida and was carried out in accordance with the ethical standards of the Declaration of Helsinki. The purpose, nature and risks of the study procedures were explained to the subjects and questions were answered prior to obtaining written informed consent.
2.2. Study design
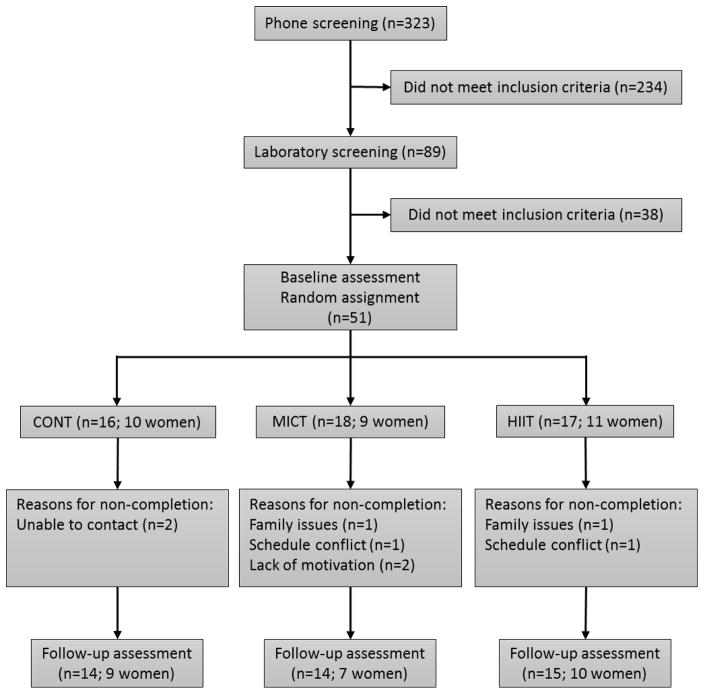
The study used a randomized controlled parallel group design which included two exercise groups (HIIT and MICT) and a non-exercise control group (CONT). Subjects were recruited and screened according to the study inclusion/exclusion criteria. Subject enrollment to the study was performed by E.M.H. who provided on site clinical support in consultation with J.W.P. Subjects who met the enrollment criteria for the intervention (n=51) completed the baseline assessment and were then randomized to HIIT (n=17), MICT (n=18) or CONT (n=16) (Figure 1). Randomization was based on a computer random-number generator and was stratified by baseline peak oxygen consumption (VO2peak, L/min). Subjects were instructed not to alter their diet during study participation. Subjects were also asked not to change their normal physical activity habits with the exception of the scheduled exercise sessions. Outcome assessments were performed at baseline and after the 8-week intervention by the same researchers while strictly adhering to established standard operating procedures. Individual subject data were coded to ensure blinding during data analysis. Study procedures and exercise training were performed at the Integrative Cardiovascular Physiology Laboratory, in the Center for Exercise Science, at the University of Florida.
Figure 1.
Study flow chart.
2.3. Exercise intervention
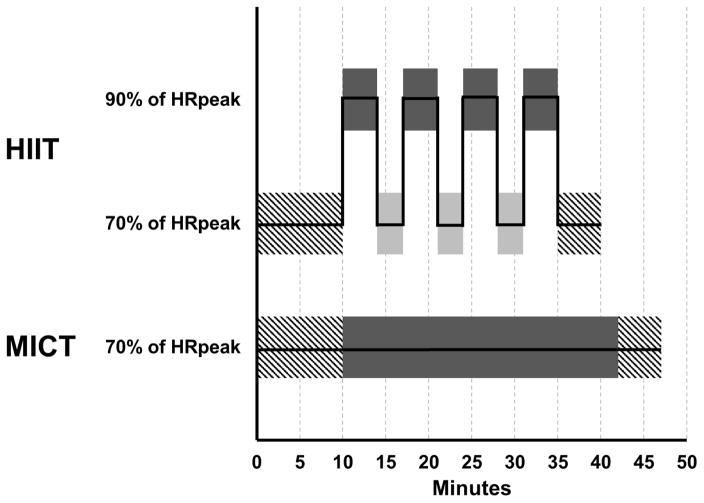
Subjects assigned to HIIT and MICT performed synchronous arm and leg exercise on a non-weight-bearing all-extremity air-braked ergometer (Airdyne model AD4, Schwinn), 4 days/week for 8 weeks, under the direct supervision of an exercise physiologist. HIIT consisted of 4×4 minute intervals at 90% of peak heart rate (HRpeak) interspersed by 3×3 minute active recovery periods at 70% of HRpeak for a total of 25 minutes, while MICT consisted of 32 minutes at 70% of HRpeak (Figure 2). These specific HIIT and MICT protocols were designed by Tjonna et al to provide equal caloric expenditure (Tjonna et al. 2008). A 10-minute warm-up and a 5-min cool-down at 70% of HRpeak was included prior to and at the end of each exercise session, respectively, for both HIIT and MICT as previously described (Tjonna et al. 2008). HRpeak was determined during the baseline maximal graded exercise test.
Figure 2.
Exercise protocol for high-intensity interval training (HIIT) and moderate-intensity continuous training (MICT) performed on an all-extremity non-weight-bearing ergometer. After a 10-minute warm-up at moderate intensity (65 to75% of peak heart rate, HRpeak; hatched bar), subjects in HIIT performed 4×4-minute bouts of exercise at high intensity (85 to 95% of HRpeak; dark solid bar) separated by 3-minute active recovery at moderate intensity (65 to 75% of HRpeak; light solid bar), while participants in MICT performed 32 minutes of exercise at moderate intensity (65 to 75% of HRpeak; dark solid bar). All study participants performed a 5-minute cool-down at moderate intensity (65 to 75% of HRpeak; hatched bar).
Exercise heart rate was displayed and recorded during each exercise session using a heart rate telemetry system (Polar Team 2 Pro, version 1.4.3). Subjects were instructed to reach target heart rate by modifying the speed of their arm and leg movement. Because subjects were sedentary and were unfamiliar to exercising on a non-weight-bearing all-extremity ergometer, a period of familiarization/pre-conditioning was completed prior to the 8-week intervention. The preconditioning sessions consisted of gradually increasing the duration of exercise as tolerated until subjects were able to perform 40 minutes of continuous all-extremity exercise at 70% of HRpeak. On average, 5±1 sessions of preconditioning were required to reach this goal.
2.4. Study procedures
2.4.1. Aerobic fitness, HRpeak and caloric expenditure of HIIT and MICT
Maximal oxygen consumption (VO2max) was measured using computer-assisted open-circuit spirometry during a maximal graded exercise test on the treadmill as we have previously published (Christou et al. 2005; Hwang et al. 2013). The protocol was individually-customized and consisted of a warm up of 6 minutes of horizontal walking at a speed corresponding to 70~80% of the age-predicted maximal heart rate, followed by grade increases of 2.5% every 2 minutes until volitional exhaustion. For each subject identical protocols were used during their baseline and follow-up assessments. Attaining three of the following four criteria defined VO2max: a) a plateau in oxygen consumption (<100 mL/min) with increasing exercise intensity; b) a maximal respiratory exchange ratio of at least 1.15; c) achievement (±10bpm) of age-predicted maximal heart rate (220-age); and d) a rating of perceived exertion of at least 18 on the Borg scale. These criteria were not met in all subjects, therefore the term VO2peak instead of VO2max will be used.
Oxygen consumption was also measured during a bout of all-extremity HIIT and MICT. Caloric expenditure for HIIT and MICT was calculated by using the caloric equivalent per 1 L of oxygen consumed based on the steady state respiratory exchange ratio.
2.4.2. Cardiac function
Transthoracic echocardiography was performed while subjects rested in the left lateral decubitus position using an ultrasound system (Aplio XV, Toshiba Medical Systems, Tokyo, Japan) equipped with a sector cardiac transducer (2–5 MHz). Cardiac measures were obtained according to the American Society of Echocardiography recommendations (Gottdiener et al. 2004; Lang et al. 2005). M–mode images of the left ventricle (LV) were obtained in the parasternal short-axis views at the midventricular level to measure wall thickness and internal dimensions. LV mass was calculated using the formula:
where LVIDd is LV internal diameter during diastole, PWTd is posterior wall thickness during diastole and SWTd is septal wall thickness during diastole. Parasternal long axis images were obtained to assess LV outflow tract. Apical four- and two-chamber views were obtained to determine ejection fraction using the Simpson’s biplane method. Peak early (E) and atrial (A) filling velocities, and deceleration time (DT) were determined by pulsed-wave Doppler at the level of the mitral valve leaflet tips. Peak early (e′) and late (a′) velocity of the medial and lateral mitral annulus were measured by tissue Doppler and then averaged. Each measure was calculated from the average of 3 cardiac cycles.
2.4.3. Body composition
Subjects were dressed in light clothing and were barefoot during these measures. Height was measured to the nearest mm using a stadiometer and the average of three measures was used in the analyses. Body weight was measured to the nearest 0.1 kg using an electronic scale (Tanita, Arlington Heights, IL, USA). Body mass index was determined as weight divided by height squared (kg/m2). Fat and fat-free mass and % body fat were estimated from a whole body scan using dual-energy x-ray absorptiometry (Lunar Prodigy Advance, GE, version 8.70.005) as we have previously described (Hwang et al. 2013).
2.4.4. Lipids, glucose and insulin
Fasting blood samples were analyzed by a clinical laboratory using standard procedures; blood lipids and glucose were assessed using spectrophotometry and insulin was assessed using an immunoassay. Insulin resistance was evaluated using the homeostasis model assessment of insulin resistance (HOMA-IR) (Matthews et al. 1985) as follows:
2.4.5. Resting blood pressure
Blood pressure was measured over the brachial artery using an automated oscillometric device (Dynamap GE) while the subject rested seated. An average of three measures was used in the analysis.
2.4.6 Habitual physical activity
Habitual physical activity was assessed using a triaxial accelerometer (ActiGraph GT3X, software version 5.10.0). Subjects were instructed to wear the accelerometer over the right iliac crest along the midaxillary line for 4 consecutive days consisting of 3 weekdays and 1 weekend day. Non-wear time was defined as ≥ 60 minutes of continuous zero count data and the minimum wear time for inclusion was set at ≥10 hours/day based on published criteria for monitoring physical activity in older adults (Gorman et al. 2014).
2.5. Statistical analyses
Statistical analyses were performed using SPSS Statistics (Version 23, Chicago, IL). Analysis of variance with repeated measures was used to test the group (HIIT, MICT and CONT) by time (baseline vs. follow-up) interaction and one-way analysis of variance was used to compare differences at baseline among the three groups. Post hoc tests were corrected for multiple comparisons using the Bonferroni correction. Secondary analysis was performed using analysis of covariance to determine whether baseline values influenced the results of the intervention. Simple linear regression was used to evaluate relations of interest. Statistical significance for all analyses was set at α=0.05. Data are presented as mean±SE.
3. Results
3.1. Feasibility and safety of novel non-weight-bearing all-extremity HIIT
Previously sedentary older adults completed 8 weeks of HIIT or MICT using synchronous arm and leg exercise on a non-weight-bearing air-braked ergometer. No adverse events occurred in HIIT or MICT groups (i.e., deaths, nonfatal serious events such as myocardial infarction and musculoskeletal problems, or other serious or non-serious health issues requiring hospitalization or medical treatment). However, during the first few HIIT or MICT exercise sessions the majority of subjects reported complaints regarding the seat of the ergometer being uncomfortable. This was resolved by wearing padded clothing designed for cycling or by allowing time for subjects to become accustomed to the ergometer. Of the 51 subjects who were randomized, 16 % did not complete the study for reasons unrelated to the intervention as described in figure 1. An equal number of men and women dropped out of the study.
The caloric expenditure was similar with HIIT and MICT (224±14 vs. 234±14 kcal per session, P=0.6). Subjects completed 88±3% and 89±4% of the scheduled exercise sessions of HIIT and MICT, respectively (P=0.8). Reasons for non-attendance were not directly related to the exercise intervention.
3.2. Subject baseline values
There were no differences in baseline measures among HIIT, MICT and CONT (Tables 1, 2, 3 and 4; P>0.05). Although baseline VO2peak might appear to be unequal among the three groups, there was no statistically significant difference (P=0.4). Habitual physical activity was also not different among the groups (P≥0.6; Table 1) and remained unchanged throughout the intervention, after adjusting for activity performed during the supervised exercise sessions (P=0.1 for counts/min/day and P=0.8 for steps/day; data not shown). Therefore, the results can be attributed to the intervention rather than to baseline differences in VO2peak or increases in the overall habitual physical activity level during study participation.
Table 1.
Baseline subject characteristics.
| CONT n=14 | MICT n=14 | HIIT n=15 | |
|---|---|---|---|
| Age, years | 63.8±1.6 | 65.6±1.8 | 64.8±1.4 |
| Body weight, kg | 73.2±4.5 | 76.8±2.7 | 73.0±3.7 |
| Body mass index, kg/m2 | 26.7±1.4 | 28.7±1.0 | 28.0±1.1 |
| Systolic blood pressure, mmHg | 118±4 | 118±4 | 123±3 |
| Diastolic blood pressure, mmHg | 70±2 | 73±2 | 72±1 |
| Medication use for | |||
| Hypertension, n | 4 | 3 | 5 |
| Lipid lowering, n | 4 | 5 | 4 |
| Physical activity | |||
| Steps/day | 5812±368 | 5436±594 | 6070±342 |
| Counts/min/day | 452±36 | 431±36 | 445±21 |
Data are mean±SE. CONT=control, MICT=moderate-intensity continuous training; HIIT=high-intensity interval training.
Table 2.
Effect of all-extremity HIIT and MICT on aerobic fitness, body composition and metabolic risk factors.
| CONT (n=14) | MICT (n=14) | HIIT (n=15) | ||||
|---|---|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | Baseline | Follow-up | |
| VO2peak, mL·kg−1·min−1 | 24.1±1.5 | 24.5±1.4 | 25.9±1.7 | 26.0±1.6 | 23.1±0.7 | 25.7±0.8* |
| VO2peak, L·min−1 | 1.72±0.11 | 1.76±0.11 | 1.93±0.13 | 1.95±0.14 | 1.72±0.10 | 1.91±0.11* |
| Body weight, kg | 73.2±4.5 | 73.4±4.4 | 76.8±2.7 | 76.1±2.5 | 73.0±3.7 | 72.8±3.5 |
| BMI, kg/m2 | 26.7±1.4 | 26.7±1.3 | 28.7±1.0 | 28.5±0.9 | 28.0±1.1 | 27.9±1.0 |
| Body fat, % | 34.1±1.9 | 34.1±1.7 | 37.5±2.2 | 37.2±2.0 | 38.8±1.8 | 37.9±1.8 |
| Fat mass, kg | 25.6±2.7 | 25.4±2.6 | 29.0±2.1 | 28.4±1.9 | 28.5±1.9 | 27.8±2.0 |
| Fat free mass, kg | 48.3±2.9 | 48.4±2.9 | 47.8±2.1 | 47.7±1.9 | 44.6±2.6 | 45.0±2.4 |
| Total cholesterol, mg/dL | 181±9 | 186±9 | 209±13 | 205±9 | 202±11 | 190±10 |
| HDL cholesterol, mg/dL | 54±3 | 60±4 | 59±4 | 57±4 | 66±6 | 66±6 |
| LDL cholesterol, mg/dL | 107±9 | 105±8 | 128±12 | 125±8 | 115±7 | 104±7 |
| Triglycerides, mg/dL | 96±11 | 106±12 | 114±14 | 116±16 | 103±21 | 96±13 |
| Glucose, mg/dL | 93±2 | 94±3 | 95±3 | 95±3 | 91±2 | 92±2 |
Data are mean±SE.
P<0.0001 vs. baseline.
CONT=control; MICT=moderate-intensity continuous training; HIIT=high-intensity interval training; VO2peak=peak oxygen consumption; BMI=body mass index; HDL=high-density lipoprotein; LDL=low-density lipoprotein.
Table 3.
Effect of all-extremity HIIT and MICT on left ventricular morphology.
| CONT (n=13) | MICT (n=11) | HIIT (n=15) | ||||
|---|---|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | Baseline | Follow-up | |
| LV Mass, g | 145±14 | 141±13 | 156±18 | 161±18 | 134±11 | 143±13 |
| PWTd, mm | 9.5±0.8 | 9.5±0.8 | 10.1±0.6 | 10.2±0.9 | 9.8±0.5 | 10.4±0.5 |
| SWTd, mm | 8.6±0.7 | 8.7±0.6 | 8.7±0.3 | 8.7±0.3 | 8.6±0.3 | 8.5±0.2 |
| LVIDd, mm | 46.0±1.3 | 45.5±1.3 | 46.7±2.8 | 47.2±2.7 | 43.5±2.0 | 44.0±1.9 |
| LVIDs, mm | 24.7±1.3 | 24.8±1.2 | 25.2±2.2 | 27.0±1.6 | 23.1±1.2 | 23.6±1.0 |
Data are mean±SE. CONT=control; MICT=moderate-intensity continuous training; HIIT=high-intensity interval training; LV=left ventricular; PWTd=posterior wall thickness during diastole; SWTd= septal wall thickness during diastole; LVIDd=left ventricle internal dimension during diastole; LVIDs=left ventricular internal dimension during systole.
Table 4.
Effect of all-extremity HIIT and MICT on left ventricular function.
| CONT (n=13) | MICT (n=11) | HIIT (n=15) | ||||
|---|---|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | Baseline | Follow-up | |
| Systolic function | ||||||
| Ejection Fraction, % | 57.0±0.8 | 55.8±0.9 | 56.2±0.5 | 56.9±0.6 | 56.2±0.8 | 58.4±0.7* |
| Diastolic function | ||||||
| E, cm/s | 76.6±4.0 | 77.7±3.6 | 83.0±5.9 | 78.6±7.2 | 80.4±4.1 | 77.1±3.6 |
| A, cm/s | 74.3±3.9 | 73.3±4.1 | 87.8±6.8 | 84.8±6.9 | 77.4±4.1 | 80.4±3.8 |
| E/A | 1.05±0.06 | 1.09±0.07 | 0.99±0.10 | 0.95±0.08 | 1.06±0.06 | 0.97±0.04 |
| DT, ms | 232±14 | 216±12 | 219±9 | 217±9 | 211±6 | 211±6 |
| e′, cm/s | 10.1±0.4 | 9.9±0.6 | 9.6±0.8 | 9.1±0.6 | 9.5±0.3 | 9.3±0.3 |
| a′, cm/s | 10.8±0.5 | 10.6±0.4 | 10.3±0.5 | 11.0±0.5 | 10.6±0.3 | 10.9±0.5 |
| E/e′ | 7.7±0.5 | 8.2±0.6 | 9.1±0.9 | 9.1±1.0 | 8.6±0.5 | 8.3±0.4 |
Data are mean±SE.
P=0.001 vs. baseline;
CONT=control; MICT=moderate-intensity continuous training; HIIT=high-intensity interval training; E=early diastolic peak filling velocity; A=late diastolic peak filling velocity; DT=deceleration time; e′=early diastolic mitral annular velocity; a′=late diastolic mitral annular velocity.
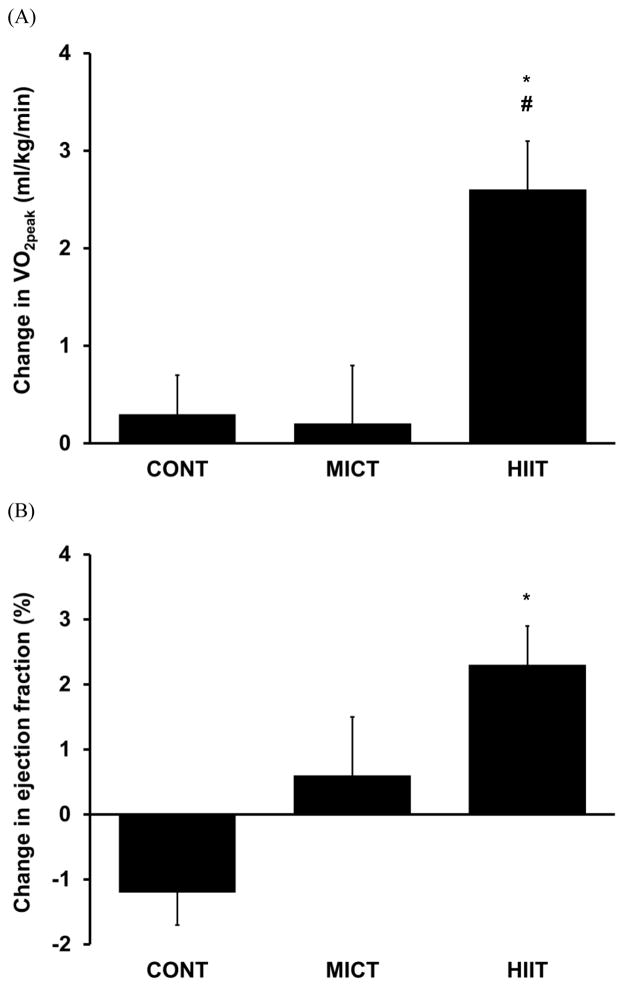
3.3 Positive responses to intervention occurred only with all-extremity HIIT
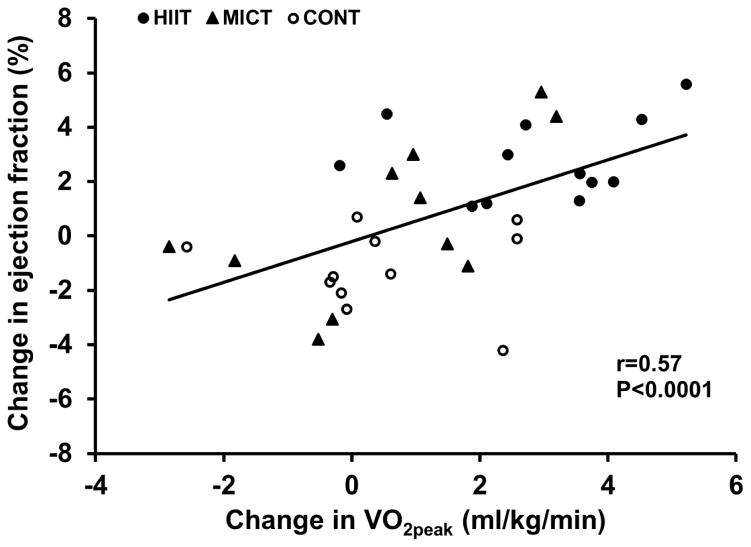
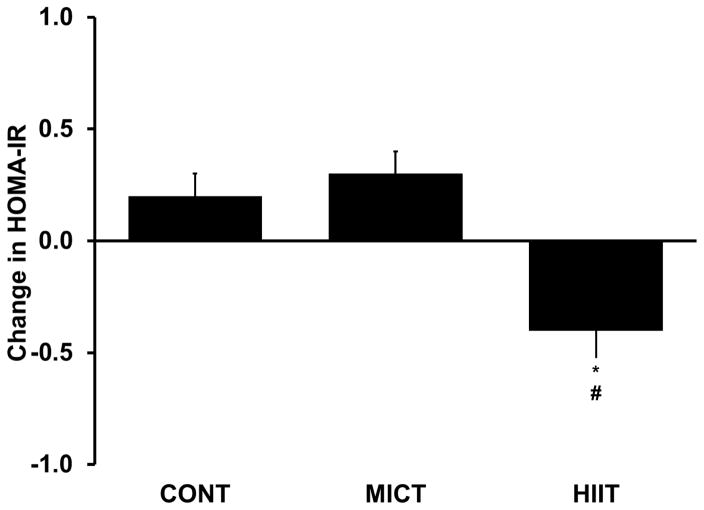
Evaluation of potential benefits of all-extremity HIIT and MICT in older adults included aerobic fitness, cardiac function, metabolic measures and body composition. Aerobic fitness, determined by VO2peak, improved only in HIIT (~11%, P<0.0001; Figure 3A and Table 2), while it did not change in MICT and CONT (P≥0.3). The results remained the same, even after covarying for baseline VO2peak. Cardiac contractile function, as assessed by ejection fraction, also improved only in HIIT (~4%, P=0.001; Figure 3B and Table 4), and remained unchanged in MICT and CONT (P≥0.1). Regression analysis between changes in ejection fraction and changes in VO2peak demonstrated a positive and significant correlation between these outcome measures, where a greater improvement in ejection fraction was associated with a greater improvement in VO2peak (r=0.57; P<0.0001; Figure 4). Additional cardiac measures, including left ventricular morphology and diastolic function, did not differ between baseline and follow-up in any of the three groups (P≥0.2; Table 3 and 4). Metabolic responses to the training regimen were also determined; blood samples were obtained on average 31.8±6.1 and 24.7±3.9 hours following the last exercise training session for HIIT and MICT, respectively (P=0.3). Insulin resistance, estimated by HOMA-IR, decreased with HIIT by 26% (P=0.016; Figure 5) while it did not change with MICT (P value was greater than the Bonferroni corrected α) and CONT (P=0.2). Fasting glucose and lipids did not significantly change in any of the groups (P≥0.1). Body weight, body mass index and body composition were also unaffected (P≥0.5).
Figure 3.
Change in peak oxygen consumption (VO2peak; panel A) and left ventricular ejection fraction (panel B) in non-exercise control (CONT), moderate-intensity continuous training (MICT), and high-intensity interval training (HIIT) groups. *P≤0.01 vs. CONT. #P=0.005 vs. MICT.
Figure 4.
Relation between the change in peak oxygen consumption (VO2peak) and the change in left ventricular ejection fraction. CONT=non-exercise control; MICT=moderate-intensity continuous training; HIIT=high-intensity interval training.
Figure 5.
Change in homeostatic model assessment of insulin resistance (HOMA-IR) in non-exercise control (CONT), moderate-intensity continuous training (MICT), and high-intensity interval training (HIIT) groups. *P=0.03 vs. CONT; #P=0.007 vs. MICT.
4. Discussion
We have established that this novel approach of performing HIIT on an all-extremity non-weight-bearing ergometer is feasible in healthy sedentary older adults and safe. This is the first randomized controlled trial to provide evidence that non-weight bearing all-extremity HIIT, but not MICT, improves aerobic fitness, cardiac systolic function, and insulin resistance without affecting body weight and composition in older adults who are free of cardiovascular and major clinical disease. Left ventricular morphology, diastolic function, glucose and lipids were not affected by the intervention.
4.1. Feasibility and safety of HIIT on all-extremity non-weight-bearing ergometer
HIIT and MICT on a treadmill have previously been shown to be highly effective in patient populations (Molmen-Hansen et al. 2012; Rognmo et al. 2004; Tjonna et al. 2008; Wisloff et al. 2007). We have demonstrated that these protocols can also be successfully adapted to an all-extremity non-weight-bearing ergometer and used in sedentary older adults. Our findings have important implications for exercise prescription particularly for individuals in which feasibility of treadmill exercise may be limited due to balance issues or musculoskeletal disorders. In our study, 8 weeks of all-extremity HIIT and MICT were well-tolerated resulting in completion of 88% of the exercise training sessions and no adverse events. From the 35 subjects assigned to either HIIT or MICT, 83% completed the exercise training intervention. A recent review on exercise training programs for older adults has reported adherence rates to be highly variable; the proportion of completed sessions over the total scheduled sessions varied from 58%–77% and the number of participants who completed the exercise intervention (i.e., did not drop out) varied from 65 to 86% (Picorelli et al. 2014). Thus, the exercise adherence rate of our subjects surpassed most, if not all, of the previously reported studies. We assert that the exercise regimen we have developed provides a new strategy for exercise prescription in older adults with minimal risk and optimal adherence rate.
4.2 Effect of 8 weeks all-extremity HIIT versus MICT on aerobic fitness
In our study, aerobic fitness improved by 2.6 mL/kg/min in response to HIIT but remained unchanged in response to MICT in sedentary older adults. The absolute increase in VO2peak with HIIT has important clinical significance, because every 3.5 mL/kg/min improvement in aerobic fitness is associated with 19% lower risk of CVD mortality (Lee et al. 2011). Our data are consistent with previous studies performed on the treadmill which demonstrated greater improvements in aerobic fitness in response to HIIT compared with MICT in healthy moderately trained young adults (Helgerud et al. 2007), obese adults (Schjerve et al. 2008) and patients with metabolic syndrome (Tjonna et al. 2008), hypertension (Molmen-Hansen et al. 2012) and cardiovascular disease (Rognmo et al. 2004; Wisloff et al. 2007). It is important to note that our findings are not confounded by differences in baseline aerobic fitness or changes in body weight or adiposity. The lack of improvement in aerobic fitness in response to MICT in our study is in agreement with previous data in healthy older adults following a moderate-intensity walking intervention (Pierce et al. 2011).
Central adaptations may be partly responsible for the greater improvements in aerobic fitness in response to HIIT in our study. HIIT resulted in small improvements in cardiac systolic function and greater improvements in systolic function were associated with greater improvements in VO2peak in our subjects. We recognize that correlations do not imply causation and additional studies would be needed to confirm this association. In addition, the mechanisms by which improvements in ejection fraction may lead to improvements in aerobic fitness in our study are not clear. Based on the Fick equation, maximal oxygen consumption is governed by maximal cardiac output and maximal arterio-venous oxygen difference. It is possible that an improved ejection fraction could lead to improved cardiac function, and in turn improved aerobic fitness, but, this remains to be established because our cardiac measures were performed during rest and may not be reflective of adaptations in cardiac function during exercise.
Previous studies suggest peripheral adaptations may also contribute to improvements in aerobic fitness in response to HIIT. HIIT, but not MICT, has been reported to decrease total peripheral resistance [9]. Moreover, greater improvements in endothelial function have been reported in response to HIIT than MICT and these were associated with greater improvements in aerobic capacity (r=0.69, P<0.05) (Schjerve et al. 2008; Tjonna et al. 2008; Wisloff et al. 2007). In addition to these cardiovascular adaptations, HIIT, but not MICT, has beneficial effects on mitochondrial biogenesis, by inducing greater increases in PGC-1α in skeletal muscle and these increases are associated with greater improvements in VO2peak (r=0.72, P<0.01) (Wisloff et al. 2007). Similar mechanisms may be responsible for the enhanced VO2peak adaptations to all-extremity HIIT in our study, although the exact mechanisms remain to be defined.
Ideally, aerobic capacity tests should be performed on the same mode of exercise as the one used for training and this factor may have contributed to the findings in our study. However, evaluating aerobic fitness during a treadmill test is a standard in the field and serves as a robust risk index for CVD morbidity and mortality. Moreover, use of a treadmill test allowed us to evaluate how our new training regimen alters aerobic capacity in comparison to related studies. Future studies need to explore the feasibility of conducting maximal exercise testing on an all-extremity non-weight-bearing ergometer in sedentary older adults and to establish age-specific reference values.
In older adults, attaining VO2max during a maximal exercise test is not entirely determined by aerobic capacity, but can also be influenced by fear of overexertion, perceived exhaustion, poor motivation and muscle weakness or fatigue (Huggett et al. 2005). Although we used a customized treadmill protocol which has previously been used successfully in sedentary older adults and we verbally encouraged our participants to exert maximal effort, our criteria for VO2max were not attained in all subjects. However, our criteria are more stringent compared to other interventions comparing HIIT versus MICT (Molmen-Hansen et al. 2012; Schjerve et al. 2008; Tjonna et al. 2008; Wisloff et al. 2007). Currently, there is a debate whether the criteria for VO2max need to be redefined for older adults (Huggett et al. 2005). The use of an all-extremity non-weight-bearing ergometer as an exercise modality for testing maximal aerobic capacity in older adults holds promising potential especially for individuals with functional limitations.
4.3. Effect of 8 weeks all-extremity HIIT versus MICT on cardiac function
We have demonstrated that all-extremity HIIT, but not MICT, results in a small but significant increase in left ventricular ejection fraction in healthy sedentary older adults, supporting that there is multi-pronged benefit of HIIT to the older population. Our observations of MICT are consistent with previous studies, where moderate-intensity aerobic exercise appears not to affect systolic function in healthy older adults (Fujimoto et al. 2013; Spina et al. 1993). Further, a recent study has reported an 8% increase in ejection fraction in older adults following 12 weeks of HIIT on the treadmill, but this finding remains to be confirmed in a randomized controlled trial (Molmen et al. 2012). Studies in patients with heart failure or hypertension have demonstrated HIIT can also be more effective in inducing left ventricular remodeling and improving systolic and/or diastolic function (Molmen-Hansen et al. 2012; Wisloff et al. 2007). In agreement with previous randomized studies, left ventricular morphology and diastolic function remained unchanged in our exercise intervention (Fujimoto et al. 2013; Haykowsky et al. 2005). Whether the modest benefits of HIIT in our study is because cardiac systolic function is usually well preserved in aging (Fleg and Strait 2012) and we excluded subjects with any cardiovascular disease, or due to the duration of the exercise intervention itself, is not clear. Thus, while our observed changes in ejection fraction following HIIT are lower than those in patient populations, they are consistent with the growing evidence that HIIT regimens evoke greater cardiovascular benefit than MICT.
4.4. Effect of 8 weeks all-extremity HIIT and MICT on metabolic risk factors and adiposity
Insulin resistance, assessed by HOMA-IR, is a direct and important predictor of diabetes (Welsh et al. 2014). In the present study, only HIIT improved insulin resistance and these findings were not confounded by changes in body weight or adiposity. Fasting glucose, triglycerides, and total, HDL and LDL cholesterol did not change in response to HIIT or MICT.
We are not aware of published studies comparing the effect of HIIT and MICT on these metabolic risk factors in older adults free from major clinical disease. Data on the effect of HIIT and MICT on glucose control and lipids are conflicting in patients with cardiometabolic disease and obese adults. In patients with chronic heart failure, both HIIT and MICT improved glucose, insulin and HOMA-IR, but only HOMA-IR was reduced significantly more with HIIT compared with MICT (Iellamo et al. 2014). However, in patients with metabolic syndrome, HOMA-IR improved only with HIIT (Tjonna et al. 2008). HDL cholesterol was also improved only with HIIT in these patients (Tjonna et al. 2008). Glucose, insulin and lipids were not influenced by either HIIT or MICT in patients with cardiovascular disease (Wisloff et al. 2007) and obese adults (Schjerve et al. 2008).
In our intervention, body weight, body mass index and total adiposity remained unchanged. This is consistent with data from a meta-analysis which demonstrated that exercise alone results in minimal weight loss (Franz et al. 2007). A combination of caloric restriction and all-extremity exercise training appears to be necessary to induce weight loss in sedentary older adults.
4.5 Study strengths
Our study has several strengths. Our intervention is the first to implement the well-established HIIT and MICT treadmill protocols on an all-extremity non-weight-bearing air-braked ergometer. Our study focused on sedentary older adults without major clinical disease, therefore our findings are not specific to a particular patient population which could limit generalizability. Our robust study design included a non-exercise control group which more definitively establishes the effectiveness of the exercise intervention. In addition, we were able to compare the effects of HIIT versus MICT without the confounding influence of unequal caloric expenditures because we used protocols designed to be isocaloric, which was confirmed by directly measuring oxygen consumption during all-extremity HIIT and MICT. Moreover, our exercise training intervention was supervised and well-controlled; heart rate was displayed and recorded to ensure the prescribed exercise intensity was attained during each session. Furthermore, we included a pre-conditioning period prior to the 8-week intervention to ensure the prescribed exercise intensity could be attained even during the first weeks of the intervention. We also monitored habitual physical activity at baseline and follow-up using an accelerometer to confirm our results can be attributed to the intervention rather than to overall increases in habitual physical activity independent of the supervised exercise sessions. Finally, our study used standardized procedures and blinding of investigators to ensure high quality data. Overall, we believe that this new non-weight-bearing all-extremity approach will help to expand the prescription of HIIT to populations unable to successfully complete these regimens on the treadmill.
4.6. Study limitations
Our study also has some limitations that should be considered when interpreting or applying our findings. We have established that 8 weeks of all-extremity non-weight-bearing HIIT is safe in sedentary older adults who are free of major clinical disease, however, safety during long-term training remains to be determined. A recent review and meta-analysis on HIIT in patients with cardiometabolic disease provided an extensive discussion of the safety of HIIT and concluded that the risk is low (Weston et al. 2014). In addition, the adaptations observed in our study are limited to the length of our intervention; a longer intervention might have resulted in greater adaptations.
Our intervention included both older men and postmenopausal women, but it was not adequately powered to examine sex-specific effects. In addition, young adults were excluded from the study; therefore, it is not possible to address whether exercise adaptations in our older participants are different compared with young adults. However, Kohrt et al have demonstrated that VO2max adapts to aerobic exercise training to the same relative level in healthy older adults compared with young adults, and adaptations are independent of sex and initial fitness level (Kohrt et al. 1991). Nevertheless, repeating our intervention in a larger cohort would allow secondary analyses to directly investigate the influence of factors such as sex and age. Although our sample size is relatively large compared to similar interventions in the literature, it is critical to reproduce the findings in larger cohorts.
Finally, we can only speculate based on the literature regarding other potential mechanisms that may explain our findings. Additional studies are needed to directly investigate the mechanisms underlying the adaptations to all-extremity exercise training in sedentary older adults.
5. Conclusions
The present study demonstrates that HIIT on an all-extremity non-weight-bearing ergometer is feasible in previously sedentary older adults and safe. All-extremity HIIT is more effective in improving aerobic fitness, cardiac systolic function, and insulin resistance compared with isocaloric MICT. HIIT on an all-extremity non-weight-bearing ergometer represents a promising alternative to weight-bearing HIIT in sedentary older adults.
Highlights.
All-extremity high-intensity interval training (HIIT) is feasible in older adults.
HIIT over 8 weeks is safe and resulted in no adverse events.
HIIT improves aerobic fitness, ejection fraction, and insulin resistance.
Acknowledgments
We would like to express our gratitude to the study participants for their time and efforts. We would also like to thank John Larocca, Karen Mackay, Andrea Vasconez, Sofia Sofianos, Kevin Priddy, Andre Revell, Austin Nolz, Blake Dalley, Lily Malone, Jessica Howard and Lindsay Wainman who assisted with conducting this intervention.
This work was supported by NIH AG 050203 to DDC. The funding source had no involvement in preparation or completion of the study or writing of the article.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Christou DD, Gentile CL, DeSouza CA, Seals DR, Gates PE. Fatness is a better predictor of cardiovascular disease risk factor profile than aerobic fitness in healthy men. Circulation. 2005;111:1904–1914. doi: 10.1161/01.CIR.0000161818.28974.1A. [DOI] [PubMed] [Google Scholar]
- Fleg JL, Strait J. Age-associated changes in cardiovascular structure and function: a fertile milieu for future disease. Heart failure reviews. 2012;17:545–554. doi: 10.1007/s10741-011-9270-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franz MJ, VanWormer JJ, Crain AL, Boucher JL, Histon T, Caplan W, Bowman JD, Pronk NP. Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. Journal of the American Dietetic Association. 2007;107:1755–1767. doi: 10.1016/j.jada.2007.07.017. [DOI] [PubMed] [Google Scholar]
- Fujimoto N, Hastings JL, Carrick-Ranson G, Shafer KM, Shibata S, Bhella PS, Abdullah SM, Barkley KW, Adams-Huet B, Boyd KN, Livingston SA, Palmer D, Levine BD. Cardiovascular effects of 1 year of alagebrium and endurance exercise training in healthy older individuals. Circulation Heart failure. 2013;6:1155–1164. doi: 10.1161/CIRCHEARTFAILURE.113.000440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gheno R, Cepparo JM, Rosca CE, Cotten A. Musculoskeletal disorders in the elderly. Journal of clinical imaging science. 2012;2:39. doi: 10.4103/2156-7514.99151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorman E, Hanson HM, Yang PH, Khan KM, Liu-Ambrose T, Ashe MC. Accelerometry analysis of physical activity and sedentary behavior in older adults: a systematic review and data analysis. European review of aging and physical activity: official journal of the European Group for Research into Elderly and Physical Activity. 2014;11:35–49. doi: 10.1007/s11556-013-0132-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottdiener JS, Bednarz J, Devereux R, Gardin J, Klein A, Manning WJ, Morehead A, Kitzman D, Oh J, Quinones M, Schiller NB, Stein JH, Weissman NJ American Society of E. American Society of Echocardiography recommendations for use of echocardiography in clinical trials. Journal of the American Society of Echocardiography: official publication of the American Society of Echocardiography. 2004;17:1086–1119. doi: 10.1016/j.echo.2004.07.013. [DOI] [PubMed] [Google Scholar]
- Haykowsky M, McGavock J, Vonder Muhll I, Koller M, Mandic S, Welsh R, Taylor D. Effect of exercise training on peak aerobic power, left ventricular morphology, and muscle strength in healthy older women. The journals of gerontology Series A, Biological sciences and medical sciences. 2005;60:307–311. doi: 10.1093/gerona/60.3.307. [DOI] [PubMed] [Google Scholar]
- Helgerud J, Hoydal K, Wang E, Karlsen T, Berg P, Bjerkaas M, Simonsen T, Helgesen C, Hjorth N, Bach R, Hoff J. Aerobic high-intensity intervals improve VO2max more than moderate training. Medicine and science in sports and exercise. 2007;39:665–671. doi: 10.1249/mss.0b013e3180304570. [DOI] [PubMed] [Google Scholar]
- Huggett DL, Connelly DM, Overend TJ. Maximal aerobic capacity testing of older adults: a critical review. The journals of gerontology Series A, Biological sciences and medical sciences. 2005;60:57–66. doi: 10.1093/gerona/60.1.57. [DOI] [PubMed] [Google Scholar]
- Hwang MH, Yoo JK, Luttrell M, Kim HK, Meade TH, English M, Segal MS, Christou DD. Mineralocorticoid receptors modulate vascular endothelial function in human obesity. Clin Sci (Lond) 2013;125:513–520. doi: 10.1042/CS20130200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iellamo F, Caminiti G, Sposato B, Vitale C, Massaro M, Rosano G, Volterrani M. Effect of High-Intensity interval training versus moderate continuous training on 24-h blood pressure profile and insulin resistance in patients with chronic heart failure. Internal and emergency medicine. 2014;9:547–552. doi: 10.1007/s11739-013-0980-4. [DOI] [PubMed] [Google Scholar]
- Kohrt WM, Malley MT, Coggan AR, Spina RJ, Ogawa T, Ehsani AA, Bourey RE, Martin WH, 3rd, Holloszy JO. Effects of gender, age, and fitness level on response of VO2max to training in 60–71 yr olds. J Appl Physiol (1985) 1991;71:2004–2011. doi: 10.1152/jappl.1991.71.5.2004. [DOI] [PubMed] [Google Scholar]
- Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. Journal of the American Society of Echocardiography: official publication of the American Society of Echocardiography. 2005;18:1440–1463. doi: 10.1016/j.echo.2005.10.005. [DOI] [PubMed] [Google Scholar]
- Lee DC, Sui X, Artero EG, Lee IM, Church TS, McAuley PA, Stanford FC, Kohl HW, 3rd, Blair SN. Long-term effects of changes in cardiorespiratory fitness and body mass index on all-cause and cardiovascular disease mortality in men: the Aerobics Center Longitudinal Study. Circulation. 2011;124:2483–2490. doi: 10.1161/CIRCULATIONAHA.111.038422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–419. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- Molmen-Hansen HE, Stolen T, Tjonna AE, Aamot IL, Ekeberg IS, Tyldum GA, Wisloff U, Ingul CB, Stoylen A. Aerobic interval training reduces blood pressure and improves myocardial function in hypertensive patients. European journal of preventive cardiology. 2012;19:151–160. doi: 10.1177/1741826711400512. [DOI] [PubMed] [Google Scholar]
- Molmen HE, Wisloff U, Aamot IL, Stoylen A, Ingul CB. Aerobic interval training compensates age related decline in cardiac function. Scandinavian cardiovascular journal: SCJ. 2012;46:163–171. doi: 10.3109/14017431.2012.660192. [DOI] [PubMed] [Google Scholar]
- Picorelli AM, Pereira LS, Pereira DS, Felicio D, Sherrington C. Adherence to exercise programs for older people is influenced by program characteristics and personal factors: a systematic review. Journal of physiotherapy. 2014;60:151–156. doi: 10.1016/j.jphys.2014.06.012. [DOI] [PubMed] [Google Scholar]
- Pierce GL, Eskurza I, Walker AE, Fay TN, Seals DR. Sex-specific effects of habitual aerobic exercise on brachial artery flow-mediated dilation in middle-aged and older adults. Clin Sci (Lond) 2011;120:13–23. doi: 10.1042/CS20100174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rognmo O, Hetland E, Helgerud J, Hoff J, Slordahl SA. High intensity aerobic interval exercise is superior to moderate intensity exercise for increasing aerobic capacity in patients with coronary artery disease. Eur J Cardiov Prev R. 2004;11:216–222. doi: 10.1097/01.hjr.0000131677.96762.0c. [DOI] [PubMed] [Google Scholar]
- Schjerve IE, Tyldum GA, Tjonna AE, Stolen T, Loennechen JP, Hansen HEM, Haram PM, Heinrich G, Bye A, Najjar SM, Smith GL, Slordahl SA, Kemi OJ, Wisloff U. Both aerobic endurance and strength training programmes improve cardiovascular health in obese adults. Clin Sci. 2008;115:283–293. doi: 10.1042/CS20070332. [DOI] [PubMed] [Google Scholar]
- Spina RJ, Ogawa T, Miller TR, Kohrt WM, Ehsani AA. Effect of exercise training on left ventricular performance in older women free of cardiopulmonary disease. Am J Cardiol. 1993;71:99–104. doi: 10.1016/0002-9149(93)90718-r. [DOI] [PubMed] [Google Scholar]
- Tjonna AE, Lee SJ, Rognmo O, Stolen TO, Bye A, Haram PM, Loennechen JP, Al-Share QY, Skogvoll E, Slordahl SA, Kemi OJ, Najjar SM, Wisloff U. Aerobic interval training versus continuous moderate exercise as a treatment for the metabolic syndrome: a pilot study. Circulation. 2008;118:346–354. doi: 10.1161/CIRCULATIONAHA.108.772822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welsh P, Preiss D, Lloyd SM, de Craen AJ, Jukema JW, Westendorp RG, Buckley BM, Kearney PM, Briggs A, Stott DJ, Ford I, Sattar N. Contrasting associations of insulin resistance with diabetes, cardiovascular disease and all-cause mortality in the elderly: PROSPER long-term follow-up. Diabetologia. 2014;57:2513–2520. doi: 10.1007/s00125-014-3383-9. [DOI] [PubMed] [Google Scholar]
- Weston KS, Wisloff U, Coombes JS. High-intensity interval training in patients with lifestyle-induced cardiometabolic disease: a systematic review and meta-analysis. British journal of sports medicine. 2014;48:1227–1234. doi: 10.1136/bjsports-2013-092576. [DOI] [PubMed] [Google Scholar]
- Wisloff U, Stoylen A, Loennechen JP, Bruvold M, Rognmo O, Haram PM, Tjonna AE, Helgerud J, Slordahl SA, Lee SJ, Videm V, Bye A, Smith GL, Najjar SM, Ellingsen O, Skjaerpe T. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients - A randomized study. Circulation. 2007;115:3086–3094. doi: 10.1161/CIRCULATIONAHA.106.675041. [DOI] [PubMed] [Google Scholar]