Abstract
Cystatin C has been regarded as a novel sensitive marker for the assessment of renal function, and the role of cystatin C as a predictor of cardiovascular events in patients with impaired renal function has been confirmed in clinical studies. In this study we assessed the association between cystatin C and Coronary artery disease [CAD] in a consecutive series of patients with normal kidney function in order to avoid the well-known effect of overt renal insufficiency on coronary atherosclerosis, and evaluate whether cystatin C has an ability to identify individuals at a higher risk for CAD among patients belonging to a low-risk category according to estimated glomerular filtration rate .The current study and review of literature demonstrated that serum levels of cystatin C, were independently associated with the development of CAD.
Key words: Cystatin C, HsCRP, Coronary artery disease, ACS, Biomarkers, cysteine protease
INTRODUCTION
Coronary artery disease (CAD) accounts for 20% of all medical emergency admissions and has the highest risk for adverse effects and deaths [1]. Clinical evaluation of suspected acute coronary artery disease depends increasingly on biomarkers to supplement electrocardiographic findings and patient history. Currently four markers apart from classic risk factors like lipids and glucose are recommended for regular clinical use: cardiac troponin I or T, B type natriuretic peptides (BNP & NT ProBNP) C reactive protein and D Dimer [2]. Apart from traditional risk factors, several novel risk factors have been found to be associated with acute coronary syndromes [3] [4]. Cystatin C is a cysteine protease inhibitor, produced by all nucleated cells. This protein is less influenced by age, gender, and muscle mass than serum creatinine and thus may be better indicator of cardiovascular risk [5] and heart failure [6] especially in the elderly.
METHODS
This prospective study was conducted in our hospital from June 2010 to February 2012. 575 patients with ‘chest pain ‘presented to emergency, who were evaluated by ECG. 173 demonstrated ECG abnormalities like ST elevation, ST depression and T inversion. They were enrolled as study population after taking consent. Cardiac enzymes CKMass and troponin I were evaluated in these patients.150 had raised enzymes and depicted onset of acute coronary syndrome. These patients were classified as cases and evaluated by coronary angiography. 150 age matched male healthy volunteers from hospital staff were taken as control group (Table 1).
Table 1.
Clinical characteristics of the study population
| Case (n =150) | Control (n = 150) | P value | |
|---|---|---|---|
| Smoking, n | 72 (47.69%) | 27 (18 %) | |
| Angiography | |||
| 1-vessel | 75 (50%) | – | – |
| 2-vessel | 54 (36%) | – | – |
| 3-vessel | 21(14%) | – | – |
| BMI (kg/m2) | 30.36 ± 5.97 | 28.67 ± 3.65 | 0.343 |
| Mean SBP (mm Hg) | 136 ± 24 | 127 ± 11 | 0.003 |
| Mean DBP (mm Hg) | 78 ± 14 | 80 ± 8 | 0.5 |
| Mean LVEF (%) | 59 ± 10 | 66 ± 8 | 0.412 |
The inclusion criteria were:
Male acute myocardial infarction [AMI] patients diagnosed by typical rise and gradual fall of biochemical markers (troponin I, creatine phosphokinase MB Mass) of myocardial necrosis with at least one of the following:Ischemic symptoms, development of pathological Q wave on ECG, ECG changes, indicative of ischemia (ST elevation or depression),coronary artery intervention.
Male Unstable angina: chest discomfort at rest with either ST depression of at least 0.1Mv or T wave inversion in two or more contiguous leads, CKMB normal and angiographically confirmed coronary artery disease.
The exclusion criteria were:
Advanced kidney failure indicated by high serum urea and creatinine
Overt heart failure, diagnosed by echocardiography
History of major surgery /trauma within the previous month
Suspected systemic inflammatory disease
Chronic stable angina (effort induced) diagnosed as chest pain of at least six month’s duration, accompanied by severe CAD on angiography (70% stenosis in any major artery)
A fasting blood sample was taken within 4-6 hours of chest pain and prior to angiography and serum extracted and stored at -70 degree C until further testing. The height was measured in metres and weight in kg. BMI was calculated by the formula Quetelet index = weight / (height) 2.
Plasma glucose, urea, creatinine, uric acid, total protein, albumin, and lipid parameters were measured using enzymatic methods (Siemens Dimension Expand plus,Siemens Healthcare Diagnostics Inc,Newark, DE 19714,U.S.A). An internal quality control from Biorad laboratories was run for every parameter in a batch Low-density lipoprotein cholesterol concentration was calculated using the Friedewald formula. [7] CKMB Mass and Troponin I levels were estimated by enzyme linked immunofluorescent assay. (Minividas,Biomerieux SA,France).. All patients had white blood cell counts within reference range. We used the turbidimetric method to measure high-sensitivity C Reactive protein [hsCRP] (CX 5 analyzer, Beckman Coulter Inc., Fullerton, California, U.S.A) and Cystatin C (Quantia, Tulip diagnostics, Goa, India) .For hsCRP, the detection limit was 0.05 mg/l, with intra- and inter-assay CVs of 2.0 % and 3.7%.For Cystatin C, the detection limit was 0.33 mg/L, with intra and inter assay CV of 1.42%-and 3.72% respectively.
All the values are expressed as mean ± SD. Continuous variables were compared with the Student’s t-test. Pearson’s correlation was used to look for association between different variables in the study group. A p-value < 0.05 was considered significant. Multivariate regression analysis was performed to ascertain the role of the different risk factors for CAD in our study. In order to analyze the performance of Cystatin C as indicator for acute coronary syndrome, the receiver operating characteristics (ROC) curve was plotted. Statistical analyses were performed with SPSS for windows version 12 (SPSS Inc,Chicago,illinois).
RESULTS
We enrolled 150 consecutive male patients, who had undergone coronary angiography for the investigation of CAD and 150 age matched healthy male volunteers. A significantly higher number of cases of acute coronary syndrome were smokers and had higher systolic blood pressure.
Serum creatinine, serum hsCRP and serum Cystatin C levels were significantly higher in patients with ACS than in healthy controls as shown in Table 2.
Table 2.
Biochemical parameters in cases (n=150) and controls (n=150)
| Case | |||
|---|---|---|---|
| control (n=150) | (n=150) | p value | |
| age (years) | 56.20±10.79 | 54.85±10.78 | NS |
| RBS(mg/dl) | 103.02±27.25 | 154.79±60.62 | < 0.0001 |
| urea(mg/dl) | 23.57±5.16 | 54.22±43.02 | < 0.0001 |
| creat(mg/dl) | 0.87±0.32 | 1.88±1.09 | < 0.0001 |
| Cystatin c(mg/L) | 0.90±0.17 | 1.47±0.94 | < 0.0001 |
| HsCRP (mg/L) | 2.06±0.83 | 3.05±0.66 | < 0.0001 |
| Cholesterol (mg/dl) | 168.41±26.07 | 188.69±26.90 | < 0.0001 |
| Triglyceride(mg/dl) | 135.40±38.82 | 170.33±39.73 | < 0.0001 |
| HDL (mg/dl) | 46.62±12.34 | 42.13±8.73 | P<0.05 |
| LDL (mg/dl) | 111.12±42.45 | 110.36±27.52 | NS |
| Cholesterol/HDL C | 3.88±1.27 | 4.71±1.38 | < 0.0001 |
| Total protein (g/dl) | 8.04±1.64 | 7.03±0.82 | < 0.0001 |
| albumin (g/dl) | 4.62±1.45 | 3.36±0.94 | < 0.0001 |
| A/G | 1.88±0.85 | 1.15±1.36 | NS |
| CKMass(ng/ml) | 2.10±1.46 | 46.10±86.24 | < 0.0001 |
| Troponin I (ng/ml) | 0.04±0.02 | 13.06±15.62 | < 0.0001 |
On applying the Chi square test, at 3 degrees of freedom, at 5 % level, the value of x squared was 7.82. At the calculated value 98.06, p was far less than 0.001, hence highly significant.
A positive correlation was found between Cystatin C and creatinine (r=0.36, p<0.0001), between hsCRP and triglyceride (r=0.18,p<0.05), between hsCRP and CKMass (r=0.21,p<0.05), between hsCRP and troponin I (r=0.22, p<0.05). No such significant correlation was seen between the other parameters [Table 3].
Table 4.
Multiple logistic regression
| T value | P value [<0.05 is significant] | |
|---|---|---|
| Age | 1.46 | 0.15 |
| RBS | 1.08 | 0.28 |
| Urea | 0.97 | 0.33 |
| Creatinine | 2.02 | 0.04 |
| Cystatin c | 2.84 | 0.00 |
| Hscrp | 0.45 | 0.65 |
| Cho | 1.94 | 0.05 |
| T.G | 1.44 | 0.15 |
| HDL | 1.71 | 0.09 |
| LDl | 1.86 | 0.04 |
| Chl/HDL | 1.83 | 0.07 |
| Protein | 0.27 | 0.79 |
| Albumin | 1.54 | 0.12 |
| A/G | 0.77 | 0.44 |
| CK Mass | 0.99 | 0.32 |
| Troponinl | 2.43 | 0.02 |
Multivariate regression analysis proved the superiority and significance of creatinine, Cystatin C, Total cholesterol and LDL cholesterol over other biochemical parameters tested.
Cystatin C showed a significant positive correlation with serum creatinine [Figure 1] and with hsCRP [Figure 2] .HsCRP showed a positive correlation with serum triglycerides, CKMB Mass, troponin I levels. Using Cystatin C cutoff of 1mg/L, we obtained a sensitivity of 77.8 % in detecting ACS patients .However the specificity was a low 6.2% [Figure 3]. Area under the curve was 0.831.At a higher cut-off we obtained a lower specificity.
Figure 1.

Scatter diagram to show correlation of Cystatin C and creatinine levels in acute coronary syndrome.
Figure 2.
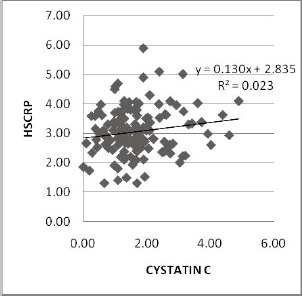
Scatter diagram to show the correlation of cystatin C with HsCRP levels in Acute coronary syndrome.
Figure 3.

ROC Curve showing Sensitivity and Specificity of Cystatin C in ACS.
DISCUSSION
Cystatin C has emerged as a novel sensitive marker for detecting renal dysfunction. In Prospective Epidemiological Study of Myocardial Infarction (PRIME), cystatin C predicted the occurrence of the first coronary events in men aged 50 to 59 years old, and displayed a strong relation with CAD independent of eGFR [8]. Several other publications have demonstrated that cystatin C was closely associated with incident congestive heart failure [9], carotid atherosclerosis [10], and peripheral vascular disease [11] superior to serum creatinine or creatinine-based eGFR.
We obtained Cystatin C levels of 0.9± 0.17 mg/L and 1.47 ± 0.94 mg/L in controls and cases respectively and a positive correlation of serum creatinine with serum Cystatin C. Reference ranges quoted by Kyhse – Anderson et al [12] was 0.61-1.21 mg/L, by Norund et al [13] 0.7-1.21 mg/L, and much higher cystatin-C concentration by Pergande et al [14]. This difference is probably due to different calibrated material.
The first study to demonstrate that the measurement of cystatin C substantially improves the early risk stratification of the large population of patients with suspected ACS was by Jernberg et al [15]. They divided patients according to final diagnosis into: a) those with non–ST-elevation ACS, b) those with other cardiac causes, c) and those with other non-cardiac or unknown causes, and showed that when adjusted for other well-known predictors of outcome, the cystatin C level remained an independent predictor of mortality. Ttaglieri et al [16] reported that few patients (0.8%) had severely impaired renal function [eGFR-MDRD <30ml/min/1.73m], 157 patients (30%) reached the study end-point. Patients in third and fourth quartile showed a higher cumulative probability of cardiac events compared to patients in the lowest quartile.
Cystatin C is expressed in all of the nucleated cells, regulates the activity of cysteine protease, and plays a role in the dynamic balance of production and degradation of ECM. Cystatin C and its fragments may also affect the phagocytic and chemotactic ability of neutrophil, participates in the inflammatory process and regulates inflammatory responses. Inflammation plays an important role in the development of atherosclerosis. Moreover, ECM degradation and positive arterial remodeling relate closely to plaque destabilization, suggesting that cystatin C may facilitate plaque vulnerability as a result of ACS. In their study, Ge et al [17] found greatly elevated plasma concentration of cystatin C and hs-CRP in patients with ACS. Cystatin C was positively correlated with hs-CRP and WBC. In our study too, Cystatin C and hsCRP were positively correlated, indicating that cystatin C plays an important role in the development of ACS, and one of the mechanisms is thought to be that cystatin C facilitates the progress of atherosclerosis by regulating inflammation.
The development of atherosclerotic plaque is primarily a lesion that progresses due to a series of reactions that are induced by repair of an injured intima. The pathophysiology of stable angina pectoris is based on the stability of atherosclerotic plaque, while unstable angina pectoris is caused by unstable atherosclerotic plaque or as it is known, vulnerable plaque. Moreover, the pathophysiology of myocardial infarction is basically the breakdown of vulnerable plaque based on platelet aggregation, different levels, and different characteristics of thrombosis. The intercellular networking that occurs among smooth muscle cells, macrophages, T lymphocytes, and endothelial cells leads to a fibroproliferative response, in which the extracellular matrix [ECM] plays an important role. The ECM, composed of a mixture of vastly different macromolecules including collagen, elastin, glycoproteins, and proteoglycans, confers tensile strength and viscoelasticity to the arterial wall. Each component of the ECM possesses unique structural properties that determine its own role during the development of atherosclerotic plaques. Not only does the ECM provide the structural integrity of the plaques, but it also participates in several key events such as cell migration and proliferation, lipoprotein retention, and thrombosis Cysteine proteinase, the major enzyme in ECM degradation, and its inhibitor as cystatin C is expressed in the plaque. An excess of cysteine proteinase over cystatin C may contribute significantly to ECM destruction rendering the plaque more prone to rupture. In our study, we found a positive correlation of Cystatin C with hsCRP [Figure 2]
Atherosclerosis is increasingly being recognised as a complex phenomenon involving the interaction of several mechanisms: dyslipidaemia, inflammation, thrombosis and other dysfunctional metabolic syndromes [18]. Parikh et al [19] showed that high concentrations of cystatin C were independently associated with cardiovascular risk factors such as age, female sex, BMI, low HDL cholesterol, and smoking, even in individuals without CKD or microalbuminuria .A cross-sectional analysis of data on individuals with CKD in the study disclosed a similar risk profile but, interestingly, those with high cystatin C concentrations and no CKD had a higher prevalence of obesity and hypertension compared to individuals with CKD and low cystatin C. Muntner et al [20] showed that the prevalence of risk factors such as cigarette smoking, hypertension, and low HDL cholesterol was higher in individuals with higher cystatin C concentrations. Moreover, the prevalence of CVD, myocardial infarction (MI), angina pectoris, and stroke increased with increasing concentrations of cystatin C. After adjustment for age, sex, race, and principal cardiovascular risk factors, cystatin C was still independently associated with CVD. Ix et al [21][22] evaluated whether serum cystatin C concentrations were associated with all-cause mortality, cardiovascular events, and incident HF in outpatient clinic patients included in the prospective “Heart and Soul” study .Windhausen et al [23] found that in patients with NSTE-ACS and increased cardiac troponin T concentrations, high plasma cystatin C concentrations are associated with a higher risk of death and spontaneous MI There is evidence that both elastolytic cysteine proteases and their inhibitors, an important one being Cystatin C, are involved in the pathogenesis of atherosclerosis[23] . Studies have suggested that rather than the circulating levels, the imbalance between proteases and inhibitors determines their net effects on the cardiovascular system[24]. Inflammatory cytokines associated with atherosclerosis stimulate the production of lysosomal cathepsins, and increased plasma concentrations of cystatin C, a cathepsin inhibitor, may reflect an attempt to counterbalance a potentially damaging increased elastolytic activity. Human cathepsins are expressed in endothelial cells, smooth muscle cells, and macro-phages, and that they are involved in the progression, the composition, and the rupture of atherosclerotic plaques .This response is likely to involve the interaction of mechanisms determined genetically [25].
Increased cystatin C concentrations identify early GFR abnormalities, and it has been suggested that this marker is highly sensitive to “preclinical” kidney dysfunction [26] which may be associated with adverse clinical outcomes. Cystatin C may thus help, in the early phases of CKD, to identify individuals who are at increased risk both for further impairment of CKD and for the development of CVD, and who may benefit from more “aggressive” preventative measures, such as lowering blood pressure to stringent targets and enrollment into strict monitoring pro-grams.
Limitations of our study merit consideration. Since the number of patients assessed by coronary angiography was fairly limited, replication of the cystatin C level association with coronary arteries stenosed is needed in a larger sample to rule out the possibility of a false-positive finding. The relation between plasma cystatin C, hsCRP concentration and severity of CAD needs to be re-examined in a larger cohort as well. We cannot rule out the possibility that cystatin C is a marker of another pathologic process that is unrelated to kidney function [27]. Finally, we cannot rule out the possibility of confounding from factors that were not measured or of residual confounding from factors for which we have accounted imperfectly.
These restrictions notwithstanding, our findings have several implications. First, a more accurate assessment of kidney function through measurement of serum cystatin C could be used to assess risk for ACS. With earlier detection of kidney dysfunction, interventions to slow the progression of kidney disease could lead to a parallel reduction in the incidence of ACS. In addition, better assessment of kidney function by measurement of cystatin C may lead to beneficial outcomes in clinical medicine, such as safer prescription of medications and a more refined evaluation of surgical risk. Our findings necessitate population-based follow-up studies to establish the role of Cystatin C in preventive cardiology.
References
- 1.Capewell S, McMurray J. Chest pains-please admit: is there an alternative? A rapid Cardiological assessment service may prevent unnecessary admissions. Br Med.J. 2000; 320:951-952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hochholzer W, Morrow DA, Giugliano RP. Novel biomarkers in cardiovascular disease: update 2010. Am Heart J 2010;160:583-594. [DOI] [PubMed] [Google Scholar]
- 3.Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE, Jr, et al. ACC/AHA 2007 Guidelines for the management of patients with unstable angina/non-ST-Elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2007; 50(7):1-157. [DOI] [PubMed] [Google Scholar]
- 4.Lodh M, Goswami B, Parida A, Patra S, Saxena A. Assessment of serum leptin, pregnancy –associated plasma protein A and CRP levels as indicators of plaque vulnerability in patients with acute coronary syndrome. Cardiovascular Journal of Africa 2012; 23(6): 330-335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nagesh CM, Roy A. Role of biomarkers in risk stratification of acute coronary syndrome. Indian J Med Res. 2010; 132(5):627–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sarnak MJ, Katz R, Stehman-Breen CO, Fried LF, Jenny NS, Psaty BM, et al. Cystatin C Concentration as a Risk Factor for Heart Failure in Older Adults. Ann Intern Med. 2005; 142: 497-505. [DOI] [PubMed] [Google Scholar]
- 7.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma without use of the preparative ultracentrifuge. Clin Chem 1972; 18: 499–502. [PubMed] [Google Scholar]
- 8.Luc G, Bard JM, Lesueur C, Arveiler D, Evans A, Amouyel P, Ferrieres J, Juhan-Vague I, Fruchart JC, Ducimetiere P: Plasma cystatin-C and development of coronary heart disease: The PRIME Study. Atherosclerosis. 2006, 185:375–380. [DOI] [PubMed] [Google Scholar]
- 9.Sarnak MJ, Katz R, Stehman-Breen CO, Fried LF, Jenny NS, Psaty BM, Newman AB, Siscovick D, Shlipak MG: Cystatin C concentration as a risk factor for heart failure in older adults. Ann Intern Med. 2005, 142:497–505. [DOI] [PubMed] [Google Scholar]
- 10.Hoke M, Pernicka E, Niessner A, Goliasch G, Amighi J, Koppensteiner R, Minar E, Mlekusch W, Rumpold H, Wagner O, et al. : Renal function and long-term mortality in patients with asymptomatic carotid atherosclerosis. Thromb Haemost. 2012, 107:150–157. [DOI] [PubMed] [Google Scholar]
- 11.O’Hare AM, Newman AB, Katz R, Fried LF, Stehman-Breen CO, Seliger SL, Siscovick DS, Shlipak MG: Cystatin C and incident peripheral arterial disease events in the elderly: results from the Cardiovascular Health Study. Arch Intern Med. 2005, 165:2666–2670. [DOI] [PubMed] [Google Scholar]
- 12.Kyhse–Andersen J, Schmidt C, Nordin G, Anderson B, Nilsson Ehle, et al. Serum Cystatin C, determined by a rapid, automated,particle – enhanced turbidometric method is a better marker than serum creatinine for glomerular filtration rate. Clin. Chem. 1994; 40:1921-1926. [PubMed] [Google Scholar]
- 13.Norfund L, Fex G., Lande J, Von Schenck H, Nilsson JE, et al. Reference intervals for the glomerular filtration rate and cell – proliferation markers; Serum /cystatin C and serum b2 microglobulin I cystatin C ratio. Scand. J. Clin.Lab Invest 1997; 57: 463-470. [DOI] [PubMed] [Google Scholar]
- 14.Pergande M, Jung K. Sandwich enzyme immuno assay of cystatin C in serum with commercially available antibodies. Clin chem 1993; 39: 1885-1890. [PubMed] [Google Scholar]
- 15.Jernberg T, Lindahl B, James S, Larsson A, Lars-Olof Hansson, Wallentin L., Cystatin C: A Novel Predictor of Outcome in Suspected or Confirmed Non-ST-Elevation Acute Coronary Syndrome. Circulation. 2004, 110:2342-2348. [DOI] [PubMed] [Google Scholar]
- 16.Taglieri N, Fernandez-Berges DJ, Koenig W, Consuegra-Sanchez L, Fernandez JM, Robles NR, Sánchez PL, Beiras AC, Orbe PM, Kaski JC; SIESTA Investigators. Plasma cystatin C for prediction of 1-year cardiac events in Mediterranean patients with non-ST elevation acute coronary syndrome. Atherosclerosis. 2010; 209 :300-305. [DOI] [PubMed] [Google Scholar]
- 17.Ge C, Ren F, Lu S, Ji F, Chen X, Wu X. Clinical prognostic significance of plasma cystatin C levels among patients with acute coronary syndrome. Clin Cardiol. 2009;32:644-648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harb TS, Zareba W, Moss AJ, Ridker PM, Rifai N, Marder WJ, et al. Association between inflammatory markers, hemostatic and lipid factors in post infarction patients. Am J Cardiol 2003; 91: 1120–1123. [DOI] [PubMed] [Google Scholar]
- 19.Parikh NI, Hwang SJ, Yang Q, Larson MG, Guo CY, Robins SJ, et al. Clinical correlates and heritability of cystatin C (from the Framingham Offspring Study). Am J Cardiol 2008; 102:1194–1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Muntner P, Mann D, Winston J, Bansilal S, Farkouh ME. Serum cystatin C and increased coronary heart disease prevalence in US adults without chronic kidney disease. Am J Cardiol 2008; 102:54–57. [DOI] [PubMed] [Google Scholar]
- 21.Ix JH, Shlipak MG, Chertow GM, Whooley MA. Association of cystatin C with mortality, cardiovascular events, and incident heart failure among persons with coronary heart disease: data from the Heart and Soul Study. Circulation 2007; 115: 173–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ix JH, Shlipak MG, Liu HH, Schiller NB, Whooley MA. Association between renal insufficiency and inducible ischemia in patients with coronary artery artery disease: the heart and soul study. J Am Soc Nephrol 2003; 14: 3233–3238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Windhausen F, Hirsch A, Fischer J, van der Zee PM, Sanders GT, van Straalen JP, et al. Cystatin C for enhancement of risk stratification in non-ST elevation acute coronary syndrome patients with an increased troponin T. Clin Chem 2009;55:1118–1125. [DOI] [PubMed] [Google Scholar]
- 24.Liu J, Sukhova GK, Sun JS, Xu WH, Libby P, Shi GP. Lysosomal cysteine proteases in atherosclerosis. Arterioscler Thromb Vasc Biol 2004; 24:1359-1366.75. [DOI] [PubMed] [Google Scholar]
- 25.Taglieri N, Wolfgang Koenig W, Kaski JC. Cystatin C and Cardiovascular Risk. Clinical Chemistry 2009;55:(11)1932–1943 [DOI] [PubMed] [Google Scholar]
- 26.Shlipak MG, Katz R, Sarnak MJ, Fried LF, Newman AB, Stehman-Breen C, et al. Cystatin C and prognosis for cardiovascular and kidney outcomes in elderly persons without chronic kidney disease. Ann Intern Med 2006; 145: 237-246. [DOI] [PubMed] [Google Scholar]
- 27.Eriksson P, Deguchi H, Samnegard A, Lundman P, Boquist S, Tornvall P, et al. Human evidence that the cystatin C gene is implicated in focal progression of coronary artery disease. Arterioscler Thromb Vasc. Biol. 2004; 24:551-557. [DOI] [PubMed] [Google Scholar]


