Abstract
The gold standard of semen analysis is still an manual method, which is time-consuming, labour intensive and needs thorough quality control. Microfluidics can also offer advantages for this application. Therefore a first step in the development of a microfluidic chip has been made, which enables the man the semen analysis at home. In this article recent efforts to determine the concentration and motility using a microfluidic chip are summarized.
INTRODUCTION
A couple that is unable to get pregnant after one year of unprotected intercourse, usually ends up at the gynaecology department of a hospital. One of the aspects that will be investigated is the fertility of the man. Therefore the man has to collect his semen in a special container and deliver it within one hour of collection to the hospital. The parameters usually determined with a semen analysis are the concentration and the motility of the spermatozoa in the semen. The haemocytometer is the gold standard for concentration determination [1], but this labour intensive method is in larger laboratories replaced by an expensive computer assisted semen analysis system (CASA). Another way that gives an estimation of the spermatozoa concentration uses flow cytometry [2, 3], while antibody binding [4] and fluorescence labelling [5] are used to determine the concentration of progressive motile spermatozoa (>5μm·s-1). None of these approaches assess the concentration of spermatozoa without the use of an expensive system, labour intensive handling and sample preparation. Furthermore, due to intra-individual variations, the results of a single test are not reliable and at least three tests have to be done [6]. A better alternative for the current procedure is a portable system that enables the man to perform several objective and reliable measurements at home. Today a few at-home tests to determine the fertility of the man exist, but these rely on subjective interpretation by the man and only give qualitative information about the semen quality [7]. For a treatment decision by the gynaecologist quantitative information is necessary. Microfluidic devices have the potential to offer this information. The small reagent- and sample volumes needed, together with the possibility to integrate several steps in one single device, provides the opportunity to improve the semen analysis. Therefore we focus on the development of a microfluidic chip for the assessment of the semen quality. Such disposable microfluidic chip will be ultimately used in combination with a handheld measurement system and management software (see figure 1). In this manuscript our recent efforts for improvement of the fertility chip are summarized.
Figure 1.

An artistic impression of the fertility chip. It consists of a handheld system, microfluidic chip and software.
ON-CHIP SEMEN ANALYSIS
Almost twenty years ago, Kricka and co-workers showed that a microfluidic chip can be used to separate motile sperm from a semen sample [8]. To our knowledge, they were the first who used microfluidics for andrology applications. Subsequently more studies have been published which focus on the use of microfluidics for (part of the) semen analysis or sperm selection and purification [9].
In our first approach, microfluidic impedance cytometry has been used to determine the concentration of spermatozoa in semen [10]. With cleanroom fabrication techniques a glass-glass chip has been made (see figure 2), which comprises an 18 μm deep microfluidic channel. At the tapering of the microfluidic channel to a width of 38 μm two platinum electrodes are positioned at one side of the channel. These electrodes are used for the detection of single spermatozoa in the semen. The electrical impedance is measured at a specific frequency between those electrodes and when a cell passes the electrode pair, it changes the average dielectric properties of the measurement volume, resulting in an impedance change. In this way every spermatozoon that passes the electrode pair is counted (see figure 3). Since the value of the impedance change of each event is also dependent on the size of the cell passing the electrode pair, we were able to distinguish between HL-60 cells, spermatozoa and 6 μm polystyrene beads [10]. To determine the concentration of spermatozoa in semen, we used a comparable method as used in conventional flow cytometry. A known concentration of polystyrene beads was added to the semen sample and by flowing them through the chip by means of applying a hydrostatic pressure, we showed that we were able to determine the spermatozoa concentration of boar semen in the range from 2·106 to 60·106mL-1 [10].
Figure 2.
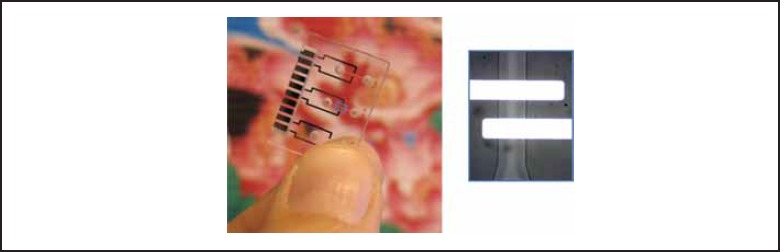
An example of the microfluidic chip and in the inset a microscopic image of the microchannel with a spermatozoon in it. The two white bars are the electrodes.
Figure 3.

The detection of spermatozoa (red circle) and larger cells (blue square) using electrical impedance measurements. In the electrical impedance signal the passage of these cells can be clearly seen.
Another parameter that is important to assess the semen quality is the motility of the spermatozoa. For the purification of the ‘best’ spermatozoa out of a semen sample for assisted reproductive technologies (e.g. in-vitro fertilisation, intracytoplasmic sperm injection) Cho and co-workers developed a microfluidic approach [11, 12]. In this approach two microchannels combine to one separation channel, where the two laminar flows from both channels join. Only motile spermatozoa have the ability to cross the flow barrier and will end up in the other channel, thereby creating a sample of spermatozoa with sufficient motility for further use. For the determination of the motility we use the same principle as mentioned before and we combine this with the electrical detection of spermatozoa at the two outlet channels (see figure 4). The detection of the spermatozoa in both outlet channels is done with the same configuration as used for determining the concentration on-chip. We propose a new model for the determination of the separation efficiency of motile spermatozoa from the semen sample [9] and compare these simulated results with experimental data, which shows a good agreement. In this way we were able to distinguish between samples with motile and immotile spermatozoa.
Figure 4.
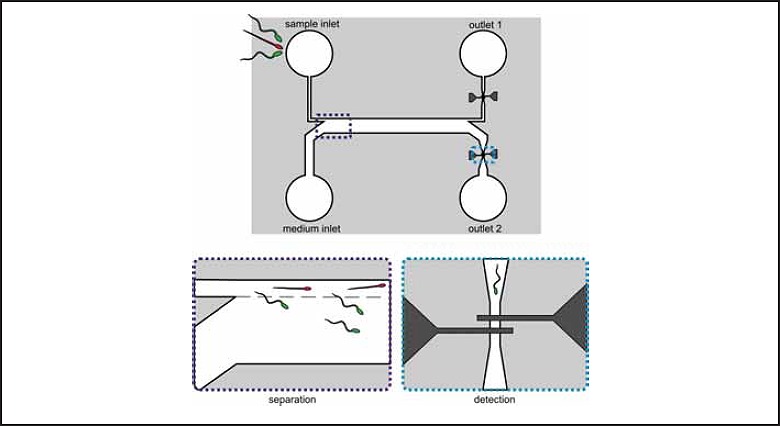
The LOC device that was used for the motility determination. It consists of two parts: separation and detection. In the 5 mm long, 18 μm deep separation channel the motile spermatozoa are able to cross the laminar flow barrier (---) and arrive in outlet 2, while the immotile cannot cross and end up in outlet 1. At both detection regions the cells are counted using electrical impedance measurement [9].
CONCLUSION AND FUTURE PERSPECTIVES
Parameters of the semen quality that are normally determined in the hospital laboratory can be measured with microfluidic devices in an objective way making point-of-care diagnostics possible. With microfluidic devices a shift toward at-home analysis can be made, thereby reducing the costs and making it more patient friendly. Additionally, more measurements can be performed over a period of time such that a better statement of the semen quality is obtained. This information can lead to a better treatment decision of the gynaecologist, thereby improving the care of the couple that is childless by default.
ACKNOWLEDGEMENTS
This research is supported by the Dutch Technology Foundation STW, which is an applied science division of NWO, and the Technology Program of the Ministry of Economic Affairs. The chip fabrication by Johan Bomer and Lennart de Vreede are gratefully acknowledged.
This article has been modified from the two following articles:
Segerink, L.I., et al., A. Lab-on-a-chip technology for clinical diagnostics: the fertility chip. Ned Tijdschr Klin Chem Labgeneesk, 2012 37:61-63.
Segerink, L.I. et al., Spermatozoa detection and counting on chip. Ned Tijdschr Klin Chem Labgeneesk, 2009 34: 254-255.
References
- 1.WHO WHO laboratory manual for the examination and processing of human semen. 5th ed. 2010, Geneva. [Google Scholar]
- 2.Eustache F., Jouannet P., Auger J., Evaluation of flow cytometric methods to measure human sperm concentration. Journal of Andrology, 2001. 22(4): p. 558-567. [PubMed] [Google Scholar]
- 3.Perticarari S., et al. , A new multiparameter flow cytometric method for human semen analysis. Human Reproduction, 2007. 22(2): p. 485-494. [DOI] [PubMed] [Google Scholar]
- 4.Björndahl L., et al. , Development of a novel home sperm test. Human Reproduction 2006. 21(1): p. 145-149. [DOI] [PubMed] [Google Scholar]
- 5.McCormack M.C., McCallum S., Behr B., A novel microfluidic device for male subfertility screening. Journal of Urology, 2006. 175: p. 2223-2227. [DOI] [PubMed] [Google Scholar]
- 6.Keel B.A., Within- and between-subject variation in semen parameters in infertile men and normal semen donors. Fertility and Sterility, 2006. 85(1): p. 128-134. [DOI] [PubMed] [Google Scholar]
- 7.Brezina P.R., Haberl E., Wallach E., At home testing: optimizing management for the infertility physician. Fertility and Sterility, 2011. 95(6): p. 1867-1878. [DOI] [PubMed] [Google Scholar]
- 8.Kricka L.J., et al. , Applications of a microfabricated device for evaluating sperm function. Clinical Chemistry, 1993. 39(9): p. 1944-1947. [PubMed] [Google Scholar]
- 9.Segerink L.I. Fertility chip, a point-of-care semen analyser. PhD thesis,. 2011, University of Twente [Google Scholar]
- 10.Segerink L.I., et al. , On-chip determination of spermatozoa concentration using electrical impedance measurements. Lab on a Chip, 2010. 10: p. 1018-1024. [DOI] [PubMed] [Google Scholar]
- 11.Cho B.S., et al. , Passively driven integrated microfluidic system for separation of motile sperm. Analytical Chemistry, 2003. 75: p. 1671-1675. [DOI] [PubMed] [Google Scholar]
- 12.Schuster T.G., et al. , Isolation of motile spermatozoa from semen samples using microfluidics. Reproductive BioMedicine Online, 2003. 7(1): p. 75-81. [DOI] [PubMed] [Google Scholar]


