Abstract
Absent or inappropriately low intact parathyroid hormone along with hypocalcemia is the diagnostic criterion of hypoparathyroidism. Clinically, hypoparathyroidism manifests predominantly as neuromuscular dysfunction caused by hypocalcemia. We present here a case of hypoparathyroidism wrongly and ineffectively treated as epilepsy for four years prior to reporting to our hospital. Hypoparathyroidism was diagnosed in our patient on the basis of low serum calcium (ionized and total), high phosphate and very low IPTH levels in face of normal magnesium levels along with radiological evidence of cerebral calcification. The authors stress on the need to include hypoparathyroidism in the differential diagnosis of seizures and the need to treat with 1, 25 dihydroxycholecalciferol.
Key words: hypoparathyroidism, hypocalcemia, vitamin D, intracerebral calcification, parathyroid hormone, seizures
CASE REPORT
A 30 year old female presented to the neurology out patients department for cramps, rigidity, tremor and twitching and abnormal movements of hands and feet. The patient complained that this problem was continuing despite treatment for 6 years. On checking her old prescriptions and reports, it was found that she was being treated with antiepileptics [eptoin 100mg bid] along with vitamin E [Evion400mgod].A CTscan of brain (done outside) revealed basal ganglia calcification [Figure 1]. She was referred to Endocrinology department. While in the OPD; two bouts of tetany were witnessed by the doctor, followed by recovery in a few minutes. She was married for twelve years, had her first child six years back, who died at 6 months of age due to high grade fever. Two years later, she had a son. Six months after delivery, she began to experience convulsions, tetany, stiffness of hands and feet and would fall down, and then recover completely on her own, in a few minutes. This happened about twice or thrice a month. She had long standing generalized weakness. She was employed in a bangle making factory, and had to give up her job due to this recurring health problem.
Figure 1.
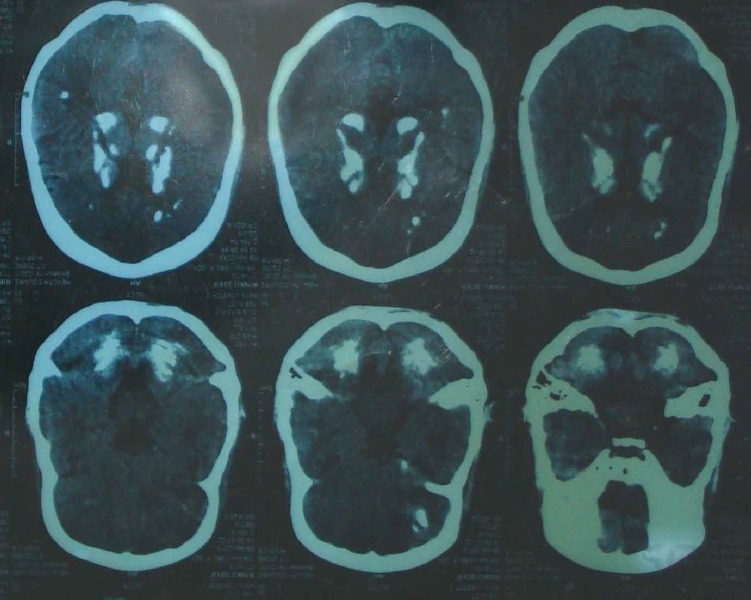
Non contrast CT scan of brain showing calcification
On examination, she weighed 32 kg, height 144 cm, and blood pressure 90/60 mm Hg. All other systems were normal on examination. Findings from an electroencephalogram were normal. Her laboratory investigations were as follows [reference range in parantheses].Serum calcium was 5.39 mg/dl [8.4-10.2], ionized calcium at 0.7 mmol/L[1.12-1.32 ], 24 hour urine calcium 259 mg [100-300], thyroid stimulating hormone [TSH] 6.73 µ IU/ ml [0.25-5], intact parathyroid hormone [IPTH] 13.54 pg/ml [15-65],phosphorus 7.57 mg/dl [2.5-4.5], magnesium 1.9 mg/dl [1.6-2.5], hemoglobin 10.5g/dl [12-15], fasting plasma glucose 100.4 mg/dl [70-110]. Albumin and 25 hydroxyvitamin D levels were within reference range. No nutritional, familial, congenital, infiltrative or autoimmune cause of hypoparathyroidism was obvious. Our tests for ANA and APLA by IFA and ELISA respectively tested negative Patient never had surgery or irradiation of neck. Eye examination revealed no abnormality. Cortisol level was within reference range, excluding hypoadrenalism. On clinical examination, there was no evidence of mucormycosis or any other fungal infection
The patient was diagnosed as primary hypoparathyroidism and treated with activated vitamin D [1, 25 dihydroxycholecalciferol].Three months later, her calcium level is 8.9 mg/dl and phosphate 5.2 mg/dl, intact parathyroid hormone is 15.9 pg/ml [15-65] and she has not experienced the seizures since two weeks. She has also regained her happiness and confidence to get back to her livelihood again.
DISCUSSION
Hypocalcaemia may be an asymptomatic laboratory finding or a life-threatening metabolic disturbance. The clinical presentation of hypocalcaemia in hypoparathyroidism is usually insidious and classical symptoms may be absent, even in patients with profound hypocalcaemia.[1] Its prevalence is 18% in all patients in hospital and 85% in the intensive care unit [2] The clinical algorithm for the workup of the patient who presents with hypocalcemia [3] aims to differentiate hypocalcemia associated with an absent or inappropriately low serum parathyroid hormone concentration (hypoparathyroidism) from hypocalcemia associated with an appropriate compensatory increase in parathyroid hormone. Transient hypoparathyroidism with biochemical abnormalities is commonly seen (>83% of cases) after thyroid surgery. [4] However, our patient had no recent or remote history of thyroid/neck surgery or irradiation. Magnesium level of our patient was normal, which ruled out nutritional deficiency.
Basal ganglia calcification occurring in idiopathic hypoparathyroidism, correlates with the duration of hypocalcaemia, choroid plexus calcification, seizures and cataract and has been observed to worsen despite maintenance of normal calcium levels. [5] The culprit is believed to be the high serum calcium-phosphorus product ratio and poor calcium control. A literature review of the clinical presentations of basal ganglia calcification revealed that there are diverse presentations, the most common including seizures, mental deterioration, and disorders of cerebellar or extra-pyramidal function. Movement disorders, chorea, or parkinsonism are present in 20 - 30% of patients with basal ganglia calcification, while some patients are asymptomatic [6] Decreased PTH level and hypocalcemia exclude other causes of intracerebral calcifications like pseudohypoparathyroidism, hyperparathyroidism, monoxide carbon intoxication, encephalitis, Fahr disease, idiopathic basal ganglia calcifications, Cocayne syndrome, tuberous sclerosis, neurofibromatosis, vascular disease (vascular malformations, chronic ischemic or hemorrhagic stroke), cerebral parasitosis [7] Our patient’s recovery from tetany with vitamin D and calcium, absence of family history of similar features and biochemical test results helped rule out Fahr’s syndrome [8] Due to financial constraints, no genetic testing could be done.
In a prospective study, Aggarwal and colleagues found there was a significant association between cognitive dysfunction and the duration of hypocalcemia, serum calcium levels, and calcium-phosphorus complex formation, but no association with serum 25(OH) D levels, serum PTH levels, or the volume or site of basal ganglia calcification. [9]
Presently, treatment consists of calcium supplementation and the use of vitamin D analogs, but PTH replacement is under investigation. [10] Oral calcium and vitamin D restore the overall calcium-phosphate balance. [11]
REFERENCES
- 1.Mukhopadhyay R, Strens LH, Winer JB, Ayuk JA, Gittoes NJ. Having the vision to measure calcium. J Neurol. 2010; 257(6):1032-1034. [DOI] [PubMed] [Google Scholar]
- 2.Cooper MS, Gittoes NJL. Diagnosis and management of hypocalcaemia. BMJ 2008; 336:1298-1302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bilezikian JP, Khan A, Potts Jr JT, Brandi ML, Clarke BL, Shoback D, et al. Hypoparathyroidism in the Adult: Epidemiology, Diagnosis, Pathophysiology, Target Organ Involvement, Treatment, and Challenges for Future Research. J Bone Miner Res. 2011; 26(10):2317–2337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dedivitis RA, Pfuetzenreiter EG, Jr, Nardi CE, Barbara EC. Prospective study of clinical and laboratorial hypocalcemia after thyroid surgery. Braz J Otorhinolaryngol. 2010; 76:71–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goswami R, Sharma R, Sreenivas V, Gupta N, Ganapathy A, Das S. Prevalence and progression of basal ganglia calcification and its pathogenic mechanism in patients with idiopathic Hypoparathyroidism. Clin Endocrinol (Oxf). 2012;77(2):200-206. [DOI] [PubMed] [Google Scholar]
- 6.Koller WC, Cochran JW, Klawans HL. Calcification of the basal ganglia: computerized tomography and clinical correlation. Neurology. 1979; 29(3):328-333. [DOI] [PubMed] [Google Scholar]
- 7.Sabau M, Comanescu A, Maghiar T, Dinulescu D. Hypoparathyroidism diagnosed by neurological signs and widespread intracerebral calcifications. Romanian journal of neurology 2010; 9[1], 44-50. [Google Scholar]
- 8.Saleem S, Aslam HM, Anwar M, Anwar S, Saleem M, Saleem A, et al. Fahr’s syndrome: literature review of current evidence. Orphanet Journal of Rare Diseases 2013; 8:156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aggarwal S, Kailash S, Sagar R. Neuro-psychological dysfunction in idiopathic hypoparathyroidism and its relationship with intracranial calcification and serum total calcium. Eur J Endocrinol 2013; 168:895-903. [DOI] [PubMed] [Google Scholar]
- 10.Wong EMM, Dahl M. Basal ganglia calcification in idiopathic hypoparathyroidism. BCMJ 2013; 55[10]:462-465. [Google Scholar]
- 11.Rizvi I, Ansari NA, Beg M, Shamim MD. Widespread Intracranial Calcification, Seizures and Extrapyramidal Manifestations in a Case of Hypoparathyroidism. North Am J Med Sci 2012; 4:369-372. [DOI] [PMC free article] [PubMed] [Google Scholar]


