Abstract
BACKGROUND
Acute coronary syndromes (ACS) are the leading cause of hospitalization and death in the modern world. Reliable indicators of risk assessment could be useful in clinical investigation. Results from recent studies suggest that apolipoprotein measurement and apoB:apoI ratio are superior to traditional lipids in the estimation of coronary risk. We compared apolipoprotein concentrations and apoB:apoAI index with traditional lipid measures in ACS patients.
METHODS
A study group consisted of 94 women diagnosed with ACS (STEMI=21, NSTEMI=25 and UA=48). Clinically healthy volunteers (n=30) served as controls. Measurements of serum cardiac TnI, lipid profile, high sensitivity C-reactive protein, apolipoprotein AI and apoB100 concentrations were performed and apoB:apoAI ratio was calculated.
RESULTS
ACS patients had significantly decreased median HDL-cholesterol, increased atherogenic indexes TC:HDL-C, apoB:apoAI and abnormally high CRP compared to controls. Median LDL-cholesterol and apoAI concentrations, although significantly higher in ACS patients, remained within the normal range. Comparison of atherogenic indexes in ACS patients has shown increased TC:HDL-C (>4) and apoB:apoAI (>0,3) in 60,4% and 96,8% of which 55,4% had moderate and high risk (>0,6). ApoB:apoAI ratio was of good diagnostic utility for discrimination between ACS cases and non-ACS controls (AUC=0,715), and little better than TC:HDL-C. In both groups similar percentage of increased LDL-C and triglycerides was observed whereas increased apoB concentration was three times more likely in ACS cases. The highest apoB:apoAI was observed predominantly in STEMI cases (49%) whereas the lowest in UA and NSTEMI (30%).
CONCLUSIONS
Determination of apolipoproteins and assessment of apoB:apoAI ratio seems to be useful and better tool than traditional lipid measures in assessing risk of acute coronary syndromes in women.
INTRODUCTION
There is no field in modern cardiology, which has changed in recent years as much as the diagnosis and treatment of acute coronary syndromes. Intensive development of invasive cardiology requires from a growing number of physicians knowledge on the rules of procedures used in acute coronary syndromes, and therefore the skills for rapid risk stratification and choice of treatment (1).
Acute coronary syndrome (ACS) is usually one of three diseases that involved the coronary arteries: ST elevation myocardial infarction (30%), non-ST elevation myocardial infarction (25%), or unstable angina (38%). Acute coranary syndromes are group of disorders characterized by changes in the coronary circulation, whose common feature is the significant reduction or cessation of flow in the coronary arteries. The most common cause of circulatory disorders is a blood clot formed at the rupture of atherosclerotic plaque. It should be emphasized that the cause of these syndromes is always the same, resulting from reduction of coronary flow, and differs only by degree of limitation. Lower limit of flow (TIMI scale) leads to the development of symptoms of UA or NSTEMI and the total cessation of flow leads to the development of STEMI (1,2).
According to Polish data published in the National Registry of Acute Coronary Syndromes (PL-ACS) every year in Polish hospitals 140.000 subjects diagnosed with ACS are treated, of which 60.000 with a diagnosis of unstable angina (UA), 30.000 with NSTEMI and 50.000 with diagnosis of STEMI (3).
The aim of diagnostic markers (cardiac troponin) is to identify patients with ACS even when there is no evidence of heart muscle damage (myeloperoxidase, ischemia-modified albumin, heart-fatty acid binding protein) and the aim of prognostic markers (including apolipoproteins apoAI and apoB100) is to reflect different components of pathophysiology of ACS. The concentration of apolipoprotein AI in the serum is approximately 100-130 mg/dL, while the vast majority of this protein, as much as 99% is a part of HDL and its catabolism largely relates to its function. ApoAI is involved in cholesterol reverse transport, which provides the antiatherogenic mechanism especially when it comes to removing excess cholesterol from macrophages resident in the place where plaques are formed.
The reference value for LDL-cholesterol (LDL-C) is <130 mg/dL and optimal apo B concentration is 90 mg/dL. Results above these values indicate an increased risk of cardiovascular disease (CVD) including ACS. Even the most accurate determination of LDL-C do not fully reflects the proatherogenic impact of this lipoprotein fraction. More credible in this regard is apoB100 concentration, whose molecule is present in every particle of low density lipoproteins (LDL), acting in a stoichiometric ratio of LDL (3). Studies showed that in subjects with normal or low levels of LDL-C, apo B is a better indicator of CVD risk. This comes from the fact that with the increased concentrations of LDL present in plasma, very often an increase of small LDL particles occurs. Small dense LDL have a lower cholesterol content than normal particles. This is evidenced by the fact that the difference in cholesterol content in large LDL particles compared with the small dense, expressed as the ratio of cholesterol to apoB reaches up to 25% (4). It is well accepted that because of that apoB is a better parameter reflecting the amount of LDL.
Previous reports have shown that apoB:apoAI ratio for men and women respectively <0,7 and <0,6 is associated with low risk for cardiovascular disease. ApoB:apoAI reflects the relationship between proatherogenic apo B-containing lipoproteins and anti-atherogenic HDL fractions (5). The advantage of calculating this index is that the concentration of apolipoproteins do not change after the meal and do not change in different times of day. In addition, with regard to the tests performed after acute coronary syndromes have occurred there is no matter how much time has elapsed since the in the blood collection. This is a valuable information, because in patients after a myocardial infarction the credibility of the lipids is questionned, if the blood was collected for 24 hours after the incident.
PATIENTS AND CONTROLS
STUDY GROUP
A study group consisted of 94 women (aged 69 ± 10 years) who were admitted to the Department of Cardiology and Internal Medicine between September 2008 and March 2009 and met clinical criteria of ACS. Electrocardiography examination was performed on admission and thereafter if clinically indicated. Echocardiography, stress tests and cardiac catheterization were performed if needed. ACS patients were subsequently definitely diagnosed with unstable angina (UA n=48), non-ST-elevation myocardial infarction (NSTEMI n=25) or ST-elevation myocardial infarction (STEMI n=21). Patients with heart failure, pulmonary embolism, chronic obstructive pulmonary disease, renal insufficiency, myocardial infarction within 6 weeks preceding the enrolment were excluded from the trial.
CONTROL GROUP
Clinically healthy volunteers (30 women, aged 54±4 years) with no evidence of present renal, metabolic or inflammatory disease, heart failure and recent myocardial infarction served as controls.
Hypertension was diagnosed if systolic blood pressure exceeded 140 mmHg and/or diastolic blood pressure was above 90 mmHg whereas dyslipidaemia if even one of the lipid profile components was above/under the following values: total cholesterol (TC) >200 mg/dL, triglycerides (TG) >150 mg/dL, LDL-C>130 mg/dL, HDL-cholesterol (HDL-C) <50 mg/dL according to ESH/ESC recommendations. The frequency of dyslipidemia in the study group was 87% and in the control group was 50%.
The study protocol was approved by the Bioethics Committee at Nicolaus Copernicus University in Torun Collegium Medicum in Bydgoszcz and written informed consent has been obtained from all patients.
MATERIALS AND METHODS
Venous blood samples were collected from patients on hospital admission within 6 hours of the chest pain onset. From controls fasting venous blood samples were collected in the morning. Serum was assayed on admission for cTnI, lipid parameters, glucose and BNP (Architect ci8200, Abbott Diagnostics). Any increase of cTnI above 0.032 ng/mL (the 99th percentile for the healthy population measured with 10% CV) was considered a positive result.
Serum ApoAI and apoB100 concentrations were measured in samples stored frozen at /?/-80ºC not longer than 6 months (Abbott ARCHITECT ci8200) and the ratio of apoB:apoAI was calculated. ApoB concentration >90 mg/dL was accepted as abnormal. ApoB:apoAI ratio <0,3 and TC:HDL-C <4 were accepted as optimal. According to Walldius et al (6) ApoB:apoAI ratio within 0,3-0,6 for women was considered as low risk and >0,8 as high risk of myocardial infarction.
Data were presented as medians and 25th and 75th percentiles. U-Mann-Whitney test and ANOVA were used to compare differences. Statistical analysis was performed using Statistica 8.0 for Windows.
RESULTS
Table 1 shows the general characteristics of the study groups. Women with ACS had significantly lower median HDL-C and CRP compared to controls. Median LDL-C and apoAI concentrations, although significantly higher in ACS patients than in controls, remained within the accepted normal range. Atherogenic indexes TC:HDL-C and apoB:apoAI were significantly increased in women with ACS. Median apoB:apoAI ratio was found to be in the range of moderate risk in patients with diagnosed ACS while in control women reflected low risk. If atherogenic indexes were compared in patients with ACS the increased TC:HDL-C ratio (>4) was found in 60,4% of women whereas increased apoB:apoAI ratio (>0,3) was found in 96,8% of which 55,4% had moderate and high risk. In the control group apoB:apoAI ratio reflected low risk (<0,6) in 83% and TC:HDL-C (≤4) in 70%.
TABLE 1.
CHARACTERISTICS OF THE STUDY GROUPS
| Parameter | ACS patients (Females n=94) |
Control group (Females n=30) |
|---|---|---|
| Age (years) | 69±10* | 54±4 |
| cTnI (ng/mL) | 0,03 (0,002-0,33) | nd |
| CRP (mg/L) | 3,2 (1,18-6,98) | 1,68 (0,96-3,63) |
| TC (mg/dL) | 195 (164-233) | 195 (181-212) |
| HDL-C (mg/dL) | 45 (39-55)* | 58 (51-63) |
| TC:HDL-C | 4,3 (3,5-4,8)* | 3,3 (2,8-4,2) |
| LDL-C (mg/dL) | 124 (98-153)* | 116 (102-129) |
| TG (mg/dL) | 112 (87-152) | 94 (75-125) |
| apoAI (mg/dL) | 132 (114-148)* | 155 (140-169) |
| apoB (mg/dL) | 80 (64-97) | 73 (67-85) |
| apoB:apoAI | 0,62 (0,5-0,75)* | 0,5 (0,42-0,57) |
*differences between ACS and control group: p<0,05; nd - non-detectable
Frequency of dyslipidemia and abnormal concentration of apolipoproteins among ACS patients and control women was shown in Table 2. Interestingly, the most characteristic feature of ACS subjects was decreased HDL-C (median 45 vs 58 mg/dL in controls) as well as decreased apoAI concentration. On the other hand, in both groups very similar percentage of increased LDL-C and triglycerides was observed, however increased apoB concentration was three times more likely in ACS cases.
TABLE 2.
FREQUENCY OF DYSLIPIDEMIA AND ABNORMAL APOLIPOPROTEIN CONCENTRATIONS IN THE STUDY GROUPS.
| Parameter | Dyslipidemia in ACS (%) | Dyslipidemia in controls (%) |
|---|---|---|
| TC >200 mg/dL | 44 | 80 |
| LDL-C>130 mg/dL | 44 | 47 |
| HDL-C<50 mg/dL | 61 | 40 |
| TG>150 mg/dL | 28 | 27 |
| apoB>90 mg/dL | 32 | 10 |
| apoAI<130 mg/dL | 46 | 7 |
In the study group a moderate direct correlation of TC:HDL-C with LDL-C and apoB (r=0,67 and 0,60; p<0,0001) was observed. ApoB:apoAI correlated directly with LDL-C (r=0,58; p<0,001) and there was a strong relation with apoB and TC:HDL-C as well (r=0,80; r=0,73; p<0,001). We did not find any relationship between CRP and atherogenic indexes, however among ACS patients with TC:HDL-C >4 and apoB:apoAI >0,6 CRP concentration >3 mg/L was found in 52% and 38%, respectively.
ROC analysis was performed for the atherogenic indexes. Calculated apoB:apoAI was of good diagnostic utility for discrimination between ACS cases and non-ACS controls, area under the ROC curve (AUC) was 0,715 whereas that of TC:HDL-C was smaller AUC=0,705.
Table 3 shows the characteristics of the study group with the clinical diagnosis. The differences between measured parameters, excluding cardiac troponin I, in ACS patients with different clinical diagnosis did not reach statistical significance.
TABLE 3.
CHARACTERISTICS OF THE ACS GROUP ACCORDING TO CLINICAL DIAGNOSIS
| Parameter | STEMI (n=21) | NSTEMI (n=25) | UA (n=48) |
|---|---|---|---|
| Age (years) | 69,5±10,7 | 71,7±10,2 | 66,9±9,1 |
| CRP (mg/L) | 4,5 (2,0-7,0) | 5,3 (1,0-9,2) | 2,4 (1,2-5,1) |
| cTnI (ng/mL) | 0,3 (0,1-4,7) | 0,36 (0,03-2,4) | 0,006 (0,0-0,02)* |
| TC (mg/dL) | 209 (179-229) | 195 (160-233) | 190 (162-233) |
| HDL-C (mg/dL) | 48 (41-58) | 42 (36-51) | 45 (40-53) |
| TC:HDL-C | 4,4 (3,5-4,7) | 4,4 (3,3-4,9) | 4,1 (3,5-4,8) |
| LDL-C (mg/dL) | 142 (116-156) | 124 (90-149) | 113 (95-149) |
| TG (mg/dL) | 142 (116-156) | 124 (90-149) | 113 (95-149) |
| apoAI (mg/dL) | 135±21,9 | 130±24,6 | 132±25,1 |
| apoB (mg/dL) | 86 (71-102) | 80 (59-91) | 76 (63-103) |
| apoB:apoAI | 0,66±0,16 | 0,6±0,21 | 0,64±0,21 |
STATISTICALLY SIGNIFICANT DIFFERENCES * P <0.05 (ANOVA TEST)
The percentage distribution of cases in apoB: apoAI tertiles, depending on the diagnosis and in controls was evaluated (Fig.1). As shown, the highest apoB:apoAI (0,65-1,29) was observed predominantly in patients with STEMI (49%). On the contrary, the lowest apoB:apoAI values were found mostly among patients with NSTEMI and UA (30%). Over 55% of controls had the lowest apoB:apoAI index.
FIG. 1.
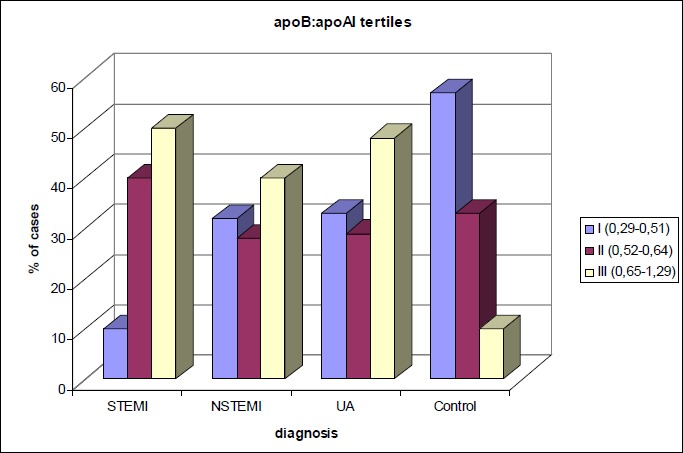
THE PERCENTAGE DISTRIBUTION OF CASES IN APOB: APOAI TERTILES, DEPENDING ON THE DIAGNOSIS AND IN CONTROLS.
DISCUSSION
In this preliminary study, performed in women with diagnosis of ACS, we aimed to compare apolipoprotein B and AI concentrations and value of their atherogenic ratio with other biochemical parametrs, associated with cardiovascular risk such as lipids and inflammatory markers.
It has been estimated that apolipoproteins are better predictors of CHD than lipids, and several studies have also shown that the value of apoB to apoAI ratio is a very good diagnostic tool in assessing coronary risk. The higher the value of apoB:apoAI, the higher the risk of cardiovascular incidents (5). We have shown that apoB:apoAI ratio was of good diagnostic utility for discrimination between ACS cases and non-ACS controls (AUC=0,715), and little better than TC:HDL-C.
Considering the results of our study, only HDL-C and LDL-C and apo-AI as well as both atherogenic ratios TC:HDL-C and apoB:apoAI were significantly different between control subjects and ACS patients. In this study we have shown that apoAI concentration was significantly lower and the ratio of apoB:apoAI was higher in ACS patients than in the control group. Decreased apoAI concentration was almost seven times more frequent and increased apoB was three times more frequent in ACS cases compared to controls. Due to decrease of HDL-C and increase of LDL-C, atherogenic ratios has increased in ACS patients. Each HDL particle have a two or three molecules of apoAI on the surface and account for nearly all serum apoAI (7). Similarly, each LDL particle has exactly one molecule of apoB on the surface. Since the ratio of cholesterol to apolipoproteins in LDL molecule, as well as in HDL may vary, the positive and negative associations of both apoB and apoAI and of LDL-C and HDL-C with risk may differ. However, many studies have confirmed that apoB and apoAI are even stronger correlates of risk than LDL-C and HDL-C are (7,8). Going further, the cholesterol balance determined as the apoB:apoAI ratio has been shown to be a better marker than lipids, lipoproteins and lipid ratios (5,6). It has been demonstrated in one of the first AMORIS study, that the coronary risk and mortality due to CHD is associated with high apoB and higher values of apoB:apoAI, and that this relationship is stronger than that for LDL-C (4,5,7). Other subsequent studies, including EPIC-Norfolk study, ULSAM and the MONICA/Cora confirmed that the apoB:apoAI ratio is a useful index of both nonfatal and fatal myocardial infarction (MI) (5). Moreover, the INTERHEART study showed that the ratio of apoB to apoAI was not only the strongest risk factor in predicting MI but was also the most prevalent risk factor of all risk factors independent of age, sex and ethnicity (4).
Taking into account the differences between the ACS groups, according to clinical diagnosis, none of them, except for cTnI was statistically significant. However, when the distribution in tertiles was assessed, the highest apoB:apoAI ratio was observed predominantly in STEMI patients. On the contrary, the lowest values of the ratio were found predominantly among patients with UA and NSTEMI. From a clinical point of view it is confirmed by the results of recently published studies (10,11). In one of them the impact of apoB:apoAI on the damage to cardiac function after a first ST-elevation AMI was explored. A significant relationship between apoB:apoAI ratio and echocardiographical parameters was observed, however apolipoproteins and conventional lipid parameters did not show such associations. Based on the results of this study it was concluded that the value of apoB:apoAI ratio in ACS patients on admission could predict the elevation of left ventricular (LV) filling pressure 2 weeks after a first STEMI onset. The higher the ratio on admission, the greater the LV damage. This results might explain why the higher values of the apoB:apoAI ratio were frequently followed by fatal MI (11). Thus the determination of apoB:apoAI on admission to the hospital can distinguish the patients of the greatest risk.
On the other hand, taking into account the frequency of dyslipidemia and abnormal apolipoprotein concentrations in the study group, we observed that percentage of dyslipidemia in patients with ACS, was much higher in the case of apolipoproteins as compared to control group. Moreover, among ACS patients with TC:HDL-C>4 and apoB:apoAI>0,6, thus reflecting the increased risk, CRP concentration >3mg/L was found in 52% and 38% respectively. This suggests that the determination of apoB: apoAI allows to further narrowing the area of risk. The superiority of cardiac markers for diagnosis in ACS patients remains indisputable, however, apolipoprotein, and especially the apoB: apoAI seem to be better indicators of the cardiovascular risk than parameters of lipid profile.
On the basis of the data of the present study we conclude that determination of apolipoproteins and in particular values of apoB:apoAI ratio may be useful and better tool than traditional lipid measures in assessing risk of acute coronary syndromes in women, as well as for the secondary prevention in ACS patients.
References
- 1.Acute coronary syndromes. Edited by Opolski Grzegorz, Filipiak Krzysztof J., Polonski Lech. Urban&Partner Wroclaw 2002. [Google Scholar]
- 2.Torres M, Moayedi S: Evaluation of the acutely dyspneic elderly patient. Clin Geriatr Med. 2007;23:307-325. [DOI] [PubMed] [Google Scholar]
- 3.Ogolnopolski Rejestr Ostrych Zespolow Wiencowych PL-ACS. www.rejestrozw.pl. [PubMed]
- 4.Chan DC, Watts GF. Apolipoproteins as markers and managers of coronary risk. QJM. 2006;99:277-287. [DOI] [PubMed] [Google Scholar]
- 5.Walldius G, Jungner I. The apoB/apoA-I ratio: a strong, new risk factor for cardiovascular disease and a target for lipid-lowering therapy--a review of the evidence. J Intern Med. 2006;259:493-519. [DOI] [PubMed] [Google Scholar]
- 6.Walldius G, Jungner I. Apolipoprotein B and apolipoprotein A-I: risk indicators of coronary heart disease and targets for lipid-modifying therapy. J Intern Med. 2004;255:188-205. [DOI] [PubMed] [Google Scholar]
- 7.Parish S et al.. The joint effects of apolipoprotein B, apolipoprotein A1, LDL cholesterol, and HDL cholesterol on risk: 3510 cases of acute myocardial infarction and 9805 controls. Eur Heart J. 2009;30:2137-2146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Graziani MS, Zanolla L, Righetti G, Marchetti C, Mocarelli P, Marcovina SM. Plasma apolipoproteins A-I and B in survivors of myocardial infarction and in a control group. Clin Chem. 1998;44:134-140. [PubMed] [Google Scholar]
- 9.Sacks FM: The apolipoprotein story. Atherioscler Suppl, 2006;7:23-27 [DOI] [PubMed] [Google Scholar]
- 10.Schmidt C, Wikstrand J. High apoB/apoA-I ratio is associated with increased progression rate of carotid artery intima-media thickness in clinically healthy 58-year-old men: experiences from very long-term follow-up in the AIR study. Atherosclerosis. 2009;205:284-289. [DOI] [PubMed] [Google Scholar]
- 11.Iwahashi N, Kosuge M, Okuda J, Tsukahara K, Tahara Y, Hibi K, Ebina T, Sumita S, Ishikawa Uchino K, Umemura S, Kimura K. Abstract 1364: Impact of the ApoB/A1-Ratio on the Prediction of the Elevation of Left Ventricular Filling Pressure After a First STEMI; Circulation 2009;120:S489. [Google Scholar]


