Abstract
Background and Purpose
Get With The Guidelines (GWTG)-Stroke is a national, hospital-based quality improvement program developed by the American Heart Association. While studies have suggested improved processes of care in GWTG-Stroke participating hospitals, it is not known whether this improved care translates into improved clinical outcomes compared to non-participating hospitals.
Methods
From all acute care US hospitals caring for Medicare beneficiaries with acute stroke between April 2003 and December 2008, we matched hospitals that joined the GWTG-Stroke program with similar hospitals that did not. Using a difference-in-differences design, we analyzed whether hospital participation in GWTG-Stroke was associated with a greater improvement in clinical outcomes compared to the underlying secular change.
Results
The matching algorithm identified 366 GWTG-Stroke-adopting hospitals that cared for 88,584 acute ischemic stroke admissions and 366 non-GWTG-Stroke hospitals that cared for 85,401 acute ischemic stroke admissions. Compared with the PRE period (18 – 6 months prior to program implementation), in the EARLY period (0 - 6 months after program implementation), GWTG-Stroke hospitals had accelerated increases in discharge to home, and reduced mortality at 30 days and 1 year. In the SUSTAINED period (6 – 18 months after program implementation), the accelerated reduction in mortality at 1 year was sustained, with a trend toward sustained accelerated increase in discharge home.
Conclusions
Hospital adoption of the GWTG-Stroke program was associated with improved functional outcomes at discharge and reduced post-discharge mortality.
Keywords: Ischemic stroke, outcomes, acute stroke, Get with the Guidelines stroke, quality of care
Introduction
Quality improvement programs frequently focus on process of care rather than clinical outcome metrics.1 Process of care measures provide rich feedback on target achievement – they apply in all eligible patients and are directly responsive to system-level changes and intervention.2 In contrast, clinical endpoints, such as mortality and functional recovery, occur in only a fraction of patients, require well validated risk adjustment models, and may be less readily responsive to system intervention. However, process outcomes are almost always designed to be a means to an end. The ultimate goal of systems interventions is to improve the health state of patients. Examples of the success of quality improvement programs altering clinical endpoints on a national scale in the United States are few.
Stroke is a devastating disease, the leading combined cause of death and disability worldwide, affecting more than 795,000 people in the U.S. each year.3 Stroke exacts a financial burden greater than $38 billion annually in the United States.4, 5 The Get With The Guidelines-Stroke (GWTG-Stroke) program was developed by the American Heart Association (AHA) as a national quality improvement program for hospitals to improve stroke care infrastructure utilizing a multidisciplinary team approach, and incorporating elements such as patient management toolkits, multidisciplinary workshops and stakeholder organizational meetings, and offering data collection, and decision support.5,6 Programs who enter into GWTG-Stroke have access to a multitude of resources and staff support, and submit patient clinical data utilizing special data collection tools, for which they receive feedback reporting. Each program upon initiation enters 30 clinical patient records into the Patient Management Tool, which becomes their unique baseline to which future performance is measured. The Patient Management Tool measures seven Achievement Measures, including deep venous thrombosis prophylaxis, early antithrombotic administration, and time to intravenous thrombolysis for eligible acute ischemic stroke patients. Improvement and success is recognized through the GWTG-Stroke program’s Achievement Awards. After a pilot phase, hospitals began enrolling in GWTG-Stroke in April 2003. By the end of 2008, there were 1,199 hospitals participating in the quality improvement program.
Prior studies have shown that hospital participation in the GWTG-Stroke program was associated with increased achievement of process quality metrics, including increased frequency of acute pharmacologic treatment (thrombolysis and early antithrombotics), interventions to prevent early complications (swallowing assessments, deep venous thrombosis prophylaxis), and start of secondary stroke prevention prior to discharge (anticoagulation for atrial fibrillation, cholesterol lowering).6-8 A prior analysis has also examined long-term clinical outcomes at hospitals participating in the GWTG-Stroke program.6 However, the impact of program participation on clinical outcomes while accounting for the underlying secular trend that occurred in non-participating hospitals has not been determined.
The Medicare administrative dataset captures important clinical outcomes in older stroke patients throughout the United States. In this study, we sought to identify whether implementation of the GWTG-Stroke program was associated with greater improvement in clinical outcomes for patients at GWTG-Stroke hospitals than for patients at matched non-GWTG-Stroke hospitals during the same time period.
Methods
We evaluated associations between implementation of the GWTG-Stroke quality improvement program and changes in discharge destination, mortality, and rehospitalization. We combined two matched cohorts and used “difference in differences” design to distinguish program-associated changes from secular changes in outcomes occurring during the study period.9-12 Changes in outcomes at hospitals that joined the GWTG-Stroke program were compared with changes in outcomes at matched hospitals that did not join the GWTG-Stroke program (changes in these latter hospitals reflect the underlying secular changes in stroke outcomes).
GWTG-Stroke is a national voluntary stroke registry and performance improvement initiative. In GWTG-Stroke, participating hospitals use an internet-based patient management tool (Outcome Sciences, Cambridge, MA) to add data to a central database on consecutive acute ischemic stroke patients. The methods for data abstraction have been previously described.13, 14 The GWTG-Stroke dataset included information on care processes during acute hospitalization and patient status at the end of an acute cerebrovascular admission.
We analyzed data from the Centers for Medicare & Medicaid Service (CMS) files, which includes data for all United States beneficiaries with fee-for-service Medicare claims aged 65 years and older. “Previous research has shown that Medicare beneficiaries admitted to GWTG-Stroke hospitals with the diagnosis of acute ischemic stroke are similar to Medicare beneficiaries admitted to non-GWTG-Stroke hospitals.14 However, differences were noted in hospital characteristics of GWTG-Stroke and non-GWTG-Stroke hospitals, indicating a need for analytic control of hospital variation.14 The CMS dataset included information on post-discharge outcomes at 1 and 12 months after an index hospitalization.
Methods: Matching algorithm/criteria
We compared hospitals that implemented GWTG-Stroke between 2003 and 2008 with matched hospitals that did not implement GWTG-Stroke during that period. To identify GWTG-Stroke hospitals, GWTG-Stroke registry admissions were first linked to CMS claims by probabilistic matching. Hospitals with multiple linked admissions were identified as GWTG-Stroke hospitals.
Control group hospitals were identified from among 3,013 non-GWTG-Stroke hospitals and were matched to the GWTG-Stroke hospitals on the basis of the following 5 criteria: a) hospital teaching status, b) hospital region, c) similar calendar time periods before the GWTG-Stroke stroke joined the program (allowable range is within ±90 days), d) annual ischemic stroke volume (allowable range is within ±20 of annual ischemic stroke volume in the GWTG-Stroke hospital), and e) 1 year observed all-cause mortality rate during the period before the GWTG-Stroke hospital joined the program (allowable range is within ±2.5% of the rate in GWTG-Stroke hospital). Teaching status was determined by hospital listing on the rolls of the Council of Teaching Hospitals. For each GWTG-Stroke hospital, one matched hospital was randomly selected from the non-GWTG-Stroke hospitals that met the above 5 matching criteria.
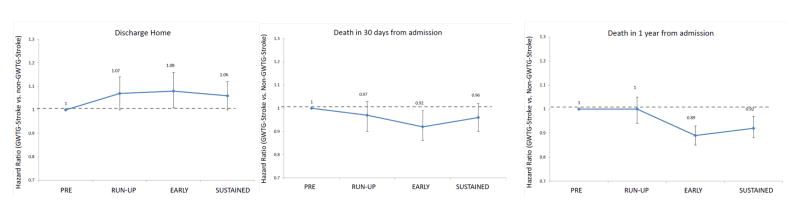
Methods: Definition of Time Period
We defined 4 separate time epochs indexed to the date a GWTG-Stroke hospital joined the GWTG-Stroke program: 1) the PRE period was defined as the time period from 18 months to 6 months prior to a hospital joining the GWTG-Stroke program; 2) the RUN-UP period as the time from 6 months to 1 day before starting date of enrollment into the program; 3) the EARLY period as the time from day 0 to 6 months after joining GWTG-Stroke; and 4) the SUSTAINED period as the time period from 6 months to 18 months after enrollment date (Figure 1). We expected there might be intermediate effects in the RUN-UP period, when hospitals may have been implementing system interventions in anticipation of joining the GWTG-Stroke program, and in the EARLY period, when hospitals would still be building and refining the full system intervention. Accordingly, the primary comparison of interest was the PRE period versus the SUSTAINED period. Because our study period was April 1, 2003 to December 1, 2008, to ensure each GWTG-Stroke qualifying site had a sufficient time span before and after the starting date, we excluded sites that started GWTG-Stroke before April 1, 2004 or after December 31, 2007, leaving only sites with at least 6 months in the PRE period and 6 months in the SUSTAINED period. We also excluded sites with small samples sizes (less than 10 admissions) in either the PRE or SUSTAINED periods. At the GWTG-Stroke hospitals and the matched non-GWTG-Stroke hospitals, analytic populations used the acute ischemic admissions with primary discharge diagnosis ICD-9 code 434 or 436 in each of the 4 time periods. To identify an index admission (and retain only that index admission for each patient), for GWTG-Stroke patients, we used the first linked admission as the index admission, and for non-GWTG-Stroke patients, we treated the first eligible admission as the index admission.
Figure 1.
Matching algorithm and timeline of study design.
At the GWTG-Stroke hospitals and the matched non-GWTG-Stroke hospitals, analytic populations were identified in the following manner. We first began by restricting to admissions for acute ischemic stroke at hospitals participating in GWTG-Stroke, with a discharge date between April 1, 2003 and December 12, 2008, who were insured by Medicare and linked to their FFS Medicare data. In the period before GWTG-Stroke launch at a target hospital and its matched non-GWTG-Stroke hospital, we identified ischemic stroke admissions (primary discharge diagnosis ICD-9 code 434 or 436) in the FFS Medicare files. In the period after GWTG-Stroke launch at a hospital, we linked GWTG-Stroke admissions to fee-for-service (FFS) Medicare data using a previously described probabilistic matching process.8
Methods: Statistical Analysis
The hospital and patient characteristics were described using percentages for categorical variables and mean (±standard deviation) for continuous variables. They were compared between the GWTG-Stroke hospital and matched non-GWTG-Stroke hospitals. The Wilcoxon rank-sum test and Chi-square test were used to test the difference for the continuous and categorical variables, respectively.
The primary clinical outcomes analyzed included functional status at discharge (discharge to home) and 6 measures of mortality (30 day all-cause mortality, 30 day stroke mortality, 30 day cardiovascular mortality, 1 year all-cause mortality, 1 year stroke mortality, and 1 year cardiovascular mortality). Secondary clinical outcomes included length of stay and 6 measures of readmission (30 day all-cause rehospitalization, 30 day stroke rehospitalization, 30 day cardiovascular rehospitalization, 1 year all-cause rehospitalization, 1 year stroke rehospitalization, 1 year cardiovascular rehospitalization).
As first step in the longitudinal analysis we first examined the differences in outcomes over the 4 time periods (i.e., Pre, RUN-UP, EARLY, and SUSTAINED) in GWTG-Stroke hospitals only, and separately in the non-GWTG-Stroke hospitals using Cox proportional hazard models. Each model was adjusted for the following covariates: patient demographics (age, sex, race-ethnicity), and patient medical history (hypertension, acute myocardial infarction, stroke, coronary artery disease, diabetes, pneumonia, renal disease, chronic obstructive pulmonary disease, dementia, carotid stenosis, and peripheral disease), and hospital characteristics (rural vs. urban setting, number of beds, and annual number of ischemic stroke discharges).
We then used a difference in differences analysis to compare the changes in outcomes that occurred over time in GWTG hospitals to the changes that occurred over the same time period in non-GWTG hospitals (it is assumed that these latter changes represent the underlying secular changes).12 These analyses were based on the 366 matched pairs of hospitals and were generated from stratified Cox proportional hazard models for time to event outcomes, and conditional logistic regression models for dichotomous outcomes where each matched pair (n=366) was defined as its own stratum. The impact of GWTG participation was estimated from the hazard ratio (from the Cox model) or the odds ratio (from the logistic model) that is generated from the interactions term between the study period and the GWTG indicator. A statistically significant interaction indicates that the change in the outcome was greater (or lesser) in the hospitals that joined the GWTG-program compared to hospitals that did not join the program.
All models included the main effects of study periods i.e., RUN-UP, EARLY or SUSTAINED vs. PRE period, a binary indicator variable of GWTG vs. non-GWTG hospital status, and the interaction between the two. All models were adjusted for the covariates previously mentioned. The annual number of ischemic stroke discharges (+/-20) (Figure 1) was used for matching hospitals but it was not an exact matching, so it was also included in the adjustment.
The impact of GWTG participation was estimated from the hazard ratio (from the Cox model) or the odds ratio (from the logistic model) that is generated from the interactions term between the study period and the GWTG indicator. A statistically significant interaction indicates that the change in the outcome was greater (or lesser) in the hospitals that joined the GWTG-program compared to hospitals that did not join the program. Additionally, to quantify the clinical impact of program implementation in absolute values, we derived risk-adjusted rates of discharge to home and mortality at 30 days and 1 year for the most common baseline patient. The characteristics used to define the most common baseline patient were: female, 80 years old, white, non-Hispanic, no past medical history, and from an average hospital (300 bed size hospital, non-teaching, annual average ischemic case load of 100-300 strokes, and urban). We analyzed these rates for all 4 time epochs.
All analyses were performed using SAS Version 9.1 or higher software (SAS Institute, Cary, NC). All authors have read and agree to the manuscript as written.
Results
Between April 1, 2003 and December 12, 2008, the FFS Medicare dataset included 1,199 GWTG-Stroke hospitals and 3,013 hospitals not participating in GWTG-Stroke. Among the GWTG-Stroke hospitals, we excluded 402 that joined the program before April 1, 2004 or after December 31, 2007 (because they did not have at least 1 year of BEFORE and AFTER data), and 77 hospitals that had fewer than 10 patients in either the PRE or SUSTAINED time periods. Among the remaining 720 GWTG-Stroke hospitals, 366 could be matched to one non-GWTG-Stroke hospital; these 366 GWTG-Stroke and 366 non-GWTG-Stroke hospitals constituted the final analytic population. The selected GWTG-Stroke hospitals contained sites that joined the program in each of the potential entry years, including 64 (17.5%) in calendar year 2004, 201 (54.9%) in 2005, and 101 (27.6%) in 2006.
The final analytic population comprised 173,985 patients, including 88,584 patients at the 366 GWTG-Stroke sites, and 85,401 patients at the 366 matched non-GWTG-Stroke sites (Figure 1). The GWTG-Stroke and non-GWTG-Stroke samples were generally well-matched in both hospital and patient characteristics (Table 1). Among hospital features, GWTG-Stroke hospitals were slightly more likely to be non-rural and have more beds. Among patient features, patients at GWTG-Stroke hospitals were slightly more likely to be older, white, and non-diabetic. In total, 89.7% (79,495 patients) patients admitted to GWTG-Stroke hospitals and 93.6% (79,967 patients) admitted to non-GWTG-Stroke hospitals were admitted under ICD-9 diagnosis code 434, of which 81.3% and 85.0%, respectively, were categorized under the diagnosis code 434.91. The majority of the remainder of admissions were categorized under ICD-9 diagnosis code 436 (5.75% in GWTG-Stroke linked admissions, 6.36% in non-GWTG-Stroke admissions), 435, or 433.
Table 1.
Characteristics of Hospitals and Patients in the GWTG-Stroke and Matched Non-GWTG-Stroke Samples
| Hospital Characteristics | GWTG-Stroke N=366 |
Non-GWTG-Stroke N=366 |
P value |
|---|---|---|---|
| Number of AIS discharges in 2008 | 109 (±63) | 104 (±60) | 0.22 |
| Categorized volume of AIS discharges in 2008 | 0.40 | ||
| 0-100 | 51.6% | 56.6% | |
| 101-300 | 47.0% | 42.4% | |
| 301+ | 1.4% | 1.1% | |
| Teaching Hospital | 9.6% | 9.6% | 1.00 |
| Region | |||
| Northeast | 29.2% | 29.2% | 1.00 |
| South | 36.1% | 36.1% | |
| Midwest | 18.0% | 18.0% | |
| West | 16.7% | 16.7% | |
| Rural Location | 0.6% | 4.9% | 0.0003 |
| Number of Beds | 293 (±173) | 264 (±163) | 0.001 |
| Patient Characteristics in the PRE Period | N=29217 | 29613 | |
| Age (mean years) | 79.6 (±7.9) | 79.3 (±7.9) | <0.0001 |
| Sex (female) | 59.5% | 60.4% | 0.03 |
| White | 84.5% | 82.9% | <0.0001 |
| Comorbidities | |||
| Hypertension | 77.8% | 78.1% | 0.36 |
| Prior Stroke | 8.6% | 9.1% | 0.05 |
| Acute myocardial infarction | 10.5% | 10.4% | 0.70 |
| Coronary artery disease | 33.7% | 34.1% | 0.36 |
| Diabetes | 28.3% | 30.2% | <0.0001 |
| Pneumonia | 8.4% | 8.7% | 0.29 |
| Renal disease | 7.1% | 7.4% | 0.09 |
| COPD | 18.6% | 19.7% | 0.001 |
| Dementia | 4.2% | 4.9% | <0.0001 |
| Carotid stenosis | 9.4% | 9.0% | 0.07 |
| Peripheral vascular disease | 9.7% | 9.8% | 0.70 |
| Clinical Outcomes in the PRE Period* | |||
| Death within 30 days, N (%) | 4519 (15.5%) | 4263 (14.4%) | 0.0003 |
| Death in 1 year from discharge, N (%) | 7753 (28.5%)* | 7461 (27.0%)* | 0.0001* |
| Discharged home, N (%) | 7169 (24.5%) | 7810 (26.4%) | <0.0001 |
| *missing data (3969 from total sample) |
Observed rates
Supplemental Table I shows the hospital and patient characteristics for the 366 GWTG-Stroke hospitals that were matched to a non-GWTG-Stroke hospital and the 354 GWTG-Stroke hospitals that could not be matched to a non-GWTG-Stroke hospital. Smaller GWTG-Stroke hospitals and non-teaching GWTG-Stroke hospitals were more likely to find a valid match among non-GWTG-Stroke hospitals. Patient baseline characteristics and clinical outcomes were similar between the GWTG-Stroke hospitals with and without a valid non-GWTG-Stroke control hospital.
Unadjusted and adjusted changes in discharge to home and mortality outcomes at the 366 GWTG-Stroke during the 4 time epochs (PRE, RUN-UP, EARLY, SUSTAINED) are shown in Table 2. Equivalent results for the 366 non-GWTG-Stroke hospitals are shown in Table 3. At GWTG-Stroke hospitals, in the adjusted analyses, improvements in 30-day and 1-year mortality were seen in the EARLY period and improvements in discharge to home and in 30-day and 1-year mortality were seen in the SUSTAINED period. In contrast, at non-GWTG-Stroke hospitals, no improvements were seen in the EARLY period and improvement only in 30-day mortality was seen in the SUSTAINED period.
Table 2.
Unadjusted and Adjusted Analyses of comparison of Discharge Home/Mortality Outcomes in RUN-UP, EARLY, and SUSTAINED period vs. PRE period, for GWTG-Stroke Hospitals
| Discharge Home/Mortality Outcomes | RUN-UP vs. PRE | EARLY vs. PRE | SUSTAINED vs. PRE | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Hazard Ratio | 95% CI | P value | Hazard Ratio | 95% CI | P value | Hazard Ratio | 95% CI | P value | |
| Unadjusted Analyses | |||||||||
| Discharge Home | 1.04 | 0.99-1.09 | 0.10 | 1.03 | 0.99-1.08 | 0.14 | 1.05 | 1.01-1.09 | 0.009 |
| Death in 30 day from admission | 1.01 | 0.96-1.07 | 0.63 | 0.94 | 0.89-0.99 | 0.02 | 0.95 | 0.91-0.99 | 0.01 |
| Death in 1 year from discharge | 1.03 | 0.99-1.07 | 0.15 | 0.94 | 0.90-0.98 | 0.001 | 0.96 | 0.93-0.99 | 0.02 |
| Adjusted Analyses | |||||||||
| Discharge Home | 1.04 | 0.99-1.09 | 0.12 | 1.04 | 0.99-1.09 | 0.14 | 1.08 | 1.04-1.12 | 0.0002 |
| Death in 30 day from admission | 1.00 | 0.95-1.05 | 0.95 | 0.92 | 0.88-0.97 | 0.002 | 0.91 | 0.87-0.95 | <.0001 |
| Death in 1 year from discharge | 1.02 | 0.98-1.06 | 0.36 | 0.91 | 0.88-0.95 | <.0001 | 0.91 | 0.88-0.94 | <.0001 |
Table 3.
Unadjusted and Adjusted Analyses of comparisons of Discharge Home/Mortality Outcomes in RUN-UP, EARLY, SUSTAINED period vs. PRE period for Non-GWTG-Stroke Hospitals
| Discharge Home/Mortality Outcomes | RUN-UP vs. PRE | EARLY vs. PRE | SUSTAINED vs. PRE | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Hazard Ratio | 95% CI | P value | Hazard Ratio | 95% CI | P value | Hazard Ratio | 95% CI | P value | |
| Unadjusted Analyses | |||||||||
| Discharge Home | 0.97 | 0.92-1.01 | 0.16 | 0.95 | 0.90-0.99 | 0.02 | 0.99 | 0.95-1.02 | 0.49 |
| Death in 30 day from admission | 1.04 | 0.99-1.09 | 0.16 | 1.02 | 0.97-1.08 | 0.42 | 1.00 | 0.96-1.05 | 0.96 |
| Death in 1 year from discharge | 1.03 | 0.99-1.07 | 0.11 | 1.05 | 1.01-1.09 | 0.01 | 1.05 | 1.01-1.08 | 0.005 |
| Adjusted Analyses | |||||||||
| Discharge Home | 0.97 | 0.93-1.02 | 0.27 | 0.96 | 0.91-1.01 | 0.09 | 1.02 | 0.98-1.06 | 0.30 |
| Death in 30 day from admission | 1.03 | 0.98-1.08 | 0.29 | 1.00 | 0.95-1.05 | 0.97 | 0.95 | 0.91-0.99 | 0.01 |
| Death in 1 year from discharge | 1.02 | 0.98-1.06 | 0.29 | 1.02 | 0.98-1.06 | 0.38 | 0.98 | 0.95-1.02 | 0.30 |
Supplemental Tables II and III show the adjusted and unadjusted rehospitalization outcome rates at GWTG-Stroke hospitals and non-GWTG-Stroke hospitals, respectively. In the GWTG-Stroke hospitals, adjusted analyses showed no differences in the EARLY vs PRE periods, but reduced rates of rehospitalization in the SUSTAINED vs PRE periods for any 30-day and 1-year rehospitalization and for 1-year stroke rehospitalization. In comparison, at the non-GWTG-Stroke hospitals, no differences for any of the 6 rehospitalization outcomes were noted in either the EARLY or SUSTAINED period compared with the PRE period.
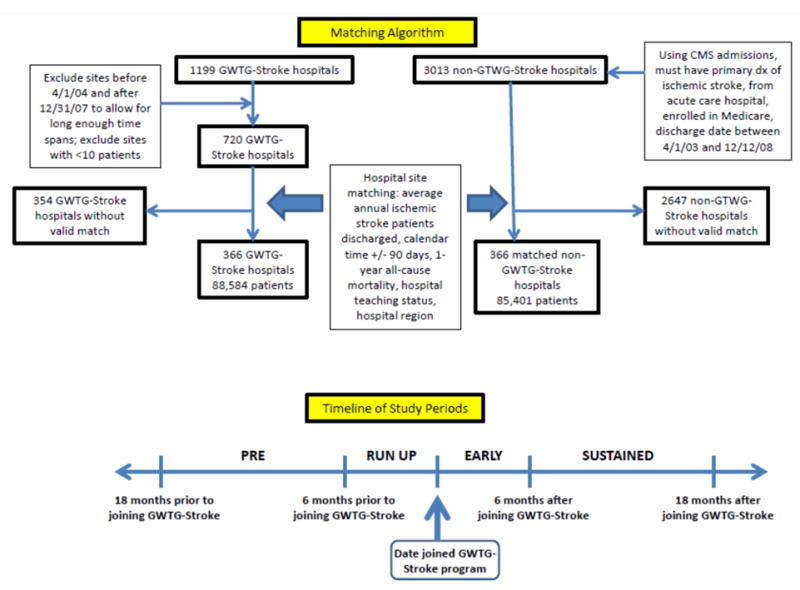
The results of the differences-in-differences analyses are shown Table 4 and Figure 2. The adjusted hazard ratios represent the interaction term between time period and GWTG-hospital status, and as such represent the differential effect of participation in GWTG-stroke on outcomes. HR < 1.0 indicate a greater decline in the outcome at GWTG hospitals compared to non-GWTG sites, whereas HR >1.0 indicate a greater increase in the outcome at GWTG hospitals. In the EARLY versus the PRE period, GWTG-Stroke hospitals showed statistically significant greater improvements than the non-GWTG-Stroke hospitals in all three clinical outcomes: discharge home, 30-day mortality, and 1-year mortality. In the SUSTAINED versus the PRE period, GWTG-Stroke hospitals showed greater improvement than non-GWTG-Stroke hospitals only in 1 year mortality (HR= 0.92, 95% CI 0.88-0.97), although the improvement in discharge home and 30-day mortality was marginally significant.
Table 4.
Adjusted comparison of change (differences in differences) on discharge home/mortality outcomes from RUN-UP, EARLY, or SUSTAINED vs. PRE period between at GWTG-Stroke Hospitals versus at matched non-GWTG-Stroke Hospitals
| Discharge Home/Mortality Outcomes | RUN-UP | EARLY | SUSTAINED | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Hazard Ratio* | 95% CI | P value | Hazard Ratio* | 95% CI | P value | Hazard Ratio* | 95% CI | P value | |
| Discharge Home | 1.07 | 1.00-1.14 | 0.06 | 1.08 | 1.01-1.16 | 0.02 | 1.06 | 1.00-1.12 | 0.06 |
| Death in 30 day from admission | 0.97 | 0.90-1.05 | 0.48 | 0.92 | 0.86-0.99 | 0.04 | 0.96 | 0.90-1.02 | 0.16 |
| Death in 1 year from discharge | 1.00 | 0.94-1.05 | 0.92 | 0.89 | 0.85-0.95 | 0.0001 | 0.92 | 0.88-0.97 | 0.0005 |
These hazard and odds ratios represent interaction term between time period and GWTG-hospital indicator in the difference-in-difference analysis. Note that we used hazard ratios for 30 days and 1 year death outcomes and odds ratio for the discharge home outcome.
Figure 2.
Ratio of changes in outcomes, from PRE time period to RUN-UP, WARM-UP, and SUSTAINED time periods, at GWTG-Stroke hospitals versus matched non-GWTG-Stroke hospitals, for outcomes of A) Discharge to home, B) 30 day mortality, and C) 1 year mortality.
In contrast, GWTG-Stroke hospitals did not show improvements over and above the changes seen at the matched non-GWTG-Stroke hospitals in the 6 readmission outcomes (Supplemental Table IV).
For the 3 outcomes affected by GWTG-Stroke program participation, risk rates for the typical, or “most common baseline” patient were calculated in each of the time epochs for GWTG-Stroke and matched non-GWTG-Stroke hospitals. As shown in Supplemental Table V at GWTG-Stroke hospitals rates of discharge to home steadily increased by a cumulative absolute 1.0%, 30 day mortality steadily declined by a cumulative absolute 2.1%, and 1 year mortality steadily declined by a cumulative 4.5%. In contrast, lesser and fluctuating changes were seen at non-GWTG-Stroke hospitals.
Discussion
This study found that implementation of the GWTG-Stroke quality improvement program was associated with greater improvement for the outcomes of discharge to home and mortality at 30 days and 1 year when compared to similar hospitals that did not join GWTG-Stroke during the same time periods. Significant differences in change over 30 day and 1 year rehospitalization rates were not observed between participating and non-participating hospitals. Limited improvements in outcomes did occur over time at the non-GWTG-Stroke hospitals, but, for GWTG-Stroke hospitals, improvements were accelerated above these secular time changes.
Previous studies of GWTG-Stroke have shown program implementation is associated with improvements in hospital acute and discharge process of care performance measures, such as appropriate in-hospital use of deep venous thrombosis prophylaxis and antithrombotic medication prescribed on discharge for ischemic stroke admissions.8, 15 Additionally, progress on these performance metrics showed continued improvement over time. Similarly, in our study, hospitals who participated in GWTG-Stroke showed a time gradient in accelerated improvement in discharge home and mortality outcome metrics. Some accelerated improvement began to appear in the 6 months before program implementation (RUN UP), when hospitals likely have declared their intention to join GWTG-Stroke and have started implementing anticipatory changes in care processes. Given that upon entry of baseline data, a hospital is eligible for Achievement Awards (which are contingent upon compliance with at least 85% in each of the 8 GWTG-Stroke Achievement measures for all eligible patients), it is reasonable to infer that care processes will have been examined and refined prior to GWTG-Stroke program initiation. Further improvement occurred in the first 6 months after GWTG-Stroke program start, when the new care processes were being officially implemented and feedback on performance using program tools was first being deployed. The greatest improvement occurred in the EARLY period, directly after joining the program to 6 months after program implementation, and continued improvements in some outcomes were seen in the SUSTAINED period, a time period when care process refinements in response to initial experience and data feedback would be implemented and the program entrenched.
The magnitude of accelerated improvement in discharge home and mortality outcomes at hospitals adopting the GWTG-Stroke program was clinically relevant. Discharge home suggests that patients were able to be in a private home setting as opposed to a rehabilitation or nursing setting, and infers improved functional status. Notably, there was greater improvement in in change for 1 year mortality for GWTG-Stroke hospitals than for non-GWTG-Stroke hospitals when comparing the SUSTAINED period with the PRE. In addition, in the SUSTAINED period after implementation, there was a 10% greater relative increase in the rate of discharge to home and 7-8% greater relative decrease in early (30 day) and late (1 year) mortality at GWTG-Stroke hospitals than at matched non-GWTG-Stroke hospitals. Considering the most typical ischemic stroke patient, at hospitals adopting the GWTG-Stroke Program, for every 1000 such patients admitted in the SUSTAINED versus the PRE period, there would be 12 more patients discharged directly to home and 34 fewer deaths at 1 year, compared to the improved outcomes seen at matched non-GWTG-Stroke hospitals which are likely reflective of the underlying secular changes in outcomes that occurred during the 2003-2008 period.
The accelerated improvement in clinical outcomes at the Get With the Guidelines – Stroke Centers are likely related to several aspects of the GWTG-Stroke quality improvement program, including reperfusion therapy, systematic supportive care, and early implementation of secondary prevention. Intravenous tissue plasminogen activator, the one proven beneficial drug intervention in acute stroke, is delivered more often at hospitals participating in the GWTG-Stroke program.6, 7 Systematic supportive stroke care has been shown in controlled trials to improve patient outcomes.16 This suite of care includes many of the process interventions included in the GWTG-Stroke program, including prevention of early complications through delivery of deep venous thrombosis prophylaxis, deterrence of early infarct recurrence by start of antithrombotic therapy, and avoidance of aspiration pneumonia by dysphagia screening. In addition, early implementation of secondary prevention therapy has been demonstrated to improve long-term stroke outcomes.17 The GWTG-Stroke program includes several process measures related to secondary prevention, including start of antithrombotic therapy and of statin therapy by the time of discharge.
GWTG-Stroke implementation was associated with accelerated improvements in discharge home and mortality outcomes in ischemic stroke patients. However, there was no impact on rates of readmission, whether for vascular disease or for all causes. These findings are consistent with the growing evidence that the major causes of variation in readmission rates are factors that a hospital cannot easily remedy during the acute admission, such as poor social supports, socioeconomic status, differential access to rehabilitation facilities, and inadequate community resources.18 These factors are especially important to ischemic stroke patients who may be disabled and unable to care for themselves after their hospital stay.19
A strength of this study is the simultaneous use of two methods to reduce confounding. First, hospitals were matched for facility-level characteristics. Second, performance of the hospitals in the post-intervention time period was compared with their own performance in the pre-intervention time period. This difference in differences analysis, comparing hospital groups with their own pre-intervention performance, further mitigates the impact of any residual confounder present after the hospital matching process.10, 11
A number of potential limitations should be considered when interpreting the results of this study. Our matching algorithms used multiple patient-level and hospital-level factors data available in the CMS administrative dataset. Greatest importance during matching was given to the variable of annual ischemic stroke volume, as caseload was hypothesized to be the hospital characteristic most strongly influencing hospital responsiveness to a hospital-wide, systems intervention. At the patient level, these factors included multiple demographic and medical history variables. However, stroke severity measures, such as the National Institutes of Health Stroke Scale (NIHSS), are not currently captured in the CMS data set, and thus were not used in the matching process. Residual measured and unmeasured confounding variables may have influenced some or all of the findings. The only postdischarge clinical outcomes assessed were mortality and rehospitalizations. Degree of residual disability among stroke survivors is an important additional postdischarge outcome, but the modified Rankin scale or other measures of disability are not captured in the CMS administrative data set. Adherence to guideline care after discharge could not be assessed. We analyzed data from patients aged 65 and older, who account for 80% of strokes; our findings are not directly applicable to younger patients. In addition, hospitals not participating in the GWTG-Stroke program may have other certification, such as primary stroke certification through the Joint Commission. This could mean that Achievement Measures documented through GWTG-Stroke data management tools are also being met by non-GWTG-Stroke hospitals who are stroke-certified, as performance measurements are similar, making the difference between GWTG-Stroke and non-GWTG-Stroke hospitals potentially less relevant.
Conclusions
In this study, we found that patients hospitalized with acute ischemic stroke at GWTG-Stroke hospitals had greater improvement of clinical outcomes over time, than at similar hospitals that did not participate in the GWTG-Stroke program. Compared with secular changes at control hospitals, GWTG-Stroke hospitals exhibited accelerated increases in the proportion of patients discharged to home and accelerated reductions in 30 day and 1 year mortality. These findings indicate that hospital adoption of the GWTG-Stroke program is associated not only with improvement in processes of care, but also in improved functional outcome at discharge and reduced post-discharge mortality.
Supplementary Material
Acknowledgments
Sources of Funding
Get With The Guidelines-Stroke (GWTG-Stroke) program is provided by the American Heart Association/American Stroke Association (AHA/ASA). The GWTG-Stroke program is currently supported, in part, by a charitable contribution from Janssen Pharmaceutical Companies of Johnson & Johnson. GWTG-Stroke has been funded in the past through support from Boeringher-Ingelheim, Merck, Bristol-Myers Squib/Sanofi Pharmaceutical Partnership, and the AHA Pharmaceutical Roundtable (PRT). Research reported in this publication was supported by the University of California, Los Angeles (UCLA) and Charles Drew University (CDU), Resource Centers for Minority Aging Research Center for Health Improvement of Minority Elderly (RCMAR/CHIME) under NIH/National Institute on Aging Grant P30-AG021684, by the UCLA Clinical and Translational Science Institute (CTSI) under NIH/National Center for Advancing Translational Sciences Grant Number UL1TR000124, by the National Institute of Neurological Disorders and Stroke of the National Institutes of Health under Award Number U54NS081764, and by an award to UCLA from the AHA PRT and David and Stevie Spina. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Disclosures
Drs. Song, Liang, Schulte, Reeves have no disclosures.
Dr Fonarow reports research support from PCORI (significant).
Dr. Schwamm serves as chair of the stroke clinical workgroup of GWTG-Stroke and is a stroke systems consultant to the Massachusetts Department of Public Health for the Paul Coverdell National Acute Stroke Registry, and reports research support from PCORI, NINDS and Genentech.
Dr. Smith is a member of the GWTG Steering Committee (unpaid).
Dr. Saver is an employee of the University of California. The University of California, Regents receive funding for Dr. Saver’s services as a scientific consultant regarding trial design and conduct to Medtronic/Covidien, Stryker, BrainsGate, Pfizer, Squibb, Boehringer Ingelheim (prevention only), ZZ Biotech, and St. Jude Medical. Dr. Saver has served as an unpaid site investigator in multicenter trials run by Lundbeck for which the UC Regents received payments on the basis of clinical trial contracts for the number of subjects enrolled. Dr. Saver serves as an unpaid consultant to Genentech advising on the design and conduct of the PRISMS trial; neither the University of California nor Dr. Saver received any payments for this voluntary service. The University of California has patent rights in retrieval devices for stroke.
Dr. Hernandez reports research support from Amgen, AstraZeneca, Bristol Myers Squibb, Merck, Novartis, and has the following disclosures: Amgen, AstraZeneca, Merck, Janssen, Novartis.
Dr. Peterson is the co-PI of the GWTG Data Analytic Center at DCRI.
References
- 1.Batalden PB, D F. What is “quality improvement” and how can it transform healthcare? Quality & Safety in Health Care. 2007;16:2–3. doi: 10.1136/qshc.2006.022046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Spertus JA, Eagle KA, Krumholz HM, Mitchell KR, Normand SL. American College of Cardiology and American Heart Association methodology for the selection and creation of performance measures for quantifying the quality of cardiovascular care. Circulation. 2005;111:1703–1712. doi: 10.1161/01.CIR.0000157096.95223.D7. [DOI] [PubMed] [Google Scholar]
- 3.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, et al. Heart disease and stroke statistics--2014 update: a report from the American Heart Association. Circulation. 2014;129:e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murphy S, Xu J, Kochanek KD. Deaths: Final Data for 2010. National Vital Statistics Reports. 2013;61:55. [PubMed] [Google Scholar]
- 5.Hong Y, LaBresh KA. Overview of the American Heart Association "Get with the Guidelines" programs: coronary heart disease, stroke, and heart failure. Crit Pathw Cardiol. 2006;5:179–186. doi: 10.1097/01.hpc.0000243588.00012.79. [DOI] [PubMed] [Google Scholar]
- 6.Schwamm LH, Fonarow GC, Reeves MJ, Pan W, Frankel MR, Smith EE, et al. Get With the Guidelines-Stroke is associated with sustained improvement in care for patients hospitalized with acute stroke or transient ischemic attack. Circulation. 2009;119:107–115. doi: 10.1161/CIRCULATIONAHA.108.783688. [DOI] [PubMed] [Google Scholar]
- 7.Reeves MJ, Grau-Sepulveda MV, Fonarow GC, Olson DM, Smith EE, Schwamm LH. Are quality improvements in the get with the guidelines: stroke program related to better care or better data documentation? Circ Cardiovasc Qual Outcomes. 2011;4:503–511. doi: 10.1161/CIRCOUTCOMES.111.961755. [DOI] [PubMed] [Google Scholar]
- 8.Fonarow GC, Smith EE, Reeves MJ, Pan W, Olson D, Hernandez AF, et al. Hospital-level variation in mortality and rehospitalization for medicare beneficiaries with acute ischemic stroke. Stroke. 2011;42:159–166. doi: 10.1161/STROKEAHA.110.601831. [DOI] [PubMed] [Google Scholar]
- 9.Joynt KE, Blumenthal DM, Orav EJ, Resnic FS, Jha AK. Association of public reporting for percutaneous coronary intervention with utilization and outcomes among Medicare beneficiaries with acute myocardial infarction. JAMA. 2012;308:1460–1468. doi: 10.1001/jama.2012.12922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lasser KE, Hanchate AD, McCormick D, Manze MG, Chu C, Kressin NR. The effect of Massachusetts health reform on 30 day hospital readmissions: retrospective analysis of hospital episode statistics. BMJ. 2015;348:g2329. doi: 10.1136/bmj.g2329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Friedberg MW, Schneider EC, Rosenthal MB, Volpp KG, Werner RM. Association between participation in a multipayer medical home intervention and changes in quality, utilization, and costs of care. JAMA. 2014;311:815–825. doi: 10.1001/jama.2014.353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dimick JB, Ryan AM. Methods for evaluating changes in health care policy: the difference-in-differences approach. JAMA. 2014;312:2401–2402. doi: 10.1001/jama.2014.16153. [DOI] [PubMed] [Google Scholar]
- 13.Reeves MJ, Smith E, Fonarow G, Hernandez A, Pan W, Schwamm LH. Off-hour admission and in-hospital stroke case fatality in the get with the guidelines-stroke program. Stroke. 2009;40:569–576. doi: 10.1161/STROKEAHA.108.519355. [DOI] [PubMed] [Google Scholar]
- 14.Reeves MJ, Fonarow GC, Smith EE, Pan W, Olson D, Hernandez AF, et al. Representativeness of the Get With The Guidelines-Stroke Registry: comparison of patient and hospital characteristics among Medicare beneficiaries hospitalized with ischemic stroke. Stroke. 2012;43:44–49. doi: 10.1161/STROKEAHA.111.626978. [DOI] [PubMed] [Google Scholar]
- 15.Fonarow GC, Reeves MJ, Smith EE, Saver JL, Zhao X, Olson DW, et al. Characteristics, performance measures, and in-hospital outcomes of the first one million stroke and transient ischemic attack admissions in get with the guidelines-stroke. Circ Cardiovasc Qual Outcomes. 2010;3:291–302. doi: 10.1161/CIRCOUTCOMES.109.921858. [DOI] [PubMed] [Google Scholar]
- 16.Lees KR, Bluhmki E, von Kummer R, Brott TG, Toni D, Grotta JC, et al. Time to treatment with intravenous alteplase and outcome in stroke: an updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials. Lancet. 2010;375:1695–1703. doi: 10.1016/S0140-6736(10)60491-6. [DOI] [PubMed] [Google Scholar]
- 17.Luengo-Fernandez R, Gray AM, Rothwell PM. Effect of urgent treatment for transient ischaemic attack and minor stroke on disability and hospital costs (EXPRESS study): a prospective population-based sequential comparison. Lancet Neurol. 2009;8:235–243. doi: 10.1016/S1474-4422(09)70019-5. [DOI] [PubMed] [Google Scholar]
- 18.Gorodeski EZ, Starling RC, Blackstone EH. Are all readmissions bad readmissions? N Engl J Med. 2010;363:297–298. doi: 10.1056/NEJMc1001882. [DOI] [PubMed] [Google Scholar]
- 19.Fonarow GCAM, Broderick JP, Jauch EC, Kleindorfer DO, Saver JL, Solis P, et al. TABLE 2Stroke outcomes measures must be appropriately risk adjusted to ensure quality of care of patients: a presidential advisory from the American Heart Association/American Stroke Association. 2014;45:1589–1601. doi: 10.1161/STR.0000000000000014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.