Abstract
Purpose
To determine the association of vision-related quality of life to demographic factors and visual function in glaucoma suspect or early glaucoma patients..
Methods
We administered the 25-item National Eye Institute Visual Function Questionnaire (VFQ-25) on the same day as a comprehensive ocular examination to participants either with glaucoma or at high risk for developing glaucoma. Regression models were used to determine the association between VFQ-25 composite and subscale scores, VF status, logMAR equivalent VA, age and gender. In all analyses we used data from the eye with the best Mean Deviation (MD), best Pattern Standard Deviation (PSD) and best VA.
Results
Data from 198 participants were analyzed. The mean best MD (± standard deviation) was 0.02 ±1.52dB (range; −5.11 to 2.63) and the mean best PSD was 1.75 ±1.03dB (range; 0.91 to 8.36). The mean VFQ-25 composite score was 91.6 ±6.7 (range; 54.5 to 100.0). Composite score, and the distance activities and color vision subscale scores were associated with best MD (p≤0.05). The general vision and driving subscale scores were associated with best VA (p≤0.03). The composite score and the distance activities, driving and color vision subscale scores were associated with age (p≤0.05). Finally, the distance activities, driving and peripheral vision subscale scores were associated with gender (p≤0.04).
Conclusions
Vision-related quality of life is associated with visual field status even in early and suspected glaucoma. It is also associated with VA, age and gender. Particular decreases in quality of life are related to distance activities, driving and color vision.
Keywords: Quality of Life, Visual Field, Visual Acuity
Introduction
Glaucoma is the second leading cause of blindness worldwide. 1 Consequently, the goal of glaucoma management is to preserve visual function and maintain patients’ vision-related quality of life (QoL). The 25-Item National Eye Institute Visual Function Questionnaire (VFQ-25) represents a validated, self-reported vision-targeted survey that measures the influence of visual disability and visual symptoms on several health domains such as emotional health and social functioning. 2, 3 It includes 25 questions representing 11 vision-related constructs, plus an additional single-item general health question. 4 Survey results can also be used to generate a composite score that represents overall vision-related QoL.
Previous reports 5–9 have examined the association between visual fields (VF) with MD worse then −2dB and QoL, but few used the VFQ-25. 10–13 Of these studies, one has reported an association between the driving subscale of the VFQ-25 and moderate VF loss, 10 such that VF loss was associated with poor performance on driving skills that require a wide field of vision. Another study 11 showed that severe glaucomatous VF damage (best eye MD worse than −25 dB) is independently associated with a loss in both disease-specific and generic QoL. McKean-Cowdin and colleagues 12 found a significant association between VFQ-25 results and VF MD in a subset of individuals with mild to moderate VF damage (−6dB < MD < −2dB). However, that study 12 did not analyze the association between VFQ-25 results and VF Pattern Standard Deviation (PSD). Another study in Japanese individuals 13 demonstrated an association between a lower quality of vision (QOV) with MD values between −2dB and −12dB in the better eye and between −7dB and −16dB in the worse eye. Loss of visual function in both eyes was correlated with poorer general vision, near vision, distant vision, mental health, driving and composite score and with greater role limitations and dependency. VF status was the only variable that was significantly correlated with social function, color vision, and peripheral vision.
Previous studies have not addressed the association between VF status and QoL in individuals with early VF loss (Mean Deviation [MD] better than −2 dB). The current study uses data from a large cohort followed longitudinally as part of the ongoing Portland Progression Project (P3) 14 and tests the hypothesis that VF status, as quantified by MD or PSD, is significantly associated with vision-related QoL. We also aim to determine which VF parameter (MD or PSD) is more closely associated with vision-related QoL. In addition, we examined the effect of mood, best visual acuity (VA), age, and gender as predictors of vision-related QoL. This may enable clinicians to better understand their patients’ QoL based on standard clinical measurements.
Materials and Methods
Participants
The study design applied in this investigation was aligned with the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board at Legacy Health in Portland, OR, USA. All participants provided written informed consent after the risks and benefits of their involvement were explained to them.
This cross-sectional analysis includes data from all participants in P3 who had taken the VFQ-25 survey. Inclusion criteria for P3 were a clinical diagnosis of glaucoma or having high-risk ocular hypertension. Participants with glaucoma had a clinical diagnosis of Primary Open Angle Glaucoma (POAG) in at least one eye based on an abnormal VF (Glaucoma Hemifield Test ‘outside normal limits’, PSD worse than the normal 5% level, or a cluster of abnormal locations on the Pattern Deviation probability plot) but MD no worse than −10dB. Individuals with ocular hypertension (untreated IOP ≥ 22 mmHg on at least two occasions) had at least one of the following: optic nerve head appearance suspicious for glaucoma, cupping asymmetry ≥ 0.2 between eyes, disc hemorrhage, rim notching, nerve fiber layer thinning or defect, immediate family history of POAG, age ≥ 70, or evidence of vascular dysregulation (≥ 2 of the following: migraine, vascular hypertension, heart disease, Reynaud’s syndrome).
Visual acuity was measured using a Snellen chart and then converted to logMAR equivalent. In analyses that involved VA, the result from the eye with the best logMAR equivalent VA (most negative or least positive) was used.
Survey Instrument
Trained technicians administered the VFQ-25 survey on the same day that they assessed VA and VF. The VFQ-25 composite and subscale scores (General Health, General Vision, Ocular Pain, Near Activities, Distant Activities, Social Functioning, Role Difficulties, Mental Health, Dependency, Driving, Color Vision and Peripheral Vision) were calculated according to published methods. 2 Questions pertaining to driving were left blank for those individuals that were not current drivers and do not contribute to calculation of the composite score.
We added a previously validated item regarding self-reported depression15 to the VFQ-25 instrument as question 1a. This depression item posed the question “How often have you felt downhearted and blue in the last 4 weeks” to which the six allowed responses were: 1) All of the time, 2) Most of the time, 3) A good bit of the time, 4) Some of the time, 5) A little of the time or 6) None of the time. A participant was considered depressed if their response was 1, 2 or 3 (feeling downhearted and blue all, most or a good bit of the time).15
Visual Field Testing
All VF testing was performed with a Humphrey Field Analyzer II (Carl Zeiss Meditec Inc., Dublin, CA, USA) using the Swedish Interactive Thresholding Algorithm (SITA) 16 and the 24-2 test pattern. Default testing parameters and appropriate refractive corrections were always used. All participants had prior experience with this form of VF testing. We defined an unreliable VF as having fixation losses or false negatives errors > 33%, or false positive errors > 15% and unreliable VF tests were excluded from all analyses. In analyses that involved MD, results from the eye (right or left) with the best MD (most positive or least negative) were used whereas in analyses that involved PSD, results from the eye with the best PSD (least positive) were used. The eye with the best VF index was used because the best-seeing eye is more likely to be associated with vision-related QoL. 12 In addition, it has been shown that the binocular sensitivity at each VF location can be predicted from the highest sensitivity between eyes at the corresponding locations, and thus is more likely to be related to the eye with the better VF. 17, 18
In this study, exclusion criteria were VA worse than 20/40 in the best eye, co-existing eye disease that could affect VF or VA, secondary glaucomas or the use of medications known to affect the VF.
Statistical analysis
All statistical analyses were performed using the R language and environment for statistical computing. 19 Ordinary linear regression analyses were performed to determine whether the VFQ-25 composite score was significantly associated with VF status (best MD or best PSD), VA, age or gender. The distribution of VFQ-25 composite scores within the cohort was heavily skewed to the right, so we used a logarithmic transformation of composite score [log(101 – composite score)] that approached a Gaussian distribution. We used univariate ordinal logistic regression to determine associations between subscale scores and VF status, VA, age and gender because the subscale scores had a limited number of ordered outcomes and could not be treated as continuous variables. We dichotomized question 1a (score of 6 -‘never feeling sad or blue’ vs. other) for the analysis of composite score in the analysis. Ordinal logistic regression was performed using cumulative link models (function clm) as implemented within the R package ordinal. 20
Results
We include data from 198 participants with 61% (121/198) female and 184 (93%) non-Hispanic White. The mean age ± standard deviation of the participants at the time of testing was 64.8 ± 11.5 years (range: 33.7 to 90.4 years). The mean best MD and mean best PSD were 0.02 ± 1.52dB (range: −5.11 to 2.63) and 1.75 ± 1.03dB (range; 0.91 to 8.36), respectively. The mean VFQ-25 composite score was 91.6 ± 6.7 (range; 54.5 to 100.0, median; 93.0). The mean best logMAR equivalent VA was 0.02 ± 0.08 (range −0.1 to 0.30; median 0.0 or 20/20). The means, empirical 95% confidence intervals (CI) and median values of the VFQ-25 composite score and all subscale scores are show in Table 1.
Table 1.
The mean, 95% confidence interval (CI) and median of the vision-related quality of life composite and subscale scores measured using the 25-item National Eye Institute Visual Function Questionnaire. Role difficulties is related to difficulties in accomplishment of work because of vision, while dependency describes how much the patient is reliant on others and needs help because of their vision. The driving subscale included data from 189/198 (95.5%) participants who were current drivers at the time the questionnaire was administered.
| Score | Mean | 95% CI | Median |
|---|---|---|---|
| Composite score | 91.6 | 75.0 – 100.0 | 93.0 |
| General Vision | 80.8 | 60.0 – 100.0 | 80.0 |
| Ocular Pain | 89.1 | 50.0 – 100.0 | 87.5 |
| Near Activities | 89.2 | 50.0 – 100.0 | 91.7 |
| Distant Activities | 87.6 | 50.0 – 100.0 | 91.7 |
| Social Function | 98.0 | 75.0 – 100.0 | 100.0 |
| Mental Health | 92.2 | 68.8 – 100.0 | 93.8 |
| Role Difficulties | 94.1 | 61.6 – 100.0 | 100.0 |
| Dependency | 98.7 | 83.3 – 100.0 | 100.0 |
| Driving | 86.2 | 64.2 – 100.0 | 83.3 |
| Color Vision | 97.9 | 75.0 – 100.0 | 100.0 |
| Peripheral Vision | 93.3 | 50.0 – 100.0 | 100.0 |
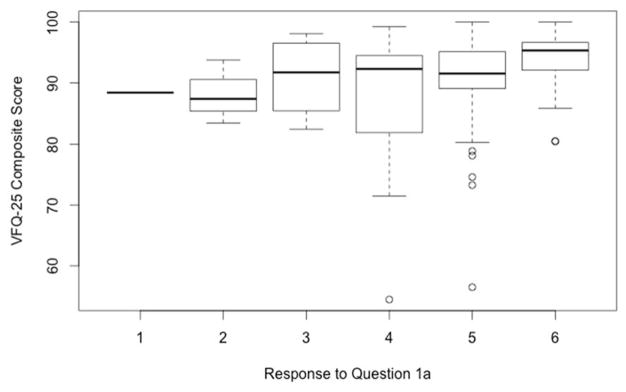
Depression (feeling downhearted and blue all, most or a good bit of the time) was not significantly associated with either the transformed composite score (P = 0.28), best MD (P = 0.08) or best PSD (P = 0.22). However, Figure 1 shows that individuals that reported feeling downhearted or blue “none of the time” (response 6, above) had higher transformed composite scores when compared to individuals reporting any other response to that question (responses 1 to 5; P < 0.001). Consequently, all additional analyses involving the transformed composite score were performed in a manner that accounted for mood as a binary covariate (feeling downhearted or blue none of the time vs. any other response to question 1a).
Figure 1.
VFQ-25 composite score was better (P < 0.001) for those individuals who reported never feeling symptoms of depression (Response = 6 vs. others) in response to question 1a: “How often have you felt downhearted and blue in the last 4 weeks?” Responses included: 1 = All of the time, 2 = Most of the time, 3 = A good bit of the time, 4 = Some of the time, 5 = A little of the time and 6 = None of the time.
Using ordinary linear regression models that accounted for mood we found a significant association between the transformed composite score and best MD (P = 0.04) and age (P = 0.03) such that better best MD and younger age were both associated with better composite scores. For individuals with the best mood (feeling downhearted or blue none of the time) having an MD of 0dB instead of −4dB resulted in the VFQ composite score being 1.7 points better (95.1 vs. 93.4). Similarly, for individuals with the best mood, being 70 years old instead of 80 years old resulted in the VFQ composite score being 0.56 points better (94.9 vs. 94.4). There were no significant associations between the transformed composite score and best PSD (P = 0.95), best VA (P = 0.17) or gender (P = 0.12), as can be seen in Table 2.
Table 2.
Cells contain beta coefficients (with P values in parentheses) from ordinary linear regression (transformed composite score) or odds ratios from ordinal logistic regression (subscales). For the visual field and visual acuity (VA) variables, the results represent the effect of the predictor variable moving toward better vision; best Mean Deviation (MD) being 1dB higher, best Pattern Standard Deviation (PSD) being 1dB lower and best logMAR VA being 0.1 (1 line) better. For age and sex, the effect is associated with being one decade younger and being male respectively. For the subscales, the risk ratios denote the probability of being in the next higher ordered level for the changes in the predictors just given. Analyses that were significant at the P≤0.05 level are shown in bold type.
| Best MD (P value) | Best PSD (P value) | Best VA (P value) | Age (P value) | Sex (P value) | |
|---|---|---|---|---|---|
| Transformed Composite | −0.063 (0.04) | −0.003 (0.95) | −0.081 (0.15) | −0.089 (0.03) | −0.066 (0.52) |
| General Vision | 1.19 (0.08) | 1.03 (0.86) | 1.50 (0.03) | 1.19 (0.18) | 0.68 (0.21) |
| Ocular Pain | 0.96 (0.72) | 1.07 (0.63) | 0.98 (0.87) | 0.94 (0.61) | 1.43 (0.20) |
| Near Activities | 1.09 (0.31) | 0.96 (0.78) | 1.03 (0.85) | 0.91 (0.41) | 0.86 (0.56) |
| Distant Activities | 1.28 (<0.01) | 1.11 (0.35) | 1.31 (0.09) | 1.31 (0.02) | 3.00 (<0.01) |
| Social Function | 1.09 (0.57) | 0.74 (0.41) | 1.22 (0.44) | 1.17 (0.44) | 0.83 (0.69) |
| Mental Health | 1.04 (0.65) | 0.90 (0.46) | 0.86 (0.33) | 0.81 (0.07) | 1.55 (0.10) |
| Role Difficulties | 1.04 (0.70) | 0.95 (0.73) | 0.86 (0.42) | 0.97 (0.79) | 0.87 (0.67) |
| Dependency | 1.29 (0.06) | 1.25 (0.16) | 0.73 (0.28) | 0.72 (0.11) | 1.57 (0.38) |
| Driving | 1.07 (0.41) | 0.84 (0.17) | 1.50 (0.02) | 1.31 (0.02) | 1.90 (0.02) |
| Color Vision | 1.60 (<0.01) | 1.42 (0.03) | 0.90 (0.76) | 1.67 (0.05) | 0.44 (0.14) |
| Peripheral Vision | 1.11 (0.32) | 1.06 (0.70) | 1.32 (0.17) | 1.07 (0.64) | 2.18 (0.04) |
Several of the subscales (Ocular Pain, Near Activities, Social Functioning, Mental Health, Role Difficulties and Dependency) were not significantly associated with any of the predictors used in this study (best MD, best PSD, best VA, age or gender) whereas the other subscales were all significantly associated with at least one of the predictors.
The General Vision subscale was significantly associated with best VA (P = 0.03) such that having one line better VA (0.1 decrease in logMAR) was associated with a 50% higher probability of scoring one level better on the General Vision subscale. The Distant Activities subscale was significantly associated with best MD (P < 0.01), age (P = 0.02) and gender (P < 0.01) such that a 1dB higher (better) best MD, being one decade younger and being male were associated with a 28% higher, a 31% higher and a 200% higher probability respectively of scoring one level better on the Distant Activities subscale. For the Driving subscale, which was based on data from 189 participants who were regular drivers at the time of the survey, we found a significant association with best VA (P = 0.02), age (P = 0.02) and gender (P = 0.02) such that having one line better VA, being one decade younger and being male were associated with a 50% higher, a 31% higher and a 90% higher probability respectively of scoring one level better on the Driving subscale. The Color Vision subscale was significantly associated with best MD (P < 0.01), best PSD (P = 0.03) and age (P = 0.05) such that a 1dB higher best MD, a 1dB lower (better) best PSD and being one decade younger were associated with a 60% higher, a 42% higher and a 67% higher probability respectively of scoring one level better on the Color Vision subscale. Finally, the Peripheral Vision subscale was significantly associated with gender (P = 0.04) such that being male was associated with a 118% higher probability of scoring one level better on the Peripheral Vision subscale.
Discussion
Maintaining QoL and preventing visual impairment is the ultimate goal when managing patients with glaucoma. While other studies have demonstrated that QoL is affected when VF damage is severe, 11 to the best of our knowledge the current study is the first to assess the association between QoL and early VF damage in patients with glaucoma or high-risk ocular hypertension. This study suggests that even in early glaucomatous disease, VF status is significantly associated with vision-related QoL, after accounting for mood.
The composite score was lower (worse) when VF status was worse as quantified by best MD (P = 0.04) but not when quantified by best PSD (P = 0.95). MD and PSD were designed to emphasize different aspects of the VF. MD will tend to be affected by generalized or extensive localized reduction of VF sensitivity, which could affect overall QoL. PSD, on the other hand, is often considered to be a more specific indicator of glaucomatous VF damage than MD 21 as it was designed to emphasize localized reductions of sensitivity; a situation that might have less effect on vision-related QoL, unless it occurs in critical locations such as in the macular region. Patients may also be able to compensate for localized VF damage using eye movements, something that cannot be done to compensate for generalized VF damage. Even though PSD may be a better indicator of early glaucomatous VF damage than MD, the VFQ-25 composite score is more strongly associated with the diffuse component of VF damage insofar as MD quantifies this. Cataract, which is another major cause of diffuse visual loss, has been shown to have a significant negative association with the QoL quantified using the VFQ-25.6, 22
Difficulty with driving is an important component of the VFQ-25. The vast majority of participants in our study (189/198 = 95.5%) were regular drivers at the time the VFQ-25 was administered. The VFQ-25 contains three questions related to driving, namely; difficulty with daytime driving in familiar places, difficulty with nighttime driving, and difficulty driving in suboptimal conditions (bad weather, rush hour, freeway or city traffic). Best VA, age and gender were all significantly associated with perceived driving difficulties. In a recent study that utilized data from 28 participants, mild to moderate peripheral VF constriction was adversely associated with specific driving skills for which a wide field of vision would be beneficial. 10 However, that study did not assess the association between MD and driving difficulties. Our results show that self-perceived driving difficulties could be compromised in individuals with early glaucoma, however it was more strongly associated with best VA, age and gender than with either best MD or best PSD.
Previous studies have found a significant association between vision-related QoL and depression. 23–27 People who feel depressed report a higher number of past physical symptoms 28 and depression is an important covariate to consider when assessing self-reported QoL. 15 In this study, we did not find a significant association between being depressed (feeling downhearted or blue all, most or a good bit of the time vs. some, a little or none of the time) and QoL or best MD. However, only a small number of individuals in this cohort (8/198 ≈ 4%) met the definition for being depressed. In contrast, there was a significant association between the transformed composite score and having the best mood, i.e. feeling downhearted or blue none of the time. This finding suggests that there is definitely an impact of mood on vision-related QoL and the lack of a significant association between depression and QoL found in this study may be due to the small number of depressed individuals in our cohort.
In this study, we sought an association between vision-related QoL and the best-seeing eye quantified by MD, PSD and VA. Quality of life will most likely depend on both eyes, although the status of the best-seeing eye may have a larger influence, 12 and patients are more likely to depend on their better eyes to accomplish their activities of daily living.
One feature of this study is that participants had early or suspected glaucoma. While this enables us to determine whether a significant association exists between QoL and VF at this early stage of the disease, it also reduces the power of the study to detect associations since the range of variables was relatively narrow. In particular, reports in the literature suggest that VA and QoL are consistently and strongly related. 29, 30 We did not find a significant association between best VA and transformed composite score, although there were significant associations between best VA and the General Vision and Driving subscales. Our exclusion criteria ensured that study participants had relatively good VA (20/40 or better), which would have narrowed the range of VA within the cohort and blunted our ability to identify an association between VA and composite score.
Another limitation of this study was that 93% of the participants were Non-Hispanic White. While the results may be different for other ethnicities, many of these differences may be accounted for using sociodemographic and socioeconomic variables. 31
In conclusion, this study suggests that self-reported vision-related quality of life is significantly related to the visual field global index MD in individuals with early or suspected glaucoma. Furthermore, best MD is more predictive of vision-related quality of life than best PSD in this cohort. This emphasizes the importance of early detection and treatment of glaucoma to limit its deleterious effect on vision-related quality of life.
Acknowledgments
Financial Support:
This project was funded in part by NIH EY019674 (SD) and The Good Samaritan Foundation.
The authors would like to thank Cindy Blachly and Michael Whitworth for assisting with recruiting participants, data collection and data aggregation.
Footnotes
No authors have any financial/conflicting interests to disclose.
References
- 1.Kingman S. Glaucoma is second leading cause of blindness globally. Bull World Health Organ. 2004;82:887–888. [PMC free article] [PubMed] [Google Scholar]
- 2.Mangione CM, Lee PP, Gutierrez PR, Spritzer K, Berry S, Hays RD. Development of the 25-item National Eye Institute Visual Function Questionnaire. Arch Ophthalmol. 2001;119:1050–1058. doi: 10.1001/archopht.119.7.1050. [DOI] [PubMed] [Google Scholar]
- 3.Kowalski JW, Rentz AM, Walt JG, et al. Rasch analysis in the development of a simplified version of the National Eye Institute Visual-Function Questionnaire-25 for utility estimation. Qual Life Res. 2012;21:323–334. doi: 10.1007/s11136-011-9938-z. [DOI] [PubMed] [Google Scholar]
- 4.Mangione CM. The National Eye Institute 25-Item Visual Function Questionnaire (VFQ-25): NEI VFQ-25 Scoring Algorithm. 2000. [Google Scholar]
- 5.Bechetoille A, Arnould B, Bron A, et al. Measurement of health-related quality of life with glaucoma: validation of the Glau-QoL 36-item questionnaire. Acta Ophthalmol. 2008;86:71–80. doi: 10.1111/j.1600-0420.2007.00999.x. [DOI] [PubMed] [Google Scholar]
- 6.Wu SY, Hennis A, Nemesure B, Leske MC. Impact of glaucoma, lens opacities, and cataract surgery on visual functioning and related quality of life: the Barbados Eye Studies. Invest Ophthalmol Vis Sci. 2008;49:1333–1338. doi: 10.1167/iovs.07-1252. [DOI] [PubMed] [Google Scholar]
- 7.Evans K, Law SK, Walt J, Buchholz P, Hansen J. The quality of life impact of peripheral versus central vision loss with a focus on glaucoma versus age-related macular degeneration. Clin Ophthalmol. 2009;3:433–445. doi: 10.2147/opth.s6024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wren PA, Musch DC, Janz NK, Niziol LM, Guire KE, Gillespie BW. Contrasting the use of 2 vision-specific quality of life questionnaires in subjects with open-angle glaucoma. J Glaucoma. 2009;18:403–411. doi: 10.1097/IJG.0b013e3181879e63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Richman J, Lorenzana LL, Lankaranian D, et al. Relationships in glaucoma patients between standard vision tests, quality of life, and ability to perform daily activities. Ophthalmic Epidemiol. 2010;17:144–151. doi: 10.3109/09286581003734878. [DOI] [PubMed] [Google Scholar]
- 10.Bowers A, Peli E, Elgin J, McGwin G, Jr, Owsley C. On-road driving with moderate visual field loss. Optometry and Vision Science. 2005;82:657–667. doi: 10.1097/01.opx.0000175558.33268.b5. [DOI] [PubMed] [Google Scholar]
- 11.van Gestel A, Webers CA, Beckers HJ, et al. The relationship between visual field loss in glaucoma and health-related quality-of-life. Eye (Lond) 2010;24:1759–1769. doi: 10.1038/eye.2010.133. [DOI] [PubMed] [Google Scholar]
- 12.McKean-Cowdin R, Varma R, Wu J, Hays RD, Azen SP. Severity of visual field loss and health-related quality of life. Am J Ophthalmol. 2007;143:1013–1023. doi: 10.1016/j.ajo.2007.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sawada H, Fukuchi T, Abe H. Evaluation of the relationship between quality of vision and visual function in Japanese glaucoma patients. Clin Ophthalmol. 2011;5:259–267. doi: 10.2147/OPTH.S16989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ren R, Yang H, Gardiner SK, et al. Anterior lamina cribrosa surface depth, age, and visual field sensitivity in the Portland Progression Project. Invest Ophthalmol Vis Sci. 2014;55:1531–1539. doi: 10.1167/iovs.13-13382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Paz SH, Globe DR, Wu J, Azen SP, Varma R. Relationship between self-reported depression and self-reported visual function in Latinos. Arch Ophthalmol. 2003;121:1021–1027. doi: 10.1001/archopht.121.7.1021. [DOI] [PubMed] [Google Scholar]
- 16.Bengtsson B, Olsson J, Heijl A, Rootzen H. A new generation of algorithms for computerized threshold perimetry, SITA. Acta Ophthalmol Scand. 1997;75:368–375. doi: 10.1111/j.1600-0420.1997.tb00392.x. [DOI] [PubMed] [Google Scholar]
- 17.Jampel HD, Friedman DS, Quigley H, Miller R. Correlation of the binocular visual field with patient assessment of vision. Invest Ophthalmol Vis Sci. 2002;43:1059–1067. [PubMed] [Google Scholar]
- 18.Nelson-Quigg JM, Cello K, Johnson CA. Predicting binocular visual field sensitivity from monocular visual field results. Invest Ophthalmol Vis Sci. 2000;41:2212–2221. [PubMed] [Google Scholar]
- 19.R Development Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2014. [Accessed 10/31/2014]. V3.1.2. URL http://www.r-project.org/ [Google Scholar]
- 20.Christensen RHB. [Accessed 11/15/2014];ordinal - Regression Models for Ordinal Data. 2014 V2014.11–14. URL http://www.cran.r-project.org/package=ordinal/
- 21.Kothari R, Bokariya P, Singh R, Singh S, Narang P. Correlation of pattern reversal visual evoked potential parameters with the pattern standard deviation in primary open angle glaucoma. Int J Ophthalmol. 2014;7:326–329. doi: 10.3980/j.issn.2222-3959.2014.02.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.To KG, Meuleners LB, Fraser ML, et al. The impact of cataract surgery on vision-related quality of life for bilateral cataract patients in Ho Chi Minh City, Vietnam: a prospective study. Health Qual Life Outcomes. 2014;12:16. doi: 10.1186/1477-7525-12-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carabellese C, Appollonio I, Rozzini R, et al. Sensory impairment and quality of life in a community elderly population. J Am Geriatr Soc. 1993;41:401–407. doi: 10.1111/j.1532-5415.1993.tb06948.x. [DOI] [PubMed] [Google Scholar]
- 24.Mitchell J, Bradley C. Quality of life in age-related macular degeneration: a review of the literature. Health Qual Life Outcomes. 2006;4:97. doi: 10.1186/1477-7525-4-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jampel HD, Frick KD, Janz NK, et al. Depression and mood indicators in newly diagnosed glaucoma patients. Am J Ophthalmol. 2007;144:238–244. doi: 10.1016/j.ajo.2007.04.048. [DOI] [PubMed] [Google Scholar]
- 26.Hayman KJ, Kerse NM, La Grow SJ, Wouldes T, Robertson MC, Campbell AJ. Depression in older people: visual impairment and subjective ratings of health. Optom Vis Sci. 2007;84:1024–1030. doi: 10.1097/OPX.0b013e318157a6b1. [DOI] [PubMed] [Google Scholar]
- 27.Ishii K, Kabata T, Oshika T. The impact of cataract surgery on cognitive impairment and depressive mental status in elderly patients. Am J Ophthalmol. 2008;146:404–409. doi: 10.1016/j.ajo.2008.05.014. [DOI] [PubMed] [Google Scholar]
- 28.Howren MB, Suls J. The symptom perception hypothesis revised: depression and anxiety play different roles in concurrent and retrospective physical symptom reporting. J Pers Soc Psychol. 2011;100:182–195. doi: 10.1037/a0021715. [DOI] [PubMed] [Google Scholar]
- 29.Brown MM, Brown GC, Sharma S, Landy J, Bakal J. Quality of life with visual acuity loss from diabetic retinopathy and age-related macular degeneration. Arch Ophthalmol. 2002;120:481–484. doi: 10.1001/archopht.120.4.481. [DOI] [PubMed] [Google Scholar]
- 30.McKean-Cowdin R, Varma R, Hays RD, Wu J, Choudhury F, Azen SP. Longitudinal changes in visual acuity and health-related quality of life: the Los Angeles Latino Eye study. Ophthalmology. 2010;117:1900–1907. 1907 e1901. doi: 10.1016/j.ophtha.2010.01.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pereira CC, Palta M, Mullahy J, Fryback DG. Race and preference-based health-related quality of life measures in the United States. Qual Life Res. 2011;20:969–978. doi: 10.1007/s11136-010-9813-3. [DOI] [PMC free article] [PubMed] [Google Scholar]