Abstract
Background
Up to 50% of patients fail to meet ST-segment elevation myocardial infarction (STEMI) guideline goals recommending a first-medical-contact (FMC)-to-device time of <90 minutes for patients directly presenting to percutaneous coronary intervention (PCI)-capable hospitals and <120 minutes for transferred patients. We sought to increase the proportion of patients treated within guideline goals by organizing coordinated regional reperfusion plans.
Methods
We established leadership teams, coordinated protocols, and provided regular feedback for 484 hospitals and 1253 emergency medical service (EMS) agencies in 16 regions across the United States.
Results
Between July 2012 and December 2013, 23,809 patients presented with acute STEMI (direct to PCI hospital: 11,765 EMS-transported and 6502 self-transported; transferred: 5542). EMS-transported patients differed from self-transported patients in symptom onset to FMC time (median: 47 versus 114 minutes), incidence of cardiac arrest (10% versus 3%), shock on admission (11% versus 3%), and in-hospital mortality (8% versus 3%) (p<0.001 for all comparisons). There was a significant increase in the proportion of patients meeting guideline goals of FMC-to-device time, including those directly presenting via EMS (50% to 55%; p<0.001) and transferred patients (44% to 48%; p=0.002). Despite regional variability, the greatest gains occurred among patients in the 5 most-improved regions, increasing from 45% to 57% (direct EMS; p<0.001), and 38% to 50% (transfers; p<0.001).
Conclusions
This Mission: Lifeline™ STEMI Systems Accelerator demonstration project represents the largest national effort to organize regional STEMI care. By focusing on FMC-to-device time, coordinated treatment protocols, and regional data collection and reporting, we were able to significantly increase the proportion of patients treated within guideline goals.
Keywords: myocardial infarction, catheterization, reperfusion, survival
INTRODUCTION
Rapid coronary artery reperfusion is the foundation of treatment for acute ST-segment elevation myocardial infarction (STEMI) to improve survival. Based upon randomized trial data, national guidelines call for primary percutaneous coronary intervention (PCI) within 90 minutes of paramedic arrival for patients who call 911 and are transferred directly to a hospital offering PCI (PCI-capable), and within 120 minutes of first medical contact (FMC) for patients requiring inter-hospital transfer.1,2 Despite 2 decades of evidence and 7 years since these guidelines were introduced, approximately 30% to 50% of patients fail to meet these standards.3–6 Considering that the number of PCI-capable hospitals increased by almost 50% and that 90% of Americans live within 60 minutes of a PCI-capable facility, inadequate access cannot entirely explain these systematic failures.7–10 Rather, the challenge lies within a highly fragmented health system comprising approximately 4750 acute care hospitals and more than 15,000 emergency medical service (EMS) agencies in the United States. The challenge is further exacerbated by structural barriers that hinder coordination between EMS providers and hospitals, as well as competition among hospitals and physician groups. Such fragmentation has hindered the development of coordinated treatment plans and procedures, common data collection and feedback systems, and systematic approaches to accurately identify and direct STEMI patients to nearby catheterization laboratories for timely coronary intervention.11
Building upon successful efforts in organizing STEMI reperfusion systems on a regional basis, we developed a demonstration project designed to implement coordinated care in selected major metropolitan regions in the United States.12,13 Our hypothesis was that by organizing leadership, data collection, common protocols, and ongoing data review with timely feedback, we could increase the percentage of patients receiving primary PCI within guideline goals. Our intervention was based upon Mission: Lifeline™ established approaches and supported by a national faculty highly experienced in organizing regional STEMI care.
METHODS
The STEMI Systems Accelerator project intervention was organized and executed between March 2012 and July 2014 (Supplemental Figure 1). Among 21 regions that applied for participation in the project, 16 met enrollment criteria by the baseline data-collection quarter and were included. These criteria included the following: 1) 70% of PCI hospitals in the region were participating in the National Cardiovascular Data Registry’s ACTION Registry®-Get With The Guidelines™ (AR-G) program, 2) there was defined organization of regional leadership, 3) common protocols were established for the diagnosis and treatment of STEMI patients presenting to EMS personnel or hospitals lacking PCI facilities (PCI non-capable), 4) there was agreement to enter patients into the AR-G for 6 consecutive quarters, and 5) regional leadership participated in a 2-day national training session directed by study faculty reviewing current evidence, guidelines, and approaches to regional STEMI care.
Project initiation was conducted on a rolling basis over 6 months, and each region specified a quarter (quarters 3 or 4, 2012; or quarter 1, 2013) as the baseline from which to assess subsequent temporal trends in outcomes. Following hospital enrollment in the AR-G and the training of leadership, each region established common protocols as outlined above, implemented the protocols, and conducted ongoing measurement and feedback on performance that was reflected in quarterly hospital letter-coded regional STEMI treatment reports. These protocols were guided by local experts, resources, and practices, and included common criteria for establishing the diagnosis of STEMI, activating a catheterization laboratory with a single phone or radio call, treating the patient with simple initial regimens, and transporting the patient by pre-identified mechanisms. In each region, 2 project faculty members, including a cardiology or emergency medicine physician and a regional coordinator, conducted a launch meeting in collaboration with regional leadership.14 These meetings reviewed the principles of STEMI diagnosis and treatment, current national guidelines, and regional models for STEMI care, as well as case studies specific to each region for patients presenting to EMS providers and patients requiring hospital transfer.
At each meeting, an EMS “wish list” was presented to encourage participating hospitals to support the needs of local providers. This list was a compilation of hospital requests by regional EMS leadership in order to facilitate diagnosis and treatment, and included requests such as activating the catheterization laboratory upon EMS call. In order to change the standard of care and create sustainable systems, we relied on local and regional mechanisms for protocol implementation, such as EMS annual training sessions or state-approved treatment protocols.
Statistical Analysis
The current study presents the primary outcomes and temporal trends over the 24 months after initiation of the STEMI Systems Accelerator project. The pre-specified primary outcome was the change in the percentage of patients meeting guideline goals over 6 quarters (post-baseline quarter). Descriptive statistics for continuous and categorical variables were described as medians (quartiles) and numbers (percentages), respectively. Patient characteristics and process measures were compared by use of the Wilcoxon rank-sum test for 2-group comparisons (the Kruskal-Wallis test was used for comparisons of more than 2 groups) for continuous variables and Pearson’s chi-square or Fisher exact tests, as appropriate for categorical variables. The Cochran-Armitage test for trend was used to assess changes in rates over time. The relationship between emergency department (ED) dwell time—defined as the period from ED arrival to cardiac catheterization laboratory arrival—and in-hospital mortality was assessed using logistic regression modeling. The rolling 12-month (4 quarters) moving-average of in-hospital mortality for STEMI Systems Accelerator hospitals versus the AR-G registry hospitals were presented graphically.
All statistical tests were conducted at the 0.05 significance level. All patients with ischemic symptoms lasting >10 minutes within 12 hours before arrival and an electrocardiogram (ECG) with diagnostic ST-segment elevation were included in the analyses. In cases where the first ECG did not have diagnostic ST-segment elevation, door or FMC time was reset to the first diagnostic ECG. Statistical analyses were performed with SAS version 9.3 (SAS Institute Inc, Cary, NC). The project was reviewed by the Duke Institutional Review Board and classified as exempt.
RESULTS
Patient Characteristics and Presentation
Between July 2012 and December 2013, 23,809 patients presented with acute STEMI, including 18,267 patients who presented directly to a PCI-capable hospital and 5542 who were transferred from hospitals without PCI capability (Table 1). Among patients presenting to PCI-capable hospitals, 64% (n=11,765) were transported by EMS providers, while 36% (n=6502) arrived by self-transport. The median age of the cohort was 60 years (quartiles 52–70 years); 29% of patients were women; 11% were black; and 10% were of Latino ethnicity.
Table 1.
Patient Characteristics, 7 Quarters (2012Q3 to 2014Q1)
| Characteristic | Direct presenter, EMS transport (N=11,765) | Direct presenter, self transport (N=6502) | Transferred (N=5542) | Overall (N=23809) |
|---|---|---|---|---|
| Age (years) | ||||
| N | 11765 | 6502 | 5542 | 23809 |
| Median | 62.0 | 59.0 | 60.0 | 60.0 |
| Q1–Q3 | 53.0–72.0 | 51.0–68.0 | 52.0–69.0 | 52.0–70.0 |
| Sex, n (%) | ||||
| Male | 8002 (68.0%) | 4811 (74.0%) | 4021 (72.6%) | 16834 (70.7%) |
| Female | 3763 (32.0%) | 1691 (26.0%) | 1521 (27.4%) | 6975 (29.3%) |
| Race, n (%) | ||||
| White | 9510 (80.8%) | 5475 (84.2%) | 4615 (83.3%) | 19600 (82.3%) |
| Black | 1456 (12.4%) | 589 (9.1%) | 508 (9.2%) | 2553 (10.7%) |
| Other | 799 (6.8%) | 438 (6.7%) | 419 (7.6%) | 1656 (7.0%) |
| Latino ethnicity, n (%) | 1181/11737 (10.1 %) | 771/6477 (11.9%) | 413/5532 (7.5%) | 2365/23746 (10.0%) |
| Insurance, n (%) | ||||
| Private/HMO | 6133/9874 (62.1%) | 3867/5415 (71.4%) | 3109/4651 (66.9%) | 13109/19940 (65.7%) |
| Medicaid | 1278/9874 (12.9%) | 481/5415 (8.9%) | 536/4651 (11.5%) | 2295/ 19940 (11.5%) |
| None | 1891 (16.1%) | 1087 (16.7%) | 891 (16.1%) | 3869 (16.3%) |
| Other | 2608 (22.2%) | 1112 (17.1%) | 1058 (19.1%) | 4778 (20.1%) |
| Prior myocardial infarction, n (%) | 1536/8025 (19.1%) | 699/4498 (15.5%) | 580/3640 (15.9%) | 2815/16163 (17.4%) |
| Prior heart failure, n (%) | 490/8021 (6.1%) | 141/4495 (3.1%) | 157/3640 (4.3%) | 788/ 16156 (4.9%) |
| Prior PCI, n (%) | 1636/8025 (20.4%) | 809/4498 (18.0%) | 618/ 3641 (17.0%) | 3063/16164 (19.0%) |
| Prior coronary bypass surgery, n (%) | 442/8021 (5.5%) | 243/4499 (5.4%) | 210/3638 (5.8%) | 895/16158 (5.5%) |
| Diabetes mellitus, n (%) | 3160/11757 (26.9%) | 1756/6501 (27.0%) | 1412/ 5537 (25.5%) | 6328/23795 (26.6%) |
| Symptom onset to FMC (minutes) | ||||
| N | 10,432 | 5587 | 4833 | 20,852 |
| Median | 47.0 | 114.0 | 89.0 | 69.0 |
| Q1–Q3 | 22.0–116.0 | 56.0–272.0 | 47.0–200.0 | 32.0–172.0 |
| Shock on presentation, n (%) | 1313/11754 (11.2%) | 215/6498 (3.3%) | 465/5533 (8.4%) | 1993/23785 (8.4%) |
| Cardiac arrest, n (%) | 1227/11703 (10.5%) | 169/6455 (2.6%) | 531/5515 (9.6%) | 1927/23673 (8.1%) |
| Heart failure on presentation, n (%) | 906/11756 (7.7%) | 351/6497 (5.4%) | 417/5534 (7.5%) | 1674/23787 (7.0%) |
| Reperfusion candidate, n (%) | 11248/11751 (95.7%) | 6180/6497 (95.1%) | 5234/5535 (94.6%) | 22662/23783 (95.3 %) |
| Heart rate on presentation (bpm) | ||||
| N | 11,737 | 6485 | 5529 | 23,751 |
| Median | 78.0 | 81.0 | 79.0 | 80.0 |
| Q1–Q3 | 64.0–93.0 | 69.0–95.0 | 66.0–94.0 | 66.0–94.0 |
| Systolic BP (mmHg) | ||||
| N | 11,734 | 6483 | 5526 | 23,743 |
| Median | 134.0 | 150.0 | 142.0 | 140.0 |
| Q1–Q3 | 111.0–155.0 | 130.0–171.0 | 122.0–162.0 | 119.0–161.0 |
| STEMI first diagnosed, n (%) | ||||
| First ECG | 11459/11693(98.0%) | 6328/6444 (98.2%) | 5415/5497 (98.5%) | 23202/23634 (98.2 %) |
| Subsequent | 234/11693 (2.0%) | 116/6444 (1.8%) | 82/5497 (1.5%) | 432/23634 (1.8%) |
| Procedures during hospitalization, n (%) | ||||
| PCI | 10579/11762 (89.9%) | 5883 (90.5%) | 4890 (88.2%) | 21352 (89.7%) |
| Coronary bypass surgery | 428 (3.6%) | 266 (4.1%) | 314 (5.7%) | 1008 (4.2%) |
| Complications, n (%) | ||||
| In-hospital death | 961 (8.2%) | 175 (2.7%) | 306 (5.5%) | 1442 (6.1%) |
| Stroke | 92 (0.8%) | 43 (0.7%) | 51 (0.9%) | 186 (0.8%) |
| Hemorrhagic stroke | 13 (0.1%) | 7 (0.1%) | 9 (0.2%) | 29 (0.1/185 (15.7%) |
| Cardiogenic shock | 1095/11747 (9.3%) | 355/6499 (5.5%) | 421/5539 (7.6%) | 1871/23785 (7.9%) |
| Congestive heart failure | 826/11748 (7.0%) | 317/6497 (4.9%) | 345/5537 (6.2%) | 1488/23782 (6.3 %) |
| Major bleeding | 560/11749 (4.8%) | 227/6496 (3.5%) | 233/5538 (4.2%) | 1020/23783 (4.3%) |
| Reinfarction | 112/11749 (1.0%) | 53/6497 (0.8%) | 44/5538 (0.8%) | 209/23784 (0.9%) |
| Not treated, n (%) | 751 (6.4%) | 385 (5.9%) | 338 (6.1%) | 1474 (6.2%) |
| ED dwell time (minutes), n (%) | ||||
| n | 10234 | 5855 | 2329 | 18418 |
| ≤20 | 2560 (25.0%) | 253 (4.3%) | 503 (21.6%) | 3316 (18%) |
| >20 to ≤30 | 2045 (20.0%) | 794 (13.6%) | 256 (11.0%) | 3095 (16.8%) |
| >30 to ≤45 | 2575 (25.2%) | 1474 (25.2%) | 850 (36.5%) | 4899 (26.6%) |
| >45 | 3054 (29.8%) | 3334 (56.9%) | 720 (30.9%) | 7108 (38.6%) |
ED = emergency department; EMS = emergency medical services; HMO = health maintenance organization; PCI = percutaneous coronary intervention; STEMI = ST-segment elevation myocardial infarction
The overall median time from symptom onset to FMC was 69 minutes. There were marked differences in time from symptom onset to FMC according to mode of arrival to the hospital. Patients transported by EMS had a median time of 47 minutes from symptom onset to FMC, while self-transported patients had a median time of 114 minutes (p<0.001). The overall rates of cardiac arrest or shock on admission was 8% for both events. For patients presenting directly to PCI-capable hospitals, those transported by EMS had significantly greater rates of cardiac arrest (10% versus 3%) and shock on admission (11% versus 3%, p<0.001 for both comparisons) compared with self-transported patients. Transferred patients had rates of cardiac arrest (10%) and shock (8%) that were similar to EMS-transported patients. STEMI was apparent on the initial ECG for 98% of patients, and 95% of patients were thought to be reperfusion candidates by medical record review. Of eligible patients, 94% were treated with reperfusion.
Primary Outcome and Temporal Trends
Comparing aggregate rates across all regions, there were significant but modest increases in the percentage of patients meeting guideline goals (time from FMC to device of <90 minutes for PCI-capable hospitals versus <120 minutes for PCI non-capable hospitals). The proportion of patients presenting directly to a PCI-capable center achieving guideline goals increased from 59% to 61% (p=0.005) (Figure 1). The subset of EMS-transported patients increased from 50% to 55% (p<0.001), and the subset of transferred patients increased from 44% to 48% (p=0.002). There was substantial regional variability, and the greatest improvements were seen in EMS-transported patients. For the 5 most-improved regions among EMS-transported patients (Figure 2a), the proportion of those treated within 90 minutes increased from 45% to 57%, with an increase from 56% to 76% for the most-improved region (Region 4) (trend test p<0.001 for both comparisons). For transferred patients, the proportion treated within 120 minutes increased from 38% to 50% (trend test p<0.001), with the most-improved region (Region 9) increasing from 33% to 56% (trend test p=0.16) (Figure 2b). The proportion of patients treated within the guideline-recommended time intervals for each of the 16 regions is shown in Supplemental Tables 1a and 1b (EMS direct) and Supplemental Tables 2a and 2b (transferred).
Figure 1.
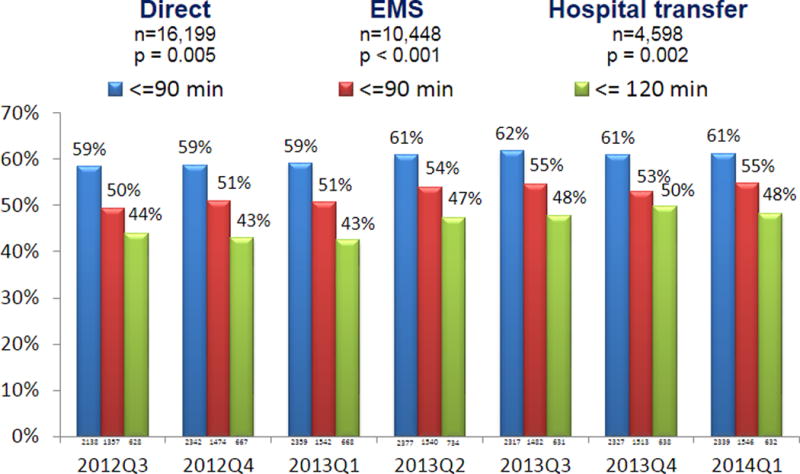
Percent of patients meeting guideline goal for FMC-to-device time by quarter. Numbers below each bar represent the total number of patients for each transportation modality for that quarter.
Direct = all patients presenting directly to PCI-capable hospitals; EMS = patients presenting to PCI-capable hospitals by EMS transport; FMC = first medical contact; Transfer = patients transferred to PCI-capable hospitals; Q = quarter.
Figure 2.
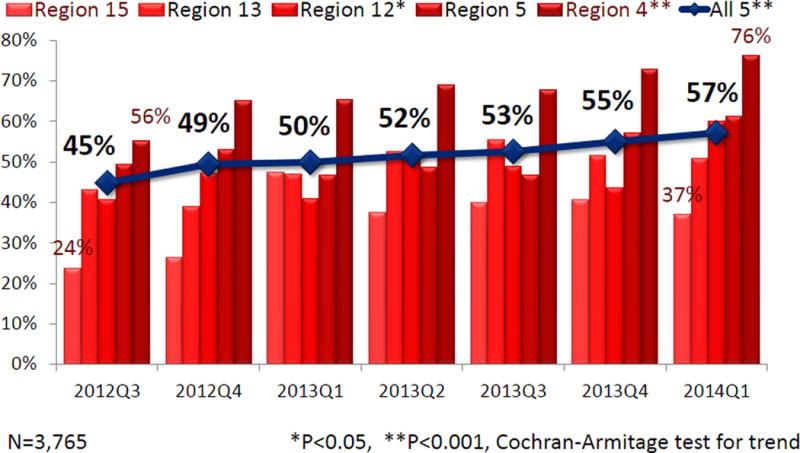
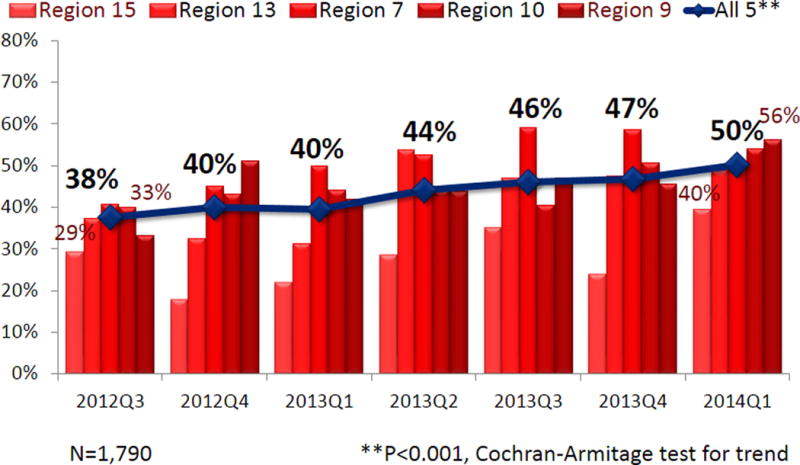
Percentage of EMS-transported patients meeting guideline goals for FMC-to-device time by quarter, 5 most-improved regions for direct EMS patients (a) and transferred patients (b)
EMS = emergency medical services’ FMC = first medical contact; Q = quarter.
Overall in-hospital mortality for the time period was 6.1%, with the highest mortality for EMS-transported patients (8.2%) and substantially lower mortality for self-transported patients (2.7%) presenting directly to a PCI-capable hospital, and an intermediate level of mortality for patients transferred to PCI-capable hospitals (5.5%). These mortality differences correlated with higher rates of cardiac arrest and shock among the higher mortality subgroups.
Over the course of the intervention, there was no significant change in in-hospital mortality. Figure 3 shows 12-month (4 quarters) moving-averages of in-hospital mortality rates over time for patients treated in the STEMI Systems Accelerator project hospitals (n=27,537) versus those treated in hospitals participating in the AR-G registry separately from this work (n=97,283). In the first 4 quarters (2012Q4–2013Q3) average, STEMI Systems Accelerator hospitals had mortality rates similar to the national comparator’s rates (in the 6.2% range). In the final 4 quarters (2013Q4–2014Q3) average, mortality for STEMI Systems Accelerator hospitals fell to 5.8%, while the comparator national hospitals’ mortality rate remained unchanged (p=0.053). Baseline clinical characteristics were similar between patients admitted to Accelerator hospitals compared with those admitted to non-Accelerator hospitals over this time period, with some exceptions (Supplemental Table 3). Compared with non-Accelerator hospitals, patients admitted to Accelerator hospitals tended to have fewer baseline co-morbidities (history of dyslipidemia, hypertension, or prior revascularization) but were more likely to present with cardiogenic shock and cardiac arrest.
Figure 3.
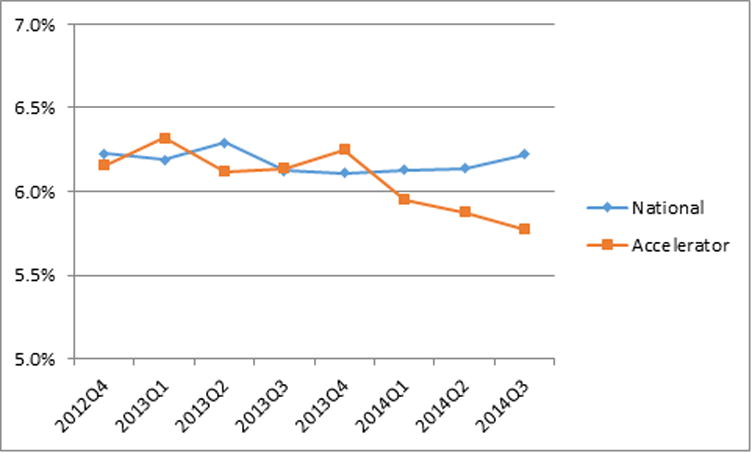
Rolling 12-month (4 quarters) moving-average of in-hospital mortality comparing AR-G patients treated in STEMI Systems Accelerator hospitals (Accelerator) versus hospitals not participating in the project (National)
ACTION Registry®-Get With The Guidelines™; Q= quarter.
We also compared FMC-to-device and door-to-device times (75th percentile) by region for baseline quarter (Figure 4). We found that all regions had door-to-device times of <90 minutes for 75% of patients, while no regions achieved this standard for FMC-to-device time at the start of our intervention.
Figure 4.
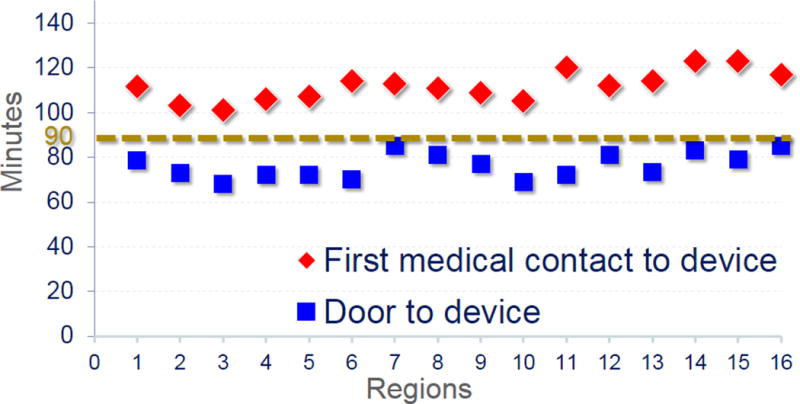
FMC and door-to-device times by region, 75th percentile for baseline quarter
FMC = first medical contact.
DISCUSSION
This work represents the largest effort to organize STEMI care on a regional basis ever attempted in the United States, involving 484 hospitals and 1253 EMS agencies in 16 regions. We found important opportunities for improvement by focusing on guideline goals of FMC to device deployment. With the collaboration and support of a diverse range of health care professionals, we were able to implement regional data collection, standardize reporting, and coordinate treatment plans over 2 years involving approximately one-quarter of all STEMI patients entered into the AR-G during the time period. There was marked variability in the time required to implement regionally agreed-upon plans. Despite this variability, we saw modest but significant improvements in guideline-mandated treatment times for the entire cohort and marked improvement in select regions. Notably, temporal trends in hospital mortality suggested favorable effects for this broad and intensive quality-improvement intervention. We expect these trends to continue to improve as the regional protocols are implemented on a more complete basis and become embedded as standards of care for all hospitals and EMS agencies within a region.
The systems organized in the STEMI Systems Accelerator project differ significantly from previously reported individualized STEMI systems—such as those organized by the Minneapolis Heart Institute, Prairie Heart Institute, Geisinger Health System, and Mayo Clinic—in that these reports generally involve a few primary PCI hospitals within a single health care network.15–18 Our hypothesis was that standards of care could be more readily changed if the majority of PCI-capable facilities and interventional cardiologists in a region could agree to a common plan, thus allowing EMS providers to diagnose and treat patients in an expedited fashion without concern or modification according to the receiving facility or cardiologist. This work is also unique in that it is the first published intervention to rely on Mission: Lifeline™ regional reports, designed according to national guidelines, representing aggregated data from the AR-G. These reports include process measures and times important to STEMI reperfusion (FMC starting at paramedic or first hospital arrival to hospital discharge) according to regional averages and hospital-specific performance.19 Hospital identifiers were letter-coded and only provided to the individuals working within those hospitals.
While much of our effort involved recruiting hospitals to participate in a common regional registry and convincing them to allow their data to be aggregated in regional reports, this effort in recruiting hospital participation appeared highly fruitful. As a result of these reports, we were able to identify opportunities for systematic improvement using objective data and ultimately convince health care systems and providers to modify protocols and improve care. The Mission: Lifeline™ reports and systems are currently being implemented in many other regions and states, including North Carolina, Mississippi, South Dakota, and Dallas, Texas.20
Of particular note is our focus on the 2006 guidelines standard of “first medical contact to device” rather than the Center for Medicare and Medicaid Services reported “door to balloon” measurement reflective of older standards.2 In our project and as nationally reported, the majority of PCI-capable hospitals achieve door-to-device times of <90 minutes. As illustrated in Figure 4, for our 16 regions in the baseline period of data collection, all regions had door-to-device times of <90 minutes for 75% of patients, while no regions achieved this standard for FMC to device. As shown, patients can still have lengthy delays in care not identified by the door-to-device metric that does not account for the time between patient presentation and hospital arrival. These delays are particularly notable for transferred patients. Thus, we believe that a reliance on the door-to-device metric leads to missed opportunities for improved care. The remaining delays in STEMI reperfusion identified by these data and national registries indicate that FMC should become the focus of national quality metrics and efforts. A reliance on the door-to-balloon metric rather than FMC to device could explain the relative lack of improvement in outcomes identified by efforts that ignore pre-hospital care.21 Findings that fail to identify benefit for faster treatment run counter to clinical experience and clinical trial data that indicate the importance of timely reperfusion in reducing morbidity and mortality for STEMI patients.22–26
In addition to our overall findings, we present treatment times for each of the 16 participating regions, as well as the top 5 performing regions for both EMS direct and transferred patients. These data have important implications. While the overall results were modest, we found significant variability between regions, including those that did not improve at all. The overall findings and the variability in improvement was primarily related to the speed with which regions could implement effective EMS and hospital transfer protocols. A large portion of this delay was related to the time required to persuade the majority of regional hospitals to participate in AR-G in shared reporting, execution of contracts, and initiation of data collection. This highlights the challenge of pursuing such a large scale implementation over a relatively short time period. Nevertheless, the results from the most-improved regions indicate that it is possible to rapidly and substantially improve reperfusion times within some regions according to our approach. With only 16 regions to compare, we cannot reliably identify those regional factors associated with the greatest improvement among a myriad of local socioeconomic and political factors that are unique to each region. Based upon our experience, we believe the regions most able to improve treatment times had common characteristics, including EMS leadership concentrated to a few dominant agencies and active daily engagement by a dedicated regional coordinator charged with implementing systematic improvements within every hospital and EMS agency in the region.
Most efforts to improve STEMI reperfusion times, including this work, have focused on the time period from when the patient enters the medical system to the provision of primary PCI or fibrinolysis. At the same time, registries have indicated that the median time from symptom onset to presentation has remained in the 2-hour range for at least 2 decades.27,28 An important observation from our study is that symptom duration for patients presenting to EMS was markedly shorter (47 minutes from symptom onset until paramedic arrival versus 114 minutes for self-transported patients who presented to EDs). This finding identifies an opportunity to achieve remarkably shorter total ischemic time (symptom onset to reperfusion) and also allows modest improvements in time to result in major improvement in salvage (and survival) since these patients are on the “steep part” of the curve describing the association of time and mortality. Emergency dispatch programs that encourage patients to call 911 for persistent symptoms of potential heart attack, direct ECG-capable providers to chest pain calls, and enable paramedics to diagnose STEMI and directly activate catheterization laboratories are best suited to markedly decrease the time from symptom onset to reperfusion. Our findings of greater illness severity and higher mortality correspond with prior work.29 We conjecture that more severe symptoms are likely associated with greater illness severity, which triggers patients and families to dispatch emergency medical care. Patients who self-transport to the hospital and experience cardiac arrest are much less likely to survive or be entered in the AR-G registry compared with those transported by EMS.
For ideal patients with recognizable symptoms who receive diagnostic ECGs, and have local access to PCI-capable facilities, total ischemic time can potentially be reduced to <2 hours, allowing for treatment during the earliest phases of MI when patients are postulated to receive the most benefit.23 Such coordinated care is reflected by short ED dwell times as patients can proceed from the ambulance to waiting catheterization laboratories with successful pre-activation. The potential benefit of such coordination is further supported by the observation that shorter ED dwell time is highly associated with lower mortality (Supplemental Figure 2). Stratifying EMS-transported patients according to ED dwell time, in-hospital mortality was 3.6% for patients with dwell times <30 minutes, 7.0% for dwell times of 30 to 45 minutes, and 10.8% for dwell times over 45 minutes. We also found that a greater proportion of patients met ED dwell times of ≤20 minutes over the course of the study (Supplemental Figure 3). While this comparison of ED time and mortality has great potential for confounding according to additional time spent treating patients who suffer life-threatening events in the ED, the relationship also suggests that processes associated with a shorter delay in the ED, such as pre-hospital lab activation by paramedics, may improve outcomes. With more than 1700 hospitals performing coronary interventions and up to 90% of the U.S. population living within a 60-minute drive time, abbreviated ED dwell times and timely intervention should be achievable for the majority of patients transported by paramedics.7–10
Limitations
There are limitations worth noting, the first of which involves the observational nature of measurements. For an intervention like this, the relationship between our efforts and treatment times and mortality is highly subject to confounding. Our finding that Accelerator hospitals experienced a trend toward a reduction in unadjusted mortality in the final 4 quarters (despite similar baseline clinical characteristics) represents post-hoc analyses that provide limited support to the potential for lower mortality in Accelerator regions compared with hospitals participating in the AR-G registry at the same time. Furthermore, other quality-improvement efforts being conducted by participating EMS agencies and hospitals may have contributed to improved treatment times. As the AR-G was regionally expanded to institutions and patients who previously would not have been included, treatment times and outcomes had the potential to change independent of our intervention if such patients faced longer delays compared with patients enrolled in prior quarters.25 Similarly, the global nature of our intervention should be considered when comparing these findings to outcomes for patients treated in hospitals participating in the AR-G that were not part of this project. The approximately 800 hospitals participating in the registry represent a subset of more than 1700 performing PCI, and their participation possibly indicates greater focus on quality, timely treatment, and ultimately better outcomes compared with the universe of hospitals performing primary PCI. With such potential for confounding, randomized trials and observational registries should serve as the basis for providing timely reperfusion, rather than findings from a rapidly expanding regional effort. Finally, despite the large number of patients in this study, measuring reperfusion times over 2 years may still be underpowered to show the true impact of the intervention, since continual improvement may continue to occur in the future.
CONCLUSIONS
This Mission: Lifeline™ STEMI Systems Accelerator Regional Systems of Care Demonstration Project represents the largest effort to date in the United States to organize treatment for STEMI on a regional basis, involving 484 hospitals, 1253 EMS agencies, and many thousands of health care professionals. By focusing on FMC-to-device time, regional consensus treatment protocols, and common data collection, we observed a significant increase in the proportion of patients treated within guideline goals. The speed with which systems could be implemented varied greatly by region, and the improvements demonstrated by our data, while modest, suggest the potential for reductions in total ischemic time. Corresponding with the fullest implementation of the intervention, we began to observe trends toward lower in-hospital mortality compared with national data toward the end of our measurement period.
Clinical Perspective.
What is new?
This work represents the largest effort ever attempted in the United States to organize ST-segment elevation myocardial infarction (STEMI) care across multiple regions.
The work involved 23,809 patients treated at 484 hospitals and 1253 emergency medical services (EMS) agencies in 16 regions, including New York City, Atlanta, Houston, and St. Louis, or roughly one in four patients entered into the NCDR’s ACTION Registry® during the 18 months of measurement.
What are the clinical implications?
Supported by thousands of colleagues and American Heart Association quality personnel, we were able to organize regional leadership and coordinate treatment plans that spanned the majority of EMS providers, emergency departments, and cardiac catheterization laboratories within each region.
These primary results show modest but significant improvements in treatment times, with marked improvement in the five top-performing regions.
These findings support continued efforts to implement regional STEMI networks.
Acknowledgments
Funding Sources: The Regional Systems of Care Demonstration Project: Mission: Lifeline™ STEMI Systems Accelerator is supported by the ACTION Registry®-Get With The Guidelines™ and education and research grants by The Medicines Company, Abiomed, Inc, Philips Healthcare, and AstraZeneca.
Footnotes
Disclosures:
JG Jollis: Research grants: The Medicines Company, Astra Zeneca, Medtronic Foundation, Philips Healthcare, Abiomed, Inc.
HR Al-Khalidi: None.
ML Roettig: None.
PB Berger: Research grants: Janssen, The Medicines Company, Astra Zeneca, Lilly, Sanofi. Consultant: Janssen, Medicure.
CC Corbett: None.
HL Dauerman: Consultant: Medtronic, Boston Scientific, Daichi Sankyo, The Medicines Company. Research grants: Medtronic, Abbott Vascular.
CB Fordyce: None.
K Fox: None.
JL Garvey: Research support & advisory board member: Philips Healthcare.
T Gregory: None.
TD Henry: None.
IC Rokos: None.
MW Sherwood: Honoraria from Boerhinger Ingelheim, Education grant from Astra Zeneca, Project Grant from Gliead Sciences.
RE Suter: None.
BH Wilson: Consultant: Medical. Advisory Board: Boston Scientific Corporation.
CB Granger: All disclosures are available at https://dcri.org/about-us/conflict-of-interest. Research support from Armetheon, AstraZeneca, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Daiichi Sankyo, FDA, GlasoSmithKline, Janssen Pharmaceuticals, The Medicines Company, Medtronic Foundation, Novartis, Pfizer, Sanofi-Aventis, and Takeda. Consulting or other services for AstraZeneca, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Eli Lilly, Daiichi Sankyo, Gilead, GlaxoSmithKline, Hoffmann-La roche, Janssen Pharmaceuticals, The Medicines Company, Medtronic Inc., NIH, Novartis, Pfizer, Sanofi-Aventis, and Takeda.
Journal subject codes: [4] Acute myocardial infarction; [24] Catheter-based coronary interventions: stents; [25] CPR and emergency cardiac care; [100] Health policy and outcome research
References
- 1.O’Gara PT, Kushner FG, Ascheim DD, Casey DE, Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis-Holland JE, Tommaso JE, Tracy CM, Woo YJ, Zhao DX. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the American College of Emergency Physicians and Society for Cardiovascular Angiography and Interventions. Circulation. 2013;127:529–555. [Google Scholar]
- 2.Antman EM, Hand M, Armstrong PW, Bates ER, Green LA, Halasyamani LK, Hochman JS, Krumholz HM, Lamas GA, Mullany CJ, Pearle DL, Sloan MA, Smith SC, Jr, 2004 Writing Committee Members. Anbe DT, Kushner FG, Ornato JP, Jacobs AK, Adams CD, Anderson JL, Buller CE, Creager MA, Ettinger SM, Halperin JL, Hunt SA, Lytle BW, Nishimura R, Page RL, Riegel B, Tarkington LG, Yancy CW. 2007 Focused Update of the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: developed in collaboration With the Canadian Cardiovascular Society endorsed by the American Academy of Family Physicians: 2007 Writing Group to Review New Evidence and Update the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction, Writing on Behalf of the 2004 Writing Committee. Circulation. 2008;117:296–329. doi: 10.1161/CIRCULATIONAHA.107.188209. [DOI] [PubMed] [Google Scholar]
- 3.Dauerman HL, Bates ER, Kontos MC, Li S, Garvey JL, Manoukian SV, Roe MT. Nationwide Analysis of Patients With ST-Segment-Elevation Myocardial Infarction Transferred for Primary Percutaneous Intervention: Findings From the American Heart Association Mission: Lifeline Program. Circ Cardiovasc Interv. 2015;8:pii:e002450. doi: 10.1161/CIRCINTERVENTIONS.114.002450. [DOI] [PubMed] [Google Scholar]
- 4.Bagai A, Al-Khalidi HR, Muñoz D, Monk L, Roettig ML, Corbett CC, Garvey JL, Wilson BH, Granger CB, Jollis JG. Bypassing the emergency department and time to reperfusion in patients with prehospital ST-segment-elevation: findings from the reperfusion in acute myocardial infarction in Carolina Emergency Departments project. Circ Cardiovasc Interv. 2013;6:399–406. doi: 10.1161/CIRCINTERVENTIONS.112.000136. [DOI] [PubMed] [Google Scholar]
- 5.Bagai A, Jollis JG, Dauerman HL, Peng SA, Rokos IC, Bates ER, French WJ, Granger CB, Roe MT. Emergency department bypass for ST-segment-elevation myocardial infarction patients identified with a prehospital electrocardiogram: a report from the American Heart Association Mission: Lifeline program. Circulation. 2013;128:352–359. doi: 10.1161/CIRCULATIONAHA.113.002339. [DOI] [PubMed] [Google Scholar]
- 6.Fosbol EL, Granger CB, Jollis JG, Monk L, Lin L, Lytle BL, Xian Y, Garvey JL, Mears G, Corbett CC, Peterson ED, Glickman SW. The impact of a statewide pre-hospital STEMI strategy to bypass hospitals without percutaneous coronary intervention capability on treatment times. Circulation. 2013;127:604–612. doi: 10.1161/CIRCULATIONAHA.112.118463. [DOI] [PubMed] [Google Scholar]
- 7.Langabeer JR, Henry TD, Kereiakes DJ, Dellifraine J, Emert J, Wang Z, Stuart L, King R, Segrest W, Moyer P, Jollis JG. Growth in percutaneous coronary intervention capacity relative to population and disease prevalence. J Am Heart Assoc. 2013;2:e000370. doi: 10.1161/JAHA.113.000370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shah RU, Henry TD, Rutten-Ramos S, Garberich R, Tighouart M, Bairey Merz CN. Increasing percutaneous coronary interventions for ST-segment elevation myocardial infarction in the United States: progress and opportunity. JACC Cardiovasc Interv. 2015;8:139–146. doi: 10.1016/j.jcin.2014.07.017. [DOI] [PubMed] [Google Scholar]
- 9.Nallamothu BK, Bates ER, Herrin J, Wang Y, Bradley EH, Krumholz HM. Driving times and distances to hospitals with percutaneous coronary intervention in the United States: implications for prehospital triage of patients with ST-elevation myocardial infarction. Circulation. 2006;113:1189–1195. doi: 10.1161/CIRCULATIONAHA.105.596346. [DOI] [PubMed] [Google Scholar]
- 10.Concannon TW, Nelson J, Kent DM, Griffith JL. Evidence of systematic duplication by new percutaneous coronary intervention programs. Circ Cardiovasc Qual Outcomes. 2013;6:400–408. doi: 10.1161/CIRCOUTCOMES.111.000019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Henry TD, Atkins JM, Cunningham MS, Francis GS, Groh WJ, Hong RA, Kern KB, Larson DM, Ohman EM, Ornato JP, Peberdy MA, Rosenberg MJ, Weaver WD. ST-segment elevation myocardial infarction: recommendations on triage of patients to heart attack centers: is it time for a national policy for the treatment of ST-segment elevation myocardial infarction? J Am Coll Cardiol. 2006;47:1339–1345. doi: 10.1016/j.jacc.2005.05.101. [DOI] [PubMed] [Google Scholar]
- 12.Jollis JG, Granger CB, Henry TD, Antman EM, Berger PB, Moyer PH, Pratt FD, Rokos IC, Acuña AR, Roettig ML, Jacobs AK. Systems of care for ST-segment-elevation myocardial infarction: a report from the American Heart Association’s Mission: Lifeline. Circ Cardiovasc Qual Outcomes. 2012;5:423–428. doi: 10.1161/CIRCOUTCOMES.111.964668. [DOI] [PubMed] [Google Scholar]
- 13.Jollis JG, Roettig ML, Aluko AO, Anstrom KJ, Applegate RJ, Babb JD, Berger PB, Bohle DJ, Fletcher SM, Garvey JL, Hathaway WR, Hoekstra JW, Kelly RV, Maddox WT, Jr, Shiber JR, Valeri FS, Watling BA, Wilson BH, Granger CB. Implementation of a statewide system for coronary reperfusion for ST-segment elevation myocardial infarction. JAMA. 2007;298:2371–2380. doi: 10.1001/jama.298.20.joc70124. [DOI] [PubMed] [Google Scholar]
- 14.Bagai A, Al-Khalidi HR, Sherwood M, Munoz D, Roettig ML, Jollis JG, Granger CB. Regional systems of care demonstration project: Mission: Lifeline STEMI Systems Accelerator: design and methodology. Am Heart J. 2014;167:15–21.e3. doi: 10.1016/j.ahj.2013.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Henry TD, Sharkey SE, Burke MN, Chavez IJ, Graham KJ, Henry CR, Lips DL, Madison JD, Menssen KM, Mooney MR, Newell MC, Pedersen WR, Poulose AK, Traverse JH, Unger BT, Wang YL, Larson DM. A regional system to provide timely access to percutaneous coronary intervention for ST-elevation myocardial infarction. Circulation. 2007;116:721–728. doi: 10.1161/CIRCULATIONAHA.107.694141. [DOI] [PubMed] [Google Scholar]
- 16.Aguirre FV, Varghese JJ, Kelley MP, Lam W, Lucore CL, Gill JB, Page L, Turner L, Davis C, Mikell FL. Rural interhospital transfer of ST-elevation myocardial infarction patients for percutaneous coronary revascularization: the Stat Heart Program. Circulation. 2008;117:1145–1152. doi: 10.1161/CIRCULATIONAHA.107.728519. [DOI] [PubMed] [Google Scholar]
- 17.Ting HH, Rihal CS, Gersh BJ, Haro LH, Bjerke CM, Lennon RJ, Lim CC, Bresnahan JF, Jaffe AS, Holmes DR, Bell MR. Regional systems of care to optimize timeliness of reperfusion therapy for ST-elevation myocardial infarction: the Mayo Clinic STEMI Protocol. Circulation. 2007;116:729–736. doi: 10.1161/CIRCULATIONAHA.107.699934. [DOI] [PubMed] [Google Scholar]
- 18.Blankenship JC, Scott TD, Skelding KA, Haldis TA, Tompkins-Weber K, Sledgen MY, Donegan MA, Buckley JW, Sartorius JA, Hodgson JM, Berger PB. Door-to-balloon times under 90 min can be routinely achieved for patients transferred for ST-segment elevation myocardial infarction percutaneous coronary intervention in a rural setting. J Am Coll Cardiol. 2011;57:272–279. doi: 10.1016/j.jacc.2010.06.056. [DOI] [PubMed] [Google Scholar]
- 19.Peterson ED, Roe MT, Rumsfeld JS, Shaw RE, Brindis RG, Fonarow GC, Cannon CP. A call to ACTION (acute coronary treatment and intervention outcomes network): a national effort to promote timely clinical feedback and support continuous quality improvement for acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2009;2:491–499. doi: 10.1161/CIRCOUTCOMES.108.847145. [DOI] [PubMed] [Google Scholar]
- 20.Jacobs AK, Antman EM, Faxon DP, Gregory T, Solis P. Development of systems of care for ST-elevation myocardial infarction patients: executive summary. Circulation. 2007;116:217–230. doi: 10.1161/CIRCULATIONAHA.107.184043. [DOI] [PubMed] [Google Scholar]
- 21.Nallamothu BK, Normand SL, Wang Y, Hofer TP, Brush JE, Jr, Messenger JC, Bradley EH, Rumsfeld JS, Krumholz HM. Relation between door-to-balloon times and mortality after primary percutaneous coronary intervention over time: a retrospective study. Lancet. 2015;385:1114–1122. doi: 10.1016/S0140-6736(14)61932-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reimer KA, Jennings RB. The “wavefront phenomenon” of myocardial ischemic cell death. II. Transmural progression of necrosis within the framework of ischemic bed size (myocardium at risk) and collateral flow. Lab Invest. 1979;40:633–644. [PubMed] [Google Scholar]
- 23.Newby LK, Rutsch WR, Califf RM, Simoons ML, Aylward PE, Armstrong PW, Woodlief LH, Lee KL, Topol EJ, Van de Werf F. Time from symptom onset to treatment and outcomes after thrombolytic therapy. GUSTO-1 Investigators. J Am Coll Cardiol. 1996;27:1646–1655. doi: 10.1016/0735-1097(96)00053-8. [DOI] [PubMed] [Google Scholar]
- 24.Gersh BJ, Stone GW, White HD, Holmes DR., Jr Pharmacological facilitation of primary percutaneous coronary intervention for acute myocardial infarction: is the slope of the curve the shape of the future? JAMA. 2005;293:979–986. doi: 10.1001/jama.293.8.979. [DOI] [PubMed] [Google Scholar]
- 25.De Luca G, Suryapranata H, Ottervanger JP, Antman EM. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation. 2004;109:1223–1225. doi: 10.1161/01.CIR.0000121424.76486.20. [DOI] [PubMed] [Google Scholar]
- 26.Koul S, Andell P, Martinsson A, Gustav Smith J, van der Pals J, Scherstén F, Jernberg T, Lagerqvist B, Erlinge D. Delay from first medical contact to primary PCI and all-cause mortality: a nationwide study of patients with ST-elevation myocardial infarction. J Am Heart Assoc. 2014;3:e000486. doi: 10.1161/JAHA.113.000486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goldberg RJ, Spencer FA, Fox KA, Brieger D, Steg PG, Gurfinkel E, Dedrick R, Gore JM. Prehospital Delay in Patients With Acute Coronary Syndromes (from the Global Registry of Acute Coronary Events [GRACE]) Am J Cardiol. 2009;103:598–603. doi: 10.1016/j.amjcard.2008.10.038. [DOI] [PubMed] [Google Scholar]
- 28.Nguyen HL, Saczynski JS, Gore JM, Goldberg RJ. Age and sex differences in duration of prehospital delay in patients with acute myocardial infarction: a systematic review. Circ Cardiovasc Qual Outcomes. 2010;3:82–92. doi: 10.1161/CIRCOUTCOMES.109.884361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mathews R, Peterson ED, Li S, Roe MT, Glickman SW, Wiviott SD, Saucedo JF, Antman EM, Jacobs AK, Wang TY. Use of emergency medical service transport among patients with ST-segment-elevation myocardial infarction: findings from the National Cardiovascular Data Registry Acute Coronary Treatment Intervention Outcomes Network Registry-Get With The Guidelines. Circulation. 2011;124:154–163. doi: 10.1161/CIRCULATIONAHA.110.002345. [DOI] [PubMed] [Google Scholar]


