Abstract
Background
The American College of Surgeons Committee on Trauma sets national targets for the accuracy of field trauma triage at ≥ 95% sensitivity and ≥ 65% specificity, yet the cost-effectiveness of realizing these goals is unknown. We evaluated the cost-effectiveness of current field trauma triage practices compared to triage strategies consistent with the national targets.
Study Design
This was a cost-effectiveness analysis using data from 79,937 injured adults transported by 48 emergency medical services (EMS) agencies to 105 trauma and non-trauma hospitals in 6 regions of the Western U.S. from 2006 through 2008. Incremental differences in survival, quality adjusted life years (QALYs), costs, and the incremental cost-effectiveness ratio (ICER; costs per QALY gained) were estimated for each triage strategy over a 1-year and lifetime horizon using a decision analytic Markov model. We considered an ICER threshold of less than $100,000 to be cost-effective.
Results
For these 6 regions, a high sensitivity triage strategy consistent with national trauma policy (sensitivity 98.6%, specificity 17.1%) would cost $1,317,333 per QALY gained, while current triage practices (sensitivity 87.2%, specificity 64.0%) cost $88,000 per QALY gained compared to a moderate sensitivity strategy (sensitivity 71.2%, specificity 66.5%). Refining EMS transport patterns by triage status improved cost-effectiveness. At the trauma system level, a high-sensitivity triage strategy would save 3.7 additional lives per year at a 1-year cost of $8.78 million, while a moderate sensitivity approach would cost 5.2 additional lives and save $781,616 each year.
Conclusions
A high-sensitivity approach to field triage consistent with national trauma policy is not cost effective. The most cost effective approach to field triage appears closely tied to triage specificity and adherence to triage-based EMS transport practices.
INTRODUCTION
Among the 28 million emergency medical services (EMS) responses in the U.S. each year, the most common clinical condition is traumatic injury.1 The decision to transport an injured patient to a major trauma center is guided by national field triage guidelines that were initially developed in 1976 by the American College of Surgeons Committee on Trauma (ACS-COT) and have been periodically updated, most recently in 2011.2,3 The triage guidelines are one of the few clinical aspects of out-of-hospital care supported by a national protocol (jointly sponsored and revised by the Centers for Disease Control and Prevention and ACS-COT), have been widely implemented into EMS and trauma systems throughout the U.S., and are integral to concentrating seriously injured patients in major trauma centers through the 9-1-1 emergency response system.
Important quality metrics for the triage guidelines include under- and over-triage rates, with national benchmarks set by ACS-COT. Under-triage (1 – sensitivity) is the proportion of seriously injured patients transported to non-trauma hospitals, a measure of reduced access to care and potentially worse outcomes4,5 (national target ≤ 5%6). Conversely, over-triage (1 – specificity) represents the proportion of patients without serious injuries transported to major trauma hospitals, a measure of resource waste and excess cost (national target ≤ 35%6). Research suggests that under-triage is as high as 34%7-11 and approximately 50% among older adults.7,10-12 Revisions to the national guidelines have sought to reduce under-triage without increasing over-triage,2 although under- and over-triage are inversely related.13 Achieving the ACS-COT benchmark of 5% under-triage would likely result in major increases in over-triage13 and increased costs.14 Evaluating the balance between health outcomes and costs among injured patients is important in optimizing the “value” of trauma systems in a resource- and cost-constrained environment. Because the survival benefit of major trauma centers appears limited to patients with serious injuries,15-19 transporting low-risk patients to high-resource trauma centers increases costs without clear benefit.14 While previous research has demonstrated some of the cost implications related to field triage practices,14,20 particularly related to differences in the cost of care between different types of hospitals,14,21-23 there have been no formal cost effectiveness analyses of field triage.
We sought to evaluate the cost effectiveness of current U.S. field trauma triage practices compared with two alternative triage strategies meeting the national policy benchmarks: (1) a high sensitivity field triage strategy consistent with the ≥ 95% sensitivity target; and (2) a moderate sensitivity approach to field triage that meets the goal for ≥ 65% specificity. We also examined the cost implications of EMS transport patterns related to the guidelines, interhospital transfers and outcome differences between Levels I versus II trauma centers.
METHODS
Study Design and Setting
We developed a decision-analytic Markov model to compare the costs and outcomes of current field trauma triage practices in these 6 regions with two alternative approaches to field triage meeting national policy benchmarks for sensitivity and specificity (TreeAge Software, Inc., Williamstown, MA). The analytical timeframe lasted from the time of 9-1-1 call until death (life time horizon). The analysis was conducted from the health system payer’s perspective with inclusion of all medical service-related costs, but exclusion of indirect societal costs (e.g., transportation cost, productivity loss, etc.). We used previously collected data from a multi-region retrospective cohort of 79,937 injured patients ≥ 18 years to determine baseline patient characteristics, diagnostic test values of current triage practices in the regions (based on the national field triage guidelines), EMS transport patterns for triage-positive and negative patients, two alternative approaches to field triage (high sensitivity and moderate sensitivity), in-hospital outcomes and acute care costs. Patients included in the cohort were transported by 48 EMS agencies to 105 hospitals (12 Level I, 5 Level II, 3 Level III, 4 Level IV, 1 Level V and 80 community and private hospitals) in 6 urban/suburban regions from January 1, 2006 through December 31, 2008. The regions included: Portland, OR/Vancouver, WA (4 counties); King County, WA; Sacramento, CA (2 counties); San Francisco, CA; Santa Clara, CA (2 counties); and Denver County, CO. The data collection processes and methods used to construct this cohort have been previously described.24 Interhospital transfers were excluded, unless the patient was originally transported by EMS within the defined geographic study regions to a non-trauma hospital and subsequently transferred to a Level I or II hospital. This inclusion strategy allowed us to track all injured patients originating in the study regions and transported by EMS, regardless of subsequent transfer between hospitals.
The primary cost measure was life-long health care cost, starting with the initial EMS transport. The primary health outcome measure was total lifetime quality-adjusted life years (QALYs), with 1-year mortality serving as a secondary health outcome. We measured the cost-effectiveness of each triage strategy using the incremental cost-effectiveness ratio (ICER), defined as the additional cost per QALY gained from the more effective (in terms of higher QALYs) triage strategy. We applied an annual 3% discount rate to both QALYs and costs.25 Institutional Review Boards at all 6 sites approved this protocol and waived the requirement for informed consent. All input parameters discussed in the following sections are listed in Table 1.
Table 1.
Triage Cost Effectiveness Input Parameters: Probabilities, Utilities and Cost Items
| Description | Value (95% CI) | Source | |
|---|---|---|---|
| Probability, % | |||
| Severely injured (ISS≥16) | 6.43 (6.26-6.60) | Cohort data | |
| Algorithm sensitivity (100%,% under triage) | |||
| Current triage | 87.2 (86.3-88.1) | Cohort data | |
| High specificity | 71.2 (70.0-72.5) | Cohort data | |
| High sensitivity | 98.6 (98.3-98.9) | Cohort data | |
| Algorithm specificity (100%, % over triage) | |||
| Current triage | 64.0 (63.7-64.4) | Cohort data | |
| High specificity | 66.5 (66.2-66.9) | Cohort data | |
| High sensitivity | 17.1 (16.9-17.4) | Cohort data | |
| Triage adherence (site transported to) | |||
| If ISS≥16, triage positive | |||
| Level I or II TC | 89.3 (88.4-90.2) | Cohort data | |
| Non TC | 10.7 (9.8-11.6) | Cohort data | |
| If ISS≥16, triage negative | |||
| Level I or II TC | 48.4 (44.6-52.2) | Cohort data | |
| Non TC | 51.6 (47.8-55.4) | Cohort data | |
| If ISS<16, triage positive | |||
| Level I or II TC | 80.2 (79.8-80.7) | Cohort data | |
| Non TC | 19.8 (19.3-20.2) | Cohort data | |
| If ISS<16, triage negative | |||
| Level I or II TC | 34.6 (34.2-35.0) | Cohort data | |
| Non TC | 65.2 (65.0-65.8) | Cohort data | |
| Level 1 among transported to TC | |||
| If ISS≥16, triage positive | 91.7 (90.8-92.5) | Cohort data | |
| If ISS≥16, triage negative | 91.8 (88.3-94.4) | Cohort data | |
| If ISS<16, triage positive | 81.8 (81.3-82.3) | Cohort data | |
| If ISS<16, triage negative | 69.2 (68.5-69.9) | Cohort data | |
| Transfer from non TC to TC | |||
| If ISS≥16 | |||
| If triage positive | 26.5 (22.8-30.6) | Cohort data | |
| If triage negative | 32.5 (27.7-37.6) | Cohort data | |
| If ISS<16 | |||
| If triage positive | 7.4 (6.7-8.1) | Cohort data | |
| If triage negative | 4.3 (4.1-4.6) | Cohort data | |
| In-hospital mortality | |||
| if ISS≥16 | |||
| Treated in level I TC | 10.0 (9.2-10.9) | Cohort data | |
| RR if treated in level II TC15* | 1.00 | Reference 15 | |
| RR if treated in non-TC15 | 1.25 (1.00-1.58) | Reference 14 | |
| If ISS<16 | 1.2 (1.2-1.3) | Cohort data | |
| 1-y Mortality after initial discharge | |||
| If ISS≥16 | |||
| Treated in TC 15 | 3.0 (2.5-3.5) | Reference 15 | |
| RR if treated in non-TC15† | 1.64 (1.08-2.49) | Reference 15 (calculated†) | |
| If ISS<16 51 | 1.7 (1.6-1.8) | Reference 51 | |
| Baseline lifetime mortality after 1-y 36 | age-specific | Reference 36 | |
| Hazard ratios for lifetime mortality 37 | |||
| If ISS≥16 | 5.19 (3.94-6.52) | Reference 37 | |
| If ISS<16 | 1.38 (1.09-1.69) | Reference 37 | |
| Utility | |||
| 1-y quality of life | |||
| If ISS≥16 | |||
| Treated in TC 21 | 0.70 (0.60-0.79) | Reference 21 | |
| Treated in non-TC 21 | 0.68 (0.57-0.78) | Reference 21 | |
| If ISS<1634 | 0.80 (0.66-0.93) | Reference 21 | |
| Yearly decrease in quality of life, % 25 | 3.0 | Reference 25 | |
| Mean adjusted per-patient cost‡ | |||
| Initial treatment14 | |||
| If ISS≥16 | |||
| Level 1 TC | 33,525 (32,724-34,326) | Cohort data, Reference 14 | |
| Level 2 TC | 26,481 (25,161-27,801) | Cohort data, Reference 14 | |
| Non TC, no transfer | 19,889 (18,894-20,884) | Cohort data, Reference 14 | |
| Non TC, transfer | 22,578 (20,908-24,247) | Cohort data, Reference 14 | |
| If ISS<16 | |||
| Level 1 TC | 24,903 (24,370-25,436) | Cohort data, Reference 14 | |
| Level 2 TC | 19,835 (19,453-20,217) | Reference 14 Cohort data, | |
| Non TC, no transfer | 14,255 (13,928-14,582) | Cohort data, Reference 14 | |
| Non TC, transfer | 16,178 (15,685-16,672) | Cohort data, Reference 14 | |
| 1-y Post-injury treatment after discharge | |||
| If ISS≥16 21 | |||
| TC (level 1 and 2, including transfer) | 35,081 (31,509-38,653) | Reference 21 | |
| Non TC | 34,442 (31,230-37,654) | Reference 21 | |
| If ISS<1635,52 | |||
| TC (level 1 and 2, including transfer) | 9,300 (8,300-10,200) | References35,52 | |
| Non TC | 10,400 (9,600-11,300) | References35,52 | |
| % Increase in lifetime healthcare expenditure 42 | |||
| If ISS≥16 | 1.45 (1.10-1.81) | Reference 42 | |
| If ISS<16 | 1.25 (1.02-1.57) | Reference 42 | |
| Yearly decrease in cost, %25 | 3.0 | Reference 25 | |
Level II trauma centers are assumed to have the same mortality reduction as Level I trauma centers. The scenario of lower mortality reduction for Level II trauma centers is tested in a sensitivity analysis.
Relative risk of 1-year mortality for seriously injured (ISS ≥ 16) patients discharged alive from non-trauma centers is calculated based on 20% in-hospital mortality reduction and 25% one-year mortality reduction in major trauma centers, compared to non-trauma centers. Approximate relative risk = ((trauma center in-hospital mortality + trauma center one-year mortality after discharge alive)/(100% - trauma center one-year mortality reduction) − trauma center in-hospital mortality/ (100% - trauma center inhospital mortality)) / trauma center one-year mortality after discharged alive = ((10%+3%)/(100%-25%)-10%/(100%-20%))/3%=1.64. Inaccuracy is due to rounding.
Adjusted to 2008 dollars
RR, relative risk; TC, trauma center; ISS, Injury Severity Score.
Defining Current and Alternative Field Triage Strategies
To define the accuracy of current field triage practices (i.e., actual triage practices by EMS personnel in the 6 regions, based on the national field triage guidelines2,6), we estimated field triage status (positive or negative) using data from the cohort of injured adults transported by EMS. We defined field triage status based on actual application of the national field triage guidelines by EMS providers. At the time of data collection, participating EMS agencies were using the 2006 national triage guidelines,26 with some local retention of field triage criteria included in previous national guidelines.27 To minimize misclassification bias, we determined triage status by triangulating multiple data sources (eMethods in the Appendix).14,28 All other patients were considered triage negative. We defined major trauma centers as all Level I and II trauma hospitals, based on ACS-COT accreditation and state-level designation. EMS transport “adherence” was based on actual ambulance transport patterns within each triage category (positive versus negative), with perfect adherence representing transport of all triage-positive patients to major trauma centers and all triage-negative patients to non-trauma centers.
To develop the two alternative triage algorithms, we used the same cohort of injured patients and classification and regression tree analysis29 (v. 8.2, Salford Systems, San Diego, CA) to generate: (1) a decision tree meeting the national benchmark for sensitivity (≥ 95%; under-triage ≤ 5%); and (2) a decision tree meeting the national benchmark for specificity (≥ 65%; over-triage ≤ 35%) (eMethods, eFigure1 and eFigure 2 in the Appendix).
Model overview and natural history of trauma triage
Our model began with the 9-1-1 call and extended through index hospitalization, including transfers between hospitals. A Markov model was then used to project health outcomes and costs of patients who survived hospitalization to one-year post-injury and until death (Figure 1). Model inputs included: serious injury, measured using the Injury Severity Score (ISS ≥ 16 vs. ISS < 16); EMS transport patterns within triage positive vs. negative groups; interhospital transfer status; costs; and in-hospital mortality (derived from our cohort and existing literature, see Table 1). Model outputs were driven by relative differences in triage probabilities based on the diagnostic test characteristics of current and alternative field triage strategies, as derived from our cohort. We assumed that EMS transport patterns based on triage status would remain the same using each field triage strategy.
Figure 1.
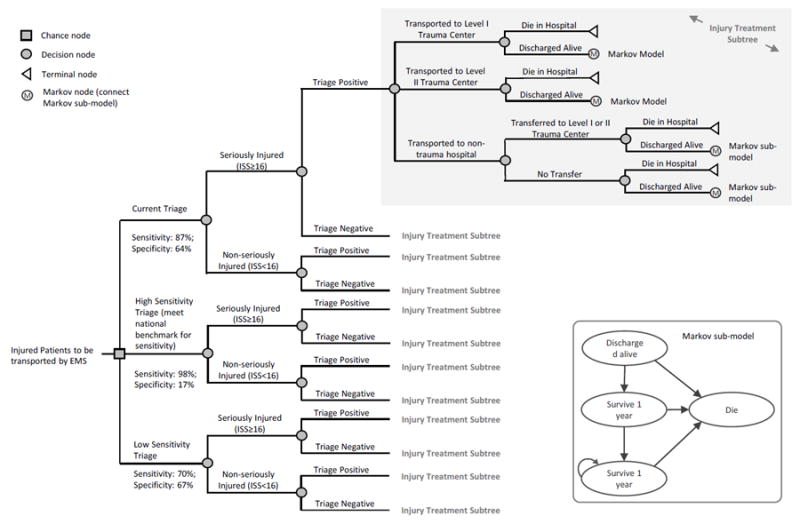
Model schematic of current field triage processes versus two alternative triage strategies. Field triage processes do not involve knowledge about injury severity prior to hospital arrival. The decision tree branch integrating injury severity is included to provide the true prevalance of serious injury in the population, providing the ability to test different prevalance values. However, input parameters were adjusted to evaluate field triage as it is actually practiced, with injury severity unknown by emergency medical service providers at the time of triage.
Health Outcomes
Differences in health outcomes between the three triage strategies were driven by 1-year survival benefits for patients with serious injuries (ISS ≥ 16) treated at major trauma centers using established estimates from the literature to estimate the survival benefit.15 We assumed that seriously injured patients treated at Level I and II hospitals had equivalent survival benefits. While some studies suggest that outcomes between Level I and II hospitals are not identical,30,31 this is not definitively established and certain regions have Level II centers that function similar to Level I centers, particularly when there is no Level I hospital in reasonable proximity.32 We explored this assumption in sensitivity analyses (described below). For patients with ISS < 16, we assumed there was no survival benefit for care at major trauma centers.33 In our base case analysis, we assumed that patients transported directly to major trauma centers had equivalent survival benefits to those transferred to the center from within the same geographic region.15 However, because some research has suggested that seriously injured patients transferred to major trauma centers may have reduced survival compared to direct transports,4,5 we also conducted sensitivity analyses to test this assumption.
To account for differences in quality of life following discharge, we used published utility weights for trauma survivors at one year, stratified by severity of injury.21,34 As applied in previous trauma cost-effectiveness research, we used a Markov model to project incremental differences in lifetime survival beyond 1-year post-injury.35 We used 2008 U.S. life tables to calculate remaining life expectancy,36 with adjustment of mortality rates to account for decreased survival after major trauma, according to a 10-year longitudinal study of trauma victims.37 Quality-adjusted life-years were calculated using the mean observed values of the Short Form-6 Dimension (SF-6D) scale at 1 year post-injury (0.70)21 with decreasing utilities over a lifetime, proportional to differences in SF-6D scores by age reported for the general U.S. population.38
Health Care Costs
We calculated total acute care costs for the decision model using mean, adjusted, composite (macro), patient-level acute care costs from the cohort, according to injury severity and hospital type.14 Acute care costs were based on four sources of expenditures: (1) initial EMS transport; (2) ED care; (3) in-hospital care; and (4) initial ED evaluation and transfer for patients subsequently transferred between hospitals. Similar to previous research, we calculated the per-unit costs of EMS scene transport, interhospital transfer and ED costs for non-admitted patients from a separate sample of injured Medicare fee-for-service patients.14 For admitted patients, we obtained composite, patient-level facility charges through linkage to state discharge databases and trauma registries. We converted charges to costs using hospital- and year-specific cost-to-charge ratios.39,40 We estimated professional fees using a conversion factor (1.27) previously calculated for injured patients using the MarketScan database.21 All costs were adjusted to 2008 U.S. dollars using a region-specific medical consumer price index.41 We adjusted total acute care costs for known confounders using a multivariable generalized linear model with a gamma distribution and log link function.14 These adjusted cost estimates were used as parameters to populate the model (Figure 1 and Table 1). We projected costs from hospital discharge to 1-year post-injury according to injury severity and hospital type using published estimates from the literature.21,35 The Markov model was also used to project lifetime health care costs beyond 1 year according to Centers for Medicare & Medicaid Services age-specific estimates of annual health care expenditures,38,42 adjusted to account for the increased health expenditures of major trauma victims compared with the general U.S. population.42
As a guide for interpreting the analyses, we considered $100,000 per QALY to be the threshold for cost-effectiveness.43 While ICER thresholds of $50,000 to $100,000 per QALY have been used in the U.S. for decades (presumably based on the $50,000 per QALY estimate for dialysis among patients with chronic renal failure43,44), the ICER threshold simply serves as a guide, rather than a determinant for making healthcare spending decisions.44
Sensitivity Analysis
We assessed the robustness of the primary results using four types of sensitivity analyses: alternative scenario analysis, one-way sensitivity analysis, probabilistic sensitivity analysis and input threshold analysis. For alternative scenario analysis, we examined the change in cost, QALYs, and mortality rates for six scenarios concerning three key model assumptions with policy implications: (1) varying EMS transport patterns within each triage strategy; (2) mortality and cost assumptions related to inter-hospital transfer; and (3) survival differences between Level I versus II trauma centers.30,31,45 For the one-way sensitivity analyses, we further explored how cost and mortality vary within each triage strategy in response to changes in EMS transport patterns (Figure 2). For the probabilistic sensitivity analyses, we performed 3,000 second-order Monte Carlo simulation trials that selected values of all input parameters from the ranges according to distributions representing the uncertainty in their estimation. We assigned a specific distribution type and calculated distribution parameters to each input parameter to depict its uncertainty (as listed in eTable 1). The probabilistic sensitivity analyses allowed us to assess the joint uncertainty across all parameters in the model on estimated outcomes, presented as cost-effectiveness acceptability curves at a given threshold of willingness-to-pay. Lastly, for the input threshold analysis, we varied each input parameter by up to +/- 20% of its baseline value, while holding all other parameters constant, in order to examine the impact of change in value of a specific parameter on ICER and choice of the most cost-effective triage strategy.
Figure 2.
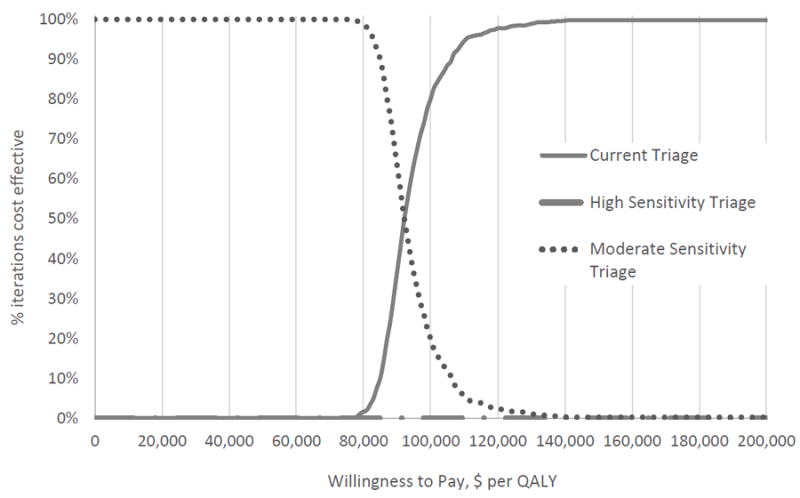
Cost-effectiveness acceptability curves for 3 different field trauma triage strategies among injured adults transported by emergency medical services. The curve shows the probability that a triage strategy is cost-effective across a range of maximum willingness to pay per quality-adjusted life year gained values. The probability is derived from 3,000 rounds of simulation that randomly sampled parameter values from the distributions assigned. The high-sensitivity triage strategy is portrayed at the bottom of the figure along the 0% axis and therefore is not visible. The probability cost effective does not increase from zero for the high sensitivity triage until willingness to pay per quality-adjusted life years is greater than $1,000,000.
RESULTS
Among the cohort of 79,937 injured patients, 5,138 (6.4%) had serious injuries (ISS ≥ 16) and 1,573 (2.0%) died. Among the 5,138 seriously injured patients, 4,481 patients were identified as triage-positive by current triage practices (87.2% sensitivity, 12.8% under-triage). There were 47,899 of 74,799 patients with ISS < 16 identified as triage-negative (64.0% specificity, 36.0% over-triage). For EMS transport practices, 25,590 of 31,381 triage-positive patients (81.6%) were transported to Level I or II trauma centers. Of the 48,556 triage-negative patients, 16,892 (34.8%) were transported to Level I or II trauma centers. The derived, hypothetical, high sensitivity triage algorithm demonstrated 98.6% sensitivity and 17.1% specificity. The derived, hypothetical moderate sensitivity triage algorithm had 71.2% sensitivity and 66.5% specificity. All parameters used to construct the cost model are detailed in Table 1.
Base Case Result
The main results are shown in the base case analysis in Table 2. Using the high sensitivity triage strategy, costs increased and expected 1-year mortality decreased due to a shift of patients to more effective and higher cost trauma centers; the high sensitivity triage strategy would cost $1,317,333 per QALY gained compared to the moderate sensitivity approach. Compared to the moderate sensitivity triage strategy, current triage practices cost $88,000 per QALY gained. Adopting a triage strategy favoring a reduction in over-triage (moderate sensitivity) would be cost-saving relative to current triage practices, but would yield higher 1-year mortality rates. Based on a willingness to pay threshold of $100,000 per QALY gained, current field triage was the preferred field triage strategy. However, at lower ICER thresholds (e.g., $50,000 per QALY gained), the moderate sensitivity approach was favored. A high-sensitivity strategy for field triage was not cost-effective.
Table 2.
Base Case Result and per Patient Scenario Analyses: Expected Cost, Quality-Adjusted Life Years and Mortality per Injured Patient Transported by Emergency Medical Service for the 3 Field Triage Scenarios
| Expected lifetime cost | Incremental cost per patient | Expected lifetime QALYs gained | Incremental QALY gained per patient | ICER ($ per QALY)* | Expected1-y mortality, absolute % | Incremental mortality reduction up to 1 y, % | |
|---|---|---|---|---|---|---|---|
| Base case analysis | |||||||
| Moderate Sensitivity | 317,318 | N/A | 12.6586 | N/A | 3.5530 | ||
| Current Triage | 317,494 | 176 | 12.6606 | 0.002 | 88,000 | 3.5417 | -0.0113 |
| High Sensitivity | 319,470 | 1,976 | 12.6621 | 0.0015 | 1,317,333 | 3.5334 | -0.0083 |
| Scenario 1: Perfect adherence for triage-positive patients (all triage- positive patients are transported to Level I or II trauma centers) | |||||||
| Moderate Sensitivity | 317,967 | N/A | 12.6611 | N/A | 3.5383 | ||
| Current Triage | 318,205 | 238 | 12.6637 | 0.0026 | 91,538 | 3.5237 | -0.0147 |
| High Sensitivity | 320,977 | 2,772 | 12.6655 | 0.0018 | 1,540,000 | 3.5132 | -0.0105 |
| Scenario 2: Perfect adherence for triage-negative patients (all triage- negative patients are transported to non-trauma hospitals) | |||||||
| Moderate Sensitivity | 315,339 | N/A | 12.6542 | N/A | 3.5779 | ||
| Current Triage | 315,672 | 333 | 12.6587 | 0.0045 | 74,000 | 3.5528 | -0.0251 |
| High Sensitivity | 318,994 | 3,322 | 12.6619 | 0.0032 | 1,038,125 | 3.5348 | -0.0179 |
| Scenario 3: Perfect adherence for triage-positive and triage-negative patients. | |||||||
| Moderate Sensitivity | 315,988 | N/A | 12.6567 | N/A | 3.5632 | ||
| Current Triage | 316,383 | 395 | 12.6617 | 0.0050 | 79,000 | 3.5347 | -0.0285 |
| High Sensitivity | 320,502 | 4,119 | 12.6653 | 0.0036 | 1,144,167 | 3.5144 | -0.0203 |
| Scenario 4: No survival benefit and no higher initial treatment cost for patients transferred from non-trauma centers to Level I or II centers. | |||||||
| Moderate Sensitivity | 317,229 | N/A | 12.6568 | N/A | 3.5711 | ||
| Current Triage | 317,421 | 192 | 12.6594 | 0.0026 | 73,846 | 3.5539 | -0.0172 |
| High Sensitivity | 319,419 | 1,998 | 12.6613 | 0.0019 | 1,051,579 | 3.5416 | -0.0123 |
| Scenario 5: No survival benefit for patients transferred from a non-trauma hospital to a Level I or II trauma center, but higher initial treatment cost, as in base case analysis. | |||||||
| Moderate Sensitivity | 317,297 | N/A | 12.6575 | N/A | 3.5712 | ||
| Current Triage | 317,480 | 183 | 12.6599 | 0.0024 | 76,250 | 3.554 | -0.0172 |
| High Sensitivity | 319,460 | 1,980 | 12.6616 | 0.0015 | 1,320,000 | 3.5416 | -0.0124 |
| Scenario 6: Lower mortality benefit among level II trauma centers compared to Level I centers (half of in- hospital and 1-y mortality reduction) | |||||||
| Moderate Sensitivity | 317,232 | N/A | 12.6580 | N/A | 3.5585 | ||
| Current Triage | 317,403 | 183 | 12.6598 | 0.0018 | 101,667 | 3.5474 | -0.0111 |
| High Sensitivity | 319,376 | 1980 | 12.6611 | 0.0015 | 1,320,000 | 3.5395 | -0.0079 |
‘Incremental’ values are the difference compared with the next less costly scenario (ie, the row above).
ICER equals incremental cost divided by incremental QALY.
QALY, quality-adjusted life years; ICER, incremental cost-effectiveness ratio.
Sensitivity Analyses
We evaluated several scenario analyses to investigate the influence of potentially modifiable aspects of trauma systems on cost-effectiveness (Table 2). For EMS transport patterns (Scenarios 1, 2 and 3), transporting all triage-negative patients to non-trauma hospitals yielded the most cost-effective approach (ICER $74,000, Scenario 2). However, perfect EMS adherence for both triage groups generated the greatest mortality reduction at 1-year, with an ICER of $79,000 (Scenario 3). We explored the influence of varying EMS transport patterns on mortality and costs for each field triage strategy in one-way sensitivity analyses (eFigures 3A and 3B). Greater transport of triage-negative patients to non-trauma hospitals (i.e., a lower proportion of triage-negative patients transported to Level I or II trauma centers) would cost less with less mortality reduction. Greater transport of triage-positive patients directly to Level I or II trauma centers would cost more, but yield greater mortality reduction.
The influence of survival assumptions and cost implications of inter-hospital transfers are demonstrated in Scenarios 4 and 5. Loss of survival benefit for inter-hospital transfer patients coming from non-trauma centers increased expected 1-year mortality, however transfers did not have major impact on the cost-effectiveness of field triage (likely because the number of transfers from within the designated geographic regions was relatively small). When the survival benefit of Level II hospitals was reduced compared to Level I hospitals, mortality increased and the cost-effectiveness of field triage worsened (Scenario 6).
Results from the probabilistic sensitivity analysis are demonstrated in Figure 2. At a willingness-to-pay threshold of zero to $80,000 per QALY, the moderate sensitivity triage strategy was favored as being cost-effective (>99% of the 3,000 simulation trials). However, current triage practices became the cost-effective choice after the willingness-to-pay threshold rose above $90,000 per QALY gained. The high sensitivity strategy was not cost-effective until willingness to pay exceeded $1,000,000 per QALY gained.
Lastly, the input threshold analysis (eFigure 4 in the Appendix) demonstrated current field triage practices for the 6 regions to be the most cost-effective strategy at a willingness-to-pay threshold of $100,000 per QALY gain across variations in parameter input values. However, there were some important exceptions. For example, if the sensitivity of current triage practices decreased from the baseline of 87.2% to 83.7% without improvement in specificity, the moderate sensitivity triage strategy became the most cost-effective choice.
1-year Impact at the Trauma System Level
In Figure 3, we illustrate the potential impact of the three field triage strategies using costs and additional lives saved at 1-year (these figures do not include survival or costs beyond 1-year, nor do they include a quality of life measurement). Calculated at the trauma system level, the high sensitivity triage strategy would cost an additional $8.78 million to save an additional 3.7 lives per year, compared to current triage practices. The moderate sensitivity triage strategy would result in an additional 5.2 lives lost with 1-year savings of $781,616.
Figure 3.
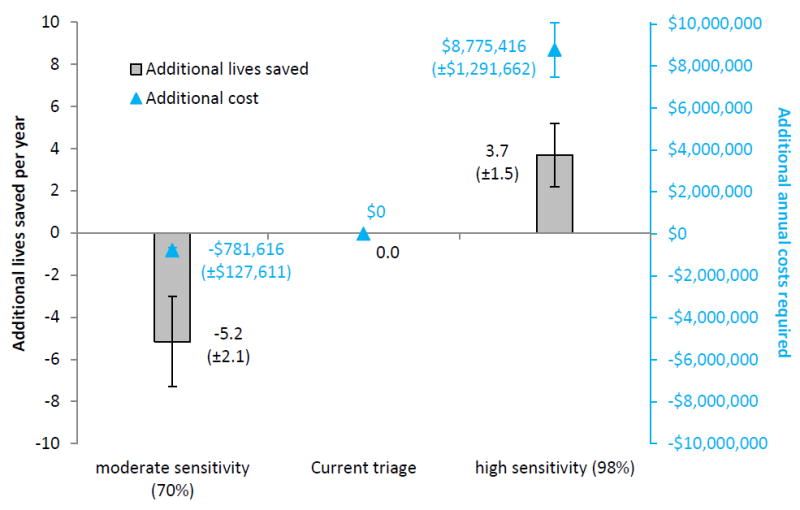
The estimated annual impact of 3 approaches to field trauma triage at the trauma system level, estimated at 1-year post-injury. The standard deviation of each estimate is derived from 3,000 rounds of simulation with input parameters sampled from the designated distribution. To generate estimates at the trauma system level, we averaged the total number of injured patients transported by emergency medical services, deaths and costs across the 6 regional trauma systems included in the cohort. We used decision analytic modeling to generate estimates and 95% confidence intervals.
DISCUSSION
This study represents the first cost effectiveness analysis of field trauma triage. We demonstrate that efforts to revise the national triage guidelines to meet the national benchmark for sensitivity (under-triage ≤ 5%) are likely to be expensive and not cost-effective, mainly due to the large requisite decrease in specificity (increased over-triage). We also show that while a moderate sensitivity (and higher specificity) approach may be cost saving, it would lead to higher trauma mortality with only marginal impact on healthcare spending. While current triage practices in these regions appeared to be the most cost effective strategy at a willingness to pay threshold of $100,000/QALY, they were not cost effective at lower thresholds. The optimal triage strategy for cost effectiveness appears closely tied to specificity and over-triage. Refining EMS transport patterns based on triage status (i.e., transporting all triage-positive patients to Level I/II trauma centers and all triage-negative patients to non-trauma centers) offers an opportunity to further improve the cost-effectiveness of field triage, as does maximizing the survival benefit of Level II trauma centers. These findings suggest an opportunity to align national trauma policy and local EMS implementation of field triage protocols with cost and outcome information to further improve the value of trauma systems. The results also illustrate the importance of specificity in field triage – reductions in under-triage are only likely to be cost-effective if over-triage is constrained.
Minimizing the under-triage of seriously injured patients to non-trauma hospitals has been a laudable goal of trauma systems for decades. However, this focus has not always been balanced with a clear understanding of the cost implications. Meeting the national goal for under-triage through revised field triage practices would require large shifts in the volume of patients sent to major trauma centers.13 Our results demonstrate that using solely field triage practices to resolve discrepancies in under-triage would not be cost effective. While selecting a single value to determine what is or is not cost-effective is difficult,43,44 the ICER for the high-sensitivity triage strategy was well above all thresholds previously used or suggested for determining cost-effectiveness. To further improve the cost effectiveness of field triage, efforts to increase sensitivity require approaches that do not sacrifice specificity. Such approaches might include scalable, out-of-hospital diagnostic methods to better identify seriously injured patients (e.g., additional physiologic markers and monitoring, point-of-care biomarkers and other field-based rapid diagnostic tests). Finally, determining the degree to which over-triage can be allowed to increase (in exchange for reduced under-triage) and still remain cost-effective would be especially helpful. While over-triage does not harm trauma centers (and may be beneficial in generating revenue for these hospitals), over-triage increases healthcare costs without measureable benefit.
Our results also provide important insight into the modifiable aspects of field triage that may help improve the efficiency and value of trauma systems. Trauma triage is a multi-step, sequential process that involves: (1) field identification of high-risk patients; (2) selection of an appropriate destination hospital; and (3) use of inter-hospital transfer to further concentrate high-risk patients in major trauma centers (including patients missed by #1 and #2). We show that focusing entirely on the field triage guidelines to concentrate seriously injured patients in major trauma centers ignores other important aspects of the triage process. Selection of a receiving hospital, optimizing inter-hospital transfer processes and assuring equivalent outcome benefits at Level I and II trauma centers all play roles in maximizing the cost-effectiveness of field triage.
There are multiple policy implications for EMS and trauma systems from our findings. First, it may be prudent to consider cost implications related to the national benchmarks to integrate the concept of “value” to the optimization of trauma systems. Next, encouraging guideline-driven EMS transport protocols based on field triage status may further reduce mortality and improve the cost-effectiveness of field triage. Also, with research suggesting that the outcome benefit of Level II hospitals decreases when in close proximity to Level I centers32 and that trauma center volume is associated with outcomes,46,47 communities should closely review the number and proximity of high-resource trauma hospitals relative to population needs. Our results also imply that having multiple levels of hospital care within a system is important in maximizing value in the system.
We used a retrospective cohort to generate the primary inputs for this project, which may be subject to unmeasured confounding and bias. Because some research has demonstrated higher estimates for under-triage than used for this study,10,11 unbiased prospectively-derived values for under- and over-triage would further inform the cost models and may shift the cost-effectiveness results. We also assumed that EMS transport patterns based on triage status would remain the same under different triage strategies, though it is possible that these patterns would shift based on the perceived accuracy (or lack thereof) of “new” triage guidelines. In addition, our sample did not include distance and proximity information related to major trauma centers (e.g., a triage-negative patient being closer to a major trauma center than to other hospitals), which can also affect hospital selection by EMS. Strategies to increase the diagnostic yield of field triage (i.e., point-of-care biomarker assays, more accurate physiological measures) that increase sensitivity without a concurrent drop in specificity may also shift the cost-effectiveness of a high-sensitivity triage strategy. Finally, the sites included in the study represent urban and suburban regions in the Western U.S. Our findings may not generalize to other regions of the U.S. or rural/frontier areas without proximity to a major trauma center.
We used a primary health outcome of mortality, which is a relatively crude measure that has been criticized in previous cost-effectiveness analyses in trauma.48 While mortality is a well-known and commonly-utilized metric in trauma systems, there may be other potential benefits of trauma center care (e.g., functional outcomes, fewer missed diagnoses and less complications) that have not been well-characterized and therefore were not represented in this analysis. We also assumed that the primary benefit of trauma centers is limited to patients with serious injuries. While this assumption is well-supported by previous literature,15,16,33 it is possible that the benefits of trauma centers may extend to less seriously injured patients.
Finally, due to the complexity of the decision model and uncertainty about the benefit of trauma centers among older adults,15,49 we did not integrate age into the decision analysis. If the survival benefit of major trauma centers is less among older adults15 or if major trauma care improves outcomes of certain older adults without regard to injury severity,50 then the cost-effectiveness of field triage could further shift.
In summary, a field triage strategy meeting the national benchmark for sensitivity was not cost-effective. Current triage practices in the 6 regions were the most cost-effective strategy at an ICER threshold of $100,000/QALY gained, but were not cost effective at lower thresholds. The cost-effectiveness of field triage appears closely tied to specificity and over-triage. Guideline-driven EMS transport patterns following triage assessment would further reduce mortality and costs, thereby enhancing the cost effectiveness of field triage, as would attention to the distribution and role of different hospitals in trauma systems.
Supplementary Material
eMethods: Categorization of field triage status and development of alternative field triage strategies.
eFigure 1. Hypothetical high-sensitivity field triage guidelines. For rule derivation, crossvalidation estimates of sensitivity and specificity were 96.6% and 23.4%, respectively. In the validation cohort, the sensitivity and specificity were 98.6% and 17.1%, respectively (validation estimates were used for the cost-effectiveness models).
eFigure 2. Hypothetical low-sensitivity field triage guidelines. For rule derivation, crossvalidation estimates of sensitivity and specificity were 54.2% and 80.7%, respectively. In the validation cohort, the sensitivity and specificity were 71.2% and 66.5%, respectively (validation estimates were used for the cost-effectiveness models).
eFigure 3. The impact of emergency medical service (EMS) transport patterns on cost and mortality, based on triage status. (A) Patients not meeting triage guidelines (triage-negative). (B) Patients meeting the triage guidelines (triage-positive). We evaluated EMS transport patterns for triage-positive and triage-negative patients, regardless of injury severity (which is unknown at the time of triage). For triage-negative patients, perfect transport adherence represents 0% transport to Level I and II trauma hospitals (baseline 34.8%). For triage-positive patients, perfect adherence represents 100% transport to Level I and II trauma centers (baseline 81.6%). In the figures, adherence is varied across a range of 60% (above and below current baseline) separately for triage-positive and negative patients to demonstrate the potential cost and mortality impact across a variety of scenarios. All changes were measured against the cost and mortality of current triage at baseline adherence. Change in costs (black) is on left y-axis; change in mortality (blue) is on right y-axis. Current triage, high sensitivity triage, and moderate sensitivity triage are shown as solid, dotted, dashed lines, respectively.
eFigure 4. One-way sensitivity analysis for all model parameters in the field triage decisionanalytic model. The figure shows how the cost-effectiveness results for each triage scenario change in response to variation in parameter values. The most cost-effective triage scenario is the one yielding the highest amount of QALY at an incremental cost-effectiveness ratio (ICER) below the common threshold of $100,000 per QALY. Parameters are varied by ±20% from baseline (e.g., percentage of ISS≥16 is varied from 5.14% [6.43%*0.8] to 7.72% [6.43%*1.2]) one at a time with other parameters held at their baseline value. Variation for probability parameters is bound within 0% to 100%.
eTable 1. Input parameter distributions for sensitivity analysis.
Acknowledgments
We acknowledge and thank all the participating EMS agencies, EMS medical directors, trauma registrars, and state offices that supported and helped provide data for this project.
Support: This project was supported by the Robert Wood Johnson Foundation Physician Faculty Scholars Program; the Oregon Clinical and Translational Research Institute (grant #UL1 RR024140); NHLBI Career Development Program in Emergency Care Research (Delgado – K12HL109009); UC Davis Clinical and Translational Science Center (grant #UL1 RR024146); Stanford Center for Clinical and Translational Education and Research (grant #1UL1 RR025744); University of Utah Center for Clinical and Translational Science (grant #UL1-RR025764 and C06-RR11234); and UCSF Clinical and Translational Science Institute (grant #UL1 RR024131). All Clinical and Translational Science Awards are from the National Center for Research Resources, a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research.
Footnotes
Disclosure Information: Nothing to disclose.
Disclaimer: The sponsors were not involved in the design and conduct of the study; collection, management, analysis, or interpretation of the data; preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
Abstract presented at the Society for Academic Emergency Medicine Annual Meeting, San Diego, CA, May 2015.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Zhuo Yang, Email: zhuoyang@live.com.
Daniel Nishijima, Email: daniel.nishijima@ucdmc.ucdavis.edu.
K John McConnell, Email: mcconnjo@ohsu.edu.
Stacy Trent, Email: Stacy.Trent@dhha.org.
James F Holmes, Email: jhholmes@ucdavis.edu.
Mohamud Daya, Email: dayam@ohsu.edu.
N Clay Mann, Email: Clay.Mann@hsc.utah.edu.
Renee Y Hsia, Email: rhsia@sfghed.ucsf.edu.
Tom Rea, Email: rea123@u.washington.edu.
N Ewen Wang, Email: ewen@stanford.edu.
Kristan Staudenmayer, Email: kristans@stanford.edu.
M Kit Delgado, Email: kit.delgado@uphs.upenn.edu.
References
- 1.Wang HE, Mann NC, Jacobson KE, et al. National characteristics of emergency medical services responses in the United States. Prehosp Emerg Care. 2013;17:8–14. doi: 10.3109/10903127.2012.722178. [DOI] [PubMed] [Google Scholar]
- 2.Sasser SM, Hunt RC, Faul M, et al. MMWR Recommendations and reports : Morbidity and mortality weekly report. RR-1. Vol. 61. Recommendations and reports / Centers for Disease Control; Jan 13, 2012. Guidelines for field triage of injured patients: recommendations of the National Expert Panel on Field Triage, 2011; pp. 1–20. [PubMed] [Google Scholar]
- 3.Mackersie RC. History of trauma field triage development and the American College of Surgeons criteria. Prehosp Emerg Care. 2006;10:287–294. doi: 10.1080/10903120600721636. [DOI] [PubMed] [Google Scholar]
- 4.Haas B, Gomez D, Zagorski B, et al. Survival of the fittest: the hidden cost of undertriage of major trauma. J Am Coll Surg. 2010;211:804–811. doi: 10.1016/j.jamcollsurg.2010.08.014. [DOI] [PubMed] [Google Scholar]
- 5.Haas B, Stukel TA, Gomez D, et al. The mortality benefit of direct trauma center transport in a regional trauma system: a population-based analysis. J Trauma Acute Care Surg. 2012;72:1510–1515. doi: 10.1097/TA.0b013e318252510a. discussion 1515-1517. [DOI] [PubMed] [Google Scholar]
- 6.American College of Surgeons. 6. 2014. Resources for Optimal Care of the Injured Patient. [Google Scholar]
- 7.Nakamura Y, Daya M, Bulger EM, et al. Evaluating age in the field triage of injured persons. Ann Emerg Med. 2012;60:335–345. doi: 10.1016/j.annemergmed.2012.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hsia RY, Wang E, Torres H, et al. Disparities in trauma center access despite increasing utilization: data from California, 1999 to 2006. J Trauma. 2010;68:217–224. doi: 10.1097/TA.0b013e3181a0e66d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vassar MJ, Holcroft JJ, Knudson MM, Kizer KW. Fractures in access to and assessment of trauma systems. J Am Coll Surg. 2003;197:717–725. doi: 10.1016/S1072-7515(03)00749-X. [DOI] [PubMed] [Google Scholar]
- 10.Xiang H, Wheeler KK, Groner JI, et al. Undertriage of major trauma patients in the US emergency departments. Am J Emerg Med. 2014;32:997–1004. doi: 10.1016/j.ajem.2014.05.038. [DOI] [PubMed] [Google Scholar]
- 11.Newgard CD, Fu R, Zive D, et al. Prospective validation of the National Field Triage Guidelines for Identifying Seriously Injured Persons. J Am Coll Surg. 2015 doi: 10.1016/j.jamcollsurg.2015.10.016. epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chang DC, Bass RR, Cornwell EE, Mackenzie EJ. Undertriage of elderly trauma patients to state-designated trauma centers. Arch Surg. 2008;143:776–781. doi: 10.1001/archsurg.143.8.776. discussion 782. [DOI] [PubMed] [Google Scholar]
- 13.Newgard CD, Hsia RY, Mann NC, et al. The trade-offs in field trauma triage: a multiregion assessment of accuracy metrics and volume shifts associated with different triage strategies. J Trauma Acute Care Surg. 2013;74:1298–1306. doi: 10.1097/TA.0b013e31828b7848. discussion 1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Newgard CD, Staudenmayer K, Hsia RY, et al. The cost of overtriage: more than one-third of low-risk injured patients were taken to major trauma centers. Health Aff (Millwood) 2013;32:1591–1599. doi: 10.1377/hlthaff.2012.1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354:366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 16.Mullins RJ, Veum-Stone J, Helfand M, et al. Outcome of hospitalized injured patients after institution of a trauma system in an urban area. JAMA. 1994;271:1919–1924. doi: 10.1001/jama.1994.03510480043032. [DOI] [PubMed] [Google Scholar]
- 17.Sampalis JS, Denis R, Lavoie A, et al. Trauma care regionalization: a process-outcome evaluation. J Trauma. 1999;46:565–579. doi: 10.1097/00005373-199904000-00004. discussion 579-581. [DOI] [PubMed] [Google Scholar]
- 18.Pracht EE, Tepas JJ, 3rd, Celso BG, et al. Survival advantage associated with treatment of injury at designated trauma centers: a bivariate probit model with instrumental variables. Med Care Res Rev. 2007;64:83–97. doi: 10.1177/1077558706296241. [DOI] [PubMed] [Google Scholar]
- 19.Nathens AB, Jurkovich GJ, Rivara FP, Maier RV. Effectiveness of state trauma systems in reducing injury-related mortality: a national evaluation. J Trauma. 2000;48:25–30. doi: 10.1097/00005373-200001000-00005. discussion 30-21. [DOI] [PubMed] [Google Scholar]
- 20.Faul M, Wald MM, Sullivent EE, et al. Large cost savings realized from the 2006 Field Triage Guideline: reduction in overtriage in U.S. trauma centers. Prehosp Emerg Care. 2012;16:222–229. doi: 10.3109/10903127.2011.615013. [DOI] [PubMed] [Google Scholar]
- 21.MacKenzie EJ, Weir S, Rivara FP, et al. The value of trauma center care. J Trauma. 2010;69:1–10. doi: 10.1097/TA.0b013e3181e03a21. [DOI] [PubMed] [Google Scholar]
- 22.Goldfarb MG, Bazzoli GJ, Coffey RM. Trauma systems and the costs of trauma care. Health Serv Res. 1996;31:71–95. [PMC free article] [PubMed] [Google Scholar]
- 23.Durham R, Pracht E, Orban B, et al. Evaluation of a mature trauma system. Ann Surg. 2006;243:775–783. doi: 10.1097/01.sla.0000219644.52926.f1. discussion 783-775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Newgard C, Malveau S, Staudenmayer K, et al. Evaluating the use of existing data sources, probabilistic linkage, and multiple imputation to build population-based injury databases across phases of trauma care. Acad Emerg Med. 2012;19:469–480. doi: 10.1111/j.1553-2712.2012.01324.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Weinstein MC, Siegel JE, Gold MR, et al. Recommendations of the Panel on Cost-effectiveness in Health and Medicine. JAMA. 1996;276:1253–1258. [PubMed] [Google Scholar]
- 26.Sasser SM, Hunt RC, Sullivent EE, et al. MMWR Recommendations and reports : Morbidity and mortality weekly report. RR-1. Vol. 58. Recommendations and reports / Centers for Disease Control; Jan 23, 2009. Guidelines for field triage of injured patients. Recommendations of the National Expert Panel on Field Triage; pp. 1–35. [PubMed] [Google Scholar]
- 27.Barnett AS, Wang NE, Sahni R, et al. Variation in prehospital use and uptake of the national Field Triage Decision Scheme. Prehosp Emerg Care. 2013;17:135–148. doi: 10.3109/10903127.2012.749966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Newgard CD, Zive D, Holmes JF, et al. A multisite assessment of the American College of Surgeons Committee on Trauma field triage decision scheme for identifying seriously injured children and adults. J Am Coll Surg. 2011;213:709–721. doi: 10.1016/j.jamcollsurg.2011.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Breiman L, F J, Stone CJ, Olshen RA. Classification and regression trees. New York: Chapman and Hall; 1984. [Google Scholar]
- 30.Cudnik MT, Newgard CD, Sayre MR, Steinberg SM. Level I versus Level II trauma centers: an outcomes-based assessment. J Trauma. 2009;66:1321–1326. doi: 10.1097/TA.0b013e3181929e2b. [DOI] [PubMed] [Google Scholar]
- 31.McConnell KJ, Newgard CD, Mullins RJ, et al. Mortality benefit of transfer to level I versus level II trauma centers for head-injured patients. Health Serv Res. 2005;40:435–457. doi: 10.1111/j.1475-6773.2005.00366.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Haas B, Gomez D, Neal M, et al. Good neighbors? The effect of a level 1 trauma center on the performance of nearby level 2 trauma centers. Ann Surg. 2011;253:992–995. doi: 10.1097/SLA.0b013e3182122346. [DOI] [PubMed] [Google Scholar]
- 33.Zocchi MS, Hsia RY, Carr BG, et al. Comparison of mortality and costs at trauma and nontrauma centers for minor and moderately severe injuries in California. Ann Emerg Med. 2015 May 23; doi: 10.1016/j.annemergmed.2015.04.021. [DOI] [PubMed] [Google Scholar]
- 34.Polinder S, Haagsma JA, Belt E, et al. A systematic review of studies measuring health-related quality of life of general injury populations. BMC Public Health. 2010;10:783. doi: 10.1186/1471-2458-10-783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Delgado MK, Staudenmayer KL, Wang NE, et al. Cost-effectiveness of helicopter versus ground emergency medical services for trauma scene transport in the United States. Ann Emerg Med. 2013;62:351–364. e319. doi: 10.1016/j.annemergmed.2013.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Arias E. National vital statistics reports. 3. Vol. 61. Hyattsville, MD: National Center for Health Statistics; 2012. United States life tables, 2008; pp. 1–63. [PubMed] [Google Scholar]
- 37.Cameron CM, Purdie DM, Kliewer EV, McClure RJ. Long-term mortality following trauma: 10 year follow-up in a population-based sample of injured adults. J Trauma. 2005;59:639–646. [PubMed] [Google Scholar]
- 38.Hanmer J, Lawrence WF, Anderson JP, et al. Report of nationally representative values for the noninstitutionalized US adult population for 7 health-related quality-of-life scores. Medical Decision Making. 2006;26:391–400. doi: 10.1177/0272989X06290497. [DOI] [PubMed] [Google Scholar]
- 39.Bazzoli GJ, Kang R, Hasnain-Wynia R, Lindrooth RC. An update on safety-net hospitals: coping with the late 1990s and early 2000s. Health Aff (Millwood) 2005;24:1047–1056. doi: 10.1377/hlthaff.24.4.1047. [DOI] [PubMed] [Google Scholar]
- 40.Corso P, Finkelstein E, Miller T, et al. Incidence and lifetime costs of injuries in the United States. Inj Prev. 2006;12:212–218. doi: 10.1136/ip.2005.010983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Phillips JA, Buchman TG. Optimizing prehospital triage criteria for trauma team alerts. J Trauma. 1993;34:127–132. doi: 10.1097/00005373-199301000-00024. [DOI] [PubMed] [Google Scholar]
- 42.Cameron CM, Purdie DM, Kliewer EV, McClure RJ. Ten-year health service use outcomes in a population-based cohort of 21,000 injured adults: the Manitoba injury outcome study. Bull World Health Org. 2006;84:802–810. doi: 10.2471/blt.06.030833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Neumann PJ, Cohen JT, Weinstein MC. Updating cost-effectiveness--the curious resilience of the $50,000-per-QALY threshold. N Engl J Med. 2014;371:796–797. doi: 10.1056/NEJMp1405158. [DOI] [PubMed] [Google Scholar]
- 44.Ubel PA, Hirth RA, Chernew ME, Fendrick AM. What is the price of life and why doesn’t it increase at the rate of inflation? Arch Intern Med. 2003;163:1637–1641. doi: 10.1001/archinte.163.14.1637. [DOI] [PubMed] [Google Scholar]
- 45.Demetriades D, Martin M, Salim A, et al. Relationship between American College of Surgeons trauma center designation and mortality in patients with severe trauma (injury severity score > 15) J Am Coll Surg. 2006;202:212–215. doi: 10.1016/j.jamcollsurg.2005.09.027. quiz A245. [DOI] [PubMed] [Google Scholar]
- 46.Minei JP, Fabian TC, Guffey DM, et al. Increased trauma center volume is associated with improved survival after severe injury: results of a Resuscitation Outcomes Consortium study. Ann Surg. 2014;260:456–464. doi: 10.1097/SLA.0000000000000873. discussion 464-455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nathens AB, Jurkovich GJ, Maier RV, et al. Relationship between trauma center volume and outcomes. JAMA. 2001;285:1164–1171. doi: 10.1001/jama.285.9.1164. [DOI] [PubMed] [Google Scholar]
- 48.Stratton SJ. Should helicopters dispatched for EMS trauma response be grounded? Ann Emerg Med. 2013;62:365–366. doi: 10.1016/j.annemergmed.2013.04.003. [DOI] [PubMed] [Google Scholar]
- 49.Pracht EE, Langland-Orban B, Flint L. Survival advantage for elderly trauma patients treated in a designated trauma center. J Trauma. 2011;71:69–77. doi: 10.1097/TA.0b013e31820e82b7. [DOI] [PubMed] [Google Scholar]
- 50.Goodmanson NW, Rosengart MR, Barnato AE, et al. Defining geriatric trauma: when does age make a difference? Surgery. 2012;152:668–674. doi: 10.1016/j.surg.2012.08.017. discussion 674-665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Davidson GH, Hamlat CA, Rivara FP, et al. Long-term survival of adult trauma patients. JAMA. 2011;305:1001–1007. doi: 10.1001/jama.2011.259. [DOI] [PubMed] [Google Scholar]
- 52.Davis KL, Joshi AV, Tortella BJ, Candrilli SD. The direct economic burden of blunt and penetrating trauma in a managed care population. J Trauma. 2007;62:622–629. doi: 10.1097/TA.0b013e318031afe3. discussion 629-630. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods: Categorization of field triage status and development of alternative field triage strategies.
eFigure 1. Hypothetical high-sensitivity field triage guidelines. For rule derivation, crossvalidation estimates of sensitivity and specificity were 96.6% and 23.4%, respectively. In the validation cohort, the sensitivity and specificity were 98.6% and 17.1%, respectively (validation estimates were used for the cost-effectiveness models).
eFigure 2. Hypothetical low-sensitivity field triage guidelines. For rule derivation, crossvalidation estimates of sensitivity and specificity were 54.2% and 80.7%, respectively. In the validation cohort, the sensitivity and specificity were 71.2% and 66.5%, respectively (validation estimates were used for the cost-effectiveness models).
eFigure 3. The impact of emergency medical service (EMS) transport patterns on cost and mortality, based on triage status. (A) Patients not meeting triage guidelines (triage-negative). (B) Patients meeting the triage guidelines (triage-positive). We evaluated EMS transport patterns for triage-positive and triage-negative patients, regardless of injury severity (which is unknown at the time of triage). For triage-negative patients, perfect transport adherence represents 0% transport to Level I and II trauma hospitals (baseline 34.8%). For triage-positive patients, perfect adherence represents 100% transport to Level I and II trauma centers (baseline 81.6%). In the figures, adherence is varied across a range of 60% (above and below current baseline) separately for triage-positive and negative patients to demonstrate the potential cost and mortality impact across a variety of scenarios. All changes were measured against the cost and mortality of current triage at baseline adherence. Change in costs (black) is on left y-axis; change in mortality (blue) is on right y-axis. Current triage, high sensitivity triage, and moderate sensitivity triage are shown as solid, dotted, dashed lines, respectively.
eFigure 4. One-way sensitivity analysis for all model parameters in the field triage decisionanalytic model. The figure shows how the cost-effectiveness results for each triage scenario change in response to variation in parameter values. The most cost-effective triage scenario is the one yielding the highest amount of QALY at an incremental cost-effectiveness ratio (ICER) below the common threshold of $100,000 per QALY. Parameters are varied by ±20% from baseline (e.g., percentage of ISS≥16 is varied from 5.14% [6.43%*0.8] to 7.72% [6.43%*1.2]) one at a time with other parameters held at their baseline value. Variation for probability parameters is bound within 0% to 100%.
eTable 1. Input parameter distributions for sensitivity analysis.


