Abstract
BACKGROUND
There is a need for continued surveillance of diabetes-related functional disability. We examined associations between diabetes, hyperglycemia, and the burden of functional disability in a community-based population.
METHODS
We conducted a cross-sectional analysis of 5,035 participants who attended visit 5 (2011–2013) of the Atherosclerosis Risk in Communities study. Functional disability was dichotomously defined by any self-reported difficulty performing 12 tasks essential to independent living grouped into four functional domains. We evaluated associations of diagnosed diabetes (via self-report), and undiagnosed diabetes and prediabetes (via HbA1c), with functional disability using Poisson regression.
RESULTS
Participants had a mean age of 75 years, 42% were male, 22% were black, and 31% had diagnosed diabetes. Those with diagnosed diabetes had a significantly greater burden of functional disability compared to those without diabetes even after adjustment for demographics, health behaviors, and comorbidities: prevalence ratios (95% CIs) were 1.24 (1.15, 1.34) for lower extremity mobility; 1.14 (1.07, 1.21) for general physical activities; 1.33 (1.16, 1.52) for instrumental activities of daily living; and 1.46 (1.24, 1.73) for activities of daily living (all P < 0.05). The associations of undiagnosed diabetes and prediabetes with disability were not statistically significant (all P < 0.05).
CONCLUSIONS
Among older adults, the burden of functional disability associated with diabetes was not entirely explained by known risk factors including comorbidities. Hyperglycemia below the threshold for the diagnosis of diabetes was not associated with disability. Research into effective strategies for the prevention of functional disability among older adults with diabetes is needed.
Keywords: Aging, Diabetes Complications, Disability, Physical Function, Prevalence
INTRODUCTION
In the US, the prevalence of diabetes among adults aged 65 years or older is approximately 20–25%.1,2 Diabetes poses major clinical and public health challenges in older adults, and the burden of the disease is predicted to rise substantially as the population ages.1,2 Diabetes is known to increase the risk for major macrovascular and microvascular conditions that can directly contribute to the development of functional decline and subsequent disability.3–5
Functional disability is frequently defined as difficulty in performing tasks essential to independent living.3–5 Such tasks include walking up several flights of stairs, lifting or carrying objects, dressing, and managing money.3–5 Older adults with a functional disability use health services more frequently and are at higher risk of dependence, hospitalization, and death compared to those without a disability.3–5 Thus, assessing the burden of functional disability associated with diabetes is essential for characterizing the health needs of older adults.
Previous research suggests that older adults with diabetes are significantly more likely to have a functional disability than those without diabetes.5 However, few studies have attempted to evaluate the extent to which diabetes-related comorbidities account for the association between diabetes and disability4–6, and studies with high-quality characterization of comorbidities in diverse populations are needed.5 Still fewer studies have examined the association of disability along the spectrum of HbA1c defined hyperglycemia in older adults, and their findings are conflicting.7,8 Additionally, very little is known about the association of disability with glucose-lowering medication, glycemic control, and duration of diabetes.4,9,10 Further research into each of these areas will help to more accurately establish the burden of functional disability associated with diabetes in older adults5 and may inform ongoing debates regarding the optimal clinical care of older adults with the disease.11
In the present study, we compared the prevalence of functional disability in older adults with and without diabetes and examined the extent to which diabetes-related comorbidities attenuated the observed association. Secondary aims were to 1) assess if the association between diabetes and functional disability was moderated by sex, age, race, or obesity status, 2) determine if prediabetes and undiagnosed diabetes were associated with functional disability, and 3) evaluate the associations of glucose-lowering medication, glycemic control, and duration of diabetes with functional disability among those with diagnosed diabetes.
METHODS
The Atherosclerosis Risk in Communities (ARIC) Study is a community-based prospective cohort study of 15,792 primarily black and white adults designed to examine risk factors for cardiovascular disease and related morbidity and mortality.12 Participants were recruited from four US communities: Forsyth County, North Carolina; Jackson, Mississippi; Minneapolis, Minnesota; and Washington County, Maryland. Data were collected at five in-person visits, each of which included an interview, physical examination, and blood collection. Visit 1 was conducted from 1987 to 1989 and visit 5 was conducted from 2011 to 2013. Interviews were conducted with participants during annual and semi-annual follow-up telephone calls. There were 6,538 participants who completed visit 5. We excluded participants missing information on functional disability (n = 370), missing covariates of interest (n = 1,117), and whose race was not black or white (n = 12), resulting in a final sample of 5,035 participants.
The institutional review boards of all participating academic recruitment sites approved the study protocol. All participants provided written informed consent.
Assessment of diabetes, prediabetes, and glycemic control
Participants were considered to have diagnosed diabetes if they self-reported being told by a physician that they had diabetes or were using glucose-lowering medication during any visit or follow-up telephone call prior to and including visit 5.13 Among those with diagnosed diabetes at visit 5, duration of diabetes was calculated as the time between when the participant was first considered to have diagnosed diabetes (as defined above) and the date of visit 5. HbA1c was measured at visit 5 in whole blood samples with a Tosoh G7 automated analyzer (Tosoh Bioscience Inc., South San Francisco, CA) using high-performance liquid chromatography.14 Among participants without diabetes, we defined normoglycemia as an HbA1c < 5.7% (39 mmol/mol), prediabetes as an HbA1c ≥ 5.7% (39 mmol/mol) and < 6.5% (48 mmol/mol), and undiagnosed diabetes as an HbA1c ≥ 6.5% (48 mmol/mol).15 Among those with diabetes, poor glycemic control was defined as an HbA1c ≥ 7.0% (53 mmol/mol).16
Assessment of functional disability
During the annual and semi-annual phone calls contemporaneous to visit 5, participants were asked how much difficulty they had completing twelve tasks. Responses included “no difficulty”, “some difficulty”, “much difficulty”, or “unable to do”. Tasks were categorized into four previously defined functional domains.4,17–19 These included lower extremity mobility (i.e., walking for a quarter of a mile and walking up 10 steps without resting), general physical activities (i.e., stooping, crouching or kneeling; lifting or carrying something as heavy as 10 pounds; and standing up from an armless chair), instrumental activities of daily living (i.e., doing chores around the house; preparing meals; and managing money), and activities of daily living (i.e., eating, dressing, getting in or out of bed, and walking from one room to another on the same level). In line with previous research, participants were considered to have a functional disability if they self-reported any difficulty (i.e., “some difficulty”, “much difficulty”, or “unable to do”) completing at least one task within a domain.4,17–19 In sensitivity analyses, functional disability was defined more stringently as self-report of having much difficulty or being unable to do at least one task within a domain. The importance of categorizing tasks into functional domains is well-established,20 and self-reported functional disability has been shown to be highly reliable.21
Covariates
Information on sex (male/female), age (continuous years), race (black/white), and education (less than high school; high school or equivalent; and college or above) was self-reported at visit 1. At visit 5, employment status (employed/unemployed), marital status (married/unmarried), income (< $25,000; $25,000 to $50,000; and > $50,000), smoking status (never, former, and current), and alcohol status (never, former, and current) were self-reported. Physical activity was assessed at visit 5 using the modified Baecke questionnaire.22,23 Standardized methods for the measurement of body mass index, blood pressure, estimated glomerular filtration rate (eGFR), and ankle brachial index (ABI) have been previously described.24–26 Obesity was defined as a body mas index ≥ 30.0 kg/m2.27 Hypertension was defined using the mean of two blood pressure readings with cut-points of systolic blood pressure ≥ 140 mmHg, diastolic blood pressure ≥ 90 mmHg, or blood pressure-lowering medication use.28 Chronic kidney disease was defined by an eGFR < 60 mL/min/1.73 m2,29 and peripheral arterial disease was defined by an ABI < 0.90 in either leg.30 Prevalent coronary heart disease, congestive heart failure, myocardial infarction, and stroke were defined as self-reported cases at visit 1 or an adjudicated event at or before visit 5.12 History of fracture hospitalization was defined as any hospitalization after visit 1 that included any of the International Classification of Diseases, 9th revision, discharge codes of 733.1–733.19, 733.93–733.98, or 800–829.31
Statistical analysis
Descriptive statistics (proportions, means, and standard deviations) were used to describe the demographics, health behaviors, and comorbidities of participants with and without diabetes. Differences were assessed using chi-square tests for categorical variables and two sample t-tests or analysis of variance for continuous variables. Five series of Poisson regression models with robust error variances were used to examine the association of diabetes with the prevalence of functional disability within each functional domain and across any functional domain. In each series, an unadjusted (crude) model included diabetes status; model 1 included diabetes status and demographic variables; model 2 included all variables in model 1 and health behaviors; and model 3 included all variables in model 2 and comorbidities. We conducted sensitivity analyses with functional disability defined as having much difficulty or being unable to do a task. Interactions between diabetes and sex, age, race, and obesity status in predicting the prevalence of any functional disability were tested in separate multiplicative models that were adjusted for all of the other potential moderators (e.g., the interaction between diabetes and sex was adjusted for age, race, and body mass index).
We examined the association between prediabetes, undiagnosed diabetes, and clinical categories of HbA1c among those with diabetes (i.e., <7.0% (53 mmol/mol); 7.0% (53 mmol/mol) to 8.0% (64 mmol/mol); and >8.0% (64 mmol/mol)) using Poisson regression models with robust error variances and the same modeling building approach as previously described. Among participants with diabetes, the association of glucose-lowering medication use (dichotomous), poor glycemic control (dichotomous), and duration of diabetes (continuous) with the prevalence of any functional disability was also assessed using Poisson regression. All reported P values are two-sided and the predefined cut-off for statistical significance was set at P < 0.05. All statistical analyses were conducted using Stata version 12 (StataCorp, College Station, TX).
RESULTS
The prevalence of diagnosed diabetes was 31.0% (Table 1). Diabetes was significantly more common among black participants and those who were unmarried, unemployed, and had less formal education and income (Table 1). Participants who were former or current alcohol consumers, had a lower physical activity level, or had a higher body mass index were significantly more likely to have diabetes (Table 1). Age and smoking status were not associated with diabetes (Table 1). Compared to participants without diabetes, those with diabetes had a greater burden of comorbidities. This included a significantly higher prevalence of hypertension, chronic kidney disease, peripheral arterial disease, coronary heart disease, congestive heart failure, and stroke, but not myocardial infarction or a history of fractures (Table 1).
Table 1.
Characteristics of ARIC Study participants overall and according to diagnosed diabetes status at visit 5, 2011–2013*
| All Participants | Diagnosed Diabetes | No Diabetes | |
|---|---|---|---|
| n | 5,035 (100.0) | 1,562 (31.0) | 3,473 (69.0) |
| Male | 2,106 (41.8) | 690 (44.2) | 1,416 (40.8) |
| Mean (SD) Age (years) | 75.3 (5.0) | 75.3 (5.1) | 75.4 (5.0) |
| Black | 1,087 (21.6) | 458 (29.3) | 629 (18.1) |
| Education | |||
| Less than High School | 656 (13.0) | 284 (18.2) | 372 (10.7) |
| High School or Equivalent | 2,105 (41.8) | 664 (42.5) | 1,441 (41.5) |
| College or Above | 2,274 (45.2) | 614 (39.3) | 1,660 (47.8) |
| Employed | 1,004 (19.9) | 264 (16.9) | 740 (21.3) |
| Married | 3,401 (67.5) | 990 (63.4) | 2,411 (69.4) |
| Family Income | |||
| Less than $25,000 | 1,250 (24.8) | 492 (31.5) | 758 (21.8) |
| $25,000 to $49,999 | 1,555 (30.9) | 471 (30.2) | 1,084 (31.2) |
| Greater than $49,999 | 2,230 (44.3) | 599 (38.3) | 1,631 (47.0) |
| Cigarette Smoking Status | |||
| Current | 291 (5.8) | 89 (5.7) | 202 (5.8) |
| Former | 2,467 (49.0) | 786 (50.3) | 1,681 (48.4) |
| Never | 2277 (45.2) | 687 (44.0) | 1590 (45.8) |
| Alcohol Drinking Status | |||
| Current | 2,544 (50.5) | 628 (40.2) | 1,916 (55.2) |
| Former | 1,437 (28.5) | 576 (36.9) | 861 (24.8) |
| Never | 1,054 (20.9) | 358 (22.9) | 696 (20.0) |
| Mean (SD) Physical Activity Index (1 to 5 scale) | 2.4 (0.6) | 2.3 (0.6) | 2.5 (0.6) |
| Mean (SD) Body Mass Index (kg/m2) | 28.6 (5.5) | 30.4 (5.6) | 27.8 (5.2) |
| Hypertension | 3,712 (73.7) | 1,327 (85.0) | 2,385 (68.7) |
| Chronic Kidney Disease | 1,402 (27.8) | 516 (33.0) | 886 (25.5) |
| Peripheral Arterial Disease | 382 (7.6) | 168 (10.8) | 214 (6.2) |
| Coronary Heart Disease | 712 (14.1) | 299 (19.1) | 413 (11.9) |
| Congestive Heart Failure | 785 (15.6) | 390 (25.0) | 395 (11.4) |
| Myocardial Infarction | 100 (2.0) | 39 (2.5) | 61 (1.8) |
| Stroke | 165 (3.3) | 80 (5.1) | 85 (2.4) |
| History of Fracture-related Hospitalization | 283 (5.6) | 83 (5.3) | 200 (5.8) |
| Mean (SD) HbA1c (% [mmol/mol]) | 5.9 [41.0] (0.8 [8.7]) | 6.6 [49.0] (1.1 [12.0]) | 5.6 [38.0] (0.4 [4.4]) |
| Use of Glucose-Lowering Medication | 993 (19.7) | 993 (63.6) | - |
| Duration of Diabetes, (years) | 10.2 (6.4) | 10.2 (6.4) | - |
| Functional Disability | |||
| Lower Extremity Mobility | 1,565 (31.1) | 689 (44.1) | 876 (25.2) |
| General Physical Activities | 2,292 (45.5) | 879 (56.3) | 1,413 (40.7) |
| Instrumental Activities of Daily Living | 707 (14.0) | 327 (20.9) | 380 (10.9) |
| Activities of Daily Living | 525 (10.4) | 250 (16.0) | 275 (7.9) |
| Any Functional Disability | 2,650 (52.6) | 1,008 (64.5) | 1,642 (47.3) |
Values are numbers (percentages) unless otherwise specified. HbA1c Glycated hemoglobin. Functional disability was defined as self-reported difficulty performing a task essential to independent living categorized into functional domains.
Compared to participants without diabetes, those with diabetes reported significantly greater difficulty completing tasks in each of the functional domains assessed (Table 1). The overall prevalence of functional disability was highest within general physical activities (diabetic 56.3% vs. non-diabetic 40.7%), followed by lower extremity mobility (diabetic 44.1% vs. non-diabetic 25.2%), instrumental activities of daily living (diabetic 20.9% vs. non-diabetic 10.9%), and activities of daily living (diabetic 16.0% vs. non-diabetic 7.9%). Unadjusted prevalence ratios ranged from 1.38 to 2.02 across the functional domains, with the highest being for activities of daily living followed by instrumental activities of daily living, lower extremity mobility, and general physical activities (Table 2, Crude, all P < 0.05). The unadjusted prevalence ratio for functional disability in any functional domain was 1.36 (Table 2, Crude, all P < 0.05). After adjustment for demographics (Table 2, Model 1), health behaviors (Table 2, Model 2), and comorbidities (Table 2, Model 3), the associations were attenuated but remained statistically significant across all functional domains (all P < 0.05). In sensitivity analyses that defined functional disability as having much difficulty or being unable to do a task within any functional domain, prevalence ratios were higher and indicated similar patterns of association (Supplementary Table S1, available online).
Table 2.
Prevalence ratios (PR) and 95% confidence intervals (CI) for the association of diagnosed diabetes with functional disability after adjustment for demographics, health behaviors, and comorbidities among ARIC Study participants at visit 5, 2011–2013 (N=5,035)*
| Diagnosed Diabetes (vs. No Diabetes) |
Lower Extremity Mobility |
General Physical Activities |
Instrumental Activities of Daily Living |
Activities of Daily Living |
Any | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| PR | 95% CI | PR | 95% CI | PR | 95% CI | PR | 95% CI | PR | 95% CI | |
| Crude | 1.75 | 1.61, 1.89 | 1.38 | 1.30, 1.47 | 1.91 | 1.67, 2.19 | 2.02 | 1.72, 2.37 | 1.36 | 1.30, 1.44 |
| Model 1: Crude + Demographics |
1.62 | 1.49, 1.75 | 1.33 | 1.26, 1.41 | 1.65 | 1.45, 1.88 | 1.81 | 1.54, 2.13 | 1.31 | 1.24, 1.37 |
| Model 2: Model 1 + Health behaviors |
1.45 | 1.34, 1.56 | 1.24 | 1.17, 1.32 | 1.50 | 1.32, 1.71 | 1.64 | 1.39, 1.93 | 1.22 | 1.16, 1.28 |
| Model 3: Model 2 + Comorbidities |
1.24 | 1.15, 1.34 | 1.14 | 1.07, 1.21 | 1.33 | 1.16, 1.52 | 1.46 | 1.24, 1.73 | 1.12 | 1.07, 1.18 |
Functional disability was defined as self-reported difficulty performing a task essential to independent living categorized into functional domains. Demographics include sex, age, race, education, employment status, marital status, and income. Health behaviors include smoking, drinking, and physical activity. Comorbidities include obesity, hypertension, chronic kidney disease, peripheral arterial disease, coronary heart disease, congestive heart failure, myocardial infarction, stroke, and history of fracture-related hospitalizations.
The prevalence of functional disability was the highest among participants with diabetes who were older than 75 years (67.1%, range 76 to 90 years), black (69.4%), women (72.8%), or obese (73.4%), and it was the lowest among those without diabetes who were male (39.3%), 75 years old or younger (41.9%, range 67 to 75 years), non-obese (41.5%), or white (45.1%) (Figure 1). There was evidence for interactions between diabetes and age, race, and obesity status in predicting the prevalence of any functional disability. Adjusted prevalence ratios indicate that the difference in the prevalence of functional disability between participants with diabetes and those without diabetes who were older than 75 years was significantly less than the difference for those who were 75 years old or younger (Figure 1, B; P < 0.001). Similar trends were found when comparing black and white participants (Figure 1, C; P < 0.05) and obese and non-obese participants (Figure 1, D; P < 0.01). There was not a statistically significant interaction between diabetes and sex in predicting the prevalence of any functional disability (Figure 1, A; P = 0.49).
Figure 1.
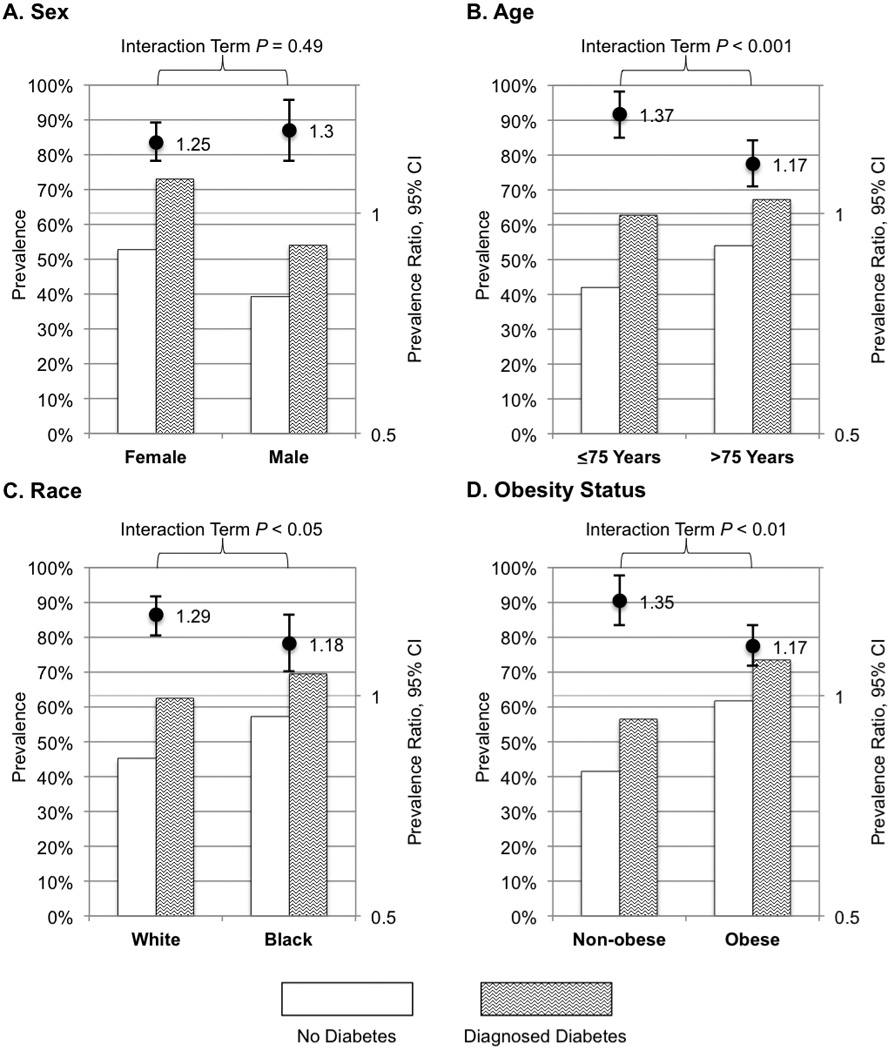
Prevalence, prevalence ratios and 95% confidence intervals (CI), and interaction term significance for examining the association of diabetes with functional disability by sex (A), age (B), race (C), and obesity status (D) among ARIC Study participants at visit 5, 2011–2013 (N=5,035). Functional disability was defined as self-reported difficulty performing a task essential to independent living. Each multiplicative model was adjusted for all of the other potential moderators.
In analyses to investigate potential associations of hyperglycemia with any functional disability, crude prevalence ratios were higher according to the progression of clinical categories of HbA1c (Table 3, Crude, all P < 0.05). However, after adjustment for demographics (Table 3, Model 1), health behaviors (Table 3, Model 2), and comorbidities (Table 3, Model 3) the associations were attenuated and no longer statistically significant for prediabetes and undiagnosed diabetes compared to no diabetes (all P > 0.05), whereas the associations remained statistically significant for each clinical category of HbA1c among participants with diagnosed diabetes (all P < 0.01).
Table 3.
Prevalence ratios (PR) and 95% confidence intervals (CI) for the association of diagnosed diabetes and HbA1c category with any functional disability after adjustment for demographics, health behaviors, and comorbidities among ARIC Study participants at visit 5, 2011–2013 (N=5,035)*
| Normoglycemia (vs. HbA1c Category) | Crude | Model 1: Crude + Demographics |
Model 2: Model 1 + Health behaviors |
Model 3: Model 2 + Comorbidities |
|||||
|---|---|---|---|---|---|---|---|---|---|
| PR | 95% CI | PR | 95% CI | PR | 95% CI | PR | 95% CI | ||
| No Diabetes | <5.7% (39 mmol/mol) | Reference | Reference | Reference | Reference | ||||
| 5.7% (39 mmol/mol) to 6.5% (48 mmol/mol) | 1.12 | 1.04, 1.20 | 1.07 | 1.00, 1.14 | 1.07 | 1.00, 1.14 | 1.02 | 0.96, 1.09 | |
| ≥6.5% (48 mmol/mol) | 1.27 | 1.05, 1.54 | 1.18 | 0.97, 1.42 | 1.13 | 0.93, 1.36 | 1.05 | 0.87, 1.27 | |
| Diagnosed Diabetes | <7.0% (53 mmol/mol) | 1.41 | 1.31, 1.50 | 1.32 | 1.24, 1.41 | 1.24 | 1.16, 1.32 | 1.13 | 1.06, 1.21 |
| 7.0% (53 mmol/mol) to 8.0% (64 mmol/mol) | 1.53 | 1.39, 1.68 | 1.43 | 1.30, 1.57 | 1.32 | 1.21, 1.45 | 1.16 | 1.06, 1.27 | |
| ≥8.0% (64 mmol/mol) | 1.59 | 1.42, 1.78 | 1.48 | 1.33, 1.65 | 1.37 | 1.23, 1.52 | 1.17 | 1.05, 1.30 | |
Functional disability was defined as self-reported difficulty performing a task essential to independent living. Demographics include sex, age, race, education, employment status, marital status, and income. Health behaviors include smoking, drinking, and physical activity. Comorbidities include obesity, hypertension, chronic kidney disease, peripheral arterial disease, coronary heart disease, congestive heart failure, myocardial infarction, stroke, and history of fracture-related hospitalizations
Among participants with diagnosed diabetes (n = 1,562), 63.6% were currently taking glucose-lowering medication, 27.9% had poor glycemic control, and the mean (SD) duration of diabetes was 10.2 (6.4) years. Participants who reported taking glucose-lowering medication had a higher prevalence of functional disability than those who reported no medication use (prevalence ratio 1.10, 95% CI 1.02 to 1.19, P < 0.05), but after adjustment for sex, age, race, and body mass index the association did not remain statistically significant (prevalence ratio 1.07, 95% CI 0.99 to 1.15, P = 0.11). Similarly, participants with poor glycemic control, defined by an HbA1c greater than or equal to 7.0% (53 mmol/mol), had a higher prevalence of functional disability (prevalence ratio 1.10, 95% CI 1.02 to 1.19, P < 0.05), but after adjustment for sex, age, race, and body mass index the association was not significant (prevalence ratio 1.06, 95% CI 0.99 to 1.15, P = 0.11). An association between the duration of the participant’s diabetes and functional disability was observed. The prevalence of functional disability increased by approximately 1.3% for every year of diabetes (prevalence ratio 1.013, 95% CI 1.007 to 1.018, P < 0.001) in an unadjusted model, and by 1.0% for every year of diabetes (prevalence ratio 1.010, 95% CI 1.004 to 1.015, P < 0.001) in a model adjusted for sex, age, race, and body mass index.
DISCUSSION
These results suggest community-dwelling older adults with diagnosed diabetes have a significantly greater burden of functional disability compared to those without a history of diabetes. The association between diabetes and functional disability was present across four distinct functional domains, with the greatest diabetes-related burden in activities of daily living followed by instrumental activities of daily living, lower extremity mobility, and general physical activities. Importantly, the associations remained statistically significant even after adjustment for demographics, health behaviors, and numerous comorbidities. The associations were stronger when we utilized a stringent definition for functional disability that included the report of having much difficulty or being unable to complete a task in any functional domain.
Our findings are consistent with previous studies of the association between diabetes and functional disability. A recent systematic review and meta-analysis pooled results from twelve cross-sectional studies and demonstrated that those with diabetes had increased odds of having difficulty completing lower extremity mobility tasks compared to those without diabetes (OR 1.71, 95% CI 1.53 to 1.91).5 Pooled point estimates similarly showed that having diabetes was associated with increased odds of disability within the domains of activities of daily living (OR 1.87, 95% CI 1.66 to 2.10) and instrumental activities of daily living (OR 1.67, 95% CI 1.57 to 1.77).5
Past research has not extensively examined potential interactions.4,10 We found evidence that age, race, and obesity status moderate the association between diabetes and functional disability. These results indicate that there may be disparities in the prevalence of functional disability overall, and they highlight the need for interventions that target key subgroups. Namely, the association between diabetes and functional disability was stronger among adults who were 67 to 75 years old, white, or non-obese compared to those who were 76 to 90 years old, black, and obese, respectively. This is likely because the prevalence of functional disability among adults in the latter groups was high, which makes it difficult to detect relative differences by diabetes status. Efforts to reduce the risk of functional disability may be most effective among adults who are older than 75 years, black, or obese, regardless of their diabetes status. Additional research is needed to confirm these findings.
In contrast with previous studies, we found that after adjustment for differences in demographics, health behaviors, and several comorbidities, adults with prediabetes and undiagnosed diabetes did not have a significantly greater burden of functional disability compared to those who were normoglycemic.7,8 Additionally, among adults with diagnosed diabetes, the use of glucose-lowering medication and poor glycemic control were not associated with functional disability after adjustment for covariates. However, the burden of functional disability did increase significantly with each year that an individual lived with diabetes suggesting a potential role for sustained glycemic exposure in the observed associations. This is only the second study we are aware of to report an association between the duration of diabetes and functional disability.10 Taken together, these results suggest that hyperglycemia below the threshold for a diagnosis of diabetes may not significantly contribute to the burden of functional disability among older adults, but this needs to be further investigated.
The precise mechanisms by which diabetes leads to functional disability remain unclear. Chronic hyperglycemia may activate inflammatory pathways that lead to a loss of muscle mass, strength, and quality, particularly in the lower extremities.32 This could then lead to decreased physical movement and participation in routine activities, thus aggravating the onset of functional disability. Further, comorbidities commonly associated with longer duration of diabetes, such as coronary heart disease, peripheral arterial disease, and stroke, can all lead to functional disability.3–5 It is also conceivable that physical and cognitive impairment may lead to subsequent chronic hyperglycemia.33 In this manner, the relation between diabetes and functional disability is possibly bidirectional. Cross-sectional study designs are unable to establish temporal associations, and longitudinal studies that assess changes in glycemia, chronic disease states, and functional disability may enhance our understanding of the mechanisms by which diabetes leads to increased risk of functional disability.
This study has several important strengths and adds significantly to existing research on this topic. First, we used a large population-based sample of black and white older adults who were well characterized, especially in regard to glycemia and potential comorbidities. This enabled us to examine differences in functional disability along the glycemic spectrum, control for several potential confounding factors, and explore interactions in subgroups. Additionally, we assessed difficulty in completing twelve common tasks within four functional domains. Previous research has established the importance of grouping tasks into functional domains.20
The findings of this study should be considered within its limitations. First, the cross-sectional nature of the study prohibits the establishment of temporal associations. Further, it does not allow us to evaluate the extent to which survival bias (i.e., the fact that individuals with diabetes are more likely to die at younger ages than those without diabetes) may have influenced the observed associations. An additional limitation is that the sample did not include institutionalized older adults who likely have a higher prevalence of functional disability than community dwelling older adults, thus limiting the generalizability of our results. Although self-reported diabetes in the ARIC study has been shown to be valid and reliable13, the use of different definitions for diabetes may result in different estimates of the strength of association between diabetes and functional disability. Lastly, random error or social desirability could have influenced the measurement of difficulty completing tasks, which in turn may have influenced our assessment of functional disability.
In summary, this study shows that diabetes is associated with a high burden of functional disability among community dwelling older adults, and this association was not entirely explained by diabetes-related comorbidities. Our data suggest that although the burden of functional disability is highest among adults who are older than 75 years, black, or obese, the burden of diabetes-related functional disability is greater among adults who were 75 years old or younger, white, or non-obese. Further, individuals with prediabetes and undiagnosed diabetes did not have a significantly greater prevalence of functional disability compared to those who were normoglycemic after accounting for potential confounders in this sample. Among those with diabetes, the use of glucose-lowering medication and poor glycemic control were not associated with functional disability, but the duration of diabetes was positively associated with the outcome. Longitudinal research that measures changes in glycemia, chronic disease states, and multiple domains of functional disability would help to further elucidate if the burden of disability increases in a graded manner from prediabetes to diabetes and would allow for a more precise estimate of the effect that diabetes duration has on the development of disability. Future studies should focus on potential underlying mechanisms that provide opportunities for intervention in the pathway between diabetes and disability. As the population ages and diabetes becomes more common, the burden of functional disability in the older population will also likely increase. This study highlights the need for continued surveillance of diabetes-related functional disability, as well as more research into effective strategies for the prevention of functional disability among those with diabetes.
Supplementary Material
THE SIGNIFICANT FINDINGS OF THE STUDY.
Diabetes is associated with a high burden of functional disability. Undiagnosed diabetes, prediabetes, use of glucose-lowering medication, and poor glycemic control were not associated with functional disability, but the duration of diabetes was positively associated with the outcome.
THIS STUDY ADDS
Use of a large, well characterized (especially in regard to glycemia and potential comorbidities) population-based sample of older adults enabled examination of differences in functional disability along the glycemic spectrum, control for several confounding factors, and explore interactions in subgroups.
Acknowledgments
J.G.G., L.J.A., and E.S. defined the research question. J.G.G. conducted the statistical analyses and drafted the manuscript. All authors contributed to the interpretation of the results, critically revised the manuscript, and have read and approved the final version of the manuscript. J.G.G. and E.S. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
J.G.G. is supported by NIH/NIA Epidemiology & Biostatistics of Aging training grant T32AG000247. C.M.P. is supported by NIH/NHLBI Cardiovascular Epidemiology training grant T32HL007024. R.R.K is supported by NIH/NIDDK grant K23DK093583. J.A.S. is supported by NIH/NIA grant K01AG048765. E.S. is supported by NIH/NIDDK grant R01DK089174. The ARIC Study is carried out as a collaborative study supported by National Heart, Lung, and Blood Institute (contracts HHSN268201100005C, HHSN268201100006C, HHSN268201100007C, HHSN268201100008C, HHSN 268201100009C, HHSN268201100010C, HHSN 268201100011C, and HHSN268201100012C).
The authors thank the staff and participants of the ARIC Study for their important contributions.
Footnotes
DISCLOSURES
None declared.
REFERENCES
- 1.Selvin E, Parrinello CM, Sacks DB, Coresh J. Trends in prevalence and control of diabetes in the United States, 1988–1994 and 1999–2010. Ann Intern Med. 2014;160:517–525. doi: 10.7326/M13-2411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boyle JP, Thompson TJ, Gregg EW, Barker LE, Williamson DF. Projection of the year 2050 burden of diabetes in the US adult population: dynamic modeling of incidence, mortality, and prediabetes prevalence. Popul Health Metr. BioMed Central Ltd. 2010;8:29. doi: 10.1186/1478-7954-8-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gregg EW, Beckles GL, Williamson DF, et al. Diabetes and physical disability among older U.S. adults. Diabetes Care. 2000;23:1272–1277. doi: 10.2337/diacare.23.9.1272. [DOI] [PubMed] [Google Scholar]
- 4.Kalyani RR, Saudek CD, Brancati FL, Selvin E. Association of diabetes, comorbidities, and A1C with functional disability in older adults: results from the National Health and Nutrition Examination Survey (NHANES), 1999–2006. Diabetes Care. 2010;33:1055–1060. doi: 10.2337/dc09-1597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wong E, Backholer K, Gearon E, et al. Diabetes and risk of physical disability in adults: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2013;1:106–114. doi: 10.1016/S2213-8587(13)70046-9. [DOI] [PubMed] [Google Scholar]
- 6.Gregg EW. Diabetes-related disability as a target for prevention. Lancet Diabetes Endocrinol. Elsevier Ltd. 2013;1:81–82. doi: 10.1016/S2213-8587(13)70054-8. [DOI] [PubMed] [Google Scholar]
- 7.Sayer AA, Dennison EM, Syddall HE, Gilbody HJ, Phillips DIW, Cooper C. Type 2 Diabetes, Muscle Strength, and Impaired Physical Function: The tip of the iceberg? Diabetes Care. 2005;28:2541–2542. doi: 10.2337/diacare.28.10.2541. [DOI] [PubMed] [Google Scholar]
- 8.Hiltunen L, Keinänen-Kiukaanniemi S, Läärä E, Kivelä SL. Functional ability of elderly persons with diabetes or impaired glucose tolerance. Scand J Prim Health Care. 1996;14:229–237. doi: 10.3109/02813439608997090. [DOI] [PubMed] [Google Scholar]
- 9.Gregg EW, Mangione CM, Cauley JA, et al. Diabetes and Incidence of Functional Disability in Older Women. Diabetes Care. 2002;25:61–67. doi: 10.2337/diacare.25.1.61. [DOI] [PubMed] [Google Scholar]
- 10.Wu JH, Haan MN, Liang J, Ghosh D, Gonzalez HM, Herman WH. Diabetes as a Predictor of Change in Functional Status Among Older Mexican Americans: A population-based cohort study. Diabetes Care. 2003;26:314–319. doi: 10.2337/diacare.26.2.314. [DOI] [PubMed] [Google Scholar]
- 11.Dardano A, Penno G, Del Prato S, Miccoli R. Optimal therapy of type 2 diabetes: a controversial challenge. Aging (Albany NY) 2014;6:187–206. doi: 10.18632/aging.100646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.The ARIC Investigators. The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. The ARIC investigators. Am J Epidemiol. 1989;129:687–702. [PubMed] [Google Scholar]
- 13.Schneider ALC, Pankow JS, Heiss G, Selvin E. Validity and reliability of self-reported diabetes in the atherosclerosis risk in communities study. Am J Epidemiol. 2012;176:738–743. doi: 10.1093/aje/kws156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Selvin E, Coresh J, Zhu H, Folsom A, Steffes MW. Measurement of HbA1c from stored whole blood samples in the Atherosclerosis Risk in Communities study. J Diabetes. 2010;2:118–124. doi: 10.1111/j.1753-0407.2010.00070.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.American Diabetes Association. Standards of medical care in diabetes-2013. Diabetes Care. 2013;36(Supple1):S11–S66. doi: 10.2337/dc13-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.American Geriatrics Society Expert Panel on the Care of Older Adults with Diabetes Mellitus. Guidelines abstracted from the american geriatrics society guidelines for improving the care of older adults with diabetes mellitus: 2013 update. J Am Geriatr Soc. 2013;61:2020–2026. doi: 10.1111/jgs.12514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kuo H-K, Bean JF, Yen C-J, Leveille SG. Linking C-reactive protein to late-life disability in the National Health and Nutrition Examination Survey (NHANES) 1999–2002. J Gerontol A Biol Sci Med Sci. 2006;61:380–387. doi: 10.1093/gerona/61.4.380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kuo H-K, Leveille SG, Yen C-J, et al. Exploring how peak leg power and usual gait speed are linked to late-life disability: data from the National Health and Nutrition Examination Survey (NHANES), 1999–2002. Am J Phys Med Rehabil. 2006;85:650–658. doi: 10.1097/01.phm.0000228527.34158.ed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen H, Guo X. Obesity and functional disability in elderly Americans. J Am Geriatr Soc. 2008;56:689–694. doi: 10.1111/j.1532-5415.2007.01624.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fried LP, Ettinger WH, Lind B, Newman AB, Gardin J. Physical disability in older adults: A physiological approach. J Clin Epidemiol. 1994;47:747–760. doi: 10.1016/0895-4356(94)90172-4. [DOI] [PubMed] [Google Scholar]
- 21.Rathouz PJ, Kasper JD, Zeger SL, et al. Short-term consistency in self-reported physical functioning among elderly women: the Women’s Health and Aging Study. Am J Epidemiol. 1998;147:764–773. doi: 10.1093/oxfordjournals.aje.a009521. [DOI] [PubMed] [Google Scholar]
- 22.Baecke Ja, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr. 1982;36:936–942. doi: 10.1093/ajcn/36.5.936. [DOI] [PubMed] [Google Scholar]
- 23.Richardson MT, Ainsworth BE, Wu HC, Jacobs DR, Leon AS. Ability of the Atherosclerosis Risk in Communities (ARIC)/Baecke Questionnaire to assess leisure-time physical activity. Int J Epidemiol. 1995;24:685–693. doi: 10.1093/ije/24.4.685. [DOI] [PubMed] [Google Scholar]
- 24.Selvin E, Wattanakit K, Steffes MW, Coresh J, Sharrett AR. HbA1c and peripheral arterial disease in diabetes: the Atherosclerosis Risk in Communities study. Diabetes Care. 2006;29:877–882. doi: 10.2337/diacare.29.04.06.dc05-2018. [DOI] [PubMed] [Google Scholar]
- 25.Wattanakit K, Folsom AR, Selvin E, Coresh J, Hirsch AT, Weatherley BD. Kidney function and risk of peripheral arterial disease: results from the Atherosclerosis Risk in Communities (ARIC) Study. J Am Soc Nephrol. 2007;18:629–636. doi: 10.1681/ASN.2005111204. [DOI] [PubMed] [Google Scholar]
- 26.Selvin E, Rawlings AM, Bergenstal RM, Coresh J, Brancati FL. No racial differences in the association of glycated hemoglobin with kidney disease and cardiovascular outcomes. Diabetes Care. 2013;36:2995–3001. doi: 10.2337/dc12-2715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.NHLBI Obesity Education Initiative Expert Panel on the Identification Evaluation and Treatment of Obesity in Adults. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: The evidence report. Bethesda, Maryland: 1998. [Google Scholar]
- 28.James Pa, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) JAMA. 2014;311:507–520. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 29.National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J KidneyDis. 2002;39:S1–S266. [PubMed] [Google Scholar]
- 30.Aboyans V, Criqui MH, Abraham P, et al. Measurement and interpretation of the ankle-brachial index: a scientific statement from the American Heart Association. Circulation. 2012;126:2890–2909. doi: 10.1161/CIR.0b013e318276fbcb. [DOI] [PubMed] [Google Scholar]
- 31.Schneider ALC, Williams EK, Brancati FL, Blecker S, Coresh J, Selvin E. Diabetes and risk of fracture-related hospitalization: the Atherosclerosis Risk in Communities Study. Diabetes Care. 2013;36:1153–1158. doi: 10.2337/dc12-1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Park SW, Goodpaster BH, Strotmeyer ES, et al. Accelerated loss of skeletal muscle strength in older adults with type 2 diabetes: the health, aging, and body composition study. Diabetes Care. 2007;30:1507–1512. doi: 10.2337/dc06-2537. [DOI] [PubMed] [Google Scholar]
- 33.Bardenheier BH, Gregg EW, Zhuo X, Cheng YJ, Geiss LS. Association of functional decline with subsequent diabetes incidence in U.S. adults aged 51 years and older: the Health and Retirement Study 1998–2010. Diabetes Care. 2014;37:1032–1038. doi: 10.2337/dc13-2216. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


