Abstract
Background
Intimate partner violence (IPV) is a global public health and human rights concern, though there is limited evidence on how to prevent it. This secondary analysis of data from the SASA! Study assesses the potential of a community mobilisation IPV prevention intervention to reduce overall prevalence of IPV, new onset of abuse (primary prevention) and continuation of prior abuse (secondary prevention).
Methods
A pair-matched cluster randomised controlled trial was conducted in 8 communities (4 intervention, 4 control) in Kampala, Uganda (2007–2012). Cross-sectional surveys of community members, 18–49 years old, were undertaken at baseline (n=1583) and 4 years postintervention implementation (n=2532). Outcomes relate to women's past year experiences of physical and sexual IPV, emotional aggression, controlling behaviours and fear of partner. An adjusted cluster-level intention-to-treat analysis compared outcomes in intervention and control communities at follow-up.
Results
At follow-up, all types of IPV (including severe forms of each) were lower in intervention communities compared with control communities. SASA! was associated with lower onset of abuse and lower continuation of prior abuse. Statistically significant effects were observed for continued physical IPV (adjusted risk ratio 0.42, 95% CI 0.18 to 0.96); continued sexual IPV (0.68, 0.53 to 0.87); continued emotional aggression (0.68, 0.52 to 0.89); continued fear of partner (0.67, 0.51 to 0.89); and new onset of controlling behaviours (0.38, 0.23 to 0.62).
Conclusions
Community mobilisation is an effective means for both primary and secondary prevention of IPV. Further support should be given to the replication and scale up of SASA! and other similar interventions.
Trial registration number
Keywords: VIOLENCE, PREVENTION, RANDOMISED TRIALS, SOCIAL EPIDEMIOLOGY, GENDER
Introduction
The global scale and ubiquity of violence against women is now widely recognised, as are the serious and diverse consequences of this violence for women's physical, mental and social well-being.1–3 With 30% of women worldwide estimated to have experienced physical and/or sexual violence at the hands of their partner,4 there is an urgent need for action.
While a plethora of interventions have focused on strengthening healthcare, justice and social sector responses to victims or perpetrators of violence, there is now a growing programming emphasis, particularly in low-income and middle-income countries, on violence prevention.5 6 Violence prevention interventions have sought variously to change attitudes and norms supportive of violence against women, promote gender equitable behaviours, and economically and socially empower women.5 7 Strategies have ranged from small group-based participatory education efforts and livelihoods programming, through to mass media edutainment programmes and community mobilisation—and yet, with a few notable exceptions,8–11 there is scant research into their effectiveness.5
We recently reported results from the SASA! Study, a cluster randomised trial (CRT) of a community mobilisation intervention to prevent violence against women and reduce HIV risk in Kampala, Uganda.12 After just under 3 years of intervention programming, women in intervention communities were 52% less likely to report past year experience of physical intimate partner violence (IPV), compared with women in control communities (adjusted risk ratio (aRR) 0.48, 95% CI 0.16 to 1.39), and also somewhat less likely to report past year experience of sexual IPV (aRR 0.76, 0.33 to 1.72). Though these results did not attain statistical significance due to high intercommunity variation in prevalence of these outcomes, large effect sizes and consistency in direction of effect between related outcomes are strongly suggestive of an intervention effect on IPV. Importantly effects were seen at the community level, not just among women reporting direct exposure to intervention activities.
While these findings are promising, they represent only a subset of SASA!'s potential impacts on the nature and extent of IPV. First, IPV comprises more than just physical and sexual acts. The WHO defines IPV as ‘any behaviour within an intimate relationship that causes physical, psychological or sexual harm to those in the relationship’, including physical aggression, sexual coercion, psychological abuse and controlling behaviours.13 Indeed, psychological (or emotional) abuse alone has been linked to a range of physical and mental health outcomes,14–18 prompting a call for researchers and health services to devote more attention to emotional abuse prevention and response.19 There is concern that programmes which focus primarily on physical and sexual violence prevention may inadvertently shift men towards emotional abuse as an alternative means of partner control.
Second, while the ultimate aim of prevention activities may be to entirely eradicate violence, reductions in frequency and severity are also important, especially in settings with high levels of violence.
Lastly, SASA! aimed at both primary violence prevention (stopping the onset of violence where it was not previously occurring) and secondary violence prevention (stopping violence from continuing where it was occurring previously). Impacts may not have been the same for both.
This paper therefore explores SASA!'s community-level impacts on a series of secondary violence outcomes. We consider different types of IPV, more severe or intense forms of each type of abuse (including injury associated with IPV), as well as examining both primary and secondary IPV prevention effects.
Methods
Study setting
The study was conducted between November 2007 and May 2012 in the Rubaga and Makindye Divisions of Kampala, Uganda. At the outset of the study, 44% of ever-partnered women aged 18–49 reported having experienced physical and or/sexual violence by an intimate partner at some point in their lives. Patriarchal norms were prevalent, with 25% of men and 58% of women reporting attitudes accepting of a man's use of violence against his wife.20
The SASA! intervention
The SASA! Activist Kit for Preventing Violence against Women and HIV21 is a community mobilisation intervention seeking to change community norms and behaviours that result in gender inequality, violence and increased HIV vulnerability for women. It was designed by Raising Voices (http://raisingvoices.org/) and implemented in Kampala by the Centre for Domestic Violence Prevention (CEDOVIP; http://www.cedovip.org/)
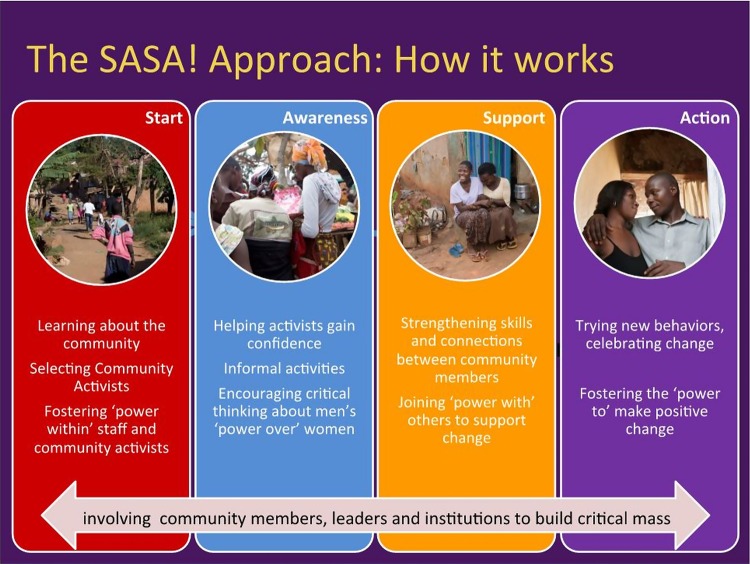
The SASA! approach draws heavily on two theoretical frameworks: the Ecological Model of violence which recognises the complex interplay of individual-level, relationship-level, community-level and societal-level factors underpinning IPV risk;22 and the Stages of Change Theory as set out by Prochaska et al,23 which identifies key stages involved in individual-level behaviour change. SASA! seeks to change individuals’ attitudes, community norms and structures, by supporting entire communities through a phased process of change. SASA!, meaning ‘Now’ in Kiswahili, is an acronym for the four phases of the approach—Start, Awareness, Support, Action (figure 1).
Figure 1.
Four phases of SASA!
In the Start phase, community activists (CAs), regular men and women interested in issues relating to violence, are selected and trained. Police officers, healthcare providers, institutional leaders, and local governmental and cultural leaders also receive training. These activists then work through the subsequent phases of SASA!, with a central focus throughout on discussions of ‘power’. After being introduced to new ways of thinking about power and encouraged to think about gender-related power imbalances in their own lives and communities, the CAs are supported to engage their communities in the same critical reflection—not only about the ways in which men and women may misuse power, with consequences for their relationships and communities, but also how people can use their power positively to foster change at an individual and community level.
SASA! uses four strategies: local activism, media and advocacy, communication materials, and training—with the specifics of intervention activities evolving in response to community priorities and characteristics. CAs conduct informal activities within their own social networks, among their families, friends, colleagues and neighbours. In this way, community members are exposed to SASA! ideas repeatedly and in diverse ways within the course of their daily lives, from people they know and trust as well as from more formal sources within their communities (see online supplementary appendix 1 for more detail).
Trial design
The evaluation design is described in detail elsewhere.24 Briefly, eight sites (comprising one or two parishes) were pair-matched on the basis of estimated population density and stability/mobility of the population. One from each pair was randomly selected to receive the intervention, and the other designated as a control. Two cross-sectional surveys of community members (18–49 years) were carried out in all sites, one prior to intervention implementation (baseline) and one approximately 4 years later (follow-up). Using calculations provided by Hayes and Bennett,25 sample size was determined with the aim of conducting the highest powered study deemed feasible given resource and staffing constraints. Interviewers conducting the baseline survey were blinded as to the allocation of the intervention, though the nature of the intervention precluded interviewer blinding at follow-up.
The study was conducted in accordance with WHO guidelines for the safe and ethical collection of data on violence against women.26 All respondents provided written informed consent and all were interviewed in a safe and private place of their choosing. For reasons of respondent safety, only one respondent per sampled household was interviewed. The study received ethical approval from the London School of Hygiene, Makerere University and the Uganda National Council of Science and Technology.
The study is registered at ClinicalTrials.gov (reference number NCT00790959) and the study protocol peer-reviewed and published in the journal Trials.24
Outcomes
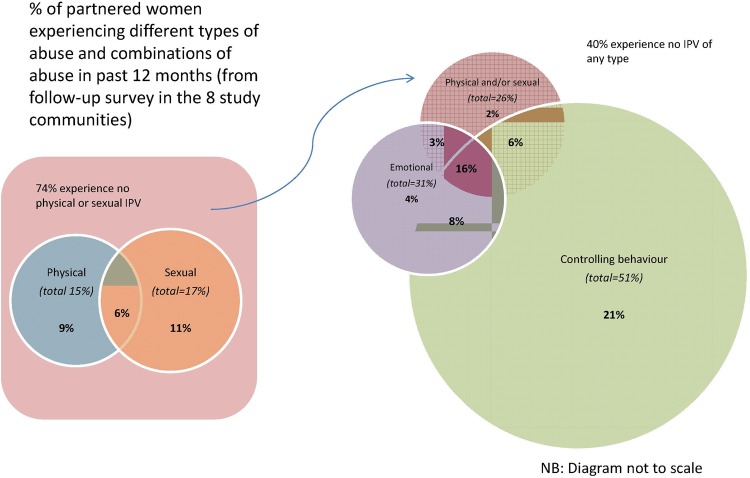
This secondary analysis focuses on women's reported past year experiences of IPV. Four categories of IPV-related outcomes are explored: physical and sexual IPV, emotional aggression, controlling behaviours, and a woman's reported fear of her partner. While women often experience multiple forms of violence in combination (figure 2), we examine them separately here to explore whether SASA! impacts on each in the same way.
Figure 2.
Venn diagram showing the overlap of women's experience of different types of partner abuse. (IPV, intimate partner violence).
For each category of abuse, indicators include overall past year prevalence, more severe/intense forms of that type of abuse, continued IPV (where there was already a history of IPV) and new onset of IPV (where there was no prior experience of IPV). Questions on IPV (measuring experiences of specific violent acts by a partner) were based on those used in the WHO Multi-country Study on Women's Health and Domestic Violence27 and Demographic and Health Surveys (DHS) including the Uganda DHS.28 29 Indicators of severe or high-intensity abuse take into account frequency and either severity or number of types of acts reported (severity for physical IPV; ≥1 type of act ‘many times’ or ≥3 types of act ‘once’ or a ‘few times’ for emotional aggression and controlling behaviours; as recommended by Heise (personal communication, 2015), based on an analysis of WHO multicountry study data). Injuries are also used as an indicator of severe physical and/or sexual IPV (see online supplementary appendix 2 for more detail on outcomes).
Statistical analysis
Intervention impacts were estimated using an adjusted cluster-level intention-to-treat (ITT) analysis comparing outcomes in intervention and control communities at follow-up (as per the primary trial analysis).12 Crude intervention effect was estimated using the geometric mean prevalence ratio. aRRs (controlling for community pair, age, marital status and baseline enumeration area-level (EA) prevalence of the outcome) were calculated from the comparison of ratios of observed to expected outcomes in intervention and control sites. Site-level expected prevalence of each outcome was predicted by fitting a logistic regression model to individual-level data, with the outcome as the dependent variable, and the above listed potential confounders as the independent variables. Statistical weighting was used to account for differences in denominators between sites.
As outlined in our study protocol,24 study power being low, we interpret effect estimates in terms of their direction and magnitude as well as their statistical significance. We also consider the consistency and coherence of results across related indicators.30
Results
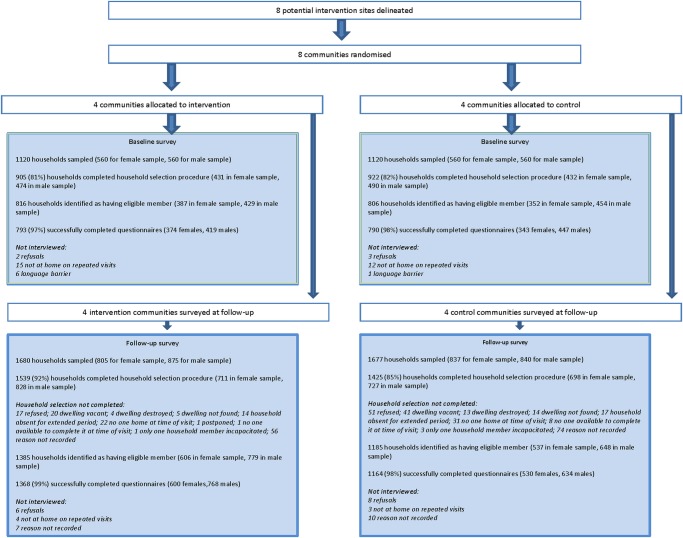
In total, 1583 respondents were interviewed at baseline (717 women, 866 men) and 2532 at follow-up (1130 women, 1402 men). Response rates for both surveys were high—98% at baseline and 99% at follow-up (figure 3).
Figure 3.
Trial profile.
Characteristics of female survey respondents are summarised in table 1. Data indicate high levels of comparability between intervention and control communities with respect to sociodemographic characteristics at both time points (table 1) and most of the outcome indicators at baseline (continued physical and continued sexual IPV were slightly more common in intervention communities than control communities; table 2).
Table 1.
Characteristics of women responding to the baseline and follow-up surveys
| Baseline | Follow-up | |||
|---|---|---|---|---|
| Intervention | Control | Intervention | Control | |
| Household level | N=374 | N=343 | N=599 | N=529 |
| Household has electricity | 259 (69%) | 264 (77%) | 503 (84%) | 445 (84%) |
| Main drinking water source—public tap | 228 (61%) | 212 (62%) | 391 (65%) | 336 (64%) |
| Toilet facility—traditional pit toilet/latrine | 225 (60%) | 203 (59%) | 389 (65%) | 302 (57%) |
| House is rented | 231 (62%) | 246 (72%) | 448 (75%) | 379 (72%) |
| House is in gated compound | – | – | 78 (13%) | 118 (22%) |
| Individual level | ||||
| Age (years) | 28.4 (7.7) | 28.2 (7.7) | 28.4 (7.4) | 29.1 (8.2) |
| Lived in same zone since before aged 12 (baseline)/for longer than 3 years (follow-up) | 44 (12%) | 45 (13%) | 353 (59%) | 313 (59%) |
| Buganda Tribe | 263 (71%) | 202 (59%) | 373 (62%) | 315 (60%) |
| Main religions | ||||
| Catholic | 119 (32%) | 108 (31%) | 209 (35%) | 165 (31%) |
| Muslim | 90 (24%) | 93 (27%) | 140 (23%) | 123 (23%) |
| Protestant | 104 (28%) | 80 (23%) | 141 (24%) | 133 (25%) |
| Born Again | 50 (13%) | 49 (14%) | 97 (16%) | 97 (18%) |
| Above primary education | 157 (42%) | 140 (41%) | 394 (66%) | 343 (65%) |
| Able to read | 345 (92%) | 313 (92%) | 535 (89%) | 480 (91%) |
| Does not earn money | 180 (48%) | 166 (48%) | 219 (37%) | 177 (33%) |
| Ever had a regular partner | 350 (94%) | 316 (92%) | 558 (93%) | 487 (92%) |
| Including casual | 574 (96%) | 497 (94%) | ||
| Had a regular partner in the past 12 months | 305 (82%) | 274 (80%) | 486 (81%) | 401 (76%) |
| Including casual | 504 (84%) | 427 (81%) | ||
| Currently married/cohabiting | 228 (61%) | 205 (60%) | 377 (63%) | 286 (54%) |
| In polygamous marriage (among those married) | 49/201 (24%) | 57/187 (30%) | 53/316 (17%) | 57/246 (23%) |
| No children | 83 (22%) | 83 (24%) | 136 (23%) | 121 (23%) |
Table 2.
Estimates of effect on violence outcomes,* comparing prevalence of outcome in intervention versus control communities
| Baseline | Follow-up | Control | Unadjusted RR† (95% CI) | Adjusted RR‡ (95% CI) | ||
|---|---|---|---|---|---|---|
| Intervention | Control | Intervention | ||||
| Past year experience of physical and sexual IPV | ||||||
| Physical IPV (among partnered in past year) | 75/302 (25%) | 57/273 (21%) | 46/504 (9%) | 93/424 (22%) | 0.45 (0.14 to 1.46) | 0.48 (0.16 to 1.39) |
| At least one act of severe physical IPV or more than one occurrence of less severe act (among partnered in past year) | 54/302 (18%) | 45/273 (16%) | 35/504 (7%) | 82/424 (19%) | 0.39 (0.16 to 0.99)* | 0.40 (0.14 to 1.17)** |
| New onset physical IPV (among ever partnered not previously experiencing physical IPV) | 25/236 (11%) | 20/214 (9%) | 20/438 (5%) | 40/360 (11%) | 0.54 (0.07 to 3.88) | 0.51 (0.09 to 3.06) |
| Continued physical IPV (among ever partnered previously experiencing physical IPV) | 50/112 (45%) | 37/102 (36%) | 26/133 (20%) | 53/135 (39%) | 0.46 (0.22 to 0.96)* | 0.42 (0.18 to 0.96)* |
| Sexual IPV (among partnered in past year) | 38/303 (13%) | 31/273 (11%) | 70/504 (14%) | 84/423 (20%) | 0.76 (0.33 to 1.74) | 0.76 (0.33 to 1.72) |
| New onset sexual IPV (among ever partnered not previously experiencing sexual IPV) | 11/294 (4%) | 11/255 (4%) | 19/463 (4%) | 15/384 (4%) | 1.08 (0.71 to 1.65) | 0.99 (0.56 to 1.73) |
| Continued sexual IPV (among ever partnered previously experiencing sexual IPV) | 27/55 (49%) | 20/61 (33%) | 51/109 (47%) | 69/111 (62%) | 0.75 (0.47 to 1.19) | 0.68 (0.53 to 0.87)* |
| Physical and/or sexual IPV (among partnered in past year) | 88/301 (29%) | 67/273 (25%) | 102/504 (20%) | 139/423 (33%) | 0.66 (0.33 to 1.33) | 0.69 (0.35 to 1.38) |
| Injury from physical/sexual IPV (among all partnered in past year) | 47/303 (16%) | 34/272 (13%) | 15/504 (3%) | 53/421 (13%) | 0.28 (0.04 to 2.14) | 0.20 (0.04 to 1.07)** |
| New onset physical and/or sexual IPV (among ever partnered not previously experiencing it) | 25/219 (11%) | 19/195 (10%) | 31/386 (8%) | 38/310 (12%) | 0.73 (0.23 to 2.31) | 0.72 (0.24 to 2.18) |
| Continued physical and/or sexual IPV (among ever partnered previously experiencing it) | 63/130 (48%) | 48/121 (40%) | 71/185 (38%) | 101/185 (55%) | 0.71 (0.42 to 1.21) | 0.64 (0.43 to 0.94)* |
| Emotional aggression§ | ||||||
| Any emotional IPV | 94/301 (31%) | 105/273 (38%) | 130/504 (26%) | 161/424 (38%) | 0.68 (0.58 to 0.80)* | 0.61 (0.47 to 0.79)* |
| High intensity emotional IPV (among all partnered in past year) | – | – | 40/504 (8%) | 95/424 (22%) | 0.37 (0.16 to 0.88)* | 0.37 (0.16 to 0.85)* |
| New onset of emotional aggression in past year | 25/235 (11%) | 26/199 (13%) | 28/357 (8%) | 38/297 (13%) | 0.61 (0.30 to 1.27) | 0.64 (0.36 to 1.12)** |
| Continued emotional aggression in past year | 69/112 (62%) | 79/116 (68%) | 102/215 (47%) | 123/198 (62%) | 0.76 (0.68 to 0.86)* | 0.68 (0.52 to 0.89)* |
| Controlling behaviours§ | ||||||
| Any controlling behaviour (among partnered in past year) | 211/303 (70%) | 192/273 (70%) | 224/504 (44%) | 253/423 (60%) | 0.75 (0.56 to 1.01)** | 0.75 (0.54 to 1.04)** |
| High-intensity controlling behaviours (among all partnered in past year) | – | – | 133/504 (26%) | 190/423 (45%) | 0.61 (0.40 to 0.93)* | 0.61 (0.39 to 0.95)* |
| New onset of controlling behaviours in past year | 17/104 (16%) | 15/89 (17%) | 19/237 (8%) | 41/184 (22%) | 0.36 (0.21 to 0.63)* | 0.38 (0.23 to 0.62)* |
| Continued controlling behaviours in past year | 194/242 (80%) | 177/226 (78%) | 205/334 (61%) | 212/310 (68%) | 0.91 (0.65 to 1.27) | 0.90 (0.69 to 1.17) |
| Fear of partner¶ | ||||||
| Fear of partner in past 12 months (among partnered in past year) | – | – | 82/500 (16%) | 121/419 (29%) | 0.64 (0.25 to 1.65) | 0.69 (0.28 to 1.72) |
| New fear of partner started in past 12 months (among ever partnered) | – | – | 23/360 (6%) | 26/287 (9%) | 0.75 (0.15 to 3.73) | 0.75 (0.15 to 3.77) |
| Fear of partner continued in past 12 months (among ever partnered) | – | – | 37/158 (23%) | 81/163 (50%) | 0.69 (0.53 to 0.90)* | 0.67 (0.51 to 0.89)* |
*p<0.05; **p<0.10.
†RRs calculated at the cluster level, both crude and adjusted ratios adjusting for community pair, and weighted according to the number of observations per village.
‡Adjusted RRs generated on the basis of expected number of events from a logistic regression model on individual data with independent variables including age, marital status and enumeration area level summary baseline measure of outcome indicator.
§Shorter list of items used to measure emotional aggression and controlling behaviours at baseline. Therefore, measures of prevalence of indicators relating to emotional aggression and controlling behaviours are not comparable between baseline and follow-up.
¶Fear of partner not measured at baseline. Adjusted RRs for these outcomes control for baseline physical and/or sexual IPV.
IPV, intimate partner violence; RR, risk ratio.
As described elsewhere, 91% of men and 68% of women in intervention communities reported any known exposure to SASA! materials or activities. Contamination of control communities was low with fewer than 2% of control respondents reporting any exposure.12
Table 2 presents community-level intervention effects on the IPV outcomes. All aRRs were in the hypothesised direction, with large effect sizes and CIs excluding unity for many of the indicators.
Overall past year prevalence by type of IPV
Women in intervention communities were less likely than their control counterparts to have experienced all types of IPV in the 12 months preceding the follow-up survey. While the largest effect size was seen in relation to physical IPV (aRR 0.48, 95% CI 0.16 to 1.39), women in intervention communities were also less likely to report sexual IPV (0.76, 0.33 to 1.72), emotional aggression (0.61, 0.47 to 0.79), controlling behaviours (0.75, 0.54 to 1.04) or fear of their partner (0.69, 0.28 to 1.72). Of these results, only that relating to emotional aggression was statistically significant—though it should be noted that high levels of intersite variation for the other indicators reduced study power to obtain statistically significant results (coefficient of variation [k] ranging from 0.15 for controlling behaviours, to 0.45 for physical IPV).
Severe or frequent IPV
Effect sizes were greater for more severe/intense forms of abuse. Women in intervention communities were much less likely than women in control communities to report severe/repeated episodes of physical IPV (0.40, 0.14 to 1.17); injury associated with physical/sexual IPV (0.20, 0.04 to 1.07); high-intensity emotional aggression (0.37, 0.16 to 0.85); and high-intensity controlling behaviours (0.61, 0.39 to 0.95). Results were statistically significant at the 5% level for high-intensity emotional aggression and controlling behaviours, and at the 10% level for injuries and severe/repeated physical IPV.
New onset and continued IPV
Women in intervention communities were at lower risk than women in control communities of both new onset of all types of IPV (except sexual IPV), and continuation of all types of IPV (where there was prior history of that form of abuse).
For physical IPV, sexual IPV, physical and/or sexual IPV, and fear of partner, prevention effects were slightly stronger in relation to continued IPV (secondary prevention) compared with new onset IPV (primary prevention). For emotional aggression, primary and secondary prevention effects were similar. For controlling behaviours, which have a higher prevalence than the other outcomes, primary prevention effects were stronger than secondary prevention effects. Statistically significant effects were observed in relation to continued physical IPV (0.42, 0.18 to 0.96); continued sexual IPV (0.68, 0.53 to 0.87); continued physical and/or sexual IPV (0.64, 0.43 to 0.94); continued emotional aggression (0.68, 0.52 to 0.89); continued fear of partner (0.67, 0.51 to 0.89); and new onset of controlling behaviours (0.38, 0.23 to 0.62).
Discussion
Intervention impacts were observed in the hypothesised direction for all types of IPV, with the strongest effects seen in relation to physical IPV and emotional aggression. Impacts were largest when the more severe or intense forms of abuse were considered, suggesting that in cases where IPV was not completely eliminated, SASA! may at least have reduced the frequency and/or severity of violent episodes. Importantly, both primary and secondary prevention effects were demonstrated, with greater impacts observed for the secondary prevention of all types of IPV except controlling behaviours (where primary prevention played a bigger role). As with the primary trial outcomes, these intervention effects were observed at the community level, not confined to individuals reporting exposure to the intervention.
Quantitative and qualitative analyses indicate that key pathways through which physical IPV was reduced include changes in community-level norms relating to gender-related power dynamics and the acceptability of IPV, as well as improved communication within relationships (Abramsky, submitted).31 These are also likely to be important pathways through which other forms of abuse and controlling behaviours were reduced. Improved community responses to IPV were also demonstrated in the primary trial analysis.12 Since SASA! led to no increase in women leaving abusive relationships (Abramsky, submitted), it is likely this improved community response which accounts for the strong secondary prevention effects observed.
This study has several strengths. Cluster randomisation removed the potential for programme placement bias. An ITT analysis on data from a random sample of community members assessed the overall community-level impact of the intervention rather than effects among self-selecting intervention participants. The repeated cross-sectional design allowed us to control for potential baseline imbalances in the prevalence of the outcomes between intervention and control communities.
The study also has a number of limitations, with several factors potentially biasing estimates of intervention effect towards the null. Despite geographical buffers between sites, some undetected contamination of control sites may have occurred—social diffusion is at the heart of the SASA! intervention, and the overall study area was small. Conversely, in intervention sites potential for intervention exposure was reduced both by moderate levels of population turnover and by extended interruptions to programming due to political unrest.
Reporting bias is a concern in a study such as this, with under-reporting of IPV common.32 33 Measurement bias was minimised through the use of standardised and widely used questions to measure IPV, administered by interviewers who had undergone 3 weeks of intensive training on how to conduct surveys relating to IPV. However, increased sensitisation to issues surrounding IPV could potentially have increased reports of IPV experience among women in intervention communities, thereby causing us to underestimate intervention effects. Nevertheless, we were still able to observe sizable effects for many IPV outcomes.
Changing trends in reporting may also explain why reports of sexual IPV increased in control sites during the course of the study (though stayed the same in intervention sites). One hypothesis to explain this is that external factors such as the Domestic Violence Act 201034 increased awareness of what constitutes sexual coercion, leading to overall increased disclosure across both intervention and control sites.
As with many trials of community-based interventions, the number of communities involved was small. High intercluster variation meant the study was underpowered to detect statistically significant effects for some of these IPV outcomes. Nevertheless, many results were statistically significant, and there was a high level of coherence in results across outcomes.
The SASA! Study yields hugely important insights for the field of violence prevention. It was the first CRT in sub-Saharan Africa, since followed by a trial of a similar intervention in rural Uganda,11 to demonstrate community-level impacts of a violence prevention intervention. This analysis further demonstrates that community mobilisation interventions have the potential to prevent both new onset of IPV among those with no prior experience of abuse and continuation of IPV where it was already occurring. These dual routes to prevention appear to validate the approach of engaging entire communities and using multiple strategies—for example, challenging existing norms, improving community responses and improving relationship dynamics—to achieve change. It is also encouraging to see that effects were observed across the spectrum of types of abuse, not just restricted to physical and sexual IPV. Some have posited that emotional abuse or controlling behaviours may provide an alternative outlet for a man who has stopped using physical or sexual violence, and could potentially increase as an unintended consequence of violence prevention programming. The fact that SASA! reduced all types of abuse might be attributed to its core focus on power and power imbalances. By tackling the underlying causes of IPV rather than its distinct manifestations, the scope of behaviours on which it impacted was likely increased.
SASA! is currently being delivered in control communities and replicated in 14 countries. Further research and investment is now urgently needed to support this process and better understand whether, and if so how, similar impacts can be achieved in other settings and on a larger scale.
What is already known on this subject.
Little is known about how to prevent intimate partner violence (IPV) against women. Evidence on extant violence interventions disproportionately comes from high-income countries, and is skewed towards evaluations of responses to violence rather than prevention. Recent evidence from sub-Saharan Africa, including earlier analysis from the SASA! Study, shows that community-based interventions can prevent IPV by addressing the underlying contexts in which violence occurs. However, little is understood about the breadth of impacts such interventions may have on different types of abuse.
What this study adds?
Community mobilisation interventions can be an effective means of preventing diverse types of abuse, including physical IPV, sexual IPV, emotional aggression and controlling behaviours. This broad scope of impacts lends support for the more wide scale adoption of interventions which seek to tackle the underlying causes of IPV, such as gender inequality and norms supportive of violence against women, rather than focusing too heavily on specific behaviours. Furthermore, community mobilisation—which uses multiple strategies to engage entire communities—can prevent both new onset of IPV, and continuation of violence where it was already occurring.
Supplementary Material
Acknowledgments
Many people, both within and outside these institutions, have helped to make this study possible. The authors thank the staff at Raising Voices and CEDOVIP, who have not only been responsible for the design and implementation of the SASA! intervention, but also tirelessly supported the research process, working with community leaders to gain consent for the study, participating in questionnaire design, training interviewers, conducting monitoring and evaluation activities and qualitative research as well as providing administrative support. Particularly, Winnie Amono, Gladys Rachiu, Clinton Okecha, Dipak Naker, Josephine Kamisya, Hope Turyasingura, Yvette Alal, Peter Wateya, Deus Kiwanuka, Denis Kizito Odok, Olive Nabisubi, Paul Buuzibwa and Rose Muduwa. Staff at the Uganda Bureau of Statistics (UBOS) were invaluable in the preparations for the surveys, both providing administrative maps and helping to recruit trained mappers to conduct the mapping exercises. The authors would also like to thank Basil Wanzira and Mabel Luzze who led the data collection and data management for the baseline survey, and Julius Lwanyaaga, Barbrah Nanyunja, Barbara Athieno, Miriam Dhikusooka, Josephine Namatovu, Angella Beatrice Nalwanga, Edgar Karungi and Betty Katengeke who led the data collection and data management for the follow-up survey. Though there are too many to list here, many thanks go to all of the researchers and data entry staff who spent months collecting and organising the data. They are also grateful to the local advisory committee, including Jessica Nkuuhe, Dr Consolata Kabonesa, Mubarak Mabuya, Helen Nviiri and Dr Freddie Ssengooba, who offered valuable feedback and advice during the design and conceptualisation of the SASA! study. Among colleagues at the London School of Hygiene and Tropical Medicine, the authors would like to thank Dr James Hargreaves and colleagues at the Centre for Evaluation, and Professor Richard Hayes for advice on aspects of study design and statistical methods for cluster randomised trials. They are extremely grateful also to the men and women who have been surveyed for the study, who graciously shared their time and stories. They would especially like to acknowledge all of the Raising Voices and CEDOVIP staff and community activists also, who work tirelessly to prevent violence in their communities. It is only through their hard work and commitment to transforming gender relationships and ending violence, that the impacts documented in this study have been achieved.
Correction notice: This article has been corrected since it was published Online First. The funding information has been updated.
Contributors: CW, LM and TM are principal investigators on the study, responsible for the overall conceptualisation, design and management of the study. TA and KMD are social epidemiologists responsible for major aspects of study design, sampling, development of research instruments, interviewer training and supervision of the quantitative survey. JN has input to the development and implementation of monitoring and evaluation instruments, the development of the follow-up questionnaire, and interviewer training, as well as being involved in baseline data collection and data management, and implementation and supervision of the follow-up survey. NK is the social scientist leading the qualitative research and analysis as well as inputting into the development of the follow-up questionnaire, interviewer training and implementation and supervision of the follow-up survey. TA drafted the manuscript and conducted the statistical analysis for this paper. All authors have commented on and offered edits to the original draft, and all have read and approved the final version.
Funding: The analysis and writing of this article was supported by an anonymous donor and the STRIVE RPC, an international research consortium funded by the UK Department for International Development (DFID) to investigate structural drivers of HIV. The authors would like to thank Irish Aid, the Sigrid Rausing Trust, 3ie (International Initiative for Impact Evaluations), an anonymous donor, AusAID and the Stephen Lewis Foundation, for providing funding for this research, and Irish Aid, American Jewish World Service, HIVOS, and the NoVo Foundation for supporting the implementation and monitoring of SASA! in the study communities. The views expressed are those of the authors alone.
Competing interests: LM is co-Director of Raising Voices and designed the SASA! intervention. JN is the Monitoring and Evaluation Officer for Raising Voices. TM is the Director of CEDOVIP and in charge of the implementation of the SASA! intervention being evaluated. They have played a central role in ensuring the appropriate conceptualisation and implementation of the evaluation, including the topics covered in the study questionnaire, the implementation of the fieldwork, and ensuring the provision of support to women requesting assistance. They have input into the interpretation of the findings.
Patient consent: Obtained.
Ethics approval: London School of Hygiene and Tropical Medicine, Makerere University, Uganda National Council of Science and Technology.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data from the follow-up survey and limited data from the baseline survey will be made available on the London School of Hygiene and Tropical Medicine data repository by the beginning of 2016.
References
- 1.Devries KM, Mak JY, Bacchus LJ, et al. . Intimate partner violence and incident depressive symptoms and suicide attempts: a systematic review of longitudinal studies. PLoS Med 2013;10:e1001439 10.1371/journal.pmed.1001439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jewkes RK, Dunkle K, Nduna M, et al. . Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: a cohort study. Lancet 2010;376:41–8. 10.1016/S0140-6736(10)60548-X [DOI] [PubMed] [Google Scholar]
- 3.Kouyoumdjian FG, Calzavara LM, Bondy SJ, et al. . Intimate partner violence is associated with incident HIV infection in women in Uganda. AIDS 2013;27:1331–8. 10.1097/QAD.0b013e32835fd851 [DOI] [PubMed] [Google Scholar]
- 4.Devries KM, Mak JY, Garcia-Moreno C, et al. . Global health. The global prevalence of intimate partner violence against women. Science 2013;340:1527–8. 10.1126/science.1240937 [DOI] [PubMed] [Google Scholar]
- 5.Ellsberg M, Arango DJ, Morton M, et al. . Prevention of violence against women and girls: what does the evidence say? Lancet 2015;385:1555–66. 10.1016/S0140-6736(14)61703-7 [DOI] [PubMed] [Google Scholar]
- 6.Garcia-Moreno C, Hegarty K, d'Oliveira AF, et al. . The health-systems response to violence against women. Lancet 2015;385:1567–79. 10.1016/S0140-6736(14)61837-7 [DOI] [PubMed] [Google Scholar]
- 7.Heise L. What works to prevent partner violence? An evidence overview. London: STRIVE Research Consortium, 2011. [Google Scholar]
- 8.Pronyk PM, Hargreaves JR, Kim JC, et al. . Effect of a structural intervention for the prevention of intimate-partner violence and HIV in rural South Africa: a cluster randomised trial. Lancet 2006;368:1973–83. 10.1016/S0140-6736(06)69744-4 [DOI] [PubMed] [Google Scholar]
- 9.Jewkes R, Nduna M, Levin J, et al. . Impact of stepping stones on incidence of HIV and HSV-2 and sexual behaviour in rural South Africa: cluster randomised controlled trial. BMJ 2008;337:a506 10.1136/bmj.a506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hossain M, Zimmerman C, Kiss L, et al. . Working with men to prevent intimate partner violence in a conflict-affected setting: a pilot cluster randomized controlled trial in rural Cote d'Ivoire. BMC Public Health 2014;14:339 10.1186/1471-2458-14-339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wagman JA, Gray RH, Campbell JC, et al. . Effectiveness of an integrated intimate partner violence and HIV prevention intervention in Rakai, Uganda: analysis of an intervention in an existing cluster randomised cohort. Lancet Glob Health 2015;3:e23–33. 10.1016/S2214-109X(14)70344-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abramsky T, Devries KM, Kiss L, et al. . Findings from the SASA! Study: a cluster randomized controlled trial to assess the impact of a community mobilization intervention to prevent violence against women and reduce HIV risk in Kampala, Uganda. BMC Med 2014;12:122 10.1186/s12916-014-0122-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Krug EG, Mercy JA, Dahlberg LL, et al. . The world report on violence and health. Lancet 2002;360:1083–8. 10.1016/S0140-6736(02)11133-0 [DOI] [PubMed] [Google Scholar]
- 14.Coker AL, Smith PH, Bethea L, et al. . Physical health consequences of physical and psychological intimate partner violence. Arch Fam Med 2000;9:451–7. 10.1001/archfami.9.5.451 [DOI] [PubMed] [Google Scholar]
- 15.Porcerelli JH, West PA, Binienda J, et al. . Physical and psychological symptoms in emotionally abused and non-abused women. J Am Board Fam Med 2006;19:201–4. 10.3122/jabfm.19.2.201 [DOI] [PubMed] [Google Scholar]
- 16.Mouton CP, Rodabough RJ, Rovi SL, et al. . Psychosocial effects of physical and verbal abuse in postmenopausal women. Ann Fam Med 2010;8:206–13. 10.1370/afm.1095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ludermir AB, Schraiber LB, D'Oliveira AF, et al. . Violence against women by their intimate partner and common mental disorders. Soc Sci Med 2008;66:1008–18. 10.1016/j.socscimed.2007.10.021 [DOI] [PubMed] [Google Scholar]
- 18.Yoshihama M, Horrocks J, Kamano S. The role of emotional abuse in intimate partner violence and health among women in Yokohama, Japan. Am J Public Health 2009;99:647–53. 10.2105/AJPH.2007.118976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jewkes R. Emotional abuse: a neglected dimension of partner violence. Lancet 2010;376:851–2. 10.1016/S0140-6736(10)61079-3 [DOI] [PubMed] [Google Scholar]
- 20.Abramsky T, Francisco L, Kiss L, et al. . SASA! Baseline report. Kampala: Raising Voices, London School of Hygiene and Tropical Medicine, 2010. [Google Scholar]
- 21.Michau L. The SASA ! Activist Kit for Preventing Violence against Women and HIV . Kampala, Uganda: Raising Voices, 2008. [Google Scholar]
- 22.Heise LL. Violence against women: an integrated, ecological framework. Violence Against Women 1998;4:262–90. 10.1177/1077801298004003002 [DOI] [PubMed] [Google Scholar]
- 23.Prochaska JO, Diclemente CC, Norcross JC. In search of how people change—applications to addictive behaviors. Am Psychol 1992;47:1102–14. 10.1037/0003-066X.47.9.1102 [DOI] [PubMed] [Google Scholar]
- 24.Abramsky T, Devries K, Kiss L, et al. . A community mobilisation intervention to prevent violence against women and reduce HIV/AIDS risk in Kampala, Uganda (the SASA! Study): study protocol for a cluster randomised controlled trial. Trials 2012;13:96 10.1186/1745-6215-13-96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hayes RJ, Bennett S. Simple sample size calculation for cluster randomised trials. Int J Epidemiol 1999;28:319 10.1093/ije/28.2.319 [DOI] [PubMed] [Google Scholar]
- 26.Watts C, Heise L, Ellsberg M, et al. . Putting women's safety first: ethical and safety recommendations for research on domestic violence against women. Geneva: World Health Organization, 1999. [Google Scholar]
- 27.Garcia-Moreno C, Jansen H, Ellsberg M, et al. . WHO multi-country study on womens health and domestic violence against women. Geneva: WHO, 2005. [Google Scholar]
- 28.Uganda Bureau of Statistics (UBOS) and Macro International Inc. Uganda Demographic and Health Survey 2006. Calverton, Maryland, USA: UBOS and Macro International Inc, 2007. [Google Scholar]
- 29.Measure DHS. Demographic and Health Surveys questionnaire modules (English, French). http://dhsprogram.com/publications/publication-dhsqm-dhs-questionnaires-and-manuals.cfm. (accessed 23 Nov 2015).
- 30.Habicht JP, Victora CG, Vaughan JP. Evaluation designs for adequacy, plausibility and probability of public health programme performance and impact. Int J Epidemiol 1999;28:10–18. 10.1093/ije/28.1.10 [DOI] [PubMed] [Google Scholar]
- 31.Kyegombe N, Starmann E, Devries KM, et al. . ‘SASA! is the medicine that treats violence’. Qualitative findings on how a community mobilisation intervention to prevent violence against women created change in Kampala, Uganda. Glob Health Action 2014;7:25082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ellsberg M, Heise L, Pena R, et al. . Researching domestic violence against women: methodological and ethical considerations. Stud Fam Plann 2001; 32:1–16. 10.1111/j.1728-4465.2001.00001.x [DOI] [PubMed] [Google Scholar]
- 33.Ellsberg M, Heise L. The challenge of defining and measuring violence in quantitative research. Researching violence against women: a practical guide for researchers and activists. Washington DC, USA: World Health Organisation, PATH, 2005. [Google Scholar]
- 34.Domestic Violence Act 2010. The Republic of Uganda. http://www.ilo.org/wcmsp5/groups/public/---ed_protect/---protrav/---ilo_aids/documents/legaldocument/wcms_172625.pdf (accessed 23 Nov 2015).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.