Introduction
Patellofemoral pain affects physically active and sedentary individuals, accounting for 11–17% of knee pain presentations to general practice1 2 and 25–40% of all knee problems seen in a sports injury clinic.3 4 Patellofemoral pain is characterised by anterior knee pain associated with activities such as squatting, rising from sitting and stair ambulation. While traditionally viewed as self-limiting, increasing research data suggest that patellofemoral pain is often recalcitrant and can persist for many years,5–8 and may cause a decline in sports participation.8 9
Despite its high prevalence among active individuals9–12 and frequent presentations for treatment, there are few published guidelines to help clinicians choose the appropriate evidence-based treatment for patellofemoral pain. The most recent and relevant paper from Barton and colleagues13 combined systematic review findings with qualitative interviews from expert clinicians to provide a clinically relevant synthesis, covering the literature up to September 2013. At the International Patellofemoral Pain Research Retreat in Manchester 2015, we held a consensus meeting to update the current evidence base and produce consensus-based recommendations regarding treatment for patellofemoral pain. All retreat registrants were active researchers in patellofemoral pain and presented their research findings. Many of the world leading researchers (eg, 8 out of the top 10 researchers with the highest number of publications, when the term ‘patellofemoral pain’ was searched in Scopus, February 2016) were in attendance and contributed to the consensus meeting.
The consensus meeting during the retreat resulted in recommendations, based on evidence published between January 2010 and June 2015. These recommendations should be combined with information gathered from individual patients, regarding their preferences, experiences, presentation and values, along with the values, expertise and skills of individual practitioners to create a patient-centred treatment approach.
Methods
Literature review
CJB searched EMBASE, MEDLINE, CINAHL and Current Contents for systematic reviews and randomised controlled trials (RCTs) published between January 2010 and June 2015. To be eligible, publications were (i) the most current systematic reviews including meta-analyses and (ii) any RCTs published subsequent to the most recent systematic review.
Search terms used to search titles and abstracts of papers relating to patellofemoral pain in each database were (patella or patellofemoral) and (pain or syndrome or dysfunction).13 To narrow the search to identify systematic reviews, these diagnostic terms were combined with the keyword review.
To narrow the search to identify any contemporary randomised trials, diagnostic terms were combined with (controlled trial or clinical trial) and additional searching was completed in the Physiotherapy Evidence Database (PEDro). Additionally, all authors on this consensus statement were consulted to identify any missing papers. To be included, randomised trials were required to evaluate one or more conservative intervention compared with a control or alternative conservative intervention, using an outcome measure related to pain (eg, pain visual analogue scale (VAS)) or patient-reported improvement, and using a randomised method for group allocation.
Data were extracted from each included paper. Where multiple systematic reviews were available for the same intervention from the same time period, findings from moderate–high quality reviews were used in preference to low-quality reviews. If no systematic reviews were available, all published RCTs related to the intervention were included. Findings from included reviews and trials were used to generate a summary table, which included study methodology, relevant outcomes and effect sizes.
The methodological quality of meta-analyses and systematic reviews was graded with the Assessment of Multiple Systematic Reviews (AMSTAR) tool; and RCTs were graded with the PEDro rating scale. Rating was completed by two independent reviewers (CJB and MvM), and discrepancies resolved through a consensus meeting. A third reviewer (KMC) was available to settle any disagreement but was not required.
Quality of evidence
For systematic reviews, the following allocation was applied based on AMSTAR scores:
High quality (HQ): ≥7
Moderate quality (MQ): 4–6
Low quality (LQ): ≤3
For RCTs, the following allocation was applied based on PEDro scores:
High quality (HQ): ≥7
Moderate quality (MQ): 4–6
Low quality (LQ): ≤3
Expert panel
The patellofemoral pain expert panel was composed of 35 of the 50 attendees at the 2015 International Patellofemoral Research Retreat (Manchester). All attendees were actively researching patellofemoral pain and included physiotherapists, doctors, podiatrists, biomechanists, epidemiologists and sports therapists.
Recommendations
Literature summary tables were developed by the consensus group (KMC, MvM, MJC, NJC, MSR, CJB) and distributed to all panel members prior to the consensus meeting. The summaries contained the quality ratings and effect sizes. Duration of treatment effect was classified as follows: <6 months considered short term, between 6 and 12 months was medium term and >12 months considered long term, unless otherwise defined in the systematic review. Statements were generated by the consensus group regarding each intervention, which reflected the evidence, and with respect to the interventions’ effect on pain, function and overall symptomatic improvement (ie, global rating of change). The panel was instructed to vote on the appropriateness of each statement.
The panel was instructed to integrate the evidence for each intervention with their expert opinions and knowledge in order to interpret the appropriateness of each intervention. At the Research Retreat, a 1-hour discussion of the summary tables (led by the consensus group) enabled clarification of the study elements, and finalisation of the statements. Following the discussion, panel members voted on the appropriateness of each intervention.
Voting and scoring
A 10-point scale (0–9, where 0 is ‘not appropriate’ and 9 is ‘appropriate’) was used to evaluate the appropriateness of each intervention. This scale was based on one similar previously used to generate the Osteoarthritis Research Society International (OARSI) guidelines for the non-surgical management of knee osteoarthritis.14
| Not appropriate | Appropriate | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
A pooled score provided a median appropriateness score for each intervention. A score of 0–3 was considered ‘inappropriate’, 4–6 ‘uncertain’ and 7–9 ‘appropriate’.
Final recommendations
Final recommendations were made on interventions where the outcome was consistent between voting and the evidence associated with this statement.
Results
The initial literature search for systematic reviews yielded 586 citations. Following screening for eligibility, a total of 22 systematic reviews were identified. Consultation with consensus authors did not yield any additional reviews. The interventions were grouped into the following: (i) exercise therapy (with separate sections for exercise therapy targeting specific bodily regions, ie, knee or hip); (ii) combined interventions (combining two or more of exercise therapy, patellar taping, mobilisation or foot orthoses); (iii) foot orthoses (in-shoe orthotic devices); (iv) patellar taping and bracing and (v) other adjunctive interventions (eg, acupuncture, mobilisation, electrophysical agents). Some of the reviews covered several interventions.
Available systematic reviews and available evidence
This included 13 (5 moderate; 1 high quality) reviews related to exercise therapy, 2 (1 moderate quality) related to combined interventions, 5 (3 moderate; 1 high quality) related to foot orthoses, 4 (2 moderate; 1 high quality) related to patellar taping and bracing, and 7 (2 moderate quality) related to other adjunctive interventions. AMSTAR ratings for each of these systematic reviews and the search date included in their methods are outlined in table 1.
Table 1.
AMSTAR quality assessment of included systematic reviews
| Systematic review | Score per AMSTAR item | Total score | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| i | ii | iii | iv | v | vi | vii | viii | ix | x | xi | Search date | ||
| Exercise therapy | |||||||||||||
| Bolgla and Boling15 | 0 | CA | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 2010—December |
| Clijsen et al16 | 0 | CA | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 5 | 2013—December |
| Collins et al17 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 4 | 2009—November |
| Frye et al18 | 0 | CA | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 2010—September |
| Harvie et al 19 | 0 | CA | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 2 | 2010—January |
| Kooiker et al20 | 0 | CA | 1 | CA | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 6 | 2014—January |
| Lack et al21 | 0 | CA | 1 | CA | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 4 | 2014—December |
| Nobre22 | 0 | CA | 0 | CA | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2011—Unclear |
| Page23 | 0 | CA | 0 | CA | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2010—August |
| Peters and Tyson24 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 3 | 2013—January |
| Regelski et al25 | 0 | CA | 0 | 0 | 0 | 0 | 1 | CA | 0 | 0 | 0 | 1 | Unclear |
| van der Heijden et al26 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 10 | 2014—May |
| Wasielewki 2011 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 6 | 2010—Unclear |
| Combined intervention | |||||||||||||
| Bolgla et al15 | 0 | CA | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 2010—December |
| Collins et al17 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 4 | 2009—November |
| Foot orthoses | |||||||||||||
| Barton et al27 | 0 | CA | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 6 | 2008—December |
| Bolgla et al15 | 0 | CA | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 2010—December |
| Collins et al17 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 4 | 2009—November |
| Hossain et al28 | 1 | 1 | 1 | CA | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 8 | 2010—March |
| Swart et al29 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 6 | 2010—January |
| Patellar taping and bracing | |||||||||||||
| Barton et al30 | 0 | CA | 1 | CA | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 4 | 2013—January |
| Callaghan and Selfe31 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 9 | 2011—August |
| Kalron and Bar-Sela32 | 0 | CA | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 3 | 2012—March |
| Swart et al29 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 6 | 2010—January |
| Other adjunctive interventions | |||||||||||||
| Bolgla et al15 | 0 | CA | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 2010—December |
| Brantingham et al 33 | 0 | CA | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2011—May |
| Collins et al17 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 4 | 2009—November |
| Dos Santos et al34 | 0 | CA | 0 | CA | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2011—Unclear |
| Lake and Wofford35 | 0 | CA | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 2 | 2010—August |
| Wasielewskiet al36 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 6 | 2010—Unclear |
Bold text=Reviews considered to be moderate or high quality.
i=‘a priori’ design; ii=duplicate study selection and data extraction; iii=comprehensive literature search; iv=search for grey literature; v=list of studies included and excluded provided; vi=characteristics of included studies provided; vii=scientific quality assessed; viii=scientific quality used to formulate conclusions; ix=methods to combine study findings appropriate; x=publication bias assessed; xi=conflict of interest.
0, no; 1, yes; AMSTAR, Assessment of Multiple Systematic Reviews; CA, cannot assess.
Additional RCT evidence
Subsequent searching for RCTs since 2010 revealed an additional 1631 citations. After taking into account the literature covered by included systematic reviews, 36 of these were considered for inclusion. Of these 36, an additional 7 randomised trials were identified. These included 1 on exercise therapy, 2 on combined interventions, 2 on foot orthoses, 1 on patellar taping and 1 on other adjunctive interventions. PEDro ratings for each of these trials are outlined in table 2.
Table 2.
PEDro quality assessment of included RCTs
| Study | Score per PEDro item | Total score | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| i* | ii | iii | iv | v | vi | vii | viii | ix | x | xi | ||
| Exercise therapy | ||||||||||||
| Ferber et al37 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 5 |
| Combined intervention | ||||||||||||
| Mason et al38 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 4 |
| Rathleff et al39 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Foot orthoses | ||||||||||||
| Lewinson et al40 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
| Mills et al41 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 9 |
| Patellar taping and bracing | ||||||||||||
| Osorio et al42 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4 |
| Other adjunctive interventions | ||||||||||||
| Hains and Hains43 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 9 |
i=eligibility criteria; ii=random allocation; iii=concealed allocation; iv=baseline comparability; v=blind subjects; vi=blind therapists; vii=blind assessors; viii=adequate follow-up; ix intention-to-treat analysis; x=between-group comparisons; xi=point estimates and variability.
*Eligibility criteria item does not contribute to total score.
0, no or unable to determine; 1, yes; PEDro, Physiotherapy Evidence Database; RCTs, randomised controlled trials.
Recommendations
Twenty-four statements (separated into time points and primary outcomes) were voted on by the panel.
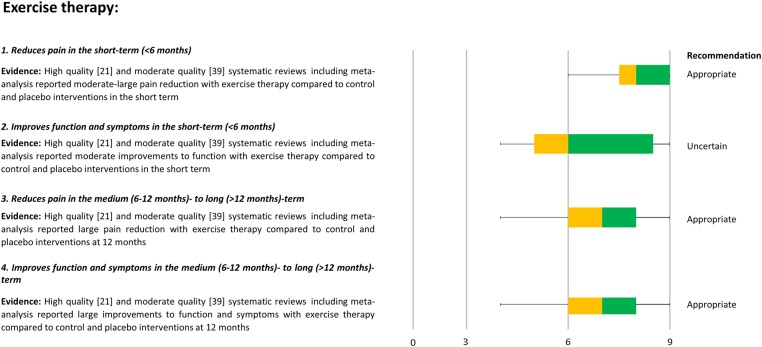
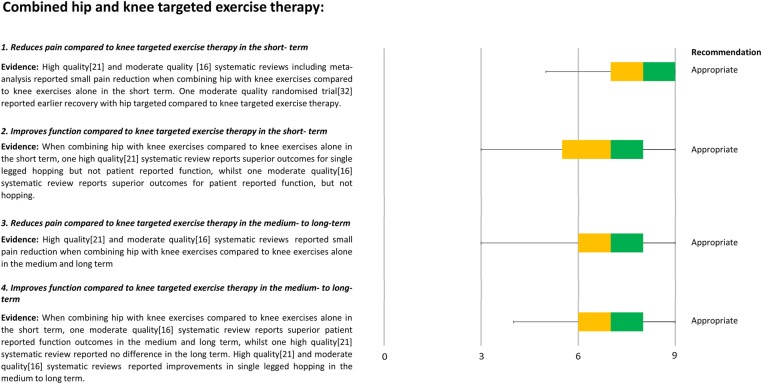
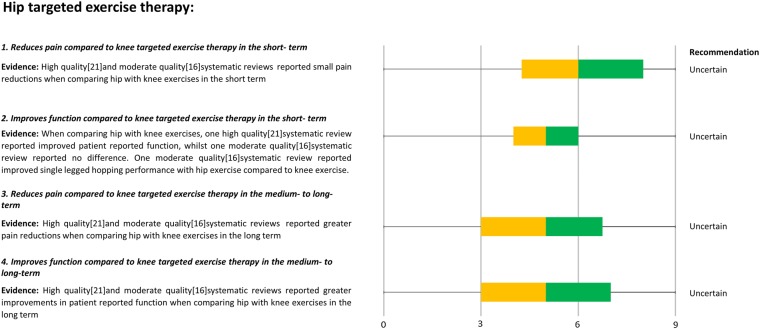
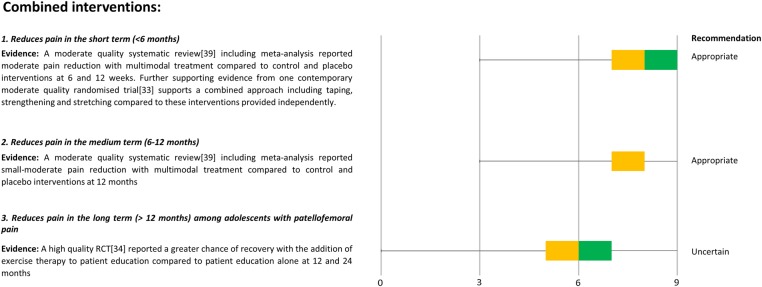
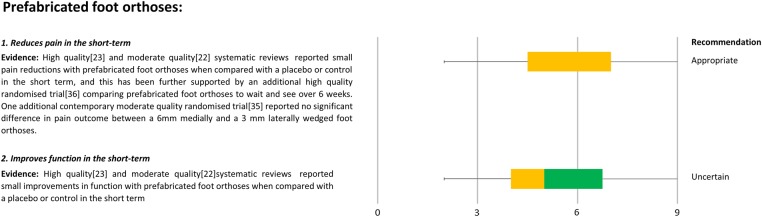
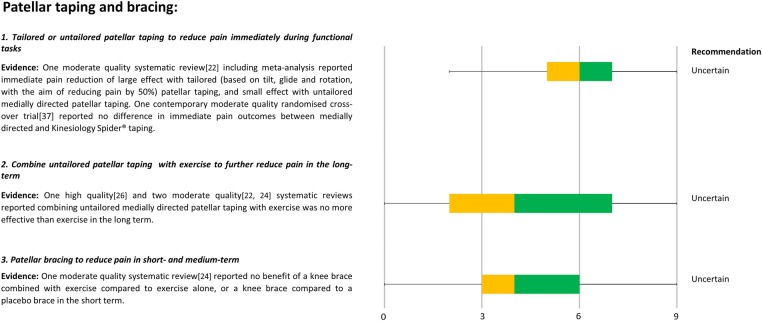
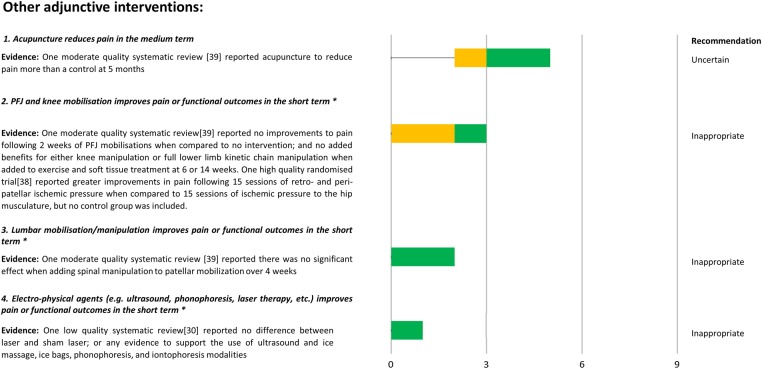
Results of this and associated evidence are outlined in figures 1–7, including 12 statements related to exercise therapy (figures 1–3), 3 statements related to combined interventions (figure 4), 2 statements related to foot orthoses (figure 5), 4 statements related to patellar taping and bracing (figure 6) and 4 statements related to other adjunctive interventions (figure 7).
Figure 1.
Synthesis of current evidence with consensus voting and recommendations for exercise therapy. First quartile=left whisker; second quartile=yellow box; median=yellow and green box intersection; third quartile=green box; fourth quartile=right whisker.
Figure 2.
Synthesis of current evidence with consensus voting and recommendations for hip combined with knee targeted exercise therapy. First quartile=left whisker; second quartile=yellow box; median=yellow and green box intersection; third quartile=green box; fourth quartile=right whisker.
Figure 3.
Synthesis of current evidence with consensus voting and recommendations for hip targeted exercise therapy. First quartile=left whisker; second quartile=yellow box; median=yellow and green box intersection; third quartile=green box; fourth quartile=right whisker.
Figure 4.
Synthesis of current evidence with consensus voting and recommendations for combined interventions. First quartile=left whisker; second quartile=yellow box; median=yellow and green box intersection; third quartile=green box; fourth quartile=right whisker. RCT, randomised controlled trial.
Figure 5.
Synthesis of current evidence with consensus voting and recommendations for prefabricated foot orthoses. First quartile=left whisker; second quartile=yellow box; median=yellow and green box intersection; third quartile=green box; fourth quartile=right whisker.
Figure 6.
Synthesis of current evidence with consensus voting and recommendations for patellar taping and bracing. First quartile=left whisker; second quartile=yellow box; median=yellow and green box intersection; third quartile=green box; fourth quartile=right whisker.
Figure 7.
Synthesis of current evidence with consensus voting and recommendations for other adjunctive interventions. First quartile=left whisker; second quartile=yellow box; median=yellow and green box intersection; third quartile=green box; fourth quartile=right whisker. *Statement worded opposite for voting, that is, based on evidence (eg, does not improve pain).
Key areas of uncertainty included combined interventions for adolescents, prioritisation of hip or knee exercise, acupuncture and patellar taping and bracing. We can make six recommendations based on consistency between consensus voting and the current evidence:
Exercise therapy
Exercise is recommended to reduce pain in the short, medium and long term, and improve function in the medium and long term.
Combining hip and knee exercises is recommended to reduce pain and improve function in the short, medium and long term, and this combination should be used in preference to knee exercises alone.
Combined interventions
Combined interventions are recommended to reduce pain in adults with patellofemoral pain in the short and medium term.
Foot orthoses
Foot orthoses are recommended to reduce pain in the short term.
Other adjunctive interventions
Patellofemoral, knee and lumbar mobilisations may not improve outcomes.
Electrophysical agents may not improve outcomes.
Discussion
The International Patellofemoral Research Retreat Consensus meeting resulted in six evidence-based recommendations. These recommendations will guide medical and health practitioners when they treat patients with patellofemoral pain. Recommendations may also be taken up by patients, other care providers, and government agencies and other organisations responsible for funding patellofemoral pain treatment. The recommendations are not intended to standardise patient care, but to be used in combination with individualised assessments of patient's needs, preferences and presentations, and clinical expertise to inform patient-centred management.44
Six recommendations from the expert panel
The six recommendations were as follows:
Exercise-therapy is recommended to reduce pain in the short, medium and long term, and improve function in the medium and long term.
Combining hip and knee exercises is recommended to reduce pain and improve function in the short, medium and long term, and this combination should be used in preference to knee exercises alone.
Combined interventions are recommended to reduce pain in adults with patellofemoral pain in the short and medium term.
Foot orthoses are recommended to reduce pain in the short term.
Patellofemoral, knee and lumbar mobilisations are not recommended.
Electrophysical agents are not recommended.
Our recommendations differ from those described in the ‘Best Practice Guide to Conservative Management of Patellofemoral Pain’.13 The best practice guide did not recommend exercise therapy as a stand-alone treatment, but recommended consideration of acupuncture, and provided no recommendations regarding treatments which may not improve outcomes. These differences likely reflect the qualitative input from clinicians in the paper.13 In contrast, the consensus voting that led to our recommendations involved some researchers who had a clinical role and some who did not. For example, it appears that clinicians have a stronger preference for combined interventions (using a combination of exercise therapy, targeting knee and hip musculature, patellofemoral taping, mobilisation and foot orthoses), which was a recommendation from our consensus, than for stand-alone treatments, such as exercise therapy. However, exercise therapy has been evaluated considerably within the scientific literature and remains a recommendation as a stand-alone treatment from our consensus based on the strength of evidence supporting it. In contrast, interventions such as acupuncture have very limited supporting evidence. Appropriateness of acupuncture was voted as uncertain, and hence was not recommended in the current consensus meeting. However, acupuncture is frequently used by clinicians who treat patellofemoral pain, and this highlights a nexus between evidence and practice which requires high-quality clinical trials. The consensus meeting has also made recommendations against interventions such as mobilisation and electrotherapy, which current evidence indicates are ineffective. The consensus meeting was also unable to make any recommendations related to patient education in isolation, due to a paucity of research in this area. Considering the perceived importance of providing patient education from clinicians,13 further research and development on patient education interventions is encouraged.
Exercise therapy: the treatment of choice
Exercise therapies had the most statements in support of their short-term, medium-term and long-term use, reflecting the large body of evidence underpinning this treatment. Exercise therapy was the only intervention tested in isolation to be supported by the expert group. The evidence clearly shows that exercise therapy is effective, regardless of the type of exercise (eg, in weight bearing or not; targeting hip or knee). There was also support for emerging but convincing evidence that combining a hip-focused with knee-focused exercise therapy regimen resulted in superior outcomes to isolated knee-focused exercise therapy. This is consistent with results from the combined intervention studies, which have included hip-focused and knee-focused exercise therapies. The uncertainty around the superiority of hip-focused when compared head-to-head with knee-focused treatments may reflect lack of clarity regarding implementation of targeted exercise therapies, and the potential for the reported exercise therapy regimens to truly only target either the hip or the knee. For example, knee-focused programmes including single-leg squatting or stair climbing activities will also target the hip, while standing exercises to target the hip with resistance will also involve a knee focus on the weight-bearing limb.
The terms ‘exercise’ and ‘exercise therapy’ were discussed at length at the meeting. There is distinct lack of clarity regarding the taxonomy and reporting of exercise therapy treatments. Even when well reported, the type of exercise in the current evidence base varies with respect to the targets of the exercise (eg, strength, cardiovascular fitness, coordination/neuromuscular retraining).21 Furthermore, measurement of the effectiveness of such interventions to achieve their target, such as increasing strength, endurance and neuromuscular coordination, was rarely undertaken. Perhaps most importantly, the lack of detailed description of the exercise therapy interventions limits the translation of the research findings into clinical practice. This lack of reporting rigour for exercise therapy extends to other interventions described in this consensus statement. As a result of this discussion, a recommendation was made to adopt minimum reporting standards for patellofemoral pain studies, similar to those published for groin pain studies,45 and these standards are published by Morrisey et al.
Combined interventions
Combined interventions (combining exercise therapy, targeting knee and hip musculature, patellofemoral taping, mobilisation and foot orthoses) were considered appropriate for patients with patellofemoral pain, which is consistent with the strongest recommendation from the ‘Best Practice Guide’.13 A combined approach to management best reflects clinical practice and provides the treating practitioner with the scope to address a number of contributing factors (not just one in isolation). However, an important recommendation made in the ‘Best Practice Guide’ regarding combined interventions is the need to individualise treatments to each patient, as not all patients will require all treatments.13 Current research evidence to guide the tailoring of interventions is very limited,46 and efforts to address this are encouraged. Uncertainty around the recommendation supporting combined interventions for adolescents with patellofemoral pain most likely reflected the lack of studies, as there is currently only one RCT39 and no systematic reviews. Outcomes for adolescents were consistent with the pooled standardised mean difference (SMD) for a similar intervention in adults,47 but the overall rates of recovery after treatment may be lower in adolescents than in adults.48 We welcome further studies investigating treatment options in this group, especially given evidence of symptoms persisting well beyond adolescence.49
Foot orthoses
Foot orthoses were recommended for short-term pain relief in people with patellofemoral pain, and this is consistent with the ‘Best Practice Guide’.13 However, an important consideration is that the average pain reduction facilitated by prefabricated foot orthoses may be considered to lack clinical significance, due to substantial individual variability in response.50 The key point is that foot orthoses may not be beneficial for all patients with patellofemoral pain, and identifying those most likely to benefit from foot orthoses is important. Published studies have reported clinical features that can be used to predict success with foot orthoses intervention, including greater midfoot mobility,41 51 less ankle dorsiflexion and immediate improvements in patellofemoral pain when performing a single-leg squat with foot orthoses.52
Patellar taping
Whether patellar taping should be first-line treatment for patellofemoral pain was unclear to this expert panel. This conclusion was consistent with the ‘Best Practice Guide’13 findings. Patellar taping approaches vary considerably with respect to the type and duration of taping, and the systematic reviews29–31 that synthesise these studies have dealt with the variability inconsistently. Lack of clarity from systematic reviews may partially explain the uncertainty around the consensus voting and associated recommendations to support patellar taping.
Uncertainty around the recommendations for taping might also reflect that greater consideration of individual patient needs may be required. For example, in Barton et al's13 synthesis, the experts described that targeting the taping to suit individual patient presentations was an important consideration. Patellar taping and bracing could play a role in patellofemoral pain management in combination with other treatments (ie, as part of a combined intervention as described above), but their role in isolation is yet to be fully determined. Other adjunctive treatments, such as joint mobilisations (patella, knee, lumbar), and electrophysical agents were not recommended for use in patellofemoral pain.
Limitations
Our consensus on physical and exercise treatments for patellofemoral pain was limited to the treatments with evidence regarding their usefulness. The inclusion of evidence stemming from moderate-quality and high-quality systematic reviews means that not all potentially valuable interventions were covered. For example, while gait retraining shows emerging evidence supporting its use in patellofemoral pain,53 more rigorous research is required before it can be considered as a recommended intervention.
Our expert panel self-selected participants who attended the International Patellofemoral Pain Research Retreat. While all participants were active in patellofemoral research and most of the productive researchers worldwide were in attendance, the panel was not specifically chosen, based on their expertise. The inclusion of researchers and clinicians is a strength (ensuring expertise with research methodology and respect for scientific rigour) as well as a limitation (some members have no experience in patient management). Furthermore, there was no patient input into the voting on our recommendations, and we recommend that their values and preferences be considered when applying recommendations clinically.44
Future directions
Our consensus group recommended some future directions regarding interventions for patellofemoral pain. We recognised the need for minimum reporting standards for clinical research on patellofemoral pain, similar to that published for groin pain in athletes,45 which is being undertaken. We recommended that future trials should publish details of the intervention in sufficient detail to enable clinicians to apply these in clinical practice (possibly as supplementary files). We require greater understanding of potential mechanisms underpinning treatment effects. We recognise that there is uncertainty regarding the usefulness of subgroups,54 or individualised (clinical reasoning) approaches to optimise treatments. As with all exercise interventions, adherence is paramount, and methods to advance adherence are urgently needed. It is still unclear which specific pain pathways (local and central pain mechanisms) are primarily involved in patellofemoral pain, but it appears that central pain mechanisms may be altered in people with patellofemoral pain.55–57 This clearly indicates the need to evaluate non-mechanical interventions to address these factors in some individuals. We recommend future trials investigating interventions for patellofemoral pain across the lifespan (ie, adolescents and those with patellofemoral osteoarthritis).
There was overarching support from the International Patellofemoral Pain Research Retreat for the Enhancing the QUality And Transparency Of health Research (EQUATOR) guidelines (http://www.equator-network.org) for reporting, and we encourage investigators to follow the appropriate reporting guideline in future patellofemoral pain publications.
Conclusion
The consensus meeting at the 4th International Patellofemoral Pain Research Retreat (Manchester 2015) provided six recommendations for use in patients with patellofemoral pain: exercise therapy, particularly combining hip and knee exercises, combined interventions and foot orthoses. Patellofemoral, knee and lumbar mobilisations and electrophysical agents were not recommended. The 5th International Patellofemoral Pain Research Retreat is scheduled for Brisbane, Australia, July 2017.
Footnotes
Twitter: Follow Christian Barton at @DrChrisBarton
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Wood L, Muller S, Peat G. The epidemiology of patellofemoral disorders in adulthood: a review of routine general practice morbidity recording. Prim Health Care Res Dev 2011;12:157–64. 10.1017/S1463423610000460 [DOI] [PubMed] [Google Scholar]
- 2.van Middelkoop M, van Linschoten R, Berger MY, et al. Knee complaints seen in general practice: active sport participants versus non-sport participants. BMC Musculoskelet Disord 2008;9:36 10.1186/1471-2474-9-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kannus P, Aho H, Järvinen M, et al. Computerised recording of visits to an outpatient sports clinic. Am J Sports Med 1987;15:79–85. [DOI] [PubMed] [Google Scholar]
- 4.Taunton JE, Ryan MB, Clement DB, et al. A retrospective case-control analysis of 2002 running injuries. Br J Sports Med 2002;36:95–101. 10.1136/bjsm.36.2.95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sandow MJ, Goodfellow JW. The natural history of anterior knee pain in adolescents. J Bone Joint Surg Br 1985;67:36–8. [DOI] [PubMed] [Google Scholar]
- 6.Lankhorst NE, van Middelkoop M, Crossley K, et al. Factors that predict a poor outcome 5–8 years after the diagnosis of patellofemoral pain: a multicentre observational analysis. Br J Sports Med 2016;50:881–86. 10.1136/bjsports-2015-094664 [DOI] [PubMed] [Google Scholar]
- 7.Collins NJ, Bierma-Zeinstra SM, Crossley KM, et al. Prognostic factors for patellofemoral pain: a multicentre observational analysis. Br J Sports Med 2013;47:227–33. 10.1136/bjsports-2012-091696 [DOI] [PubMed] [Google Scholar]
- 8.Rathleff MS, Rathleff CR, Olsen JL, et al. Is knee pain during adolescence a self-limiting condition?: prognosis of patellofemoral pain and other types of knee pain. Am J Sports Med 2016;44:1165–71. 10.1177/0363546515622456 [DOI] [PubMed] [Google Scholar]
- 9.Hall R, Barber Foss K, Hewett TE, et al. Sport specialization's association with an increased risk of developing anterior knee pain in adolescent female athletes. J Sport Rehabil 2015;24:31–5. 10.1123/jsr.2013-0101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Myer GD, Ford KR, Barber Foss KD, et al. The incidence and potential pathomechanics of patellofemoral pain in female athletes. Clin Biomech (Bristol, Avon) 2010;25(7):700–7. 10.1016/j.clinbiomech.2010.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rathleff MS, Skuldbøl SK, Rasch MN, et al. Care-seeking behaviour of adolescents with knee pain: a population-based study among 504 adolescents. BMC Musculoskelet Disord 2013;14:225 10.1186/1471-2474-14-225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boling M, Padua D, Marshall S, et al. Gender differences in the incidence and prevalence of patellofemoral pain syndrome. Scand J Med Sci Sports 2010;20:725–30. 10.1111/j.1600-0838.2009.00996.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barton CJ, Lack S, Hemmings S, et al. The ‘Best practice guide to conservative management of patellofemoral pain’: incorporating level 1 evidence with expert clinical reasoning. Br J Sports Med 2015;49:923–34. 10.1136/bjsports-2014-093637 [DOI] [PubMed] [Google Scholar]
- 14.McAlindon TE, Bannuru RR, Sullivan MC, et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis Cartilage 2014;22:363–88. 10.1016/j.joca.2014.01.003 [DOI] [PubMed] [Google Scholar]
- 15.Bolgla LA, Boling MC. An update for the conservative management of patellofemoral pain syndrome: a systematic review of the literature from 2000 to 2010. Int J Sports Phys Ther 2011;6:112–25. [PMC free article] [PubMed] [Google Scholar]
- 16.Clijsen R, Fuchs J, Taeymans J. Effectiveness of exercise therapy in treatment of patients with patellofemoral pain syndrome: systematic review and meta-analysis. Phys Ther 2014;94:1697–708. 10.2522/ptj.20130310 [DOI] [PubMed] [Google Scholar]
- 17.Collins NJ, Bisset LM, Crossley KM, et al. Efficacy of nonsurgical interventions for anterior knee pain systematic review and meta-analysis of randomized trials. Sports Med 2012;42:31–49. 10.2165/11594460-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 18.Frye JL, Ramey LN, Hart JM. The effects of exercise on decreasing pain and increasing function in patients with patellofemoral pain syndrome: a systematic review. Sports Health 2012;4:205–10. 10.1177/1941738112441915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harvie D, O'Leary T, Kumar S. A systematic review of randomized controlled trials on exercise parameters in the treatment of patellofemoral pain: what works? J Multidiscip Healthc 2011;4:383–92. 10.2147/JMDH.S24595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kooiker L, van de Port IG, Weir A, et al. Effects of physical therapist-guided quadriceps-strengthening exercises for the treatment of patellofemoral pain syndrome: a systematic review. J Orthop Sports Phys Ther 2014;44:391–B1. 10.2519/jospt.2014.4127 [DOI] [PubMed] [Google Scholar]
- 21.Lack S, Barton C, Sohan O, et al. Proximal Muscle Rehabilitation is effective for patellofemoral pain: a systematic review with meta-analysis. Br J Sports Med 2015;49:1365–76. 10.1136/bjsports-2015-094723 [DOI] [PubMed] [Google Scholar]
- 22.Nobre T. Comparison of exercise open kinetic chain and closed kinetic chain in the rehabilitation of patellofemoral dysfunction: an updated revision. Clin Med Diagn 2012;2:7–11. [Google Scholar]
- 23.Page P. Effectiveness of elastic resistance in rehabilitation of patients with patellofemoral pain syndrome: what is the evidence? Sports Health 2011;3: 190–4. 10.1177/1941738111398595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Peters JS, Tyson NL. Proximal exercises are effective in treating patellofemoral pain syndrome: a systematic review. Int J Sports Phys Ther 2013;8:689–700. [PMC free article] [PubMed] [Google Scholar]
- 25.Regelski C, Ford B, Hoch M. Hip strengthening compared with quadriceps strengthening in conservative treatment of patients with patellofemoral pain: a critically appraised topic. Int J Athl Ther Train 2015;20:4–12. 10.1123/ijatt.2014-0048 [DOI] [Google Scholar]
- 26.van der Heijden RA, Lankhorst NE, van Linschoten R, et al. Exercise for treating patellofemoral pain syndrome. Cochrane Database Syst Rev 2015;1:CD010387 10.1002/14651858.CD010387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Barton CJ, Munteanu SE, Menz HB, et al. The efficacy of foot orthoses in the treatment of individuals with patellofemoral pain syndrome: a systematic review. Sports Med 2010;40:377–95. 10.2165/11530780-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 28.Hossain M, Alexander P, Burls A, et al. Foot orthoses for patellofemoral pain in adults. Cochrane Database Syst Rev 2011;(1):CD008402 10.1002/14651858.CD008402.pub2 [DOI] [PubMed] [Google Scholar]
- 29.Swart NM, van Linschoten R, Bierma-Zeinstra SM, et al. The additional effect of orthotic devices on exercise therapy for patients with patellofemoral pain syndrome: a systematic review. Br J Sports Med 2012;46:570–7. 10.1136/bjsm.2010.080218 [DOI] [PubMed] [Google Scholar]
- 30.Barton C, Balachandar V, Lack S, et al. Patellar taping for patellofemoral pain: a systematic review and meta-analysis to evaluate clinical outcomes and biomechanical mechanisms. Br J Sports Med 2014;48:417–24. 10.1136/bjsports-2013-092437 [DOI] [PubMed] [Google Scholar]
- 31.Callaghan MJ, Selfe J. Patellar taping for patellofemoral pain syndrome in adults. Cochrane Database Syst Rev 2012;4:CD006717 10.1002/14651858.CD006717.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kalron A, Bar-Sela S. A systematic review of the effectiveness of Kinesio Taping—fact or fashion? Eur J Phys Rehabil Med 2013;49:699–709. [PubMed] [Google Scholar]
- 33.Brantingham JW, Bonnefin D, Perle SM, et al. Manipulative therapy for lower extremity conditions: update of a literature review. J Manipulative Physiol Ther 2012;35:127–66. 10.1016/j.jmpt.2012.01.001 [DOI] [PubMed] [Google Scholar]
- 34.Dos Santos R, Souza M, Dos Santos F. Neuromuscular electric stimulation in patellofemoral dysfunction: literature review. Acta Orthop Bras 2013;21:52–8. 10.1590/S1413-78522013000100011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lake DA, Wofford NH. Effect of therapeutic modalities on patients with patellofemoral pain syndrome: a systematic review. Sports Health 2011;3:182–9. 10.1177/1941738111398583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wasielewski NJ, Parker TM, Kotsko KM. Evaluation of electromyographic biofeedback for the quadriceps femoris: a systematic review. J Athl Train 2011;46:543–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ferber R, Bolgla L, Earl-Boehm JE, et al. Strengthening of the hip and core versus knee muscles for the treatment of patellofemoral pain: a multicenter randomized controlled trial. J Athl Train 2015;50:366–77. 10.4085/1062-6050-49.3.70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mason M, Keays SL, Newcombe PA. The effect of taping, quadriceps strengthening and stretching prescribed separately or combined on patellofemoral pain. Physiother Res Int 2011;16:109–19. 10.1002/pri.486 [DOI] [PubMed] [Google Scholar]
- 39.Rathleff MS, Roos EM, Olesen JL, et al. Exercise during school hours when added to patient education improves outcome for 2 years in adolescent patellofemoral pain: a cluster randomised trial. Br J Sports Med 2015;49:406–12. 10.1136/bjsports-2014-093929 [DOI] [PubMed] [Google Scholar]
- 40.Lewinson RT, Wiley JP, Humble RN, et al. Altering knee abduction angular impulse using wedged insoles for treatment of patellofemoral pain in runners: a six-week randomized controlled trial. PLoS ONE 2015;10:e0134461 10.1371/journal.pone.0134461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mills K, Blanch P, Dev P, et al. A randomised control trial of short term efficacy of in-shoe foot orthoses compared with a wait and see policy for anterior knee pain and the role of foot mobility. Br J Sports Med 2012;46:247–52. 10.1136/bjsports-2011-090204 [DOI] [PubMed] [Google Scholar]
- 42.Osorio JA, Vairo GL, Rozea GD, et al. The effects of two therapeutic patellofemoral taping techniques on strength, endurance, and pain responses. Phys Ther Sport 2013;14:199–206. 10.1016/j.ptsp.2012.09.006 [DOI] [PubMed] [Google Scholar]
- 43.Hains G, Hains F. Patellofemoral pain syndrome managed by ischemic compression to the trigger points located in the peri-patellar and retro-patellar areas: a randomized clinical trial. Clin Chiropr 2010;13:201–9. 10.1016/j.clch.2010.05.001 [DOI] [Google Scholar]
- 44.Barton CJ, Crossley KM. Sharing decision-making between patient and clinician: the next step in evidence-based practice for patellofemoral pain? Br J Sports Med 2016;50:833–4.. 10.1136/bjsports-2015-095607 [DOI] [PubMed] [Google Scholar]
- 45.Delahunt E, Thorborg K, Khan KM, et al. Minimum reporting standards for clinical research on groin pain in athletes. Br J Sports Med 2015;49:775–81. 10.1136/bjsports-2015-094839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lack S, Barton C, Vicenzino B, et al. Outcome predictors for conservative patellofemoral pain management: a systematic review and meta-analysis. Sports Med 2014;44:1703–16. 10.1007/s40279-014-0231-5 [DOI] [PubMed] [Google Scholar]
- 47.Collins NJ, Bisset LM, Crossley KM, et al. Efficacy of nonsurgical interventions for anterior knee pain: systematic review and meta-analysis of randomised trials. Sports Med 2012;42:31–49. 10.2165/11594460-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 48.Rathleff MS, Vicenzino B, Middelkoop M, et al. Patellofemoral pain in adolescence and adulthood: same same, but different? Sports Med 2015;45:1489–95. 10.1007/s40279-015-0364-1 [DOI] [PubMed] [Google Scholar]
- 49.Nimon G, Murray D, Sandow M, et al. Natural history of anterior knee pain: a 14- to 20-year follow-up of nonoperative management. J Pediatr Orthop 1998;18:118–22. [PubMed] [Google Scholar]
- 50.Collins N, Crossley K, Beller E, et al. Foot orthoses and physiotherapy in the treatment of patellofemoral pain syndrome: randomised clinical trial. BMJ 2008; 337:a1735 10.1136/bmj.a1310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vicenzino B, Collins N, Cleland J, et al. A clinical prediction rule for identifying patients with patellofemoral pain who are likely to benefit from foot orthoses: a preliminary determination. Br J Sports Med 2010;44: 862–6. 10.1136/bjsm.2008.052613 [DOI] [PubMed] [Google Scholar]
- 52.Barton CJ, Menz HB, Crossley KM. Clinical predictors of foot orthoses efficacy in individuals with patellofemoral pain. Med Sci Sports Exerc 2011;43: 1603–10. 10.1249/MSS.0b013e318211c45d [DOI] [PubMed] [Google Scholar]
- 53.Neal BS, Barton CJ, Gallie R, et al. Runners with patellofemoral pain have altered biomechanics which targeted interventions can modify: a systematic review. Gait Posture 2016;45:69–82. 10.1016/j.gaitpost.2015.11.018 [DOI] [PubMed] [Google Scholar]
- 54.Selfe J. “Measurement properties of patient-reported outcome measures (PROMS) in patellofemoral pain syndrome: a systematic review.” Green et al. (in press corrected proof). Man Ther 2015;20:e6 10.1016/j.math.2014.11.015 [DOI] [PubMed] [Google Scholar]
- 55.Rathleff MS, Roos EM, Olesen JL, et al. Lower mechanical pressure pain thresholds in female adolescents with patellofemoral pain syndrome. J Orthop Sports Phys Ther 2013;43:414–21. 10.2519/jospt.2013.4383 [DOI] [PubMed] [Google Scholar]
- 56.Rathleff MS, Petersen KK, Arendt-Nielsen L, et al. Impaired conditioned pain modulation in young female adults with long-standing patellofemoral pain: a single blinded cross-sectional study. Pain Med 2015;17:980–8. 10.1093/pm/pnv017 [DOI] [PubMed] [Google Scholar]
- 57.Noehren B, Shuping L, Jones A, et al. Somatosensory and biomechanical abnormalities in females with patellofemoral pain. Clin J Pain 2015. 10.1097/AJP.0000000000000331epub ahead of print PMID:26626291 [DOI] [PMC free article] [PubMed] [Google Scholar]