Abstract
Objective
Although children are frequently referred to subspecialist physicians, many inadequacies in referral processes have been identified from physician and system perspectives. Little is known, however, about how to comprehensively measure or improve the quality of the referral systems from a family-centered perspective. To foster family-centered improvements to pediatric subspecialty referrals, we sought to develop a framework for high-quality, patient-centered referrals from the perspectives of patients and their families.
Methods
We used stakeholder-informed qualitative analysis of parent, caregiver, and patient interviews to identify outcomes, processes, and structures of high-quality pediatric subspecialty referrals as perceived by patients and their family members.
Results
We interviewed 21 informants. Informants identified five desired outcomes of subspecialty referrals: improved functional status or symptoms; improved long-term outcomes; improved knowledge of their disease; informed expectations; and reduced anxiety about the child’s health status. Processes that informants identified as supporting these outcomes centered around six key steps in subspecialty referrals, including the referral decision, pre-visit information transfer, appointment scheduling, subspecialist visit, post-visit information transfer, and ongoing care integration and communication. Health care delivery structures identified by informants as supporting these processes included physical infrastructure, human resources, and information technology systems.
Conclusion
We identified family-centered outcomes, processes, and structures of high-quality pediatric subspecialty referrals. These domains can be used not only to improve measurement of the quality of existing referral systems but also to inform future interventions to improve patient-centered outcomes for children in need of specialty care.
Keywords: pediatric, subspecialty, specialty, referral, consultation, family-centered, patient-centered, quality, outcomes
Introduction
Subspecialty care is crucial to the health and well-being of many children, especially given rising rates of chronic illness in the pediatric population.1 Despite the importance of subspecialty consultation, both primary care providers (PCPs) and subspecialists identify numerous frustrations and inefficiencies with subspecialty referrals.2 Multiple studies demonstrate inadequate transfer of information between PCP and subspecialist, lack of coordination of care between PCP and subspecialist, and conflicting expectations regarding patient comanagement.2–5
Although such prior work identified clear targets for improvement in subspecialty referrals from the viewpoint of PCPs and subspecialists, less is known about the viewpoint of patients and families, particularly regarding the overall experience of subspecialty care. Prior studies have focused on parent perspectives of specific aspects of subspecialty referrals, such as information exchange, shared decision making, and continuity of care,6–8 but have not examined the broader experiences and preferences of families receiving subspecialty care. Relatedly, a recent systematic review found that the majority of measures in studies of subspecialty referrals focused on referral initiation, subspecialist accessibility, and appointment attendance rather than patient experiences, patient satisfaction, or health outcomes,9 indicating that family perspectives also received little weight in prior evaluations of subspecialty referrals. The Patient Centered Outcomes Research Institute and others have emphasized the importance of family perspectives in identifying appropriate patient and family-centered measures and defining value in pediatric health care systems.10–13 To ensure future health care system interventions lead to patient-centered improvements, it is important to understand referral quality from the perspectives of patients and their families, who are uniquely positioned to benefit from, or be harmed by, the referral experience.10–13 Without such knowledge, health care systems seeking to improve the quality of subspecialty referral systems risk developing interventions that are poorly informed and targeting endpoints that are not maximally relevant to patients and families.
To address this knowledge gap, we sought to identify the aspects of subspecialty referral systems that define a high-quality referral experience from the perspective of patients and families. Using stakeholder-guided semi-structured interviews, we elicited family experiences of successful and unsuccessful subspecialty referrals. Based on qualitative analysis of the interview transcripts, we identified family-centered outcomes, processes, and structures associated with high-quality pediatric subspecialty referrals and developed a family-centered conceptual model for use in future quality improvement and research initiatives.
Methods
We examined family experiences of subspecialty referrals though qualitative analysis of family member interviews (including parents, caregivers, and patients) informed by a stakeholder advisory group. Using recommended best practices for engaging stakeholders as research collaborators,14,15 we assembled a group of six individuals representing patients, parents/caregivers, providers, and payers, including individuals who self-identified as living in communities with poor access to pediatric subspecialty care. The purpose of this group was to optimize the relevance and interpretability of this work for a range of stakeholders. Stakeholders were consulted throughout the research process, guiding development of the interview guide, recruitment of participants, interpretation of results, and dissemination of findings.
We developed the interview guide through an iterative process informed by prior models of subspecialty care2,9,16 and refined through multiple discussions with our stakeholder advisory group and through pilot interviews. Interview guide domains included positive and negative experiences with subspecialty referrals, perceived benefits and costs of subspecialty referrals as well as patient and parent/caregiver decision making around subspecialty referrals. The interview guide was targeted to an interview length of between 30 and 60 minutes. A copy of the parent interview guide, which was modified for adolescents and young adults, is provided in the supplementary Appendix 1. Individual interviews were conducted by telephone from March 2015 to September 2015.
Subjects were recruited through an existing practice-based research network, Pediatric PittNet, which consists of 24 pediatric and adolescent primary care sites in six counties across Western Pennsylvania, including practices both near and far to subspecialty referral centers. Parents or other caregivers (with children ages 0–21 years old), young adults (ages 18–21 years old), and adolescents (ages 14–17 years old) who had ever been referred to a subspecialist were eligible for participation. Eligible parents/caregivers and young adults who presented for primary care visits at participating practices were notified of the study by practice physicians or care coordinators during their visits. For additional caregiver recruitment, we performed snowball sampling with caregiver interviewees. To recruit adolescents, we obtained caregiver permission to contact adolescents at the time of caregiver interviews and subsequently obtained assent from the adolescent. Throughout the recruitment process, we used purposeful sampling at the practice level to ensure diverse representation, including interviewees living both near and far from subspecialty care (by interviewee-reported travel time) as well as interviewees with both high and low subspecialty utilization (by self-reported number of visits). Participation was incentivized using a $25 gift card which was mailed to participants after interview completion.
All interviews were conducted by a trained investigator with experience in qualitative data collection (LEA). This individual obtained verbal consent prior to each interview. Interviews were recorded and transcribed with identifiers removed. Interview transcripts were analyzed using thematic content analysis,17 first identifying broad themes and subsequently differentiating subthemes. Two investigators (KNR and LEA) trained in qualitative methods coded all interviews. A preliminary codebook was developed based on the first five interviews. This codebook was reviewed by our stakeholder group to enhance reliability. Interviews were then coded by the two investigators, compared for agreement, and finalized through consensus. Coding was performed using NVIVO 10 (QSR, Melbourne, Australia).
We continued interviews until we reached thematic saturation.18 To increase the trustworthiness of our results, we performed two additional member checking steps. First, for parent/caregiver interviews in which the child in question was 14–21 years old, we also sought parental permission and child assent to interview the child to gain their complementary perspective as discussed above. Second, at the conclusion of coding, themes were again reviewed with our stakeholder group and refined based upon their feedback.
We then categorized themes and subthemes into three domains based on the Donabedian model of health care quality: outcomes, processes, and structures.19 Under this model, outcomes are the changes to knowledge, behavior, satisfaction, or health that occur due to health care. Processes are the activities carried out by professionals or families in the delivery of healthcare. Structures are the characteristics of the setting where care occurs, including material resources, human resources, and organizational characteristics. We further organized the identified processes by sequential steps of subspecialty referrals based on prior conceptual models2,9 with modifications based on interview content. Interview results are presented as a series of key outcomes, processes, and structures of pediatric subspecialty referrals supported by relevant quotes, as well as a conceptual model of domains crucial to high-quality family-centered subspecialty referral systems.
The Institutional Review Board at the University of Pittsburgh provided ethical review and approval for this study.
Results
In total, we conducted 21 interviews, including 19 parents/caregivers (referred to collectively here as caregivers) whose children ranged in age from 0–21 years old (Table 1). In addition to these caregiver interviews, two adolescent or young adult children of these caregivers completed interviews. Two thirds of caregivers identified as white, and one quarter identified as black. Caregivers reported a median travel time to their pediatric subspecialist of 40 minutes, ranging from 5 to 120 minutes. The majority of caregivers reported their child had a PCP, but at the same time most did not identify any professionals who coordinated care for them. Primary child diagnoses as identified by caregivers represented acute conditions, common chronic conditions, and complex chronic conditions, including asthma, autism, bone fracture, brain tumor, CHARGE syndrome, club feet, cystic fibrosis, gastro-esophageal reflux, growth deficiency, juvenile idiopathic arthritis, postural orthostatic tachycardia syndrome, prematurity, spina bifida, and tetralogy of Fallot.
Table 1.
Demographics
| PARENTS/CAREGIVERS (n=19) | N (%) | |
|---|---|---|
|
| ||
| Child age | ||
| - 0–5 | 7 (37%) | |
| - 6–13 | 2 (11%) | |
| - 14–17 | 7 (37%) | |
| - 18–21 | 3 (16%) | |
|
| ||
| Caregiver age* | ||
| - 18–34 | 7 (37%) | |
| - 35–50 | 8 (42%) | |
| - 51–70 | 3 (16%) | |
|
| ||
| Caregiver self-identified race* | ||
| - White | 13 (68%) | |
| - Black | 5 (26%) | |
|
| ||
| Insurance* | ||
| - Commercial | 4 (21%) | |
| - Medicaid | 8 (42%) | |
| - Both | 6 (32%) | |
|
| ||
| Travel time to pediatric subspecialists | ||
| - 0–29 minutes | 6 (32%) | |
| - 30–59 minutes | 9 (47%) | |
| - ≥60 minutes | 4 (21%) | |
|
| ||
| Child has a PCP* | 17 (89%) | |
|
| ||
| Child has care coordinator other than family member* | 3 (16%) | |
|
| ||
| Number of subspecialists involved, median (range) | 4 (1–21) | |
|
| ||
| Number of subspecialist visits in past year, median (range)* | 8 (2–130) | |
One parent/caregiver participant did not answer indicated demographic questions.
Note: Two adolescent/young adult interviews (ages 17 and 19) also completed for total of 21 interviews.
In the following sections, we first present the outcomes desired by informants, then the processes informants perceived to lead to these outcomes, and finally the structures informants identified as supporting these processes. Representative quotes for each identified outcome, process, and structure are provided in Appendix 2.
Outcomes of high-quality pediatric subspecialty referrals
Five domains were identified as expected or desired health outcomes of high-quality pediatric subspecialty referrals from the family’s perspective (Table 2). These included (1) improved functional status or symptoms; (2) improved long-term health; (3) improved knowledge and understanding of diagnosis, prognosis and/or treatment options; (4) improved family expectations regarding goals of care; and finally, (5) decreased worry or anxiety when faced with changes in their child’s health status, exemplified in the following quote:
And then cardiology, they’ve been telling me he had a heart murmur since he was little and then we finally got an appointment to go see it—even though it’s an innocent, slow heart murmur, they wanted us to make sure that he’s alright… It just felt good to hear that, “Oh, his heart is fine,” instead of worrying about every time he got sick, that there’s going to a possibility of him being admitted into the hospital. So I felt like that was a very important part of the whole outlook on the whole situation.
Table 2.
Outcomes and costs of high-quality pediatric subspecialty referrals
| Domain | Definition |
|---|---|
| Desired Outcomes (Benefits) | |
| Improved knowledge & understanding | Receipt of new information or improved understanding regarding diagnosis, prognosis, evaluation plan and/or treatment plan |
| Informed expectations | Receipt of information that helped parents/caregivers build appropriate expectations, often focused on issues of obtaining cure versus managing symptoms |
| Improved functional status or symptoms | Improvement in symptoms or functional status through new or modified treatment plan |
| Improved long-term health | Improvement or expected improvement in long-term health outcomes or life expectancy through subspecialty care |
| Decreased worry and/or anxiety | Alleviation of worry or anxiety through information received or through ability to contact subspecialist with questions or changes in status |
| Costs (Harms) | |
| Missed school | Time spent out of school for child for visit |
| Missed work | Time spent away from work by caregiver for visit, including travel time and wait time |
| Travel burden/travel costs | Time and money spent traveling to appointment |
| Financial costs | Out-of-pocket costs for family |
Of note, improvements in functional status or symptoms and decreased worry/anxiety about the child’s health status were often discussed as the outcomes necessitating more urgent subspecialty referrals. Costs of subspecialty referrals included missed school, missed work, travel burden/costs, and monetary costs.
Processes of high-quality pediatric subspecialty referrals
Informants described processes supporting desired outcomes within six distinct steps in the referral process. These steps included (1) the referral decision; (2) pre-visit information transfer; (3) appointment scheduling; (4) the subspecialty visit; (5) post-visit transfer of information; and (6) ongoing care integration and after-visit communication (Table 3).
Table 3.
Processes of high-quality pediatric subspecialty referrals
| Domain/Step | Subdomain | Definition |
|---|---|---|
| 1. Referral decision | Shared decision making | Collaborative decision making between patients and providers |
| Clear referral reason | Decision making results in clear reason for referral | |
| Specific subspecialist identified | Decision making results in identification of specific subspecialist for referral | |
| 2. Pre-visit information transfer | PCP records provided to subspecialist | PCP records available to subspecialist either through active transfer or shared electronic health record |
| Subspecialist reviews records prior to visit | Subspecialist reviews available records prior to visit | |
| 3. Appointment scheduling | Amount of time spent scheduling appointment | Cumulative amount of time spent by family calling subspecialty office to schedule appointment, including repeat calls, time on hold, etc |
| Reliability of processes for scheduling appointment | Certainty that messages left with subspecialty office will be returned in a timely manner | |
| Timely appointment scheduled | Ability to schedule appointment within an appropriate timeframe for the child’s medical needs | |
| Convenient appointment scheduled | Ability to schedule appointment that accommodates child’s non-medical needs (school, etc) as well as needs of the family (work schedule, school/daycare schedules for other children) | |
| Avoidance of unexpected cancellations | Appointments cancelled by subspecialist office, potentially without adequate explanation or rescheduling | |
| 4. Subspecialist Visit | Diagnosis modified | New diagnosis or refined diagnosis obtained through visit |
| Treatment plan modified | New treatment plan or modified treatment plan obtained through visit | |
| Tasks completed | Ability to accomplish needed tasks, such as medication refills, testing/evaluation, form completion | |
| Developmental/transition needs addressed | Attention to child’s developmental/transition stage throughout visit | |
| Education/community needs addressed | Attention to child’s non-medical needs including education needs and connection with community resources | |
| Financial/insurance needs addressed | Attention to impact of child’s health on family finances and identification of potential resources/solutions | |
| Family needs addressed | Attention to impact of child’s health on family relationships and needs, and identification of potential resources | |
| Efficiency of registration processes | Minimization of time spent registering or completing paperwork | |
| Appointment occurs on time | Minimization of time spent waiting for care | |
| Avoidance of unnecessary visits | Avoidance of visits where the caregiver/child perceived no value | |
| Adequate time with subspecialist | Caregiver/patient reports adequate time with subspecialist during scheduled visit to accomplish all needed goals of visit | |
| Subspecialist listened, showed respect | Caregiver/patient perceives that subspecialist listened adequately and respected their contribution to the visit | |
| Subspecialist views patient as unique individual | Caregiver/patient perceives that subspecialist understood unique value and unique needs of their child | |
| Subspecialist considered comprehensive needs | Caregiver/patient perceives that subspecialist addressed comprehensive needs of their child | |
| Shared decision making during visit | Patient/caregiver preferences considered by subspecialist during visit | |
| 5. Post-visit information transfer | Received clear after-visit plan of action | Clear actionable summary provided by subspecialist to patient/caregiver |
| Recommended to see additional subspecialists | Discussion of additional subspecialists to be seen | |
| Subspecialist communicated with PCP in a timely manner | Transfer of written or verbal information to PCP in a timely manner | |
| Subspecialist followed through as promised | Certainty that subspecialist would complete follow-up tasks as promised (i.e., follow-up phone calls, faxing prescriptions, etc) | |
| 6. Ongoing care integration and after-visit communication | Ability to contact subspecialist with questions or changes in status | Family is able to communicate with subspecialist after or between visits |
| Ability to contact subspecialist in a timely manner | Family is able to hear back from subspecialist in a timely and reliable manner between visits | |
| Ability to schedule timely follow-up visit | Family is able to schedule follow-up appointments within the timeframe designated by subspecialist | |
| Ability to complete tasks between appointments | Family is able to obtain prescription refills, coordinate labwork/imaging, obtain results, etc between visits | |
| Comprehensive care between visits | Perception that a provider is able to address comprehensive needs between visits | |
| Continuous care (rather than episodic, visit-based care) | Perception that subspecialist thinks about child between visits and/or is accessible to advance care between visits | |
| Patient/PCP able to access subspecialist records after/between visits | Ability of patient/caregiver and PCP to view subspecialty notes, recommendations, or results | |
| PCP involvement with care coordination | Involvement of PCP in ongoing care coordination, appointment scheduling | |
| PCP and subspecialist comanagement | Clear roles and areas of care for PCP and subspecialist in ongoing care relationship | |
| Communication between subspecialists | Perception of adequate communication and coordination between different subspecialists | |
| Continuity with subspecialist | Ability to maintain continuity for follow-up visits and for communication between visits | |
| Respect for/trust in subspecialist | Perception of ongoing care by trusted subspecialist |
Regarding the referral decision, specific actions perceived to support successful subspecialty referrals included shared decision making between the PCP and family, identification of clear reasons for referral, and referral to a specific named subspecialist.
During the pre-visit information transfer, processes supporting high-quality subspecialty referrals included timely sharing of PCP records with subspecialists and actual review of those records by the subspecialist:
Having people read his chart – as simple as that sounds, and just being able to know what is going on with him before we have to repeat everything a million times makes a world of a difference.... it automatically makes me trust them because I don’t feel like I have to have my guard up of thinking, “You don’t know anything about this kid, and how are we going to get anywhere with knowing what he needs if we have to spend all this extra time just getting you on the same page?”
Informants discussed successful information transfer through both active transfer of information from PCP to subspecialist via electronic communication, faxes, or telephone calls as well as more passive transfer of information through shared electronic health records.
During appointment scheduling specific aspects of this process discussed by informants included the ability to schedule an appointment that accommodated both the child’s medical needs and the family’s other obligations, the amount of time spent making the appointment, and uncertainty regarding appointment scheduling procedures:
Whenever you call to make an appointment if you have to leave a message I find sometimes that’s not returned in a timely manner. Or it just seems like you don’t get a call-back. Like you have to go back and kind of take that initiative, you know, to make sure then you schedule that appointment.
During the actual subspecialist visit, beyond completion of typical tasks (obtaining diagnosis, treatment modification, medication refills, surgery decisions) informants believed a high-quality referral also meant more comprehensive care tasks (addressing educational, financial, and family needs and attending to the child’s developmental stage and transition needs). A good referral also involved adequate time with the subspecialist, being listened to by the subspecialist, and participating in shared decision making with the subspecialist.
During the immediate post-visit transfer of information, informants echoed the need for successful information transfer back to the PCP, but also stressed the need for information transfer to the patient and family. Key processes related to these events included the receipt of a clear after-visit summary by families and receipt of after-visit documentation by PCPs.
Finally, ongoing care integration and communication was also heavily emphasized by informants. Processes desired included the ability to easily communicate with subspecialists outside of a visit with questions and with changes in status, including the ability to reach their personal subspecialist by phone in a timely manner:
Being able to get a hold of people, so whether that is not having to go through a “Press 1, Press 5, Press 10” a million times just to get a real person, or even knowing when people are available, or people returning phone because I have that -- I will call, and nobody gets back to me.
Many informants expressed a desire for a subspecialist who provides continuous care rather than episodic care, which was exemplified by ease of communication between visits, including subspecialist-initiated follow-up contact and efficient completion of care tasks between visits (i.e., refilling medications, obtaining lab results), as opposed to care occurring only during face-to-face visits (“Don’t just look at it when I’m in the office. When I leave, you still should look, you know, and see, “Well, what’s going on with this child?””). Continuity with a trusted subspecialist was valued by informants during this step (including the ability for follow-up communication with their personal subspecialist rather than a member of the subspecialist’s group) as was effective communication between subspecialists about the child’s care needs.
Structures supporting high-quality pediatric subspecialty referrals
Informants identified multiple structures that supported desired processes and outcomes of subspecialty referrals (Table 4). These structures included physical infrastructure (e.g., parking, signage) and human resources (e.g. PCP, subspecialist, and office personnel capacity and expertise). Additionally, informants highlighted the importance of adequate information technology systems at both PCP and subspecialist practices as supporting high-quality pediatric subspecialty referral experiences, potentially including shared electronic health records, patient portals, functional telephone triage systems, and electronic messaging systems. Such systems promoted ongoing communication and sharing of information between patients, parents/caregivers, PCPs, and subspecialists.
Table 4.
Structures supporting high-quality pediatric subspecialty referrals
| Domain | Subdomain | Definition |
|---|---|---|
| Physical Infrastructure | Parking structures | Convenient, accessible, affordable parking |
| Signage/instructions | Clear information about where to go for visit | |
| Human Resources | PCP capacity and expertise | PCP accessibility, availability, and knowledge |
| Subspecialist capacity, training, and expertise | Subspecialist availability, training, and knowledge regarding the patient’s specific medical needs, including use of pediatric versus adult subspecialists and use of trainees versus attending physicians | |
| Subspecialist office staff capacity and expertise | Office staff capacity to answer phones and check-in patients in efficient and knowledgeable manner | |
| Information Technology Systems | Shared electronic health records | Electronic health records that can be viewed by multiple providers, including PCPs and subspecialists |
| After visit summaries | Relevant and actionable summary of ongoing plan of care and tasks to be completed | |
| Patient Portals | Web-based system providing patients with access to personal health information | |
| Telephone triage systems | Automated or non-automated system that directs incoming phone calls to specific individuals or voicemail boxes | |
| Electronic messaging systems | Messaging system that may range from secure messaging within electronic health record or patient portal to more informal messaging via email or text |
External factors influencing pediatric subspecialty referrals
While the focus of the interviews was on aspects of the medical system that facilitated high-quality subspecialist referrals, informants noted multiple external factors that modified their experience including the child’s medical needs (chronic conditions and severity), child’s developmental/transition needs, patient/caregiver self-efficacy and self-advocacy skills, parent/caregiver networks, and insurance barriers.
Prioritization and trade-offs
To assess the relative prioritization of these identified domains for informants, each informant was asked to describe exceptional subspecialty care. In their responses, informants generally emphasized processes associated with scheduling, visits, post-visit information transfer, and ongoing care integration. Additionally, in discussion of the costs of subspecialty care (travel burden, missed school and work), informants often acknowledged a willingness to accept larger costs in exchange for continuity with subspecialists, higher levels of subspecialist expertise, and/or achievement of desired outcomes.
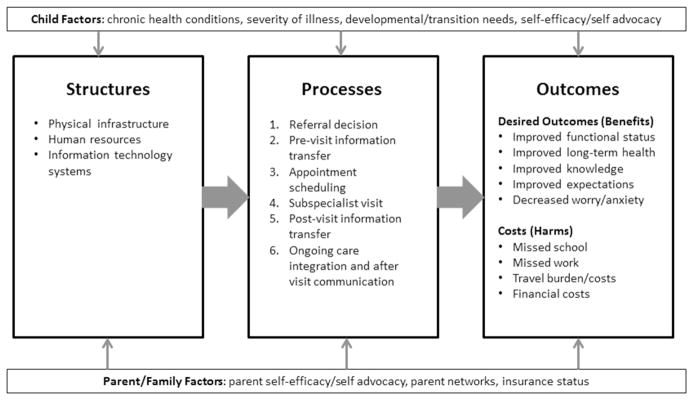
Conceptual Model
We integrated the outcomes, processes, and structures identified by informants to develop a conceptual model of high-quality family-centered pediatric subspecialty referrals (Figure 1). Overall, this model highlights the five identified family-centered outcomes of high-quality subspecialty referral systems, the four cost domains, the six sequential referral steps required to achieve these outcomes, and the underlying structures and external factors that impact these processes and outcomes.
Figure 1.
Structures, processes, and outcomes associated with pediatric subspecialty referral quality by caregivers and patients
Discussion
Through qualitative interviews with caregivers and patients, we developed a family-centered model of high-quality subspecialty referrals. This conceptual model builds upon prior models for subspecialty referrals2,9 by emphasizing the outcomes desired by families and patients and the processes and structures that families identified as supporting these outcomes. The model reflects the importance informants placed on aspects of the referral process that physicians and researchers might not typically see as critical. For example, informants viewed improved knowledge of child’s condition, clear expectations regarding treatment goals, and reduced anxiety regarding child health status as key outcomes in successful referrals. Additionally, the model highlights the degree to which overall quality was impacted by processes occurring during every step of the referral (including appointment scheduling and follow-up subspecialist communication), and not limited solely to referral decisions within the medical home or the face-to-face encounter with the subspecialist.
Our model may help guide future efforts to measure the quality of the subspecialty referral process by emphasizing domains of importance to families that have received inadequate attention in the published literature.9 For example, many prior studies examined the availability of timely appointments (i.e., ability to schedule an appointment within 3 days),9 but did not assess the flexibility of those appointment times or the time burden required to schedule the appointment. Similarly, measures of access and availability often measure geographic proximity and timeliness of face-to-face care, 9,20 but access to timely communication with subspecialists after the completion of the face-to-face visit, while clearly important to families, is not consistently examined. Additionally, the contents of letters between PCP and subspecialist are often studied,9 but informants note that these records must actually be reviewed by the receiving physician. Informants also accentuated the importance to them of domains that have been only intermittently assessed (such as missed work, travel time, and continuity of care), suggesting a need for these domains to be considered more consistently in family-centered evaluations of subspecialty referrals. Finally, informants also underscored the need for measures that are being developed through initiatives such as the Pediatric Quality Measures Program,21 including improved measures of care coordination (i.e., the Family Experiences with Coordination of Care survey22) and improved measures of transition-appropriate care (such as the Adolescent Assessment of Preparation for Transition survey23), emphasizing the need for appropriate uptake of these emerging measures. Altogether, the range of potential measurement domains identified (and the limited attention to many of these domains to date) underscore the complexity of subspecialty referral evaluation and the value of family perspectives in identifying family-centered measurement targets.
In addition to identifying opportunities to improve measurement, our findings also elucidate additional targets to improve pediatric subspecialty referrals. For example, our results suggest that families are interested in engaging with subspecialists in order to not only improve short term and long term health outcomes, but also to facilitate increased family knowledge of the child’s condition, improved alignment of expectations regarding treatment goals, and reduced burden of anxiety when facing fluctuations in their child’s health. To achieve these outcomes, families desire processes that are timely, efficient, coordinated, transparent, reliable, effective, and personalized. Recent focus on interventions to improve shared decision making6 and care coordination12 have the potential to address some of these domains, particularly during face-to-face subspecialty visits. Further attention, however, is needed to pre and post-visit processes in order for families to schedule appointments and communicate follow-up needs in a more patient-centered system. Of note, informants frequently identified information technology solutions as structures to achieve these goals. These results make sense given the capacity of information technology to facilitate communication between all involved parties (patients, caregivers, and providers).
To some degree, our results suggest that families desire a direct relationship with subspecialty care that has similar qualities to the patient-centered medical home (“accessible, continuous, comprehensive, family-centered, coordinated, compassionate, and culturally effective”24). While there are efforts to develop patient-centered specialty practices and to strengthen the connection between the medical home and the “medical neighborhood”,25,26 the primary focus in these efforts is on improving the PCP-subspecialist interface rather than the patient-subspecialist interface. It is possible that families’ desire for more direct communication with subspecialists would be addressed by improved communication between their PCP and subspecialists through achievement of the medical home/medical neighborhood models, but our findings suggest that families may also desire more direct participation in care coordination and follow-up communication than these models incorporate.
The burden of uncertainty in the referral system was frequently discussed, but has not received adequate attention in prior conceptualizations of health care quality. The reduced uncertainty appeared as a desired outcome (e.g., increased knowledge of the child’s condition; increased clarity of expectations). However, informants also wished for more certainty in referral processes (e.g., reason for referral; whether schedulers would return their calls; whether messages left for subspecialists would reach the intended recipient). The uncertainty resulted in frustration, additional caregiver time, and delays in care. The Institute of Medicine identified transparency as one of the ten rules for care delivery redesign,10 but transparency is generally framed in terms of transparency of patient choices rather than more quotidian concerns such as whether a physician received a message or when a callback could be expected. Informants recurrently expressed the sense that waiting for appointments or phone calls was acceptable if they were fully informed of reasons for delays and when to expect contact, suggesting that increased transparency throughout these processes, while not necessarily changing health outcomes, may greatly improve family experience and satisfaction.
Our study has several limitations. First, additional quality domains not discussed by informants, such as health care disparities, are still highly relevant in certain contexts. It is not our goal to de-emphasize quality domains identified in prior work, but rather to ensure that the domains identified as important by patients and families receive appropriate attention. Second, while we included both patients and caregivers, our study was not designed to compare responses in these two groups, but rather to incorporate voices from both patients and their caregivers in our analysis. Third, our sample was not proportionately representative of Western Pennsylvania as we sought to include a heterogeneity of perspectives. Thus, our informants included a larger percentage of African Americans, Medicaid beneficiaries, and children with chronic conditions. Relatedly, as a qualitative study, our findings should be viewed as exploratory and hypothesis-generating. The study design aimed to identify the broad range of quality domains relevant to families seeking subspecialty care, not to rank the relative importance of these domains or establish definitive links between the outcomes, processes, and structures we identified. Future work should assess the relative importance of these domains in general and for specific patient populations and test the hypothesized relationships between these domains using quantitative methods.
In conclusion, to better align observational and interventional analyses of pediatric subspecialty referral processes with family-centered outcomes, we identified a broad range of outcomes, processes, and structures of interest to families and patients receiving subspecialty referrals. Future work should consider these domains when assessing the quality of the subspecialty referral process in order to identify and prioritize gaps in care and to design appropriate interventions to ensure that specialty referrals meet the needs of children and their caregivers.
Supplementary Material
What’s New.
Little is known about family-centered perspectives on pediatric subspecialty referral systems. Through stakeholder-guided, qualitative analysis of parent, caregiver, and patient interviews, we identified family-centered outcomes, processes, and structures of high-quality pediatric subspecialty referrals.
Acknowledgments
The authors gratefully acknowledge the Pediatric Care Delivery stakeholder advisory group, including Pamela DeGeorge, Kathleen Dempsey, Deborah Moss, Amy Philips-Haller, and Mary Ann Rigas, for their invaluable contribution of time, experience, and insight throughout this study. We also appreciate the time of the care coordinators who assisted with recruitment.
Funding: Supported in part by grants from the Agency for Healthcare Research and Quality (K12HS022989, Dr. Ray) and the Children’s Hospital of Pittsburgh of the UPMC Health System (Dr. Ray) and by the National Institutes of Health (UL1TR000005). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funders. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Abbreviations
- PCP
primary care provider
Footnotes
Financial Disclosures/Conflicts of Interest: The authors have no financial relationships or conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Kristin N. Ray, Email: Kristin.ray@chp.edu.
Laura Ellen Ashcraft, Email: ashcraftlg@upmc.edu.
Jeremy M. Kahn, Email: kahnjm@upmc.edu.
Ateev Mehrotra, Email: mehrotra@hcp.med.harvard.edu.
Elizabeth Miller, Email: Elizabeth.miller@chp.edu.
References
- 1.Van Cleave J, Gortmaker SL, Perrin JM. Dynamics of obesity and chronic health conditions among children and youth. JAMA. 2010;303(7):623–630. doi: 10.1001/jama.2010.104. [DOI] [PubMed] [Google Scholar]
- 2.Mehrotra A, Forrest CB, Lin CY. Dropping the baton: specialty referrals in the United States. Milbank Q. 2011;89(1):39–68. doi: 10.1111/j.1468-0009.2011.00619.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Forrest CB, Glade GB, Baker AE, Bocian A, von Schrader S, Starfield B. Coordination of specialty referrals and physician satisfaction with referral care. Arch Pediatr Adolesc Med. 2000;154(5):499–506. doi: 10.1001/archpedi.154.5.499. [DOI] [PubMed] [Google Scholar]
- 4.Stille CJ, McLaughlin TJ, Primack WA, Mazor KM, Wasserman RC. Determinants and impact of generalist-specialist communication about pediatric outpatient referrals. Pediatrics. 2006;118(4):1341–1349. doi: 10.1542/peds.2005-3010. [DOI] [PubMed] [Google Scholar]
- 5.Stille CJ, Primack WA, Savageau JA. Generalist-subspecialist communication for children with chronic conditions: a regional physician survey. Pediatrics. 2003;112(6 Pt 1):1314–1320. doi: 10.1542/peds.112.6.1314. [DOI] [PubMed] [Google Scholar]
- 6.Stille CJ, Fischer SH, La Pelle N, Dworetzky B, Mazor KM, Cooley WC. Parent partnerships in communication and decision making about subspecialty referrals for children with special needs. Acad Pediatr. 2013;13(2):122–132. doi: 10.1016/j.acap.2012.12.003. [DOI] [PubMed] [Google Scholar]
- 7.Miller AR, Condin CJ, McKellin WH, Shaw N, Klassen AF, Sheps S. Continuity of care for children with complex chronic health conditions: parents’ perspectives. BMC Health Serv Res. 2009;9:242. doi: 10.1186/1472-6963-9-242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stille CJ, Primack WA, McLaughlin TJ, Wasserman RC. Parents as information intermediaries between primary care and specialty physicians. Pediatrics. 2007;120(6):1238–1246. doi: 10.1542/peds.2007-1112. [DOI] [PubMed] [Google Scholar]
- 9.Guevara JP, Hsu D, Forrest CB. Performance measures of the specialty referral process: a systematic review of the literature. BMC Health Serv Res. 2011;11:168. doi: 10.1186/1472-6963-11-168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Committee on Quality of Health Care in America of the Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C: Institute of Medicine; 2001. [Google Scholar]
- 11.Frank L, Basch E, Selby JV Patient-Centered Outcomes Research I. The PCORI perspective on patient-centered outcomes research. JAMA. 2014;312(15):1513–1514. doi: 10.1001/jama.2014.11100. [DOI] [PubMed] [Google Scholar]
- 12.Council on Children with D, Medical Home Implementation Project Advisory C. Patient- and family-centered care coordination: a framework for integrating care for children and youth across multiple systems. Pediatrics. 2014;133(5):e1451–1460. doi: 10.1542/peds.2014-0318. [DOI] [PubMed] [Google Scholar]
- 13.Forrest CB, Silber JH. Concept and measurement of pediatric value. Acad Pediatr. 2014;14(5 Suppl):S33–38. doi: 10.1016/j.acap.2014.03.013. [DOI] [PubMed] [Google Scholar]
- 14.Hoffman A, Montgomery R, Aubry W, Tunis SR. How best to engage patients, doctors, and other stakeholders in designing comparative effectiveness studies. Health Aff (Millwood) 2010;29(10):1834–1841. doi: 10.1377/hlthaff.2010.0675. [DOI] [PubMed] [Google Scholar]
- 15. [Accessed September 13, 2014];PCORI Patient and Family Engagement Rubric. http://www.pcori.org/sites/default/files/announcement-resources/PCORI-Patient-and-Family-Engagement-Rubric.pdf.
- 16.Forrest CB. A typology of specialists’ clinical roles. Arch Intern Med. 2009;169(11):1062–1068. doi: 10.1001/archinternmed.2009.114. [DOI] [PubMed] [Google Scholar]
- 17.Ryan G, Bernard H. Data management and analysis methods. In: Denzin N, Lincoln Y, editors. Handbook of Qualitative Research. Thousand Oaks, CA: Sage; 2000. pp. 769–802. [Google Scholar]
- 18.Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods. 2006;18(1):59–82. [Google Scholar]
- 19.Donabedian A. An introduction to quality assurance in health care. Vol. 1. New York, NY: Oxford University Press; 2003. [Google Scholar]
- 20.Kuhlthau KA. Measures of availability of health care services for children. Acad Pediatr. 2011;11(3 Suppl):S42–48. doi: 10.1016/j.acap.2010.11.007. [DOI] [PubMed] [Google Scholar]
- 21.Mistry KB, Chesley F, KLL, Dougherty D. Advancing children’s health care and outcomes through the pediatric quality measures program. Acad Pediatr. 2014;14(5 Suppl):S19–26. doi: 10.1016/j.acap.2014.06.025. [DOI] [PubMed] [Google Scholar]
- 22.Measures: Family Experiences with Care Coordination measure set (FECC) Measure Fact Sheet -- the AHRQ-CMS Pediatric Quality Measures Program (PQMP) AHRQ Pub. No. 15-P002-EF. March 2015.. Available at http://www.ahrq.gov/sites/default/files/wysiwyg/policymakers/chipra/factsheets/chipra_15-p002-ef.pdf.
- 23.Sawicki GS, Garvey KC, Toomey SL, et al. Development and Validation of the Adolescent Assessment of Preparation for Transition: A Novel Patient Experience Measure. J Adolesc Health. 2015;57(3):282–287. doi: 10.1016/j.jadohealth.2015.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Medical Home Initiatives for Children With Special Needs Project Advisory Committee. American Academy of P. The medical home. Pediatrics. 2002;110(1 Pt 1):184–186. [Google Scholar]
- 25.Huang X, Rosenthal MB. Transforming specialty practice--the patient-centered medical neighborhood. N Engl J Med. 2014;370(15):1376–1379. doi: 10.1056/NEJMp1315416. [DOI] [PubMed] [Google Scholar]
- 26.Taylor EF, Lake T, Nysenbaum J, Peterson G, Meyers D. Coordinating care in the medical neighborhood: critical components and available mechanisms. White Paper (Prepared by Mathematica Policy Research under Contract No HHSA290200900019ITO2) Rockville, MD: Agency for Healthcare Research and Quality; 2011. AHRQ Publication No. 11-0064. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.