Abstract
Background
The episodic nature of major depressive disorder (MDD) in clinically referred adults has been well-characterized, particularly by the NIMH Collaborative Depression Study. Previous work has established that MDD also is episodic prior to adulthood, but no study has yet provided comprehensive information on the actual course of MDD in clinically referred juveniles. Thus, the present investigation sought to characterize recovery, recurrence, and their predictors across multiple episodes of MDD in initially 8- to 13-year-old outpatients (N=102), and to estimate freedom from morbidity (“well-time”) across the years.
Method
Clinically referred youngsters with MDD were repeatedly assessed in an observational study across two decades (median follow up length: 15 years). Survival analytic techniques served to model recovery from the 1st, 2nd and 3rd lifetime episodes of MDD, the risk of developing the 2nd, 3rd, and 4th episodes, and the effects of traditional psychosocial and clinical predictors of outcomes. “Well-time” across the follow-up and its predictors also were examined.
Results
Recovery rates ranged from 96% to 100% across MDD episodes; episode lengths ranged from 6 to 7 months. Up to 72% of those recovered from the first episode of MDD had a further episode; median inter-episode intervals were about 3 to 5 years. No single demographic, social, or clinical variable, nor treatment, consistently predicted recovery/recurrence. Psychiatric morbidity over time derived mostly from non-affective disorders, which, however, did not alter the course of MDD.
Limitations
The sample was relatively small and power to detect small effects further declined with each MDD episode recurrence.
Conclusions
Echoing findings on adults, the course of pediatric-onset MDD in this clinical sample was unequivocally episodic. Traditional course predictors had limited temporal stability, highlighting the need to examine novel predictor variables. The ongoing risk of depression episodes into the second and third decades of life suggests that prevention efforts should start in late childhood.
Keywords: childhood depression, major depressive disorder/episode, clinical course, recovery and recurrence, longitudinal follow-up, course predictors
1. Introduction
Empirical research on major depressive disorder (MDD) has yielded various important findings, at least two of which have significant implications for public health initiatives, namely, that this psychiatric disorder is highly recurrent (Burcusa and Iacono, 2007) and that the age-at-first-onset interval extends down to childhood (Rao and Chen, 2009). There also has been an emerging consensus that the combination of early-onset and recurrence represents the most severe form of MDD (Wilson et al., 2014). The high recurrence rate is prognostic information that is useful to patients and clinicians and suggests that preventive interventions should be given priority in the delivery of mental health services; the lowered age for risk of first-onset implies that such services ought to be available to pediatric populations.
Empirically based follow-up studies of adults over the years have overwhelmingly confirmed Kraepelin’s (1921) description of the episodic nature of depressive illness (for reviews, see Beshai et al., 2011; Burcusa and Iacono, 2007; Hardeveld et al., 2010). Irrespective of whether they are clinically referred or community based, and treated or not, the vast majority of adults recover from the given episode of major depression, but then, a substantial portion develops further MDD episodes (reviewed by Beshai et al., 2011; Burcusa and Iacono, 2007; Hardeveld et al., 2010). By the early 1980’s, it also became increasingly evident that major depression exists in school-age children as well (Kovacs et al., 1984a, 1984b), with more recent indications that age at first-onset can be as early as the pre-school years (Luby et al., 2003). With a few exceptions (e.g., Weissman et al., 1999b), studies of clinically referred youngsters have found that, just as adults do, most youngsters recover from depression but a notable portion then has a recurrence (Kovacs et al., 1984a, 1984b; McCauley et al., 1993; Rao et al., 2010; Weissman et al., 1999a).
While follow-up studies (usually involving only two assessment points) have provided an overall view of the outcomes of patients with MDD, only longitudinal studies (involving multiple assessment points) can yield a detailed picture of clinical course. The best known example of this approach has been the naturalistic, longitudinal, NIMH Collaborative Depression Study of adults. That study has been particularly informative because of its design: clinically referred adult in- and out-patients in their mid-30’s with mood disorder were repeatedly assessed across a period of about 20 years; diagnostic interviews were standardized; important course features (e.g. recovery) were operationally defined; and recovery and recurrence rates were estimated via longitudinal statistical procedures, which are more accurate than cross-sectional summaries (Leon et al., 2003; Posternak et al., 2006; Solomon et al., 1997, 2000, 2008).
The prospective design of the Collaborative study has enabled a characterization of the temporal unfolding of MDD episodes in the same sample. For example, after the index episode, the cumulative recovery rates for the first five prospectively observed MDD episodes were 92%, 88%, 90%, 90%, and 90%, respectively (Solomon et al., 1997). There also was a (nonsignificant) tendency toward a somewhat shorter episode with each recurrence, with median lengths of 22 weeks, 20 weeks, 21 weeks, 19 weeks, and 19 weeks, respectively (Solomon et al., 1997). After recovery from the index episode, the cumulative probabilities of the first, second, and third prospectively observed recurrent episodes (each modeled across a 5-year interval) were .60, .74, and .79, respectively(Solomon et al., 2000). There have been no comparable reports of the temporal course of depression in clinically referred children and adolescents.
Given the episodic nature of MDD, predictors of course have been extensively studied, with most variables representing one five major domains: Sociodemographic characteristics (e.g., sex, age, socioeconomic status, living arrangement), clinical features (number of episodes, age at episode onset, episode severity, comorbid psychiatric disorders), treatment exposure (presence or absence of psychosocial or pharmacological treatment, treatment adequacy), family history (mood or depressive disorders in first degree relatives), and theory- or conceptually-based constructs (e.g., cognitive or attribution styles, stress reactivity). Experts in the field have agreed that, with some exceptions, most variables have not consistently predicted course features of MDD across the age span (Burcusa and Iacono, 2007; Hardeveld et al., 2010; Rao and Chen, 2009; Solomon et al., 2008). The exceptions are family history of mood disorder, number of prior episodes, and stressful events, which typically predict recurrence across the age span, and initial severity and comorbidity, which have been implicated in recurrence among adults but not youths (Burcusa and Iacono, 2007; Rao and Chen, 2009; Solomon et al., 2008). The generally inconsistent findings regarding predictors of course in adult samples may reflect that only one recurrence in a given cohort is typically studied, and that first and later episodes, which may have different correlates, often are lumped together (Pettit et al., 2013; Solomon et al., 2008).
Such “lumping” of episodes also characterizes follow up studies of clinically referred depressed children and adolescents. Indeed, most work with young patients sought to establish simply if they had any depressive recurrence subsequent to the index episode (e.g., Rao et al., 2010; Weissman et al., 1999a, 1999b). Consequently, little is known about the course of MDD and its features in youths identified in mental health service settings. For example, it is not known, whether recovery rates for recurrent MDD episodes in young patients follow any temporal patterns or if predictors of recurrence vary across episodes.
In light of the literature, the present study had three goals. First, we sought to characterize recovery and recurrence across multiple episodes of MDD in the same group of initially clinically referred youths. Second, we examined a set of traditional predictors of recovery and recurrence in the areas of socio-demographics, clinical characteristics, naturalistic treatment exposure, and family history. And third, because recovery and recurrence rates do not convey the cumulative morbidity of psychiatric illness, we also examined the extent to which young patients were free of depressive and other psychiatric disorders across the years (well-time), along with selected predictors of well-time.
2. Method
2.1. Subjects
This naturalistic follow up study of depression in childhood was initiated in 1979 at an urban, mid-Western University Medical Center. It enrolled 191 young patients, 8- to 13-years old, free of major systemic medical disorder, and not intellectually limited (and their parents) from a variety of outpatient pediatric clinical settings, as described in detail previously (Kovacs et al., 1984a). Study entry psychiatric diagnoses were determined by the research team (see below) and included: (a) a diagnosis of depression, including major depression, dysthymia, or adjustment disorder with depressed mood (n= 134), (b) bipolar disorder (n=8) and (c) miscellaneous non-depressive control psychiatric disorders (n=49). “Childhood-onset” of depression was operationally defined as a first depressive episode that onset by the age of 13 years. Starting with the entire sample of 191 youngsters, the present article focuses on 102 subjects, whose first episode of major depressive disorder (MDD) met the definition of “childhood-onset.”
The 102 cases, aged 11.2 years, on average (SD=1.5 years), at study entry, were about evenly split between boys (n=50) and girls; 66% were Caucasian, 32% were African-American, and 2% had mixed ethnic origins. At study entry, 56% of the youths lived in 2-parent households (for 29%, both biological parents were present), and 68% had a head-of-household of lower socioeconomic status (Hollingshead indices IV and V). Altogether 49% of the sample had prior outpatient psychiatric treatment, 8% had past psychiatric hospitalizations, and 9% had a history of psychotropic medication use.
2.2. Follow-Up Procedures
During the first 5 years of the study, we sought to evaluate subjects at least twice per year; the assessments were eventually tapered to once every 12 to 20 months. Subjects were followed naturalistically over a maximum of 24 years (median=15 years; SD=7 years). Over time, 20 different clinical interviewers were involved in the study. While crisis intervention was provided when warranted, the follow-up was naturalistic and did not include treatment (although relevant data were repeatedly collected).
2.3. Diagnostic Assessment of Youths
Up to age 18 (or while the subject was living in the parental household), each evaluation involved the child (who informed about him or herself) and the parent (or other responsible adult) who informed about the family and the target youth. After age 18, youths themselves became primary informants, although a parent or adult partner of the subject served as informant, if appropriate and warranted. At each assessment, the same clinician interviewed both the subject and second informant. Throughout the study, trained clinicians (M.D., Ph.D., or Master’s level) administered the Interview Schedule for Children and Adolescents (ISCA) or its version for Young Adults (YAIS), and associated diagnostic addenda, using either the intake version, or the follow up version, which covered the time since the last assessment (Sherrill and Kovacs, 2000). The inter-rater reliability of these symptom-based, semi-structured psychiatric interviews have been reported as satisfactory by us (Sherrill and Kovacs, 2000) and other investigators (Goldston et al., 2015). Using pre-coded, structured data sheets, interviewers also gathered psychosocial data, including information on treatment exposure.
Using the ISCA and YAIS ratings, the interviewing clinician generated the initial diagnoses that captured the presentation and history of the case at that point in time. These diagnoses were first subjected to a review by contemporaneous interviewers, and then to further levels of review by senior raters, resulting in multi-step, consensus-based diagnoses. As noted previously, we used DSM-III (American Psychiatric Association, 1980) criteria. We also generated operational rules to diagnose comorbid psychiatric disorders that had overlapping symptoms (Kovacs et al., 1984a, 1984b). Mirroring the approach of the Collaborative Study (Keller et al., 1983), operational rules were used to date onset and offset of episodes of disorder (Kovacs et al., 1984a, 1984b) Onset was the first point in time when the condition met the relevant DSM-III criteria (American Psychiatric Association, 1980). Offset of mood (and other emotional) disorders (recovery) was dated to the point in time when the patient had no more than one clinical and few (if any) mild symptoms of the disorder and then maintained this relatively asymptomatic state for a minimum of 2 months (9 weeks). Once confirmed, the offset (or recovery) date was set at the start of that 2 month verification interval. Re-emergence of symptoms of the disorder within the 2 month recovery-verification interval was defined as relapse and the episode was then considered as continued. For behavior disorders, we required a minimum of 3 months of relatively symptom free interval to verify recovery from the episode in question.
At each assessment, the interviewer identified meaningful (personal, familial, or community-wide) marker events for the patient and family to anchor the vexing and waning of symptoms across time, and to estimate disorder onset/offset. In assessing long follow up intervals, an emphasis was placed on levels of functioning to identify symptoms. If a disorder’s onset/offset date could not be determined with reasonable certainty, the “mid-point rule” was used: that is, the interviewer determined a probable time interval during which the onset/offset was likely to have occurred (e.g., “sometime between the start of the fifth grade and before the next summer”) and used the calendar midpoint of that interval for the date in question. Because a major goal of this study was to characterize the clinical course of pediatric affective disorders, interviewers were always provided with the results of prior research assessments and thus were able to follow-up on previously reported symptoms.
2.4. Family History of Psychiatric Disorders
As reported previously (Kovacs et al., 1997), using state-of- the art, semi-structured, diagnostic interviews, history of psychiatric disorders in parents and other relatives was determined independent of the youths’ follow up assessments by interviewers who were blind to the nature of the offspring’s specific diagnostic status (i.e., control or mood disorders). In the present sample, 77% of the biological parents had a lifetime history of depression-spectrum diagnosis (major depression, dysthymic disorder, depressive disorder NOS); 18% of the parents had bipolar spectrum diagnoses; and 28% had a history of psychotropic medication use. Altogether 24% of the families had a member (parent/grandparent and/or sibling) with a history of psychiatric hospitalization.
2.5. Statistical Analyses
Using SAS statistical software (SAS Institute, 2008), time to recovery and time to a recurrent episode were modeled using the Kaplan-Meier (KM) estimator (Kaplan and Meier, 1958). The effects of covariates on recovery and recurrence were examined using Cox proportional hazards regression models. For joint analysis of (potentially) multiple episodes of recovery from or recurrence of MDD, Cox models with shared frailty (i.e., including random effects) were run using Stata 11 (Cleves et al., 2010; StataCorp 2009a,b). In multivariate models of recovery from or risk of recurrence of a given MDD episode, variables were entered via a forward stepwise procedure, with p=0.10.
Time-dependent predictors (e.g. mental health treatment, a specific comorbid disorder) were defined as present (yes or no) during the episode or the inter-episode interval being modeled. We considered four sets of predictors: (a) DEMOGRAPHIC variables included sex, SES of head of household, both biological parents in the household and two-parent household at intake; (b) CLINICAL variables included age at onset of the first Major Depressive Episode (MDE) and age at each recurrent episode, comorbid dysthymic, anxiety, or behavior disorder (each coded as yes or no) during the episode in question, or during the inter-episode interval being modeled; (c) FAMILIAL variables included parental lifetime history of depression and highest level of maternal depression symptoms during the episode, or during the inter-episode period being modeled (indexed via the total score on the Beck Depression Inventory-II or BDI-II (Beck et al., 1996); and (d) three indices of TREATMENT received (yes or no) during the period being modeled, namely, prescribed psychotropic medication, psychological therapy, and inpatient hospitalization. When modeling a recurrence, additional predictors included the length of the just prior depression episode and the youth’s age at that episode’s offset.
“Well-time” was defined as being free of: (a) any depressive disorder and (b) any major non-depressive psychiatric disorder. It was computed as the number of days free of the specified outcome divided by the total number of days counting from onset of the first episode of MDD to the date of the last assessment. The Wilcoxon signed rank rest served to assess whether median proportions of well time (using the two definitions) differed as a function of sociodemographic characteristics including sex, SES, parental household arrangement at study entry, and age at first major depression episode.
3. Results
Of the 102 youths, 2 had only intake evaluations and were lost to follow-up. The remainder were followed for variable durations (maximum of 24 years), with 81% of the sample having been observed for five years or longer. On average, subjects had 17 interviews during the follow-up (SD=10; Median=18). Altogether 1,772 interviews were conducted, which revealed 226 major depressive episodes. The index episodes with which they entered the study were the first MDEs for almost all cases.
Over the follow-up, altogether 26 youths switched from unipolar to bipolar disorder. For 11 (42%) of these 26 youths, the switch in polarity occurred after the first episode of major depression, while the rest had multiple MDEs prior to manifesting bipolar disorder. (Three of these subjects are not accounted for in Table 1 because their change in polarity occurred after the fourth MDE). Altogether 12 (46%) youths had Bipolar I, while the rest had Bipolar II disorder as the first bipolar episode. For those with unipolar depression across the entire observation period, the number of recurrent episodes (partly a function of follow-up length) ranged from 0 to 8. However, we modeled recovery only from the first three MDEs because the number of cases with subsequent episodes was too small for meaningful analysis. For example, the 4th depression episode was actually observed only in 18 youths. At their last assessment, subjects were 24 years old, on average (SD= 6.6 years; median= 26 years).
Table 1.
Rates of Recovery and Recurrence Across Multiple Episodes of MDD
| Event | Number of Subjects |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| at Risk for Event |
Had the Event |
Switched to Bipolar d/oa |
Median Time to Event (years)b |
Cumulative Event Rate (95% C.l.)c at | Relative Hazard (vs. 1st Episode) |
||||
| Recovery | |||||||||
| From MMD | 6 months | 1 Year | 3 Years | 5 Years | |||||
| Episode | |||||||||
| 1st | 102 | 94 | 5 | 0.71 (0.55, 0.82) | 0.35 (0.26, 0.45) | 0.71 (0.62, 0.80) | 0.94 (0.88, 0.98) | 0.96 (0.91, 0.99) | 1.0 |
| 2nd | 54 | 52 | 3 | 0.60 (0.42, 0.69) | 0.39 (0.27, 0.53) | 0.72 (0.60, 0.84) | 0.96 (0.88, 0.99) | 1.00(0.91, 1.00) | 1.23 (0.87, 1.73) |
| 3rd | 34 | 34 | 1 | 0.48 (0.30, 0.72) | 0.53 (0.37, 0.70) | 0.82 (0.68, 0.93) | 1.00 (0.87, 1.00) | 1.64(1.10,2.44) | |
| Recurrence | |||||||||
| of MMD | 1 Year | 5 Years | 10 Years | 15 Years | |||||
| Episode | |||||||||
| 2nd | 89 | 54 | 6 | 4.21 (2.45, 9.48) | 0.21(0.14,0.31) | 0.55 (0.45, 0.66) | 0.65 (0.54, 0.75) | 0.72 (0.60, 0.83) | 1.0 |
| 3nd | 49 | 34 | 6 | 2.82(1.94,4.19) | 0.20(0.11,0.35) | 0.69 (0.54, 0.82) | 0.82 (0.68, 0.93) | 0.91 (0.72, 0.99) | 1.22(0.77, 1.95) |
| 4rd | 33 | 18 | 2 | 4.58 (1.54, 10.7) | 0.22 (0.11, 0.40) | 0.56 (0.38, 0.76) | 0.70 (0.49, 0.89) | 0.80(0.56,0.96) | 0.86 (0.48, 1.55) |
Subjects who switched to bipolar disorder from MDD were removed from subsequent analyses.
Event time was measured from MDD episode onset to its offset for recovery, and from MDD episode offset to next episode onset for recurrence.
Kaplan-Meier estimates.
By definition, rates of time-dependent variables varied during the follow-up. Across the six time intervals and associated outcomes that were modeled (three recovery periods and three inter-episode intervals), comorbid dysthymic disorder was present among 14.7% to 37.3% of the youths, comorbid anxiety disorder was present among 35.2% to 50.0%, and comorbid behavior disorder was present among 11.8% to 24.1%. Changes in these rates over time did not show any linear or nonlinear temporal trends. Rates of mental health treatment (psychotherapy, psychotropic medication, inpatient hospitalization) also varied with no clear temporal trend over the years. During the depression episodes that were modeled, from 48.5% to 72.3% of the youths reportedly received mental health care; during the inter-episode intervals, such contacts were reported for between 61.3% and 79.8% of the cases.
3.1. Rates of Recovery and Their Predictors
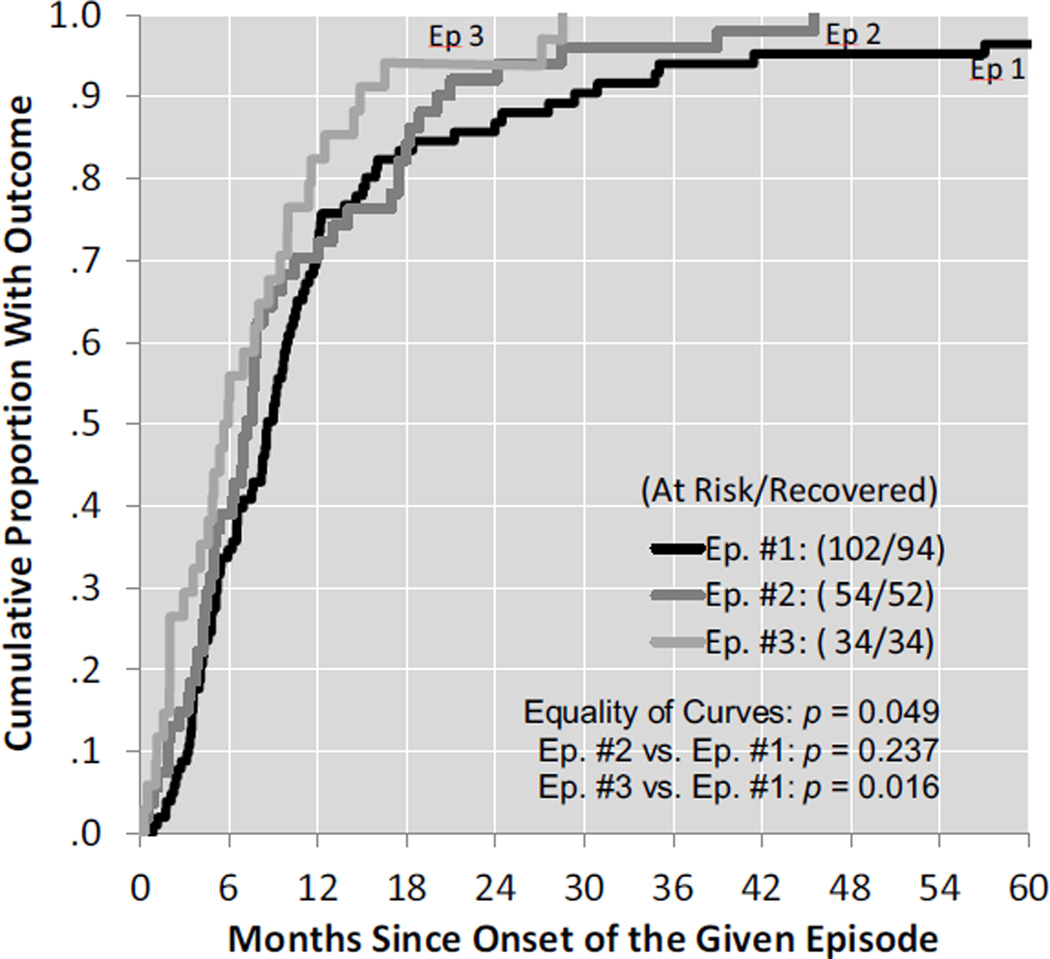
The cumulative portion of subjects recovering from the 1st, 2nd, and 3rd MD episodes was estimated as 96%, 100%, and 100%, respectively. Median episode durations were 0.71 year, 0.60 year, and 0.47 year (or 37 weeks, 31 weeks, and 24 weeks) respectively, for the 1st, 2nd, and 3rd MDD episodes (see the Kaplan-Meier estimates plotted in Figure 1). For cases that eventually switched polarity, only those depression episodes were modeled, which occurred before that change point in the clinical course.
Figure 1.
Rates of Recovery From the First Three Lifetime MDD Episodes
The upper part of Table 1 presents the Cox regression hazard ratio estimates of recovery for each episode (using a robust variance estimate for shared frailty). The overall hypothesis that these hazard ratios are similar and hence equal to 1 was rejected (p=0.049, 2 d.f.). Given that hazard ratios > 1 indicate higher instantaneous rates of recovery (i.e., shorter episode durations), comparisons of the individual hazard ratios showed that the overall difference is driven by episode 3: Namely, episode 3 is significantly shorter than is episode 1 (hazard ratio=1.64; p=0.016), while episodes 1 and 2 are similar in duration (p=0.24). To compare recovery from episodes 3 and 2, the model was re-parameterized, with episode 3 as the baseline; the difference was not significant (p=0.20, data not shown).
From among all the predictors that were entered in modeling recovery, Table 2 lists only those that emerged as significant in at least one analysis.1 In the rows summarizing episode-specific recovery (Table 2), the absence of demographic variables (sex, SES) and most clinical variables (e.g., age at onset of a given episode) indicate that they had failed to predict recovery from any of the episodes. Further, there was little consistency in the predictive value of any given variable. For example, for depression episode 1, comorbid dysthymic disorder (DD) was associated with more rapid recovery (hazard ratio 1.64, p=0.024), but DD did not measurably affect the subsequent course of MDD. As another example, youths with comorbid behavior disorder during MDE #2 had a more protracted recovery from episode 2 (hazard ratio 0.50, p=0.054), while this type of comorbidity did not affect recovery from the other depression episodes. No variable emerged as a significant predictor of recovery from episode 3 (p>0.10 for all variables).
Table 2.
Final Models of Recovery from and Recurrence of MDD Episodesa
| Outcome | Predictorb | Hazard Ratio (95% C.I.) |
p |
|---|---|---|---|
| Recovery from Ep. #1 | |||
| Model a | Comorbid dysthymic disorder | 1.64 (1.07,2.53) | 0.024 |
| Model b | Comorbid dysthymic disorder | 1.62 (1.03,2.54) | 0.036 |
| Mental health treatment | 0.59 (0.37,0.95) | 0.031 | |
| Recovery from Ep.#2 | |||
| Model a | Comorbid behavior disorder | 0.50 (0.25,1.01) | 0.054 |
| Model b | Treatment does not enter | 0.17 | |
| Recovery from Ep.#3 | |||
| Models a and b | No predictors enter | NS | |
| Time to Ep.#2 | |||
| Model a | Two-parent household | 2.04 (1.16,3.60) | 0.014 |
| Model b | Two-parent household | 2.16 (1.19,3.94) | 0.012 |
| Mental health treatment | 2.35 (0.93,5.95) | 0.070 | |
| Time to Ep.#3 | |||
| Model a | Comorbid behavior disorder | 0.31 (0.11,0.87) | 0.026 |
| Two-parent household | 0.52 (0.24,1.10) | 0.087 | |
| Model b | Mental health treatment does not enter | 0.55 | |
| Time to Ep.#4 | |||
| Model a | Length of ep. #3 > 0.496 yrs. (median) | 2.94 (1.03,8.34) | 0.043 |
| Model b | Length of ep. #3 > 0.496 yrs. (median) | 3.23 (1.13,9.24) | 0.029 |
| Mental health treatment | 2.67 (0.86,8.24) | 0.09 |
Each model was run twice: Model a = treatment variable excluded; Model b = treatment variable included.
See the text for the list of all variables that were considered for each model
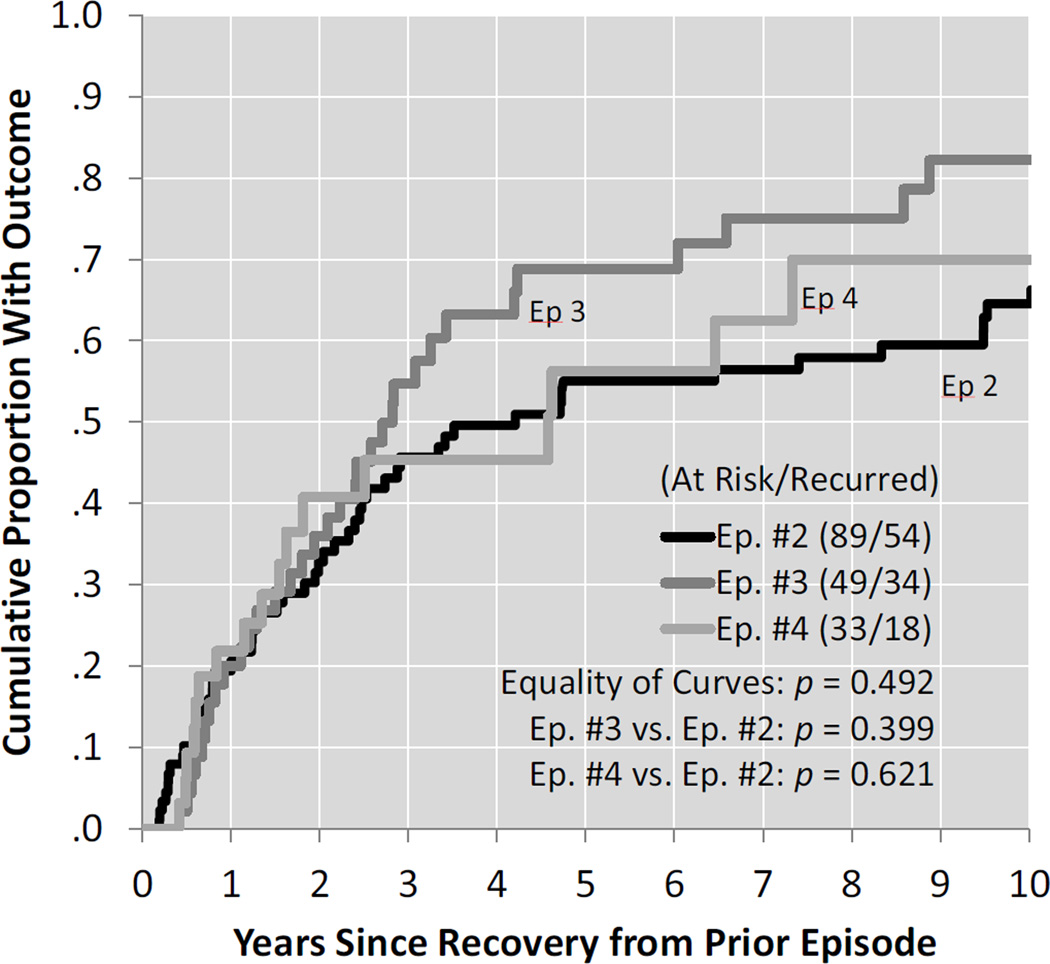
3.2. Rates of Recurrent Episodes and Their Predictors
Subsequent to the first MD episode from which patients recovered, there were 203 periods of possible recurrence in 89 subjects (of the 102 cases with first episodes, 8 were censored and 5 switched polarity); 84% of these periods followed recoveries from the first three episodes of major depression. If a given depression episode was followed by mania or hypomania, and thus a “switch” from unipolar to bipolar illness had taken place, the course after the polarity change occurred was excluded from modeling recurrences. (Table 1 shows the number of cases withdrawn from the analyses at each point because of bipolarity). Results of the survival analyses are presented in the bottom half of Table 1 and K-M estimates are plotted in Figure 2. The cumulative probability of the 2nd, 3rd, and 4th episode of MDD is .0.72, 0.91, and 0.80, respectively. There was considerable variation across inter-episode intervals: the estimated median time interval was 4.21 years between the 1st and 2nd episodes, 2.82 years between the 2nd and 3rd episodes, and 4.58 years between the 3rd and 4th major depression episodes.
Figure 2.
Rates of 2nd, 3rd, and 4th Recurrent MDD Episodes After Recovery From Prior Episode
Table 1 also includes Cox regression hazard ratio estimates of recurrence (using a robust variance estimate for shared frailty). An overall test that the hazard ratios are equal to 1 was not significant (p=0.49, 2 df.), indicating that the likelihood of a recurrence did not vary as a function of episode number. Results regarding predictors of recurrence are variable and are summarized in Table 2. The probability of a second depression episode was higher for children who had lived in two-parent households (hazard ratio 2.04, p=0.014) compared to those who did not. A third MDE was less likely among children who were free of comorbid behavior disorders (hazard ratio 0.31, p=0.026) and somewhat less likely if they lived in two-parent households (hazard ratio 0.52, p=0.087). Finally, a longer third episode (at least 0.496 years, the median Episode 3 length) was associated with a higher probability of the next (fourth) major depression episode (hazard ratio 2.94, p=0.043).
3.3. Mental Health Treatment and Recovery/Recurrence
Treatment (psychotherapy, inpatient care, and/or medication) during a given episode or inter-episode interval had a negative but inconsistent relationship to the outcomes (Table 2). Across the three MDEs for which we modeled recovery, treatment was related only to the first (index) episode--treated children took longer to recover. As also shown in Table 2, across the recurrences (or inter-episode intervals) that we modelled, treatment was related at a trend level to risk of recurrence during 2 of the 3 at-risk intervals-- cases who received treatment in the just prior inter-episode interval were somewhat more likely to have a next episode of major depression.
3.4. Proportion of Time Free of Depressive or Other Major Mental Disorders
We computed for each subject the proportion of time spent free of depression and free of any other major psychiatric disorder from onset of first MDE through the last interview (including time periods subsequent to bipolar turns). For the sample, the median proportion of time having been free of depression was 0.78 (IQR 0.54 ,0.89); median proportion of time free of major non-affective psychiatric disorder was 0.29 (IQR 0.03,0.67). In other words, in spite of recurrent major depressive episodes, subjects tended to be free of diagnosable depression most of the time as the years went by. However, about half of the sample spent about 70% of the time having some type of non-affective mental disorder. Age at first MDE (dichotomized at the median), did not predict time spent free from depression (p=0.83) or non-affective major psychiatric disorder (p=0.54). Further, parental socioeconomic status (dichotomized as high vs. low), living in a 2-parent household at study entry, or the youth’s sex also were unrelated to well-time (all p>.13). Only one sociodemographic characteristic was significant: children living with both biological parents at study entry spent less time in a psychiatric disorder over the years (p=.041), with a trend toward less time in depression as well (p=.11), compared to peers living in non-intact families.
4. Discussion
There has been a call for a life-span approach to the treatment and prevention of MDD, given its typically recurrent nature among adults (Shelton and Hollon, 2012). Based on the findings of the present study that most cases of childhood-depression likewise have recurrences by young adulthood, along with previously reported results (reviewed in Rao and Chen, 2009), the life-span prevention perspective should be extended to the years of childhood.
The repeated assessment of the same pediatric cohort from childhood to adulthood, which is a novel feature of the present study, enabled a mapping of important course features of very early onset MDD. This longitudinal perspective revealed that MDD in clinically referred youngsters signals high recovery rates regardless of episode number, but also a significant risk of recurrence, which also appears fairly stable across the initial 15 years of the disorder. The high recovery rate (96%) for the first lifetime episode of major depression in our sample also was characteristic of later episodes, confirming prior reports of high recovery rates (for unspecified episodes) in various depressed pediatric samples (e.g., Birmaher et al., 2004; McCauley et al., 1993; Rao et al., 2010). But the consistently high risk of recurrence we found to be associated with the second to fourth episodes (72%, 91%, and 80%, respectively), which did not statistically differ as a function of the number of prior episodes, suggests a worse course for pediatric depression than many other studies have reported. Specifically, while in a 10-year follow up of a clinical sample of depressed adolescents, 63% had recurrent MDD (Weissman et al., 1999a), lower estimates of recurrence have ranged from 40% to 54% (Birmaher et al., 2004; McCauley et al., 1993; Rao et al., 2010). However, the lower recurrence rates were typically based on follow-up intervals of 5 years or shorter, which provide a truncated picture of clinical course. Importantly, we found no compelling temporal trends in episode durations, recurrence risk, or inter-episode intervals from childhood up to young adulthood.
Of the various traditional predictors of course that we examined, only one demographic (living in a 2-parent household at intake) and three clinical variables (comorbid dysthymic or behavior disorder, longer third MDE) were associated with some features of depression across the years, but these associations were not consistent. With the exception of demographic variables, which have repeatedly failed to predict recovery from pediatric depression (Birmaher et al., 2004; McCauley et al., 1993; Rao et al., 2010), other follow-up studies of youths likewise found generally negative or inconclusive results with regard to predictors of depression course. For example, clinical characteristics such as episode severity (McCauley et al., 1993) or having prior episodes (Birmaher et al., 2004) were found to predict recovery (inversely) only in single studies. These findings suggest that contextual factors, which vary as a function of time, probably interact with and alter the predictive utility of variables in ways that are currently not well understood nor typically examined. For example, during adolescence, the negative prognostic value of depression episode number for later course may conceivably be attenuated for youths who are able to leave a toxic family context and align with peers capable of providing coping resources. Indeed, the findings underscore the need for new approaches to longitudinal data, which can model clinical course as a function of dynamic contextual factors.
In prior studies of pediatric depression, there was considerable interest in whether stage of pubertal development, or child- versus adolescent- onset, influenced course and outcome (Rao and Chen, 2009). Supporting this interest, the Maudsley follow-up study of children with depression symptoms reported that the risk of recurrent depression was lower among pre-pubertal (and younger) subjects; however, this was no longer the case when the index episode was defined via more stringent diagnostic criteria (Harrington et al., 1990) and did not appear to be the case on much longer follow-up (Fombonne et al., 2001). In an earlier analysis on a smaller sample, we ourselves reported that being pre-pubertal (established by pediatric examination) and younger at depression onset predicted longer episodes (Kovacs and Paulauskas, 1984), but these age effects did not replicate in a larger sample (Kovacs et al., 1997). We also found no clear age effects in the current data set. Birmaher et al., (2004) likewise reported that the clinical course (e.g., recovery, recurrence, comorbidity) of young patients with pre- versus post-pubertal onset of MDD were practically indistinguishable. Thus, pre- versus post-pubertal onset of depression does not appear to be a clear determinant of clinical outcomes.
Mental health treatment was (inconsistently) associated with worse clinical course, as also reported by other follow up studies (McCauley et al., 1993). This finding probably reflects that youths with significant depression symptoms were more likely to be referred for treatment than the rest of the cases. Somewhat surprisingly, parental history of depressive illness and number of prior MDEs were unrelated to recovery or recurrence. However, a recent large, community-based study found that, while parental mood disorder predicted early-onset depression, it did not predict depression recurrence (Wilson et al., 2014). Thus, early-onset, recurrence, and positive familial history may all be alternate indicators of an underlying dimension of depression severity (Burcusa and Iacono, 2007).
An unexpected finding was the persistence of non-affective psychiatric disorders in our sample. Over the years, our subjects spent more time in comorbid disorders (median: 78% of the time) than being depressed (median: 29% of the time). The high rate of comorbid psychopathology in juvenile-onset depression, which is well documented (e.g., Angold, Costello & Erkanli, 1999), is not unique to that age group. Among adults with MDD, from 69% (Brown et al., 2001) to 79% (Melartin et al., 2002) were found to have current comorbid psychiatric disorders. And yet, in a longitudinal context, comorbidity had no consistent effects on the course features of MDD in our sample. However, because comorbid non-affective disorders in pediatric depression have been associated with worse response to treatment (Brent et al., 1998), they warrant further scrutiny.
Because methodological features of the present study were inspired by the NIMH Collaborative study of adults, a comparison of key findings is informative. In the Collaborative study, recovery across the first 5 prospectively observed MDD episodes ranged from 88% to 92% (Solomon et al., 1997): we found similarly high recovery rates in youths. The depression episode recurrence rates in our youths also mirror the recurrence rates among adults in the Collaborative study (from 60% to 79%; Solomon et al., 2000). However, the episodes in our pediatric sample were longer (median: 24 weeks to 37 weeks) than in the Collaborative study (median: 19 weeks to 21 weeks; Solomon et al., 1997); our inter-episode intervals also were longer (median: about 3 to 4.5 years) than in the Collaborative study (about 1 to 2.9 years; Solomon et al., 2000). Combining these findings, it appears that, across the years of childhood and adulthood, episode durations and inter-episode intervals both seem to become progressively shorter, possibly indicating that the course of illness “speeds” up. Such a possibility is consistent with Post and colleagues’ (2012) argument that the recurrent nature of mood disorders typically mirrors a progressively deteriorating course. Indeed, neurobiological changes and treatment resistance have been linked to increasing episode numbers or total illness duration (Lui et al., 2011; Segal et al., 2010). Further, similar to the findings in our sample, Solomon et al. (1997) reported that none of the sociodemographic (e.g., sex, age, SES) or clinical (e.g., comorbidity, prior episodes) variables was a consistent predictor of recovery for the first 5 prospectively observed recurrent MDD episodes. Admittedly, having more prior episodes was associated with recurrence using a different analytic approach (Mueller et al., 1999), but that finding was based on a far greater range of episodes than in the current study.
A comment also is in order about the rate of bipolar switch in our cohort, which we already detected in a smaller sample (Kovacs et al., 1994). Over the follow-up, altogether 26 youths (25%) switched polarity by the time they were adults. Although the “turn” rate from unipolar to bipolar illness in initially youth samples has been reported as low as about 5% (Weissman et al., 1999a, 1999b), our rate of 25%, along with the turn rate of 33% reported by Geller et al., (2001), suggest that a change in polarity is far more frequent in juvenile-onset depression compared to depression that onsets later in the life course. For example, during the first decade of the Collaborative Study follow-up, only 6% of the adult patients with unipolar depression switched polarity (Solomon et al., 1997). Therefore, juvenile-onset depression may be a marker of bipolarity in a subset of youths.
4.1. Practical implications of the present findings
First, as already noted, childhood-onset and later-onset depressive disorders should be considered on a continuum and similarly targeted in a life-span approach to prevention. The importance of prevention in the younger ages is supported by work with adult patients, which has shown that functional outcomes are worse for very early- compared to later-onset depression (Zisook et al., 2007). This finding is likely to reflect the fact that mental disorder during the juvenile years is particularly detrimental because it interferes with normal developmental tasks. Indeed, we have previously reported that depression in our juvenile sample was associated with impaired school performance and academic achievement, had a negative impact on verbal intellectual performance (Kovacs and Goldston, 1991), and had detrimental effects on social competence, particularly in combination with comorbid conduct disorder (Renouf et al., 1997). Second, there is now considerable evidence that traditional demographic and clinical variables are not reliable predictors of the course of MDD. As noted, this may reflect that the implications and consequences of predictors can change as a function of time and context, which cannot be adequately controlled statistically or otherwise. Importantly, the few reliable predictors of course that emerged from prior work (e.g., family history, prior number of episodes) are not amenable to change. Therefore, it may be time for researchers to focus on dynamic and potentially malleable vulnerability factors, including physiological processes, which undergird sensitivity to recurrence (Farb et al., 2015; Post et al., 2012). And third, while we found that only a minority of clinically referred youngsters with a first MDD episode remain free of depression recurrence on long-term follow up, community samples appear to include a larger portion of single episode cases (Monroe and Harkness, 2011). Although there is a need to identify unique features of cases with single versus multiple depression episodes, such a study is made difficult by the fact that recurrence is time dependent: Namely, a subject with a single-episode MDD in the context of a 5-year follow up may no longer be a single episode case if followed for another 5- to 10-years.
4.2. Limitations
While the present findings derive from the longest longitudinal study in which clinically referred youngsters with major depression were repeatedly assessed, the results are constrained by the relatively small sample size. This reduced our statistical power to detect small effects on the outcomes and also limited the range of predictors that were examined. Some investigators may find fault with the fact that the evaluations were not conducted blind to prior diagnostic results. While keeping interviewers blind to prior information may minimize bias, it makes it impossible to obtain temporally meaningful data or to counter serious memory distortions by informants, and does not correspond to the way in which diagnoses are made in clinical practice. Another constraint is that treatment contacts were included in the statistical models as dichotomous information (yes/no), which did not account for the length or adequacy of treatment exposure. Also, we could not determine if mental health treatment during the follow up was specifically for depression symptoms or other complaints. Further, because MDD in community samples of (mostly) adults appears to have a more benign course (Kessler et al., 1997), findings from the present study may not fully generalize to non-referred youths with MDD.
4.3. Conclusions
All in all, there now is compelling evidence of the recurrent nature of MDD across the juvenile and adult years, as it unfolds in the context of naturalistic treatment (or lack thereof). However, even state-of-the- art interventions for depressed youths have had limited impact on post-treatment course. For example, within 2 years of completing a randomized depression treatment trial, 38% of the adolescents had a recurrent episode (Birmaher et al., 2000); by 4 years post-treatment, 47% of the youths in another randomized treatment trial had a recurrent depression (Curry et al., 2011). Such findings are further proof of the intrinsically phasic nature of major depressive illness and unquestionably argue for recurrence prevention as the priority public health intervention.
Highlights.
Clinically referred 8- to 13-year-olds with major depression were followed across two decades
Recovery was modeled from each of the first 3 lifetime major depressive episodes (MDE)
Risk of the 2nd, 3rd, and 4th lifetime MDEs also were modeled
Childhood-onset major depression signals high recovery and high recurrence rates
No single variable consistently predicted MDE recovery or recurrence across the years
Acknowledgments
Disclosure of Funding Source: This research and preparation of the manuscript were supported by National Institutes of Health grants: MH 33990, MH-056193, and MH 085722
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
We examined the inter-correlation coefficients among our predictor variables and found that most of them did not survive Bonferroni corrections for multiple contrasts. For example, of 45 inter-correlation coefficients among predictors used to model recovery from Episode 1, only two survived Bonferroni correction at an overall p<.05: living in a 2-parent household and living with both biological parents at study entry were significantly associated at r=.57; while older age at depression episode onset was associated with comorbid behavior disorder at r=.35. In general, most correlation coefficients were of modest magnitudes, suggesting that collinearity was unlikely to have significantly affected the results.
Conflict of Interest: Dr. Kovacs receives royalties from Multi-Health Inc., a test publisher. The other authors have no disclosure to report.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. third. Washington, DC: Author; 1980. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck Depression Inventory – II (BDI-II) San Antonio, TX: Pearson; 1996. [Google Scholar]
- Beshai S, Dobson KS, Bockting CLH, Quigley L. Relapse and recurrence prevention in depression: Current research and future prospects. Clin Psychol Rev. 2011;31:1349–1360. doi: 10.1016/j.cpr.2011.09.003. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Brent DA, Kolko D, Baugher M, Bridge J, Holder D, Iyengar S, Ulloa RE. Clinical outcome after short-term psychotherapy for adolescents with major depressive disorder. Arch Gen Psychiatry. 2000;57:29–36. doi: 10.1001/archpsyc.57.1.29. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Williamson DE, Dahl RE, Axelson DA, Kaufman J, Dorn LD, Ryan ND. Clinical presentation and course of depression in youth: Does onset in childhood differ from onset in adolescence? J Am Acad Child Adolesc Psychiatry. 2004;43:63–70. doi: 10.1097/00004583-200401000-00015. [DOI] [PubMed] [Google Scholar]
- Brent DA, Kolko DJ, Birmaher B, Baugher M, Bridge J, Roth C, Holder D. Predictors of treatment efficacy in a clinical trial of three psychosocial treatments for adolescent depression. J Am Acad Child Adolesc Psychiatry. 1998;17:906–914. doi: 10.1097/00004583-199809000-00010. [DOI] [PubMed] [Google Scholar]
- Burcusa SL, Iacono WG. Risk for recurrence in depression. Clin Psychol Rev. 2007;27:959–985. doi: 10.1016/j.cpr.2007.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cleves M, Gould W, Gutierrez RG, Marchenko YV. An introduction to survival analysis using stata. third. College Station, TX: Stata Press; 2010. [Google Scholar]
- Curry J, Silva S, Rohde P, Ginsburg G, Kratochvil C, Simons A, Kirchner T, May D, Kennard B, Mayes T, Feeny N, Albano AM, Lavanier S, Reinecke M, Jacobs R, Becker-Weidman E, Weller E, Emslie G, Walkup J, Kastelic E, Burns B, Wells K, March J. Recovery and recurrence following treatment for adolescent major depression. Arch Gen Psychiatry. 2011;68:263–270. doi: 10.1001/archgenpsychiatry.2010.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farb NAS, Irving JA, Anderson AK, Segal ZV. A two-factor model of relapse/recurrence vulnerability in unipolar depression. J Abnorm Psychol. 2015;124:38–53. doi: 10.1037/abn0000031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geller B, Zimerman B, Williams M, Bolhofner K, Craney JL. Bipolar disorder at prospective follow-up of adults who had prepubertal major depressive disorder. Am J Psychiatry. 2001;158:125–127. doi: 10.1176/appi.ajp.158.1.125. [DOI] [PubMed] [Google Scholar]
- Goldston DB, Daniel SS, Erkanli A, Heilbron N, Doyle O, Weller B, Sapyta J, Mayfield A, Faulkner M. Suicide attempts in a longitudinal sample of adolescents followed through adulthood: Evidence of escalation. J Consult Clin Psychol. 2015;83:253–264. doi: 10.1037/a0038657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardeveld F, Spijker J, De Graaf R, Nolen WA, Beekman ATF. Prevalence and predictors of recurrence of major depressive disorder in the adult population. Acta Psychiatr Scand. 2010;122:184–191. doi: 10.1111/j.1600-0447.2009.01519.x. [DOI] [PubMed] [Google Scholar]
- Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. [Google Scholar]
- Keller MB, Lavori PW, Endicott J, Coryell W, Klerman GL. “Double Depression”: two year follow-up. Am J Psychiatry. 1983;140:689–694. doi: 10.1176/ajp.140.6.689. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Zhao S, Blazer DG, Swartz M. Prevalence, correlates, and course of minor depression and major depression in the national comorbidity survey. J Affect Disord. 1997;45:19–30. doi: 10.1016/s0165-0327(97)00056-6. [DOI] [PubMed] [Google Scholar]
- Kovacs M, Akiskal HS, Gatsonis C, Parrone PL. Childhood-onset dysthymic disorder: Clinical features and prospective naturalistic outcome. Arch Gen Psychiatry. 1994;51:365–374. doi: 10.1001/archpsyc.1994.03950050025003. [DOI] [PubMed] [Google Scholar]
- Kovacs M, Devlin B, Pollock M, Richards C, Mukerji P. A controlled family history study of childhood-onset depressive disorder. Arch Gen Psychiatry. 1997;54:613–623. doi: 10.1001/archpsyc.1997.01830190033004. [DOI] [PubMed] [Google Scholar]
- Kovacs M, Feinberg TL, Crouse-Novak MA, Paulauskas SL, Finkelstein R. Depressive disorders in childhood: I. A longitudinal prospective study of characteristics and recovery. Arch Gen Psychiatry. 1984a;41:229–237. doi: 10.1001/archpsyc.1984.01790140019002. [DOI] [PubMed] [Google Scholar]
- Kovacs M, Feinberg TL, Crouse-Novak MA, Paulauskas SL, Pollock M, Finkelstein R. Depressive disorders in childhood: II. A longitudinal study of the risk for a subsequent major depression. Arch Gen Psychiatry. 1984b;41:643–649. doi: 10.1001/archpsyc.1984.01790180013001. [DOI] [PubMed] [Google Scholar]
- Kovacs M, Goldston D. Cognitive and social cognitive development of depressed children and adolescents. J Am Acad Child Adolesc Psychiatry. 1991;30:388–392. doi: 10.1097/00004583-199105000-00006. [DOI] [PubMed] [Google Scholar]
- Kovacs M, Paulauskas SL. Developmental stage and the expression of depressive disorders in children: An empirical analysis. New Dir Child Dev. 1984;26:59–80. [Google Scholar]
- Kraepelin E. Manic-depressive Insanity and Paranoia. Edinburgh: E & S Livingston; 1921. [Google Scholar]
- Leon AC, Solomon DA, Mueller TI, Endicott J, Rice JP, Maser JD, Coryell W, Keller MB. A 20-year longitudinal observational study of somatic antidepressant treatment effectiveness. Am J Psychiatry. 2003;160:727–733. doi: 10.1176/appi.ajp.160.4.727. [DOI] [PubMed] [Google Scholar]
- Luby JL, Heffelfinger AK, Mrakotsky C, Brown KM, Hessler MJ, Wallis JM, Spitznagel EL. The clinical picture of depression in preschool children. J Am Acad Child Adolesc Psychiatry. 2003;42:340–348. doi: 10.1097/00004583-200303000-00015. [DOI] [PubMed] [Google Scholar]
- Lui S, Wu Q, Qiu L, Yang X, Kuang W, Chan RCK, Huang X, Kemp GJ, Mechelli A, Gong Q. Resting-state functional connectivity in treatment-resistant depression. Am J Psychiatry. 2011;168:642–648. doi: 10.1176/appi.ajp.2010.10101419. [DOI] [PubMed] [Google Scholar]
- McCauley E, Myers K, Mitchell J, Calderon R, Schloredt K, Treder R. Depression in young people: Initial presentation and clinical course. J Am Acad Child Adolesc Psychiatry. 1993;32:714–722. doi: 10.1097/00004583-199307000-00003. [DOI] [PubMed] [Google Scholar]
- Monroe SM, Harkness KL. Recurrence in major depression: A conceptual analysis. Psychol Rev. 2011;118:655–674. doi: 10.1037/a0025190. [DOI] [PubMed] [Google Scholar]
- Mueller TI, Leon AC, Keller MB, Solomon DA, Endicott J, Coryell W, Warshaw M, Maser JD. Recurrence after recovery from major depressive disorder during 15 years of observational follow-up. Am J Psychiatry. 1999;156:1000–1006. doi: 10.1176/ajp.156.7.1000. [DOI] [PubMed] [Google Scholar]
- Pettit JW, Hartley C, Lewinsohn PM, Seeley JR, Klein DN. Is liability to recurrent major depressive disorder present before first episode onset in adolescence or acquired after the initial episode? J Abnorm Psychol. 2013;122:353–358. doi: 10.1037/a0032655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Post RM, Fleming J, Kapczinski F. Neurobiological correlates of illness progression in the recurrent affective disorders. J Psychiatr Res. 2012;46:561–573. doi: 10.1016/j.jpsychires.2012.02.004. [DOI] [PubMed] [Google Scholar]
- Posternak MA, Solomon DA, Leon AC, Mueller TI, Shea MT, Endicott J, Keller MB. The naturalistic course of unipolar major depression in the absence of somatic therapy. J Nerv Ment Dis. 2006;194:324–329. doi: 10.1097/01.nmd.0000217820.33841.53. [DOI] [PubMed] [Google Scholar]
- Rao U, Chen LA. Characteristics, correlates, and outcomes of childhood and adolescent depressive disorders. Dialogues Clin Neurosci. 2009;11:45–62. doi: 10.31887/DCNS.2009.11.1/urao. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao U, Hammen CL, Poland RE. Longitudinal course of adolescent depression: Neuroendocrine and psychosocial predictors. J Am Acad Child Adolesc Psychiatry. 2010;49:141–151. doi: 10.1097/00004583-201002000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renouf AG, Kovacs M, Mukerji P. Relationship of depressive, conduct, and comorbid disorders and social functioning in childhood. J Am Acad Child Adolesc Psychiatry. 1997;36:998–1004. doi: 10.1097/00004583-199707000-00023. [DOI] [PubMed] [Google Scholar]
- SAS Institute. Software and Guide. SAS/STAT® 9.2. Cary, NC: SAS Institute Inc; 2008. [Google Scholar]
- Segal ZV, Bieling P, Young T, MacQueen G, Cooke R, Martin L, Bloch R, Levitan RD. Antidepressant monotherapy vs sequential pharmacotherapy and mindfulness-based cognitive therapy, or placebo, for relapse prophylaxis in recurrent depression. Arch Gen Psychiatry. 2010;67:1256–1264. doi: 10.1001/archgenpsychiatry.2010.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shelton RC, Hollon SD. The long-term management of major depressive disorders. Journal of Lifelong Learning in Psychiatry. 2012;10:434–441. [Google Scholar]
- Sherrill JT, Kovacs M. Interview schedule for children and adolescents (ISCA) J Am Acad Child Adolesc Psychiatry. 2000;39:67–75. doi: 10.1097/00004583-200001000-00018. [DOI] [PubMed] [Google Scholar]
- Solomon DA, Keller MB, Leon AC, Mueller TI, Shea MT, Warshaw M, Maser JD, Coryell W, Endicott J. Recovery from major depression: A 10-year prospective follow-up across multiple episodes. Arch Gen Psychiatry. 1997;54:1001–1006. doi: 10.1001/archpsyc.1997.01830230033005. [DOI] [PubMed] [Google Scholar]
- Solomon DA, Keller MB, Leon AC, Mueller TI, Lavori PW, Shea MT, Coryell W, Warshaw M, Turvey C, Maser JD, Endicott J. Multiple recurrences of major depressive disorder. Am J Psychiatry. 2000;157:229–233. doi: 10.1176/appi.ajp.157.2.229. [DOI] [PubMed] [Google Scholar]
- Solomon DA, Leon AC, Coryell W, Mueller TI, Posternak M, Endicott J, Keller MB. Predicting recovery from episodes of major depression. J Affect Disord. 2008;107:285–291. doi: 10.1016/j.jad.2007.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release 11. College Station, TX: StataCorp LP; 2009a. [Google Scholar]
- StataCorp. Stata 11 Base Reference Manual. College Station, TX: Stata Press; 2009b. [Google Scholar]
- Weissman MM, Wolk S, Goldstein RB, Moreau D, Adams P, Greenwald S, Klier CM, Ryan ND, Dahl RE, Wickramaratne P. Depressed adolescents grown up. JAMA. 1999a;281:1707–1713. doi: 10.1001/jama.281.18.1707. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Wolk S, Wickramaratne P, Goldstein RB, Adams P, Greenwald S, Ryan ND, Dahl RE, Steinberg D. Children with prepubertal-onset major depressive disorder and anxiety grown up. Arch Gen Psychiatry. 1999b;56:794–801. doi: 10.1001/archpsyc.56.9.794. [DOI] [PubMed] [Google Scholar]
- Wilson S, Vaidyanathan U, Miller MB, McGue M, Iacono WG. Premorbid risk factors for major depressive disorder: are they associated with early onset and recurrent course? Dev Psychopathol. 2014;26:1477–1493. doi: 10.1017/S0954579414001151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zisook S, Lesser I, Stewart JW, Wisniewski SR, Balasubramani GK, Fava M, Gilmer WS, Dresselhaus TR, Thase ME, Nierenberg AA, Trivedi MH, Rush AJ. Effect of age at onset on the course of major depressive disorder. Am J Psychiatry. 2007;164:1539–1546. doi: 10.1176/appi.ajp.2007.06101757. [DOI] [PubMed] [Google Scholar]