Abstract
Transitional care may be an effective strategy for preparing older adults for transitions from skilled nursing facilities (SNF) to home. In this systematic review, studies of patients discharged from SNFs to home were reviewed. Study findings were assessed (1) to identify whether transitional care interventions, as compared to usual care, improved clinical outcomes such as mortality, readmission rates, quality of life or functional status; and (2) to describe intervention characteristics, resources needed for implementation, and methodologic challenges. Of 1,082 unique studies identified in a systematic search, the full texts of six studies meeting criteria for inclusion were reviewed. Although the risk for bias was high across studies, the findings suggest that there is promising but limited evidence that transitional care improves clinical outcomes for SNF patients. Evidence in the review identifies needs for further study, such as the need for randomized studies of transitional care in SNFs, and methodological challenges to studying transitional care for SNF patients.
Introduction
Annually in the U.S., nearly 2 million older adults receive post-acute care in skilled nursing facilities (SNF).1 Older adults who enter SNFs following hospitalization are at risk for poor patient outcomes, such as deteriorating health, hospital readmissions, and death.2,3 When they complete care in SNFs and transition to home, SNF patients’ advanced age, frailty, comorbidity and limited social support contribute to poor outcomes.3,4 Transitional care provided by SNF staff members is an important and potentially modifiable factor to improve these outcomes. Transitional care ideally will prepare patients and their caregivers to provide self-care and coordinate medical services after transitions from SNFs to home and other settings.5 However, unlike transitional care for hospital discharge, transitional care from SNF to home is rarely evaluated or improved upon.
Evidence from clinical trials indicates that outcomes of hospitalized patients (e.g., satisfaction, preparedness for discharge and hospital readmissions in 30 days) are improved when hospital and other professional provide transitional care services.6,7 Designed to promote continuity and coordination of care during patient transitions in care, effective models of transitional care in acute care include a heterogeneous combination of pre, post, and “bridging” discharge interventions done by different professional staff at different times.8 Transitional care may be an appropriate strategy to improve clinical outcomes of SNF patients.6,9–11 Evidence is needed to assess further research needs and, where possible, to guide the clinical practice of nurses and other health professionals. To synthesize existing evidence, a systematic review of published research was conducted, with the objectives of describing 1) associations of transitional care interventions and clinical outcomes of SNF patients, and 2) characteristics of interventions, resources needed for implementation, and methodologic challenges.
Methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) was used to guide the search, abstraction, synthesis and review.12,13
Search
A research librarian was consulted to identify randomized controlled trials, non-randomized controlled trials, and non-randomized before and after studies that were published in English after January 1, 2000. The PubMed, CINAHL and Embase databases were searched on September 1, 2015. The Pubmed search was conducted using the following algorithm: [(“continuity of care” OR “care continuum” OR “continuum of care” OR “care coordination” OR “coordination of care” OR “care planning” OR “care plan”) OR (Transition*[tw] AND (care[tw] OR caring[tw] OR healthcare[tw] OR coordinat*[tw] OR track*[tw])) OR ((Patient[tw] OR patients[tw] OR patient's[tw]) AND (transfer*[tw] OR handover*[tw] OR handoff*[tw] OR coordinat*[tw])) OR ((“Patient Handoff”[Mesh] OR “Patient Navigation”[Mesh] OR “Case Management”[Mesh] OR “Patient Care Planning”[Mesh] OR “Patient Care Management”[Mesh] OR “Continuity of Patient Care”[Mesh]))] AND [(“Residential Facilities”[Mesh:NoExp] OR “Assisted Living Facilities”[Mesh] OR “Nursing Homes”[Mesh]) OR “skilled nursing”[tw] OR “skilled facility”[tw] OR “skilled facilities”[tw] OR SNF[tw]] AND [ (Discharg*[tw] OR postdischarg*[tw] OR post-discharg*[tw]) OR “Patient Discharge”[Mesh]]. Other databases using similar search terms were searched. Also, reference lists, research databases (NIH RePORTER, clinicaltrials.gov) were hand searched and experts in the field were consulted to locate additional studies.
Data Abstraction
Two reviewers (MT and JA) separately reviewed abstracts. Studies were included for full text review if they: 1) included data on randomized, non-randomized concurrent or historical controls, 2) targeted older adults who discharged from SNFs to home, and 3) described the influence of interventions on at least one clinical outcome such as mortality, hospital readmission rates, preparedness for discharge, and functional status. Two reviewers read the full text of selected studies to identify the final set for data abstraction.
Two reviewers abstracted data (MT and JA). Studies were categorized as randomized controlled trials, non-randomized controlled trials, and non-randomized before and after studies. Abstracted data included study and participant characteristics, risk of bias, intervention characteristics, implementation characteristics, clinical outcomes. Risk of bias was described with the Cochrane Collaboration’s “Tool for Assessing Risk of Bias” (e.g., allocation, attrition, selection, performance, detection, reporting); also Cochrane criteria were used to evaluate the risk of bias as low, high or unclear.14 Intervention characteristics were described using the “Taxonomy of Interventions to Reduce 30-day Re-hospitalization,” which includes: (a) predischarge services (discharge planning, patient teaching, medication reconciliation, appointment scheduled before discharge), (b) postdischarge services (e.g., timely follow-up, timely communication with follow-up clinicians, follow-up telephone call, patient hotline, home visit) and (c) bridging interventions (transition coach, patient-centered discharge instructions, provider continuity).8 Based on the Contextual Frameworks for Research on the Implementation of Complex System Interventions,15 five criteria were developed for describing the resources needed to implement interventions, including new staff, use of electronic medical records systems, specialized training for existing SNF staff and targeting the intervention for primary caregivers and/or patients. The corresponding author of one study was contacted to clarify data about the population included in the study. Abstractors resolved differences by consensus.
Data Synthesis
Data tables were created to categorize studies by population, intervention and control, outcomes, design, risk for bias, and resources needed for implementation. Heterogeneity between studies precluded meta-analysis; thus, associations between types of transitional care services and clinical outcomes were qualitatively described. All research team members participated in the synthesis of study findings.
Results
Study Characteristics
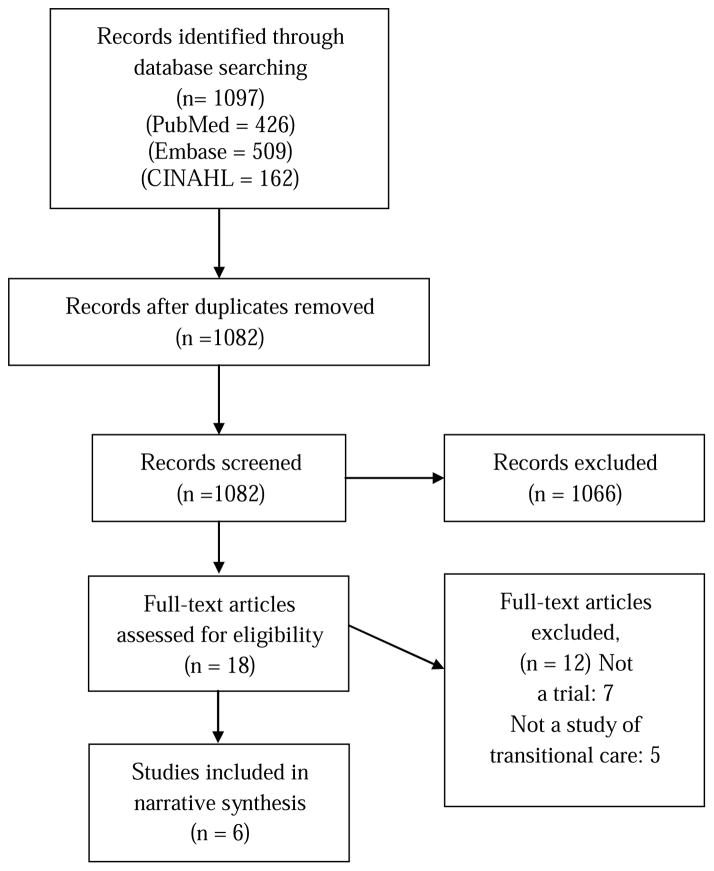
The search yielded 1,082 unique studies (Figure 1). The full texts of 18 studies were reviewed and 6 studies were found that met criteria for inclusion in the review (Table 1). Studies were published between 2001 and 2013, were conducted in the U.S., and tested transitional care for patients in individual SNF sites, 16–18 and in SNFs affiliated with a Veteran’s Affairs hospital, 19 a hospital in a health maintenance organization, 20 and a county human services department.21
Figure 1.
Flow of Study Search and Selection
Table 1.
Main Study Findings1
| Study | Design | Population | Intervention and Control | Main Outcomes (control vs. intervention) |
|---|---|---|---|---|
| Newcomer et. al, 2006 | RCT | Patients in 4 SNF
|
|
|
| Dolansky et al., 201117 | RCT | Cardiac patients in 5 SNF and 1 HHA
|
|
|
| Delate et al., 200820 | Non-randomized controlled trial | Patients in 1 HMO
|
|
|
| Tappen et al., 200118 | Non-randomized controlled before and after | Patients in 1 SNF
|
|
|
| Park et al., 201219 | Non-randomized before and after | Patients from 1 VA Hospital
|
|
|
| Berkowitz, et al. 201316 | Non-randomized before and after | Patients in 1 SNF
|
|
|
RCT=Randomized controlled trial, Intv.=Intervention, HMO=Health maintenance organization, HR=hazard ratio, CI=Confidence interval, SNF=Skilled nursing facility, HHA=Home health agency, FIM=Functional Independence Measure, VA=Veteran’s Affairs, NP=Nurse practitioner, ED=Emergency department, OD=Odds ratio
The range of the odds ratio for these 4 single item scales is reported.
Sample Characteristics
Across studies, a total of 619 older adults were intervention subjects, with sample sizes ranging from 17–217. In 5 studies, participants had average age ranging from 77–80 years; female gender (61–74%); white non-Hispanic race (73–89%); and diverse medical conditions such as fractures, congestive heart failure and pneumonia. In one study, participants were 95% male, 19 and in a second study, participants were treated exclusively for cardiac medical conditions.17
Risk of Bias
Using the Cochrane Collaboration criteria, the potential for bias in all the reviewed studies was estimated as high. Two studies used a randomized controlled design; however, these studies were conducted with samples of 33 or fewer older adults in the intervention group and did not clearly satisfy four of five of the Cochrane criteria.21 Of four studies with non-random controls, one used a concurrent control group20 and three were before and after quasi-experimental studies.16,18,19 While blinding was not feasible for study interventionists and patients, no study explicitly required data collectors to be masked to intervention or control status, which may have contributed to performance bias in study findings. Third, the similarity of intervention and control groups at baseline was not clear; for example, studies included intervention and control samples with comparable age, gender and race; however, differences in patients (such as functional status, caregiver support and community supports) were not specified. This limitation was addressed in one before and after study, in which the investigators used propensity score analysis to develop a statistical model for testing the intervention.16 Fourth, it was not clear how comparable conditions were maintained throughout the study period; studies did not describe the degree to which participants received components of bundles of intervention and usual care services. Finally, in three studies where patient or caregiver self-reported outcomes were assessed, the rate that participants were lost to follow-up was not clear in one study18 and greater than 20% in one other.17
Intervention Characteristics
Studies reported tests of different combinations of predischarge, postdischarge and bridging transitional care services; however, data from the review were insufficient data to describe the efficacy of different combinations of services (Table 2). Three studies tested a combination of pre-, post-, and bridging services. For example, in Tappen, 18 SNF nurses planned discharges, provided patient-centered instructions to bridge care in the SNF and home, and made telephone calls and home visits after discharge. One study tested a combination of new predischarge and postdischarge services; in Newcomer, 21 an added transitional care nurse prepared patients for discharge and an added social worker worked with the patient and caregivers after discharge at home. One study tested a combination of usual care predischarge services and a new postdischarge service; in Delate, 20 before discharge, SNF staff provided usual care and, after discharge, pharmacists in the health maintenance organization reconciled medications and, as needed, made follow-up calls with patients and/or physicians.
Table 2. Transitional Care Interventions.
1 (Usual care was described for protocols that added transitional care services to usual care)
| Study | Predischarge Services | Bridging Services | Postdischarge Services | Implementation Characteristics |
|---|---|---|---|---|
| Newcomer et. al, 200621 |
|
None reported |
|
|
| Delate et al., 200820 |
|
None reported |
|
|
| Tappen et al., 200118 |
|
|
|
|
| Dolansky et al., 201117 |
|
|
|
|
| Park et al., 201219 |
|
|
|
|
| Berkowitz, et al. 201316 |
|
|
|
|
RN= Registered Nurse, SW=Social worker, SNF=Skilled nursing facility, NP=Nurse practitioner, EMR=Electronic medical record
Usual Care included discharge planning, patient teaching, referrals and recommendations for follow-up medical care.
Resources Needed for Implementation
In three studies, providers of transitional care were existing SNF staff that had been trained to use new procedures and tools;16–18 in three studies, providers of transitional care were added staff, including a part time registered nurse and full time social worker,21 nurse practitioners and a supervising geriatrician,19 and clinical pharmacists.20 In four studies, transitional care was delivered in the SNFs and in two others, based in more integrated health systems, staff working outside of the SNFs delivered care, including pharmacists in a health care management call center20 and nurse practitioners located in a geriatric clinic affiliated with a Veteran’s Affairs Hospital.19 In three studies, new tools (such as screening and assessment templates) for providing transitional care were embedded in electronic medical records systems.16,19,20 Five studies indicated that patients and family caregivers were included as targets of the intervention; for example, in Newcomer,21 intervention staff visited homes of patients and comprehensively assessed caregivers’ needs and encouraged their participation in care.
Clinical Outcomes
Studies included diverse clinical outcomes; outcomes were classified as (a) Acute Care Use 30 or 60 Days after SNF Discharge and (b) Mortality and Other Outcomes, which included mortality, satisfaction with transitional care, function, and participation in clinical services after discharge. In the following, reviewed studies are described and evaluated the by type of clinical outcome.
Acute Care Use 30 or 60 Days after SNF Discharge
Studies of transitional care interventions and hospital readmissions in 30 or 60 days after SNF discharge were mixed. In four of six studies reporting this outcome, interventions were not associated with a decreased rate of hospital readmissions. For example, in Newcomer (a randomized controlled trial) 21 no difference in hospital readmissions was observed among control and intervention patients. However, there was not sufficient information in these four studies to determine whether they were adequately powered for this endpoint. In two nonrandomized studies, interventions were associated with a decreased rate of hospital readmissions. For example, in Park, 19 a significantly higher rate of hospital readmissions was observed in control relative to intervention groups (23% vs. 14%, p=0.02). In a another study, which adapted an evidence-based transitional care model (Re-engineered Discharge Planning),16 intervention patients, compared to those who received usual care, had lower odds of hospital readmission in 30 days (odds ratio (OR) 0.69, p<0.045). In addition, in three of six studies which examined the impact of transitional care interventions on emergency department (ED) use after SNF discharge19–21 no significant difference was observed for intervention and control subjects. Findings across studies were limited by potential biases from observational designs, small samples and un-blinded outcomes assessment. However, studies suggest that a combination of robust predischarge services and at least some postdischarge services, may contribute to the effect of interventions on hospital readmission.
Mortality and Other Outcomes
Studies in the review did not provide sufficient data for describing the effects of transitional care services on mortality, patient satisfaction, physical function or follow-up care after discharge. Mortality after discharge was assessed in only one study, in which a pharmacist-led intervention, when added to usual care, was associated with lower risk of any cause of death in the 30 days after SNF discharge (hazard ratio (HR) 0.22, CI: 0.06–0.8=).20 Findings were limited by the risk for bias in the study design that used a non-random allocation procedure and a small sample size for SNF patients in one health maintenance organization.
Other outcome measures included satisfaction with transitional care, physical function and participation in follow-up medical care after SNF discharge. Satisfaction with transitional care was assessed in only two studies; findings indicated that interventions, compared to usual care, were associated with improved patient satisfaction.16,18 Physical function after SNF discharge was examined in two studies and results were mixed.17,18 In one study, physical function after discharge to home was the same for SNF patients who received supplemental teaching and discharge instructions about cardiac rehabilitation, compared to the control group.17 In a another study, physical function, measured with the Functional Independence Measure (FIM), was greater for intervention subjects, compared to those in control group, after SNF discharge.18 Finally, participation in follow-up care after discharge was assessed in two studies.16,17 In one study, patients in the intervention group were more likely than those in the control group to attend medical appointments (OR 1.56, p=0.001).16 In a second study, patients in the intervention group were more likely than those in control group to attend cardiac rehabilitation (χ2 = 4.5, p<0.05).17
Discussion
SNF patient outcomes within 90 days of transitions from SNFs to home are poor; approximately 20% visit EDs without hospitalization, 30% are re-hospitalized and 8% die.3 Transitional care services designed for hospital patients who transfer home will likely need to be modified to implement in SNFs for several reasons.22 First, SNF patients, compared to hospital patients, tend to be older (average age is greater than 80 years); to be hospitalized for unplanned changes in health (such as falls and exacerbation of chronic illnesses); to have longer hospital admissions;23 and to have higher levels of pre-illness functional dependence, cognitive impairment, and co-morbidities. Second, SNF patients experience additional transitions in care (hospital to SNF to home, sometimes with additional SNF to hospital to SNF transitions), which compound the risk for omissions in medical care, such as unreconciled medication orders and poor hand-offs of clinical care between providers.2,24 Third, resource and staffing constraints in SNFs may limit the quality of services available to SNF patients and caregivers to prepare them for effective self-care at home.4,5 Thus, unique transitional care services may be necessary to improve clinical and financial outcomes after care in SNFs.
In studies reviewed, there is promising but limited evidence that transitional care improves clinical outcomes for SNFs patients. Patients that received transitional care, compared to those in control groups, had improved clinical outcomes, such as the rate of re-hospitalization and mortality after SNF discharge.16,18–20 Limited findings suggested that transitional care interventions were associated with improvements in quality of life (e.g., physical function). However, there was considerable heterogeneity in transitional care interventions, resources needed to implement interventions, and outcome measures across the six studies included in the review. However, outcomes were inconsistent and the risk of bias in all studies was high. Thus, evidence is not yet available for recommending transitional care to improve clinical outcomes for SNF patients. Evidence in the review does identify needs for further study and methodological challenges to studying transitional care for SNF patients, which are described below.
Findings in the review suggest strategies for testing whether and how transitional care services improve clinical outcomes. Across studies, interventions involved changes in the organization of patient care (such as new procedures for planning care and resources in electronic medical records); thus, implementing transitional care in SNFs will likely require strong administrative support. Findings in two more effective studies (Berkowitz16 and Tappen18) suggest that the cost of adding staff to provide transitional care is potentially avoidable, provided that existing SNF staff are adequately trained and supported. Finally, the high risk for bias in existing studies suggests that future studies will require more robust experimental designs. Thus, an ideal future study might be a cluster randomized trial (randomized at the level of individual SNFs), in which investigators evaluate the degree to which interventions with pre, post and bridging transitional care services alter clinical outcomes of SNF patients within 30 days of returning home. However, the optimal combination of pre, post and bridging transitional care services to support SNF patients and caregivers is not yet known. Hospital-based studies suggest that predischarge services (assessment, care planning, and education) directed at the patient can be sufficient to prepare them for successful transitions to home;25 however, because of the prevalence of functional impairment in SNF patients, future studies in SNFs will likely need to test these predischarge services for both patients and their family caregivers, who are frequently the main providers of care for SNF patients at home.26–28 Reviewed studies suggest the feasibility of delivering bridging services in SNFs,16,18,19,29 such as providing patient-centered discharge instructions; a goal of future studies will also be to design useful discharge instructions and test whether more patient- and family- centered tools contribute to clinical successes at home. Finally, effective hospital-based transitional care interventions commonly include post-discharge services, but follow-up calls and home visits were tested in only two reviewed studies.20,21 Future studies are needed to determine when home visits, versus follow-up calls are needed, and how long postdischarge services should continue (7, 30, 90 days or longer). Moreover, future research will also be needed to determine how to coordinate transitional care services among groups of staff within SNFs and among service providers outside of SNFs, such as care coordinators, coaches or navigators in bundled care arrangements and patient-centered medical homes.
These findings also suggest the need for research to address measurement challenges related to transitional care for SNF patients. In the reviewed studies, investigators frequently assessed clinical outcomes using the rate of re-hospitalization and measures of physical function. In the context of care for SNF patients, these measures are limited by: (a) the heterogeneity of SNF patients (e.g., patients with and without chronic medical conditions/functional limitations before the index hospitalization)3 and (b) the availability of social support after SNF discharge, which is likely a strong predictor of utilization or functional decline.30,31 Thus, in future studies, approaches for addressing these challenges will be necessary; for example, evaluating changes in outcomes over time, as opposed to cross sectional measurement, and evaluating outcomes using multiple perspectives, such as patient- and caregiver- reported outcomes and administrative data. In addition, new measures are also needed to assess intermediate outcomes of transitional care, including measures of patient and caregiver preparedness for continuing health care activities at home, and measures of clinician preparedness for assuming care of SNF patients after discharge.
The focus of this systematic review was interventions that were designed to improve transitions in care from SNFs to home, which meant that the review did not include studies of transitional care across the continuum of care; for example, hospital-based studies that tested interventions with post-discharge services that continued from the hospital to the SNF to home or studies of large integrated health systems with transitional care services spanning the continuum of care. However, the reviewed studies do provide evidence for designing services that specifically target care of patients during and immediately after their care in SNFs.
Conclusion
Findings in this systematic review suggest promising but limited evidence that transitional care improves clinical outcomes for SNFs patients. Future studies using randomized experimental designs are needed to test the efficacy of providing pre, post and bridging transitional care interventions to reduce acute care use and improve other clinical outcomes for SNF patients and their caregivers after transitions from SNFs to home.
Acknowledgments
BLINDED work in this study was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, grant number BLINDED.
Abbreviations
- SNF
skilled nursing facilities
- ED
emergency department
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Mark Toles, Email: mtoles@email.unc.edu, University of North Carolina at Chapel Hill, School of Nursing, Carrington Hall, CB#7460, Chapel Hill, NC 27599, USA.
Cathleen Colón-Emeric, Email: cathleen.colonemeric@duke.edu, Duke University, School of Medicine, 2100 Erwin Rd, Durham, NC 27705, USA.
Josephine Asafu-Adjei, Email: jasafuad@email.unc.edu, University of North Carolina at Chapel Hill, School of Nursing, Carrington Hall, CB#7460, Chapel Hill, NC 27599, USA.
Elizabeth Moreton, Email: emoreton@email.unc.edu, University of North Carolina, Health Sciences Library, 335 S. Columbia Street CB#7585, Chapel Hill, NC 27599-7585, USA.
Laura C. Hanson, Email: laura_hanson@med.unc.edu, University of North Carolina, School of Medicine, 321 S Columbia St, Chapel Hill, NC 27516, USA.
References
- 1.Medicare Payment Advisory Commission. Report to Congress. [Accessed April 7, 2015];Medicare Payment Policy. 2013 http://www.medpac.gov/-documents-/reports.
- 2.Coleman EA, Min SJ, Chomiak A, Kramer AM. Posthospital care transitions: patterns, complications, and risk identification. Health Serv Res. 2004 Oct;39(5):1449–1465. doi: 10.1111/j.1475-6773.2004.00298.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Toles M, Anderson RA, Massing M, et al. Restarting the cycle: incidence and predictors of first acute care use after nursing home discharge. J Am Geriatr Soc. 2014 Jan;62(1):79–85. doi: 10.1111/jgs.12602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Popejoy LL, Dorman Marek K, Scott-Cawiezell J. Patterns and problems associated with transitions after hip fracture in older adults. J Gerontol Nurs. 2013 Sep;39(9):43–52. doi: 10.3928/00989134-20130620-01. [DOI] [PubMed] [Google Scholar]
- 5.Toles M, Barroso J, Colon-Emeric C, Corazzini K, McConnell E, Anderson RA. Staff interaction strategies that optimize delivery of transitional care in a skilled nursing facility: a multiple case study. Fam Community Health. 2012 Oct-Dec;35(4):334–344. doi: 10.1097/FCH.0b013e31826666eb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Naylor MD, Aiken LH, Kurtzman ET, Olds DM, Hirschman KB. The care span: The importance of transitional care in achieving health reform. Health Aff (Millwood) 2011 Apr;30(4):746–754. doi: 10.1377/hlthaff.2011.0041. [DOI] [PubMed] [Google Scholar]
- 7.Verhaegh KJ, MacNeil-Vroomen JL, Eslami S, Geerlings SE, de Rooij SE, Buurman BM. Transitional care interventions prevent hospital readmissions for adults with chronic illnesses. Health Aff (Millwood) 2014 Sep 1;33(9):1531–1539. doi: 10.1377/hlthaff.2014.0160. [DOI] [PubMed] [Google Scholar]
- 8.Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011 Oct 18;155(8):520–528. doi: 10.7326/0003-4819-155-8-201110180-00008. [DOI] [PubMed] [Google Scholar]
- 9.Coleman EA, Berenson RA. Lost in transition: challenges and opportunities for improving the quality of transitional care. Ann Intern Med. 2004 Oct 5;141(7):533–536. doi: 10.7326/0003-4819-141-7-200410050-00009. [DOI] [PubMed] [Google Scholar]
- 10.Oakes SL, Gillespie SM, Ye Y, et al. Transitional care of the long-term care patient. Clin Geriatr Med. 2011 May;27(2):259–271. doi: 10.1016/j.cger.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 11.Toles M, Colon-Emeric C, Barroso J, Naylor M, Anderson RA. Safely returning home: Strategies for improving transitional care in nursing homes. J Am Med Dir Assoc. in review. [Google Scholar]
- 12.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS medicine. 2009 Jul 21;6(7):e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Vol. 2011 The Cochrane Collaboration; 2011. [Google Scholar]
- 15.Rojas Smith L, Ashok M, Dy SM, Wines RC, Teixeira-Poit S. Contextual Frameworks for Research on the Implementation of Complex System Interventions. Methods Research Report. Rockville, MD: Agency for Healthcare Research and Quality; 2014. [PubMed] [Google Scholar]
- 16.Berkowitz RE, Fang Z, Helfand BK, Jones RN, Schreiber R, Paasche-Orlow MK. Project ReEngineered Discharge (RED) Lowers Hospital Readmissions of Patients Discharged From a Skilled Nursing Facility. J Am Med Dir Assoc. 2013 Oct;14(10):736–740. doi: 10.1016/j.jamda.2013.03.004. [DOI] [PubMed] [Google Scholar]
- 17.Dolansky MA, Zullo MD, Boxer RS, Moore SM. Initial efficacy of a cardiac rehabilitation transition program: Cardiac TRUST. J Gerontol Nurs. 2011 Dec;37(12):36–44. doi: 10.3928/00989134-20111103-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tappen RM, Hall RF, Folden SL. Impact of comprehensive nurse-managed transitional care. Clin Nurs Res. 2001 Aug;10(3):295–313. doi: 10.1177/c10n3r6. [DOI] [PubMed] [Google Scholar]
- 19.Park HK, Branch LG, Bulat T, Vyas BB, Roever CP. Influence of a transitional care clinic on subsequent 30-day hospitalizations and emergency department visits in individuals discharged from a skilled nursing facility. J Am Geriatr Soc. 2013 Jan;61(1):137–142. doi: 10.1111/jgs.12051. [DOI] [PubMed] [Google Scholar]
- 20.Delate T, Chester EA, Stubbings TW, Barnes CA. Clinical outcomes of a home-based medication reconciliation program after discharge from a skilled nursing facility. Pharmacotherapy. 2008 Apr;28(4):444–452. doi: 10.1592/phco.28.4.444. [DOI] [PubMed] [Google Scholar]
- 21.Newcomer R, Kang T, Graham C. Outcomes in a nursing home transition case-management program targeting new admissions. Gerontologist. 2006 Jun;46(3):385–390. doi: 10.1093/geront/46.3.385. [DOI] [PubMed] [Google Scholar]
- 22.Toles M, Young M, Ouslander JG. Improving Care Transitions in Nursing Homes. Generations. 2012;36(4):78–85. [Google Scholar]
- 23.Burke RE, Juarez-Colunga E, Levy C, Prochazka AV, Coleman EA, Ginde AA. Patient and Hospitalization Characteristics Associated With Increased Postacute Care Facility Discharges From US Hospitals. Med Care. 2015 Jun;53(6):492–500. doi: 10.1097/MLR.0000000000000359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Coleman EA. Falling through the cracks: Challenges and opportunities for improving transitional care for persons with continuous complex care needs. J Am Geriatr Soc. 2003 Apr;51(4):549–555. doi: 10.1046/j.1532-5415.2003.51185.x. [DOI] [PubMed] [Google Scholar]
- 25.Kripalani S, Jackson AT, Schnipper JL, Coleman EA. Promoting effective transitions of care at hospital discharge: A review of key issues for hospitalists. Journal of Hospital Medicine. 2007 Sep;2(5):314–323. doi: 10.1002/jhm.228. [DOI] [PubMed] [Google Scholar]
- 26.Coleman EA, Min SJ. Patients' and Family Caregivers' Goals for Care During Transitions Out of the Hospital. Home Health Care Serv Q. 2015 Oct 23; doi: 10.1080/01621424.2015.1095149. [DOI] [PubMed] [Google Scholar]
- 27.Coleman EA, Roman SP. Family caregivers' experiences during transitions out of hospital. J Healthc Qual. 2015 Jan-Feb;37(1):12–21. doi: 10.1097/01.JHQ.0000460117.83437.b3. [DOI] [PubMed] [Google Scholar]
- 28.Levine C, Halper D, Peist A, Gould DA. Bridging troubled waters: family caregivers, transitions, and long-term care. Health Aff (Millwood) 2010 Jan-Feb;29(1):116–124. doi: 10.1377/hlthaff.2009.0520. [DOI] [PubMed] [Google Scholar]
- 29.Dolansky MA, Hitch JA, Pina IL, Boxer RS. Improving heart failure disease management in skilled nursing facilities: lessons learned. Clin Nurs Res. 2013 Nov;22(4):432–447. doi: 10.1177/1054773813485088. [DOI] [PubMed] [Google Scholar]
- 30.Kind AJ, Jencks S, Brock J, et al. Neighborhood socioeconomic disadvantage and 30-day rehospitalization: a retrospective cohort study. Ann Intern Med. 2014 Dec 2;161(11):765–774. doi: 10.7326/M13-2946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reinhard SC, Levine C, Samis S. [Accessed February 20, 2014];Home Alone: Family Caregivers Providing Complex Chronic care. 2012 http://www.aarp.org/home-family/caregiving/info-10-2012/home-alone-family-caregivers-providing-complex-chronic-care.html.