Abstract
Introduction
This study examined changes in self-management behaviors after high school graduation in a cohort of emerging adults with type 1 diabetes.
Methods
Sixty-four emerging adults reported on diabetes self-management behaviors at three time points over a one year period. Glycemic control and blood glucose monitoring frequency were collected from medical chart review.
Results
Collaboration with parents decreased, diabetes problem-solving and communication increased, and glycemic control worsened over the first year post-high school (ps<.05). Problem solving appeared to be protective against worsening glycemic control; higher baseline diabetes problem solving significantly predicted better glycemic control at the one year follow-up.
Discussion
Emerging adults demonstrate increased independence in diabetes problem solving and communication with health care providers in the year post-high school. Problem-solving skills may help emerging adults adapt type 1 diabetes self-care in response to unpredictable schedules post high-school, and promoting these skills may prevent deteriorations in glycemic control during this risky period.
Keywords: type 1 diabetes, adolescents, self-management, adherence, glycemic control, problem solving
Introduction
Type 1 diabetes is a common childhood chronic illness which affects more than 1 in every 500 children, corresponding to over 165,000 American youth under age 20 living with diabetes (Pettitt et al., 2014). The treatment of type 1 diabetes involves rigorous self-control and management, including several daily insulin injections or use of an insulin pump, measurement of blood glucose (BG) levels four to six times per day, regulation of carbohydrate intake, routine physical activity, and the prevention of acute and long term complications (American Diabetes Association, 2015; Chiang, Kirkman, Laffel, & Peters, 2014). This requires youth to be highly self-motivated and increasingly independent in order to meet glycemic goals and maintain a healthy lifestyle.
Emerging adulthood marks a point of transition for patients with type 1 diabetes with its own unique set of challenges and consequences (Garvey, Markowitz, & Laffel, 2012). In this developmental period which spans from ages 18 to 25, youth are no longer dependent adolescents reliant solely on parents, but are not yet ready to assume the full responsibilities of adulthood (Arnett, 2000). During this period, youth typically assume full responsibility for key tasks related to their diabetes management, including but not limited to BG monitoring, scheduling clinician appointments, planning and preparing meals, and awareness of hemoglobin A1c (A1c) goals (Hanna et al., 2013; Schilling, Knafl, & Grey, 2006). Many emerging adults with type 1 diabetes also experience a decrease in parental monitoring and involvement due, in part, to moving away for college or entering the workforce after high school graduation (Peters, Laffel, & American Diabetes Association Transitions Working Group, 2011). Likely influenced by these simultaneous transitions, emerging adulthood is associated with worsening glycemic control, acute complications, and poor long term health outcomes for youth with type 1 diabetes (Bryden, Dunger, Mayou, Peveler, & Neil, 2003; Bryden et al., 2001; Peters et al., 2011). Few emerging adults meet the American Diabetes Association recommendation for glycemic control for adults (A1c < 7.0%) (American Diabetes Association, 2015). However, research has shown that adolescence and emerging adulthood are critical times to establish lifelong healthy habits and routines (Nelson, Story, Larson, Neumark-Sztainer, & Lytle, 2008; Schulenberg, Sameroff, & Cicchetti, 2004). Therefore, identification and evaluation of salient self-management behaviors in emerging adults with type 1 diabetes is needed to better understand which skills are important during this transition to adulthood, and what factors are protective against worsening health outcomes.
The Self-Management of Type 1 Diabetes in Adolescents scale (SMOD-A) is a self-report measure which was designed to broaden the scope of measurement of diabetes self-care skills and provide clinicians with a tool to evaluate and promote self-management in youth with type 1 diabetes (Schilling et al., 2009). The SMOD-A identifies five separate categories of self-management: Collaboration with Parents, Diabetes Care Activities, Diabetes Problem Solving, Diabetes Communication, and Goals. It is a reliable self-report measure with good content validity with experiential experts (adolescents with type 1 diabetes and their parents) as well as professorial experts (Schilling et al., 2007). Therefore, this questionnaire is a valid tool which can be used to gather information about self-management skills in emerging adults and may provide insight into various aspects of behavior which facilitate better glycemic control.
Previous studies using the SMOD-A have found that youth with a shorter duration of diabetes perform more diabetes care activities and report more communication regarding their diabetes than do youth with a longer disease duration (Chao, Whittemore, Minges, Murphy, & Grey, 2014). Diabetes self-management also mediates the relationships between depression and family functioning with glycemic control and quality of life (Whittemore et al., 2014). Furthermore, one cross-sectional study has examined differences in SMOD-A scores between early, middle and late adolescents/emerging adults, finding less collaboration with parents and more problem solving capabilities in emerging adults as compared to younger adolescents (Keough, Sullivan-Bolyai, Crawford, Schilling, & Dixon, 2011).
While research has used the SMOD-A to evaluate the adolescent population cross-sectionally, little is known about its benefit in a longitudinal framework and potential applications in an emerging adult sample undergoing significant transitions over a 1 year period. By consistently using the same cohort of emerging adults, the variability between youth surveyed at different ages will be diminished, allowing interpretation of trends over a 1 year time frame. The specific aim of this study was to examine differences in self-management behaviors during a 1 year period in a cohort of emerging adults with type 1 diabetes as they transitioned from senior year of high school into their first year of college or work post-graduation. We hypothesized that the SMOD-A would capture increases in self-management behaviors evidenced over this time and self-report on the SMOD-A would be associated with indicators of diabetes care, including A1c, BG monitoring frequency, and mean BG level.
Methods
Data were drawn from a longitudinal study evaluating executive function, adherence, and parental involvement in emerging adults with type 1 diabetes. A sample of 79 emerging adults was recruited from a large pediatric diabetes clinic in the Mid-Atlantic. Inclusion criteria were emerging adults diagnosed with type 1 diabetes for at least 6 months, currently in the second half of their senior year of high school, with no other major chronic illnesses or psychiatric disorders, no pervasive developmental disorders or cognitive limitations, and who were fluent in reading and writing English. Recruitment letters were sent to 207 emerging adults who potentially met recruitment criteria. Forty-eight participants could not be contacted by phone; an additional 4 participants cancelled their clinic visit after the initial letter was sent and were not reached. Of the 155 participants contacted, 50 were not interested in participating and 17 participants were ineligible, resulting in 88 participants who expressed interest in participating. Of these, 9 did not complete consent and baseline questionnaires, resulting in a total of 79 participants who enrolled in the study and completed the baseline time point. Trained research personnel obtained informed consent from the parents, assent from the participating emerging adults, and answered any questions the participants had pertaining to the study. All participating emerging adults received modest incentives for study participation ($25 at baseline increasing to $30 at the 6 month follow up and $35 at the 12 month follow up). The Institutional Review Board at the study site approved the study.
To complete the study in its entirety, participants completed questionnaires at three consecutive clinic visits representing baseline, 6 month, and 12 month time points. 6 participants did not complete the 6 month questionnaires and 9 additional participants failed to complete the 12 month questionnaires, resulting in 64 participants who successfully completed this study at all 3 time points. Participants with complete data at each time point were more likely to be Caucasian and to attend a 4 year university than those who did not complete the study (p<.05). For the purposes of this secondary data analysis, only participants with complete data at each time point were included in the final sample.
Measures
Demographic Data
Following informed consent, demographic information on the participant's age, gender, race/ethnicity, insulin therapy type, family income level, and parent's marital status were collected.
Diabetes Self-Management
Diabetes self-management was measured with the SMOD-A. The SMOD-A is a 52 item self-report questionnaire which measures self-management activities, development, and goals (Schilling et al., 2009). It consists of 5 subscales that measure unique aspects of self-management: Collaboration with Parents (range 0 to 39), Diabetes Care Activities (range 0 to 45), Diabetes Problem Solving (range 0 to 21), Diabetes Communication (range 0 to 30), and Goals (range 0 to 21). The Collaboration with Parents subscale measures the frequency that parents are involved in their child's diabetes management. The Diabetes Care Activities subscale measures the frequency with which the emerging adult performs various activities which are essential to diabetes management. The Diabetes Problem Solving subscale assesses how frequently the emerging adult adjusts his/her regimen and knows his/her A1c numbers and goals. The Diabetes Communication subscale looks into how frequently the emerging adult communicates with his/her parents, healthcare providers, and friends about his/her health condition. Finally, the Goals subscale provides 7 potential diabetes goals and assesses the degree to which the emerging adult endorses or meets these goals. Higher scores are associated with better self-management behaviors (Schilling et al., 2009). In addition to the test-retest reliability of the SMOD-A, construct validity has been established with other measures of diabetes care and management in youth, including the Diabetes Self-Management Profile (Harris et al., 2000) and Self-Care Inventory (Lewin et al., 2009), in addition to A1c. Reliability estimates are adequate, with reliabilities of the subscales ranging from 0.62 to 0.80 (Schilling et al., 2009). Reliability estimates in the current sample were similarly fair to good: Collaboration with Parents (α=0.69), Diabetes Care Activities (α=0.78), Diabetes Problem Solving (α=0.77), Diabetes Communication (α=0.70), and Goals (α=0.60).
Clinical Data
Medical record data, including the duration of diabetes, age at diagnosis, A1c, average frequency of BG monitoring, and average BG level were extracted from medical charts from regularly scheduled clinic visits at the time of questionnaire completion. Average frequency of BG monitoring and mean BG level were calculated using 30 days of BG data for the month prior to the clinic visit; BG data were extracted from meter downloads or participant print-outs of meter data downloaded at home. If meters were unable to be downloaded, a trained research assistant reviewed the glucometer with the emerging adult to document the most recent 30 days of BG data.
Statistical Analysis
SPSS version 22 (SPSS Inc, Chicago, Illinois) was used for all statistical analyses. Descriptive statistics were calculated for all study variables to calculate frequencies, means, standard deviations, and range of values. One sample t tests were used to calculate differences between previously reported SMOD-A subscale means for emerging adults with type 1 diabetes with the current sample (Keough et al., 2011). Correlations were analyzed to identify associations between baseline SMOD-A mean values and measures of glycemic control, namely, A1c, frequency of BG monitoring, and mean blood glucose level at baseline and 12 month time points. Paired-samples t tests and one-way Analyses of Variance (ANOVAs) assessed for differences between SMOD-A subscale scores at baseline, 6 month, and the 12 month time points. Finally, a bivariate linear regression model was conducted to evaluate the association of baseline SMOD-A subscales in relation to glycemic control (A1c) at the 12 month time point to assess for potential subscales which can predict health outcomes at the 1 year mark. P values <0.05 were considered to be statistically significant.
Results
Sixty-four emerging adults with type 1 diabetes completed all three study time points; baseline demographic and clinical information is presented in Table 1. Participants were predominantly Caucasian, representing approximately equal numbers of males and females. All participants were between 17-19 years old and in the second half of their senior year of high school at baseline. Mean glycemic control was 8.00%, above the ADA guideline of an A1c < 7.5% for youth 18 and under. BG levels were monitored an average of 3.95 times per day, with an average blood glucose level of 179.52 mg/dL, and participants had been diagnosed with type 1 diabetes for an average of 6.65 years.
Table 1.
Demographic Characteristics (n=64).
| % | Mean | SD | Range | |
|---|---|---|---|---|
| Gender (% female) | 51.60 | |||
| Race (% Caucasian) | 75.00 | |||
| Plans post high school | ||||
| 4 year college | 67.20 | |||
| 2 year college | 26.60 | |||
| Employment | 6.30 | |||
| Living situation post-high school (% living away from home) | 70.30 | |||
| Parent Marital Status (% married) | 83.90 | |||
| Parent household income (>$100,000/year) | 64.50 | |||
| Insulin therapy | ||||
| Pump | 37.50 | |||
| Basal-bolus injections | 42.20 | |||
| 2-3 injections/day | 20.30 | |||
| Age (years) | 18.12 | 0.44 | 17.26-19.07 | |
| Disease Duration (years) | 6.65 | 4.37 | 0.72-17.30 | |
| A1c (%) | 8.00 | 1.25 | 6.00-12.30 | |
| BG monitoring frequency | 3.95 | 2.04 | 0.27-11.40 | |
| (checks/day) | ||||
| Average BG level (mg/dL) | 179.52 | 43.85 | 106-350 |
Baseline scores on the SMOD-A are presented in Table 2. The mean score on the Goals subscale differed significantly from values reported by Keough et al. in emerging adults ages 17-21, with the current sample endorsing a higher score (Keough et al., 2011). There were no other significant differences between the current sample's mean scores and previously reported values. SMOD-A subscale scores were not significantly different by participant sex, race, or living situation post-high school (home or away from home); SMOD-A subscale scores were also not significantly associated with participant age or disease duration. Participants with lower family income reported less diabetes problem-solving skills (p<.05). Additionally, SMOD-A scores varied by insulin regimen, with participants on conventional insulin regimens consisting of 2-3 injections/day reporting more collaboration with parents and less diabetes care activities, diabetes problem solving, diabetes communication, and goals as compared to patients on intensive insulin regimens (insulin pump or multiple daily injections; ps <.05).
Table 2.
SMOD-A Subscale Definitions, Means, and Standard Deviations.
| SMOD-A Subscale | Definition | Mean | SD | Range |
|---|---|---|---|---|
| Collaboration | How frequently parents are involved in diabetes | 9.45 | 4.72 | 2-23 |
| management | ||||
| Diabetes Care | How frequently the adolescent/emerging adult performs key activities of diabetes management | 30.36 | 6.38 | 8-42 |
| Diabetes Problem Solving | How frequently the adolescent/emerging adult adjusts regimen and knows A1C numbers and goals | 16.00 | 3.90 | 0-21 |
| Diabetes Communication | How frequently the adolescent/emerging adult communicates with parents, healthcare providers, and friends about their disease | 16.67 | 4.56 | 6-26 |
| Goals | The degree to which the adolescent/emerging adult has endorsed seven potential diabetes goals | 17.22 | 2.23 | 12-21 |
Over the 1 year period from high school graduation to post high-school, markers of glycemic control worsened. Average A1c levels increased from 8.00% at baseline to 8.50% at the 12 month follow-up. Average BG monitoring frequency decreased from 3.95 checks/day at baseline to 3.24 checks/day at the 12 month follow-up. Mean BG levels also increased from 179.52 mg/dL at baseline to 196.40 mg/dL at the 12 month follow-up. Correlation coefficients were computed between the five SMOD-A subscales at baseline and markers of glycemic control at the baseline and 12 month time points (Table 3).
Table 3.
Baseline SMOD-A correlation with A1c, Frequency of BG Monitoring, and Mean BG Level.
| Baseline | 12 month follow-up | |||||
|---|---|---|---|---|---|---|
| A1c | BG Frequency | Mean BG Level | A1c | BG Frequency | Mean BG Level | |
| Collaboration with Parents | 0.16 | -0.06 | 0.10 | 0.12 | -0.09 | 0.08 |
| Diabetes Care Activities | -0.42** | 0.46** | -0.36** | -0.21 | 0.45** | -0.32** |
| Diabetes Problem Solving | -0.11 | 0.20 | -0.12 | -0.26* | 0.17 | -0.18 |
| Diabetes Communication | -0.18 | 0.21 | -0.02 | -0.07 | 0.21 | -0.04 |
| Goals | -0.21 | 0.24 | -0.22 | -0.21 | 0.33** | -0.29* |
p<.05;
p<.01
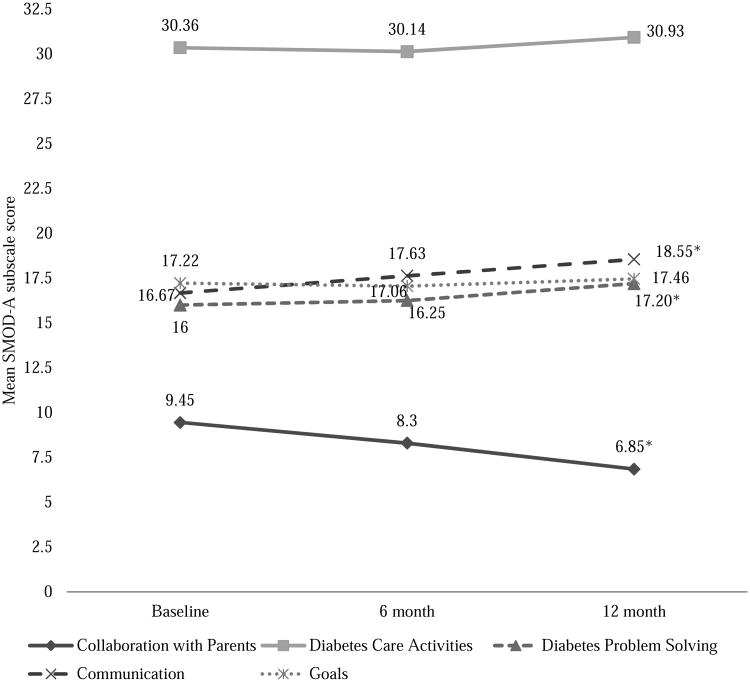
The 5 SMOD-A subscales changed with varying degree over the 1 year period (Figure 1). The mean score on the Collaboration with Parents subscale decreased from 9.45 at baseline to 6.85 at 12 month follow-up (p<0.05). A one-way ANOVA indicated a significant time effect (F(2, 62)= 13.81, p<0.01, η2=0.31). The mean score on the Diabetes Problem Solving subscale increased from 16.00 at baseline to 17.20 at the 12 month follow-up (F(2, 62)=5.71, p<0.05, η2=0.16). In addition, mean scores on the Diabetes Communication subscale increased from 16.67 to 18.55 at the 12-month follow-up (F(2, 61)= 3.94, p<0.05, η2=0.11). No significant changes were found on the Diabetes Care Activities and Goals subscales from baseline to 12 month follow-up.
Figure 1.
Mean SMOD-A Subscale Scores Across Time.
*p <0.05
A hierarchical multiple regression analysis was conducted to evaluate if SMOD-A subscales predicted glycemic control (A1c) at the 12 month follow-up. Demographic variables significantly associated with SMOD-A subscale scores were included in the model (i.e. family income, insulin regimen). Baseline A1c levels were also included in analyses to control for variability based on glycemic status alone. The linear combination of these factors was significantly related to A1C at the 12 month time point (F(4,54) = 15.91, p<.01; adjusted R2=.51). Results indicated that baseline A1c had the most significant predictive effect on A1c at 12 months (β = .68; p<0.01). After accounting for baseline A1c, family income, and regimen, the Diabetes Problem Solving subscale significantly predicted A1c at 12 months (β = -.25; p<0.05).
Discussion
Study results find changes in diabetes self-management occur in emerging adults with type 1 diabetes as they transition from high school to college or employment post-graduation, with collaboration with parents decreasing and diabetes problem solving and communication with health care providers increasing. Findings also demonstrate the utility of the SMOD-A for measuring self-management skills in emerging adults. While other studies have used the SMOD-A in cross-sectional studies (Keough et al., 2011; Schilling et al., 2009), this study is one of the first to our knowledge that applies the measure longitudinally with the same group of participants. Emerging adults are a group at risk to loss of follow up, given their changes in living situation and/or medical care setting, making them a difficult group to study and fully characterize (Peters et al., 2011). These factors make the results found through this study particularly impactful, allowing for detection of changes in self-management of diabetes in the context of potential transitions in education or living situation.
Changes in the various subscales were evident over the post-high school transition, with the biggest decrease seen in Collaboration with Parents and increases seen in Diabetes Problem Solving and Diabetes Communication. These findings corroborate well with previous studies, demonstrating that as emerging adults gradually accrue independence from the home environment, they rely less on parental supervision, feel more equipped to troubleshoot issues related to diabetes on their own, and are more comfortable communicating with peers, healthcare providers, and parents about their diabetes (Hanna et al., 2013; Schilling et al., 2009; Schilling et al., 2006). The lack of significant change on the Diabetes Care Activities subscale was not surprising. This subscale consistently received the highest score at all 3 time points, and it is most likely that these technical skills (e.g. checking BG levels before meals, re-checking BG levels if high) are some of the first that youth master once diagnosed with diabetes. Additionally, the lack of difference on the Goals subscale implies that while emerging adults experience multiple changes after high school, their goals and motivation for diabetes management remain relatively constant. It is also possible that this did not change because emerging adults have not yet prioritized long term goals in light of all the immediate transitions they are experiencing. In general, youth on conventional insulin regimens consisting of a fixed number of insulin injections per day reported more collaboration with parents and less diabetes care activities, problem solving, and communication, and fewer diabetes-related goals. This may be, in part, due to the inflexibility of the regimen, as youth on conventional regimens may not have the same opportunity to adjust insulin doses in response to changes in diet, activity, or BG levels.
Among the subscales, the Diabetes Care Activities subscale had the strongest correlations with markers of glycemic control at both the baseline and 12 month time points. This was expected, as the subscale assesses adherence to the diabetes regimen, and is therefore closely related to BG monitoring frequency and mean BG levels. The Diabetes Problem Solving subscale correlated significantly with A1c at the 12 month time point, and was the only subscale which significantly contributed to A1c at 12 months in regression analyses. These findings indicate that as emerging adults begin mastering more nuanced skills of diabetes care (e.g. knowing goal A1c values, adjusting insulin based on BG levels), long term glycemic control is improved. Recent studies recognize the importance that problem solving skills play in glycemic control (Hill-Briggs et al., 2006; Mulvaney et al., 2014), and interventions promoting problem solving skills in adults with diabetes have been successful in improving glycemic control (Hill-Briggs et al., 2006). Our findings suggest problem solving skills may be critical to managing the unpredictability often present in the daily lives of emerging adults, and promoting problem solving skills in adolescents may help to protect against the worsening glycemic control seen during this developmental period.
Limitations and Future Directions
This study had several limitations. First, the attrition rate of the study was about 19%, given that data needed to be collected at all 3 time points and be complete in regards to the SMOD-A. Therefore, this study may underrepresent youth with more risk factors or who are in poorer control. Second, the demographics of the sample included a majority of Caucasian participants from families of high socioeconomic status, which limits the generalizability of the findings. Participants also predominantly enrolled in higher education after high school, and youth who entered into full-time employment post-high school made up a small minority of the sample. Third, although the study was designed to capture a transitional period from high school to post-high school, the study time frame of 1 year was relatively short. Finally, the effect sizes found in this study were modest. Future research should confirm these findings in a more diverse sample of emerging adults with type 1 diabetes with a wider range of income levels, racial diversity, and post-high school trajectories over a longer period of time.
Clinical Implications
These findings, taken together, can inform the role that healthcare providers have in supporting emerging adults with type 1 diabetes during this transition period. It is important to normalize changes in diabetes responsibility for both parents and emerging adults and to not only encourage the emerging adult to take on more responsibility as appropriate, but also to prepare them with the skills necessary to make this transition seamless. The SMOD-A may be a useful tool for healthcare providers and understanding self-management patterns may guide effective strategies targeted toward these areas of self-management in an effort to prepare their patients for this transition period post-high school. For example, there are a number of university-based supports for diabetes care (e.g. College Diabetes Network chapters, on-campus health services) and pediatric healthcare providers can develop partnerships and resources to familiarize their patients with these services before college entrance. Targeted education and workshops for emerging adult patients may also encourage key self-management skills during this transitional period (Sequeira et al., 2015). Specifically, encouraging patient engagement in active problem solving around diabetes management may enhance the ability to proactively and confidently adapt diabetes care routines to changing routines and schedules evident in emerging adulthood. The advance of technology can aid in this domain. There are a number of diabetes-related smartphone apps that can assist with tracking and prompting self-management behaviors (Eng & Lee, 2013). In addition, the growing use of electronic health records allows for more frequent, dynamic communication with healthcare providers (Corathers et al, 2015). Such strategies can maintain or improve glycemic control, and help emerging adults and their families prepare for the post-high school transition.
Conclusion
Emerging adults with type 1 diabetes are at risk for poor glycemic control, as evidenced by increased A1c and mean BG level and decreased BG monitoring frequency over the first year post-high school. Study results suggest that emerging adults are assuming increased responsibility for diabetes management and are more willing to discuss problems related to their diabetes. However, they are also adjusting to new schedules and may struggle with incorporating diabetes management strategies into daily routines, resulting in transition from high school to post-high school being a time of worsening glycemic control. It is important that pediatric health care providers promote appropriate developmental responsibility for diabetes care and partner with emerging adults to promote skills essential to good diabetes management, including diabetes-related problem solving and good communication with health care providers.
Acknowledgments
Dr. Monaghan is currently funded by the National Institutes of Health (PI: Monaghan; NIH K23DK099250). This publication was supported by Award Numbers UL1TR000075 and KL2TR000076 from the NIH National Center for Advancing Translational Sciences. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Center for Advancing Translational Sciences or the National Institutes of Health.
Footnotes
Disclosures: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Diabetes Association. Standards of Medical Care in Diabetes - 2015. Diabetes Care. 2015;38(S1):S1–S93. doi: 10.2337/dc15-S001. [DOI] [Google Scholar]
- Arnett J. Emerging adulthood:A theory of development from late teens through the twenties. American Psychologist. 2000;55(5):469–480. doi: 10.1037//0003-066X.55.5.469. [DOI] [PubMed] [Google Scholar]
- Bryden K, Dunger D, Mayou R, Peveler R, Neil H. Poor prognosis of young adults with type 1 diabetes: A longitudinal study. Diabetes Care. 2003;26(4):1052–1057. doi: 10.2337/diacare.26.4.1052. [DOI] [PubMed] [Google Scholar]
- Bryden K, Peveler R, Stein A, Neil H, Mayou R, Dunger D. Clinical and psychological course of diabetes from adolescence to young adulthood: a longitudinal cohort study. Diabetes Care. 2001;24(9):1536–1540. doi: 10.2337/diacare.24.9.1536. [DOI] [PubMed] [Google Scholar]
- Chao A, Whittemore R, Minges K, Murphy K, Grey M. Self-management in early adolescence and differences by age at diagnosis and duration of type 1 diabetes. The Diabetes Educator. 2014;40(2):167–177. doi: 10.1177/0145721713520567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiang JL, Kirkman MS, Laffel LMB, Peters AL. Type 1 Diabetes through the life span: A position statement of the American Diabetes Association. Diabetes Care. 2014;37(7):2034–2054. doi: 10.2337/dc14-1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corathers SD, Schoettker PJ, Clements MA, List BA, Mullen D, et al. Lee J. Health-system-based interventions to improve care in pediatric and adolescent type 1 diabetes. Current Diabetes Reports. 2015;15:91. doi: 10.1007/sl1892-015-0664-8. [DOI] [PubMed] [Google Scholar]
- Eng DS, Lee JM. The promise and peril of mobile health applications for diabetes and endocrinology. Pediatric Diabetes. 2013;14(4):231–238. doi: 10.1111/pedi.12034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garvey KC, Markowitz JT, Laffel LM. Transition to adult care for youth with type 1 diabetes. Current Diabetes Reports. 2012;12(5):533–541. doi: 10.1007/s11892-012-0311-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanna KM, Weaver MT, Stump TE, Dimeglio LA, Miller AR, Crowder S, Fortenberry JD. Initial findings: Primary diabetes care responsibility among emerging adults with type 1 diabetes post high school and move out of parental home. Child: Care, Health, & Development. 2013;39(1):61–68. doi: 10.1111/j.1365-2214.2011.01320.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris M, Wysocki T, Sadler M, Wilkinson K, Harvey L, Buckloh L, et al. White N. Validation of a structured interview for the assessment of diabetes self-management. Diabetes Care. 2000;23(9):1301–1304. doi: 10.2337/diacare.23.9.1301. [DOI] [PubMed] [Google Scholar]
- Hill-Briggs F, Gary TL, Yeh H, Batts-Turner M, Powe NR, Saudek CD, Brancati FL. Association of social problem solving with glycemic control in a sample of urban African Americans with type 2 diabetes. Journal of Behavioral Medicine. 2006;29(1):69–78. doi: 10.1007/s10865-005-9037-0. [DOI] [PubMed] [Google Scholar]
- Keough L, Sullivan-Bolyai S, Crawford S, Schilling L, Dixon J. Self-management of type 1 diabetes across adolescence. The Diabetes Educator. 2011;37(4):486–500. doi: 10.1177/0145721711406140. [DOI] [PubMed] [Google Scholar]
- Lewin A, LaGreca A, Geffken G, Williams L, Duke D, Storch E, Silverstein J. Validity and reliability of an adolescent and parent rating scale of type 1 diabetes adherence behaviors: The Self-Care Inventory (SCI) Journal of Pediatric Psychology. 2009;34(9):999–1007. doi: 10.1093/jpepsy/jsp032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulvaney S, Jaser S, Rothman R, Russell W, Pittel E, Lybarger C, Wallston K. Development and validation of the diabetes adolescent problem solving questionnaire. Patient Education and Counseling. 2014;97(1):96–100. doi: 10.1016/j.pec.2014.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson M, Story M, Larson N, Neumark-Sztainer D, Lytle L. Emerging adulthood and college-aged youth: An overlooked age for weight-related behavior change. Obesity. 2008;16(10):2205–2211. doi: 10.1038/oby.2008.365. [DOI] [PubMed] [Google Scholar]
- Peters A, Laffel L American Diabetes Association Transitions Working Group. Diabetes care for emerging adults: recommendations for transition from pediatric to adult diabetes care systems: a position statement of the American Diabetes Association, with representation by the American College of Osteopathic Family Physicians, the American Academy of Pediatrics, the American Association of Clinical Endocrinologists, the American Osteopathic Association, the Centers for Disease Control and Prevention, Children with Diabetes, The Endocrine Society, the International Society for Pediatric and Adolescent Diabetes, Juvenile Diabetes Research Foundation International, the National Diabetes Education Program, and the Pediatric Endocrine Society (formerly Lawson Wilkins Pediatric Endocrine Society) Diabetes Care. 2011;34(11):2477–2485. doi: 10.2337/dc11-1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettitt D, Talton J, Dabelea D, Divers J, Imperatore G, Lawrence J, et al. for the SEARCH for Diabetes in Youth Study Group. Prevalence of diabetes in U.S. youth in 2009: The SEARCH for Diabetes in Youth Study. Diabetes Care. 2014;37(2):402–408. doi: 10.2337/dc13-1838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schilling L, Dixon J, Knafl K, Grey M, Ives B, Lynn M. Determining content validity of a self-report instrument for adolescents using a heterogeneous expert panel. Nursing Research. 2007;56(5):361–366. doi: 10.1097/01.NNR.0000289505.30037.91. [DOI] [PubMed] [Google Scholar]
- Schilling L, Dixon J, Knafl K, Lynn M, Murphy K, Dumser S, Grey M. A new self-report measure of self-management of type 1 diabetes for adolescents. Nursing Research. 2009;58(4):228–236. doi: 10.1097/NNR.0b013e3181ac142a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schilling L, Knafl K, Grey M. Changing patterns of self-management in youth with type 1 diabetes. Journal of Pediatric Nursing. 2006;21(6):412–424. doi: 10.1016/j.pedn.2006.01.034. [DOI] [PubMed] [Google Scholar]
- Schulenberg J, Sameroff A, Cicchetti D. The transition to adulthood as a critical juncture in the course of psychopathology and mental health. Development and Psychopathology. 2004;4:799–806. doi: 10.1017/S0954579404040015. [DOI] [PubMed] [Google Scholar]
- Sequeira PA, Pyatak EA, Weigensberg MJ, Vigen CP, Wood JR, et al. Peters AL. Let's Empower and Prepare (LEAP): Evaluation of a structured transition program for young adults with type 1 diabetes. Diabetes Care. 2015;38(8):1412–1419. doi: 10.2337/dc14-2577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whittemore R, Liberti L, Jeon S, Chao A, Jaser S, Grey M. Self-management as a mediator of family functioning and depressive symptoms with health outcomes in youth with type 1 diabetes. Western Journal of Nursing Research. 2014;36(9):1254–1271. doi: 10.1177/0193945913516546. [DOI] [PMC free article] [PubMed] [Google Scholar]