OVERVIEW
In response to the increased volume of injured geriatric patients presenting to trauma centers, the American Association for Surgery of Trauma (AAST) established the Ad Hoc Geriatric Trauma Committee. The Committee was tasked to survey the membership of the AAST to understand the current conditions under which geriatric trauma patients (GTPs) are receiving care, to identify the major problems associated with providing that care, and to suggest potential solutions. Concurrent to the survey, the Committee also reviewed the current literature on geriatric trauma care and developed a consensus on the problems and potential solutions.
INTRODUCTION
In the 2010 US Census, the number of persons age 65 years and older constituted 13% of the population and is projected to constitute 22% of the population by 2020.1 As the US population ages, there is an increasing volume of GTPs; injury is now the seventh leading cause of death for those age 65 years.2 Geriatric trauma is increasing both in absolute number and as a proportion of annual volume presenting to trauma centers. Based on the National Trauma Data Bank, the proportion of trauma patients aged 65 years or older in Level I and II trauma centers increased from 23% in 2003 to 30% in 2009. This is likely a significant underestimate because most GTPs are treated at lower-level or nontrauma centers.3,4 In Washington State, for example, the annual number of GTPs in the state registry has increased from 4,266 in 2000 to 11,226 in 2012, an increase from 30% to 42% of the total trauma population. Clearly, the management of injury in geriatric patients will continue to be a major challenge for trauma care providers.
In his presidential address to the AAST entitled “For the care of the undeserved,” Dr. Robert Mackersie identified the growing population of elderly injured patients as medically underserved in terms of limited trauma center access, age-related treatment biases, and as a result, deprived of many of the recent advances in modern trauma care.5 To specifically address these inequalities, he convened an Ad Hoc Geriatric Committee and charged it, “To advise the AAST regarding the problems, issues, and needs of the geriatric patient.” What follows is the work product of the Committee in responding to President Mackersie’s charge. The initial priority was to survey the membership of the AAST to better understand the current conditions under which hospitalized GTPs are receiving care. The second task of the Committee was to enumerate the major problems associated with the care of GTPs and to suggest potential solutions to the identified problems. While the Committee does not presume infallibility in its pronouncements, the material presented is intended to initiate discussion, stimulate research, and to ultimately result in evidence-based guidelines that will better serve this “underserved” segment of our population.
MEMBER SURVEY
Two distinct surveys were distributed to the membership of the AAST on two separate occasions. Responses to the surveys were solicited via e-mail, two e-mails for each survey. Responses were entirely voluntary, and respondents were asked to respond to each survey only once. Surveys were distributed in an electronic format using SurveyMonkey (SurveyMonkey, Inc., Palo Alto, CA). All responses were completely blinded, and no unique respondent identifiers were solicited. Results of the two surveys were collated and tabulated separately.
In addition to basic demographic questions designed to characterize respondents, the first survey (Survey 1) consisted of 12 additional questions. The first survey was designed to achieve the following:
Garner expert consensus on an appropriate definition of geriatric trauma
Evaluate knowledge of current epidemiology of geriatric trauma care
Evaluate how frequently geriatric specific resources are currently used
Identify areas of specific clinical interest in the management of GTPs.
The second survey (Survey 2) was distributed 2 months later and focused on identifying strategies for geriatric care with respect to who provides care to a variety of GTPs and identifying research priorities.
One hundred forty-three completed surveys were obtained for Survey 1, and 99 respondents completed Survey 2. The majority of respondents were aged 41 years to 60 years, with one quarter of respondents older than 60 years (Table 1). Most respondents were male, worked at large urban academic level 1 or 2 trauma centers, and self-identified their primary area of specialty as trauma surgery, critical care, emergency surgery, and/or general surgery. These demographic profiles are similar to other published studies of surveys of the AAST membership.6
TABLE 1.
Demographics of Respondents
| Respondents | Survey 1 | Survey 2 | |
|---|---|---|---|
| N | 143 | 99 | |
| Age | |||
| ≤30 | 0.0% | 0.0% | |
| 31–40 | 5.6% | 3.0% | |
| 41–50 | 35.0% | 27.3% | |
| 51–60 | 35.0% | 39.4% | |
| 61–70 | 21.0% | 23.2% | |
| G70 | 3.5% | 7.1% | |
| Sex | |||
| Male | 85.3% | 84.7% | |
| Female | 14.7% | 15.3% | |
| Facility location | |||
| Urban | 76.2% | 79.4% | |
| Rural | 6.3% | 5.2% | |
| Suburban | 14.5% | 16.5% | |
| Military | 0.0% | 0.0% | |
| American College of Surgeons or state level verification | |||
| Level I or II | 95.1% | 98.0% | |
| Level III–V | 2.1% | 0.0% | |
| Nonverified trauma center | 0.7% | 0.0% | |
| Nontrauma center | 2.1% | 2.0% | |
| Size of facility | |||
| ≤200 beds | 3.5% | 2.0% | |
| 201–400 beds | 26.6% | 29.6% | |
| 401–600 beds | 34.3% | 32.7% | |
| <600 beds | 35.7% | 35.7% | |
| Primary area of specialty (all that apply) | |||
| Trauma surgery | 91.5% | 92.6% | |
| Critical care | 83.7% | 73.7% | |
| Emergency surgery | 59.6% | 57.9% | |
| General surgery | 54.6% | 56.8% | |
| Pediatric surgery | 2.8% | 2.1% | |
| Emergency medicine | 1.4% | 1.1% | |
| Orthopedics | 0.0% | 1.1% | |
| Neurosurgery | 0.0% | 1.1% | |
| Type of practice | |||
| University based | 72.7% | 72.2% | |
| Non–university based with residents | 17.3% | 13.4% | |
| Non–university based without residents | 10.1% | 14.4% | |
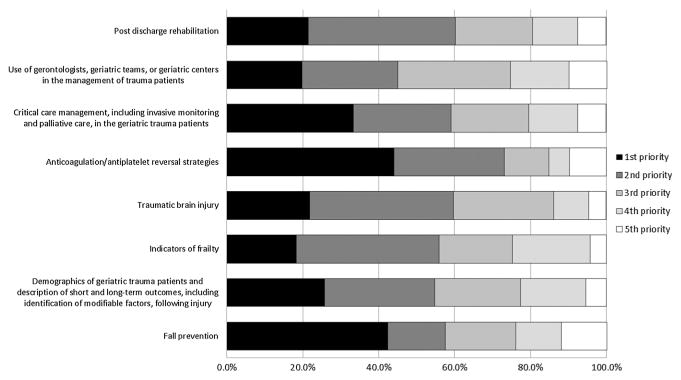
When asked about the best definition of the GTP, 42% felt that an age cutoff should be used to define geriatric, while 11% preferred a disease- and/or injury-specific cutoff. The majority (61%) felt that both age and comorbidities should be considered when defining geriatric trauma. More than 40% of the respondents felt that age of greater than 65 years was the most appropriate definition, while just more than 30% favored a definition of age greater than 55 years with major comorbidities and age greater than 65 years without major comorbidities (Fig. 1).
Figure 1.
Responses to “Which of the following do you feel is the best definition of ‘geriatric trauma’?” Respondents could only select one answer.
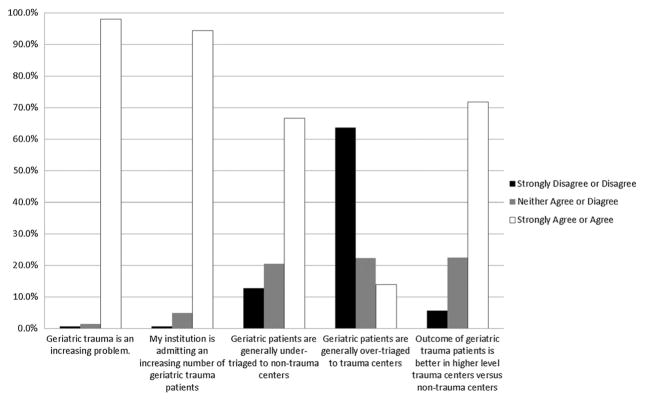
There was strong consensus among respondents with respect to the volume, triage, and outcome of geriatric trauma (Fig. 2), which was based on general impression (25%), actual data from the respondent’s institution or literature (16%), and a combination general impression and the literature (60%).
Figure 2.
Responses to “Please state how strongly you agree or disagree with the following statements.” Respondents could select strongly disagree, disagree, neither agree nor disagree, agree, or strongly agree.
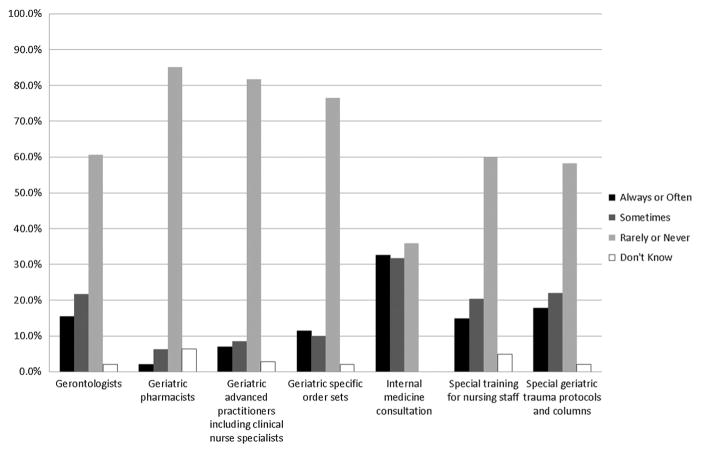
Gerontologists, geriatric pharmacists, geriatric advanced practitioners, or geriatric specific order sets are rarely used at respondent institutions (Fig. 3). There was also relatively strong consensus on the areas of specific clinical interest in the management of GTPs (Fig. 4).
Figure 3.
Responses to “Please state how frequently your institution uses the following resources for geriatric trauma patients.” Respondents could select always, often, sometimes, rarely, never, or do not know.
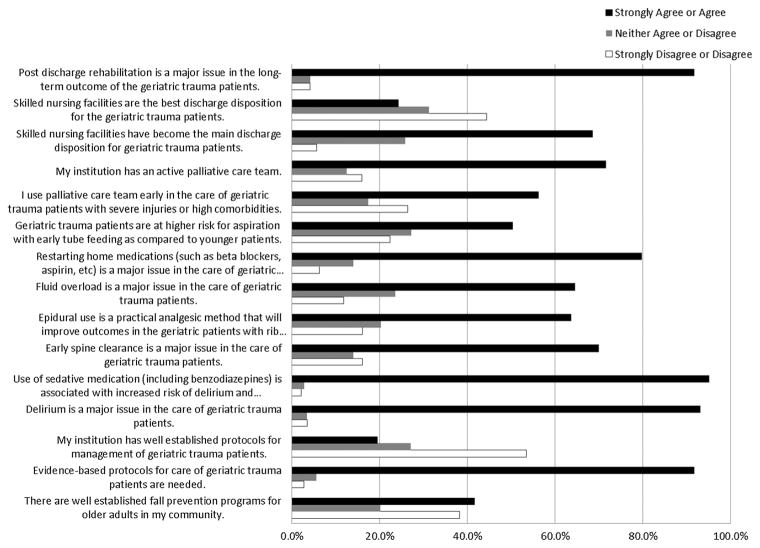
Figure 4.
Responses to “Please state how strongly you agree or disagree with the following statements.” Respondents could select strongly disagree, disagree, neither agree nor disagree, agree, or strongly agree.
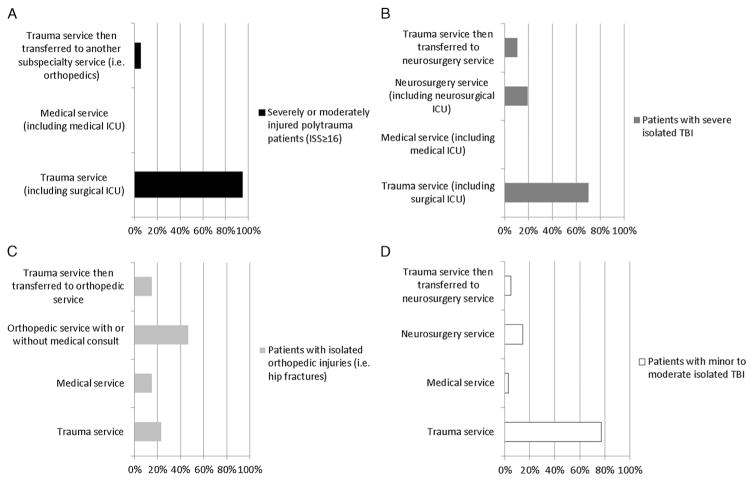
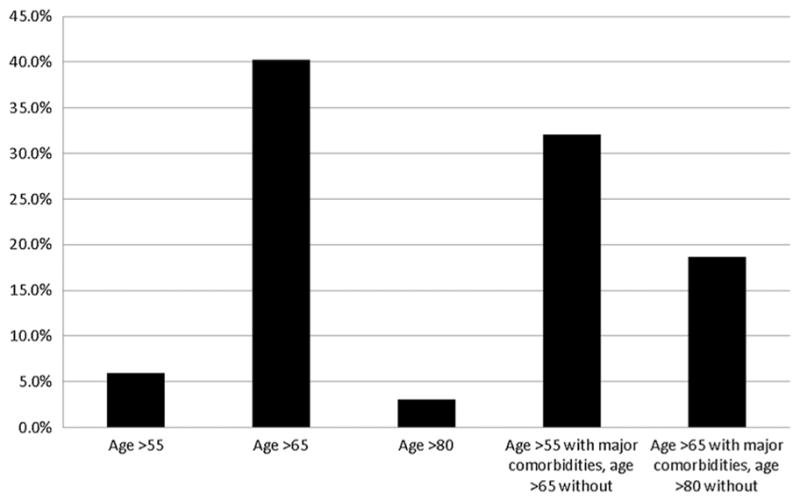
Responses to Survey 2 demonstrated a surprising amount of homogeneity in the primary service providing care for moderately to severely injured geriatric patients and GTPs with traumatic brain injury, but there was significant heterogeneity in who provided care for GTPs with isolated orthopedic injuries (Fig. 5)A–D. Research priorities for the respondents included fall prevention and strategies for the reversal of anticoagulants and antiplatelet agents (Fig. 6).
Figure 5.
Responses to “To which service do the following geriatric patients most frequently get admitted in your trauma center?” A. Severely or moderately injured polytrauma patients (ISS ≥ 16). B. Patients with isolated orthopedic injuries (i.e., hip fractures). C. Patients with severe isolated traumatic brain injury. D. Patients with minor-to-moderate isolated traumatic brain injury. Respondents could only select one answer for each.
Figure 6.
Responses to “Please rate the following with respect to which you believe are the greatest research priorities for geriatric trauma from 1 to 5, 1 being the most important and 5 being the least important.”
The survey clearly indicated that geriatric trauma is a significant and growing concern among trauma surgeons. Most survey participants believed that their institution was admitting an increasing number of GTPs. A troublesome question for the respondents was defining who qualified as a GTP; most favored a combination of age, comorbidities, and frailty as a more comprehensive definition. However, the traditional definition of 65 and older was the most frequently selected option, perhaps recognizing that a determination of frailty involves a complicated and cumbersome assessment.
Respondents believe that there is significant undertriage of GTPs to lower-level trauma centers or to nontrauma centers. They also believe that the outcome of GTPs is better in higher-level trauma centers than in lower-level or nontrauma centers.
The survey indicated that there are gaps in the development and implementation of treatment protocols for GTPs. While the care of injured children is based on well-defined protocols and dedicated services, there are few such guidelines or recommendations for the care of GTPs.7 Less than 20% of responders had specific geriatric protocols or order sets. Even fewer centers use geriatric advance practitioners or specially trained nurses. This void in protocol use was brought into sharp relief when the survey specifically asked about established geriatric trauma protocols (Fig. 4). More than 90% stated that there is a need for evidence-based management protocols for GTPs. The lack of nationally accepted guidelines is evident in the management of GTPs with extremity fractures; survey participants admitted these patients to orthopedics, trauma, or internal medicine, depending on the institution (Fig. 5).
Almost all responders stated that postdischarge rehabilitation is a major issue affecting the long-term outcome of GTPs. Almost 70% of responders stated that skilled nursing facilities (SNFs) have become the main discharge disposition for GTPs. However, when asked if SNFs are the best discharge disposition, most responders disagreed or strongly disagreed. Because there is a dearth of information addressing outcomes of trauma patients discharged to SNFs, 60% of responders considered postdischarge rehabilitation as the highest research priority.
The AAST survey indicated that more than 90% of the responders consider delirium a major issue in geriatric trauma. The responders consider use of sedatives, including benzodiazepines, as a major risk factor for delirium, which is also supported by the literature.8
One area of consensus was the increasing use of the palliative care team. The majority of survey participants (approximately 70%) have an active palliative care team in their institution. Moreover, most (<50%) use the palliative care team early in treatment of GTPs.
The survey participants identified the reversal of anticoagulants and antiplatelet agents and prevention of falls as the highest research priorities. As the US population is getting older, falls have become the number one mechanism of injury and mortality caused by injury. Moreover, with the changing demographic of the trauma population, chronic oral anticoagulant therapy is used with increasing frequency.9
In summary, this survey of AAST participants showed a significant concern regarding the increasing number of elderly injured patients, lack of uniformly accepted protocols, and the prehospital, hospital, and posthospital management of these patients.
Problems in Geriatric Trauma Care
Definition of the GTP
Published reports on the care of the elderly are inconsistent in the age definition of what constitutes the GTP. This lack of clarity introduces a problem with generalizing the findings of such studies. The most commonly used age is 65 years and older, and we propose that as defining the age descriptor. This is reasonable given its compatibility with the age descriptor used by the Centers for Medicare and Medicaid Services and is consistent with our survey respondents.
There is also a problem with delineating what constitutes trauma, particularly as related to ground-level and nonmechanical falls and the resultant injury, such as a hip fracture. Hip fractures are included in some reports and not in others, which obfuscates the reporting of complications and mortality in the GTP.10–12
Factors Leading to Poor Outcomes in the GTP
It has been repeatedly demonstrated that GTPs have outcomes worse than those of younger trauma patients.10,13,14 Care of GTPs is also more resource intensive than caring for younger patients with similar injuries.15,16 The cause of this difference is multifactorial and includes comorbid medical conditions, medications, and frailty, all of which affect the physiologic response to injury and can complicate treatment and recovery. Frailty, an indicator of senescence, is clinically distinct from age, comorbidity, and disability. The frailty syndrome is broadly considered as decreased physiologic reserve across multiple organ systems leading to an impaired ability to withstand physiologic stress.17 The prevalence of frailty in the GTP is high,18,19 and understanding it is relevant for trauma surgeons because frailty is associated with injury following falls.20 Recent data show that frailty may be more predictive of adverse outcomes than age alone in trauma patients.21
There are multiple models for measuring frailty, and there is no consensus on which is best to use across all clinical settings.22 Two popular models are the deficit accumulation model,23 which considers frailty as a reflection of health deficits across several domains (disabilities, comorbidities, symptoms, signs, and laboratory data) and the Fried Frailty Phenotype,18 which is based on the concept of energy depletion as a predictor of outcomes. These models lack feasibility in the GTP because they require assessment of up to 30 to 70 variables, many of which (i.e., gait speed and hand grip strength) cannot be performed on the GTP.
Limitations of current frailty measures have prompted some investigators to use functional status and sarcopenia as surrogate measures of frailty. Sarcopenia is the progressive loss of skeletal muscle mass and strength. The Vulnerable Elders Survey 13 (VES-13) is a validated screening tool to identify functional decline and has been shown to predict hospital complications and death in older trauma patients.24 GTPs frequently experience age-related sarcopenia and, with trauma-induced catabolism, are extremely susceptible to loss of lean body mass.25 Computed tomography (CT) is being used as a noninvasive method for measuring muscle mass and changes in body composition over time. Moisey et al.26 have shown that 71% of injured elderly patients admitted to the intensive care unit were sarcopenic and that sarcopenia was associated with fewer ventilator-free days. Sarcopenia also increases the need for posthospital medical care and rehabilitation. As a result, GTPs are less likely to go home after discharge and are less likely to meet the criteria for admission to an inpatient rehabilitation facility.27–29 Currently, trauma centers have responded to this growing demand by substantially increasing discharge to SNF, which is one of the most important independent predictors of poor long-term outcomes.10,30
Falls
Falls are the leading cause of injury and deaths caused by injury in GTPs. One of three adults 65 years and older falls annually. The cost of falls in 2012 was estimated to total 30 billion dollars.31 Falls are the most common cause of traumatic brain injury in the elderly. Factors that influence gait and reaction times (such as sarcopenia, arthritis, osteoporosis, and altered sensory input) predispose the elderly to falls. Osteoporosis and the tendency to fall increase the risk for hip fractures, which is the most frequent injury in elderly patients. While there is a debate about who should care for hip fracture patients, outcomes are superior when they are managed by a specialized multidisciplinary team with a protocol that promotes early operative intervention (even the day of injury but not later than 48 hours), early ambulation, and daily physical therapy.32 Environmental factors and medications also contribute to falls. Interventions have included nutritional supplements, vision correction, exercise, physical therapy, and environmental modification.31 Reliable data on the efficacy of these preventive strategies, either alone or in the aggregate, are lacking.
Motor Vehicle Collisions
Drivers age 65 and over and the number of older drivers involved in fatal motor vehicle collision (MVC) is increasing.33 Even at lower speeds, the elderly are significantly more likely to experience a serious injury.34 In certain driving environments such as intersections, the elderly, especially those 70 years and older, are more likely to contribute to a crash.35 Hearing and vision impairment as well as decreased reaction time and cognitive dysfunction can all play a role in crashes.
Interventions used for falls, such as vision and hearing testing, exercise, and medication review, can also be used to prevent injury from MVC. Seat belt use, extra following distance, and trip planning to avoid challenging driving conditions are recommended by the Centers for Disease Control (CDC) and National Highway Traffic Safety Administration.36 Health care providers should screen for sensory and cognitive impairment and inquire about medications that could impair driving.37 Trauma professionals should review licensing requirements for elders and discuss these with GTPs injured in MVC.38
Pedestrian Injuries
Approximately 1 in 5 pedestrians killed and 1 in 10 pedestrians injured is an elder.39 This is especially problematic in urban areas. In New York City, for example, those 65 years and older constitute one third of the pedestrian deaths.40 Factors that contribute to falls and MVCs also contribute to pedestrian injury. Environments, such as road width and time to cross intersections, also influence injury in the elderly. Recommendations to prevent or reduce pedestrian injury in the elderly include footwear and assistive devices while walking, walking with others, and using visual and hearing assist devices as well as changes in the environment at intersections, such as increasing crossing times and reducing distances at crosswalks, adding auditory signals to the visual for crosswalk indicators, and modifying curbs and walkways.41
Suicide
Depression is more frequent in the elderly than in the general population.42 Elders that commit suicide make fewer attempts per completed suicide, are usually socially isolated, and are more often divorced or widowed.43 Depression or other mental disorders, stressful life events, access to guns, previous imprisonment, and media exposure to suicidal actions are risk factors.44 A high index of suspicion combined with screening for depression is the first steps in prevention.
Elder Abuse
The CDC defines elder abuse as “... any abuse and neglect of persons age 60 and older by a caregiver or another person in a relationship involving an expectation of trust.”45 In 2010, 1 in 10 people older than 60 years experienced some form of mistreatment.46 The CDC reported that more than 500,000 older adults are believed to be abused or neglected each year.47 Elder abuse includes physical, sexual, emotional, or psychological as well as financial exploitation, neglect, and abandonment. An estimated four of five cases are not reported because of shame, ignorance of rights, self-blame, and fear of a loss of independence. Abuse can occur in institutions; almost one third of elders in an assisted living or nursing home experienced abuse.48 Measures to reduce or prevent elder abuse must begin with mandatory reporting. Practitioners must be educated in the signs of abuse and the methodology for reporting such events. Tools and resources are available to assist them in these efforts.49
Who Should Care for the Injured Elderly?
Triage, Trauma Activation, and Trauma Center Care
The excess mortality of the GTP, even with minor injuries, would seem to justify triage to trauma centers and trauma team activation. However, undertriage of GTPs is common. In New Jersey, for example, a study performed in three counties demonstrated an 18% undertriage of elderly men and 15% of elderly women.50 Multiple studies indicate that prehospital providers adhere to the physiologic, anatomic, and mechanistic parameters set forth in the CDC field triage guidelines.51 However, contrary to the guidelines, older age was associated with transport to the lower level of trauma care.3,52,53 Furthermore, older age was associated with not being transferred to the higher level of trauma care.3 Importantly, undertriage of GTPs increases mortality.52
Triage to a trauma center is associated with decreased mortality compared with nontrauma center care; the benefit seems to increase with age.54–56 The volume of GTPs treated at a trauma center is linked to improved outcome. In Pennsylvania, a larger volume of GTPs was significantly associated with lower in-hospital mortality, major complications, and failure to prevent a clinically important deterioration, such as death or permanent disability.57 However, not all studies support this notion. One prospective study by MacKenzie et al.58 who examined the effect of trauma center care on mortality demonstrated that there was a significant reduction in mortality in younger patients treated at trauma centers. Although the risk of death among GTP was lower, there was no significant difference in mortality. The authors of this study acknowledge that the small number of older patients with severe injuries resulted in large confidence intervals.
Specific physiologic triage criteria that are valid in younger patients may not be valid in GTPs. For example, a systolic blood pressure of 90 mm Hg or less in younger patients may be too low for the GTP, and there are data to support raising it to as high as 120.59
Interdisciplinary Care
A team approach (geriatricians, social workers, pharmacists, nursing, etc.) to the care of the hospitalized elderly patient has been shown in the geriatric literature to work best. Interdisciplinary care improves quality because it addresses the associated comorbidities, improves processes and outcomes for geriatric syndromes, and provides value for the health care system.60,61 Geriatric consultation improves trauma care by identifying additional diagnoses not found by the trauma service, assisting with advanced care planning, managing medication changes, improving pain management, decreasing length of stay, and reducing discharges to long-term care.62–64 Geriatric nursing, using an acute care elderly unit model, has also improved care.65 Acute care elderly units incorporate a patient-centered, homelike environment that includes plans for preventing disability and iatrogenic illness as well as providing comprehensive discharge planning and management.
Leadership of the multidisciplinary team should be vested in the trauma surgeon who is best equipped to perform the initial trauma evaluation and to guide management. The severity of injury in the GTP population may vary significantly by trauma center, and therefore, the number of GTPs evaluated will not be uniform. However, we propose that any significantly injured patient should be admitted by the trauma surgeon with appropriate consultation and multidisciplinary input.
Geriatrician Workforce
The sheer volume of GTPs demands that others caring for them, including trauma surgeons, become familiar with their special needs and requirements to provide optimal care. Geriatricians account for only a very small portion of the total physician workforce. There is only one geriatrician for every 2,546 older Americans.66 By 2030, one estimate shows that this number will decrease to only one for every 4,254 older Americans, far short of the total predicted need.66 Some argue that there could be a net decrease in geriatricians because of the decreasing number of physicians entering training programs and the decreasing number of geriatricians recertifying.67 To meet the coming demand, more geriatric specialists are needed.
Factors Leading to Poor Outcomes in GTPs
Age-Specific Alterations in Response to Injury
Shock in the elderly may not be recognized. The aging myocardium is less able to respond to circulating catecholamines. Therefore, the elderly patient may not develop tachycardia in the presence of hypovolemia. As many elderly patients have hypertension, a “normal” or borderline blood pressure should be treated with suspicion. A systolic blood pressure less than 110 mm Hg may indicate a relative hypotension in the GTP. Cardiac responsiveness to hypovolemia (due to decreased sensitivity to catecholamines and associated β-blocker therapy) complicates resuscitation. Liberal use of echocardiography is recommended. Occult hypoperfusion may be detected by monitoring tissue hemoglobin oxygen saturation (StO2)68 or by measuring a base deficit or lactate. However, GTPs do not develop the magnitude of base deficit or lactate as younger patients, so these parameters must be evaluated with great care.69
Anticoagulants
Approximately 2.3 million individuals in the United States currently have been diagnosed with atrial fibrillation, and it is projected that 5.6 million Americans will develop it by 2050.70 Some community-based studies have projected a much higher atrial fibrillation disease burden, in the range of 15 to 16 million adults by the year 2050.71 Since anticoagulation therapy has been shown to reduce the risk of stroke in atrial fibrillation,72 the use of oral anticoagulants in patients with atrial fibrillation has become the standard of care and a quality benchmark measure. Recent studies have demonstrated that 11% to 20% of trauma patients 65 years or older were being treated with warfarin at the time of injury.73,74 In addition to warfarin, there are newer anticoagulants, such as direct thrombin inhibitors and factor Xa inhibitors. Because of the predictable anticoagulation response, these newer agents do not require routine anticoagulation monitoring75 but have the disadvantage of having no or limited reversal agents. While chronic anticoagulation may be beneficial in management of some medical conditions, it is a significant liability in trauma. Rapid confirmation of intracranial hemorrhage with expedited head CT scan, combined with prompt treatment and reversal of anticoagulation when indicated, has been shown to decrease progression of intracranial hemorrhage and reduce mortality;76 however, the correct protocols, role of prothrombin complex concentrate, and management of newer oral anticoagulants in the face of trauma remain unresolved significant issues.
Anticoagulation places GTPs at higher risk for serious bleeding even from minor injuries.77 Thus, CT scanning should be used to identify sources of hemorrhage and occult injuries. While the liberal use of CT scanning has been criticized in young patients, occult injuries (especially cervical spine and musculoskeletal injuries) are common in the elderly and the risk of radiation is minimal.78 If bleeding is identified, reversal protocols should be a used.
Other Medications
Patients or their family should be queried about medications that may have contributed to the injury, such as anti-hypertensives, sedatives, and antidepressants, or those that may confound the diagnosis of shock (e.g., β-blockers). Preexisting medical comorbidities, such as cerebrovascular disease, coronary artery disease, chronic obstructive pulmonary disease, or sepsis may complicate or precipitate the injury.79 GTPs with significant comorbidities should be admitted for monitoring, recognizing that delayed recognition or deterioration may not be well tolerated. The trauma team, as part of the tertiary survey, should clarify home medications (including dosages), comorbidities, baseline functional and cognitive impairments, and degree of frailty to facilitate hospital care and discharge planning.
Providers caring for GTPs should be aware of the impact of aging on specific organ functions and how this might affect common interventions. For those older than 50 years, renal mass is lost, decreasing glomerular filtration rate and increasing the risk of acute kidney injury. It is important to avoid unnecessary contrast exposure, adjust medication dosing based on renal function, and insure euvolemia. Respiratory function is also commonly compromised. There is an observed loss of the lung elastic recoil and significant reduction of the vital capacity. Decreased ventilation-perfusion mismatch with age decreases baseline arterial oxygen tension. Alterations in compliance and airway resistance result in an increased work of breathing. The combination of these factors increases the need for mechanical ventilation and difficulty in subsequent weaning.
Delirium
Hospital delirium in GTPs is common and is associated with increased mortality. Delirium is a global disturbance of consciousness characterized by fluctuating mental status, inattention, and disorganized thinking.8 Recent studies using standardized and validated tools have shown that delirium is significantly underdiagnosed,80 especially in the elderly. More importantly, delirium is a predictor of a threefold higher mortality and a higher cost of care.81 Most studies confirm the significantly high rate of delirium in geriatric patients.82
Medications are a frequent cause of delirium. The elderly are particularly sensitive to sedatives and analgesics. Benzodiazepines should be avoided, and narcotic use should be closely monitored. Consider early implementation of patient-controlled analgesia (with elderly-appropriate medications and dosing) and the early use of nonnarcotics. The presence of delirium should be routinely monitored and aggressively treated with a standard protocol. Rib fractures are quite common in the elderly, and a rib fracture protocol that emphasizes early effective pain management (with epidural or paravertebral catheters) coupled with aggressive respiratory therapy and mobilization has been shown to reduce pneumonia, in-hospital delirium, and mortality.83,84
Medication Mismanagement
Medications can be a serious cause of morbidity and mortality in the elderly; 30% of hospital admissions in the elderly are linked to drug-related problems or toxicity.85 It is estimated that medication-related problems cause 106,000 deaths annually at a cost of $85 billion.86 Medications and drug-related problems now rank as one of the leading causes of death and disability-adjusted life-years lost in the in the United States.87 Dr. M.H. Beers authored a landmark article in 1991 on the criteria for safe medication use in adults 65 years and older. The Beers criteria are well-known and universally consulted by the geriatric care community and are available on the Web site of the American Geriatric Society.88
End-of-Life Issues
Epidemiology of Death in the GTP
The epidemiology and demographics of traumatic death in the elderly have not been specifically examined. Data are available on the demographics of all-cause mortality in seniors, but specifics regarding the cause of death following injury are sparse and have been obtained from retrospective analyses of data derived from either single trauma centers or extracted from large data sets, such as the National Trauma Data Bank.
There are major impediments to obtaining accurate data on mortality following injury in seniors. First, reports on traumatic death often do not include mortalities caused by hip fractures following a fall from standing–one of the most common injuries associated with death in seniors.12 Second, there is disagreement regarding whether transfers to hospice care are counted as mortalities or survivors.89 Third, there is no explicit methodology for assigning the cause of death in GTPs, who may succumb as a direct result of the injury or die as a consequence of either an associated comorbidity or having life-sustaining treatment withdrawn.90 Finally, the convention of assessing quality and outcome based on the index hospitalization alone does not capture all GTP deaths that are trauma related, many of which occur after discharge.12 Consideration should be given to including postdischarge mortality data for the GTP.
From the available literature, it seems that the median age of GTPs dying after admission to a hospital for trauma is 82; 26% of whom died as a direct result of their injuries, while 60% died as a result of comorbidities or complications; hip fracture, as an isolated injury, was responsible for one third of the deaths in hospital.12 Head injury following a fall is the major cause of death in seniors.91,92
Compared with age- and sex-matched cohorts, GTPs have a diminished life expectancy compared with the uninjured elderly for up to 6 years following injury.12 The mortality rate following injury does not stabilize until 60 days after discharge from the index hospitalization, suggesting that in-hospital mortality should not be used as a quality indicator for seniors.12
Death of a GTP is due not only to the severity of injury but also to the admitting physiology and preexisting conditions. The exact contribution of each of these variables and their interplay relating to the outcome has not been thoroughly investigated. The “lethal dose” of injury producing mortality in 50% of GTPs is significantly less than it is in younger patients, but we do not know why this is so.
Goals of Care
One of the complexities of caring for elderly trauma patients is a failure of appreciation of their treatment goals. Early discussion of goals of care, with the patient or their surrogate, provides the opportunity to clarify desired treatments and avoid unwanted and perhaps invasive care. Addressing whether the patient has an advanced directive, health care power of attorney, or living will on admission is the best practice. Ongoing discussion is also important, as patient and/or surrogate desires may change based on changes in clinical status. Routine family meetings allow this ongoing discussion and will limit miscommunication.93 All of these discussions should be documented in the medical record.
Do-Not-Resuscitate and Advance Directives
Although often used interchangeably, the terms do not resuscitate (DNR), advance directives, and living will are not synonymous. An advance directive, which can include a living will, is a written expression of how a patient would want to be treated in certain medical circumstances. A DNR is a physician order specifying therapy if the patient were to experience cardiopulmonary arrest. Unfortunately, data on DNR and withdrawal of life-sustaining treatment in the injured elderly are sparse. Two recent publications addressed withdrawal of life-sustaining treatment in trauma-related deaths90,91 with remarkably similar findings. Withdrawal of life-sustaining treatment occurred in 42% to 54% of deaths; only 15% to 18% had advanced directives.
Ethical Challenges
Among the ethical issues that may arise in caring for elderly trauma patients is conflict between family members or between members of the health care team or between family and health care team. Perhaps, the most common is the inherent conflict between what the patient would want and what the decision maker wants. Explicit clarification is important because surrogate decision making is necessary in at least 30% of hospitalized elderly patients.94
Futility
Medical futility refers to the “appropriateness” of medical treatment.95 There are two types as follow: quantitative utility may occur when the treatment has a small (typically <1%) chance of success; qualitative utility may occur when the perceived quality of the benefit will be exceedingly poor for the individual patient. Texas and California currently have futility policies, while other states rely on individual institutional policies.
Improving Quality of Care at End of Life
The World Health Organization defines palliative care as, “an approach that improves the quality of life of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual.”96 It is distinct from hospice care, which specifically refers to care given to people in the final phase of a terminal illness, focusing on comfort and quality of life, rather than cure. The use of palliative care is associated with significant cost savings both for hospitals and payers.97
There is a deficit in provision of quality palliative care to geriatric patients. Numerous studies have reported poor pain management, lack of treatment for depression, and failure to address important emotional issues.98 Experts in the field have recently listed geriatric hip fracture as a condition in which the palliative care approach may be beneficial because of the staggering morbidity and mortality of this injury.99
Palliative care begins with symptom assessment. There are a number of age-specific validated tools that can be used to assess for symptoms,100 but none are specifically designed for GTPs. Once identified, symptom management is of paramount importance, with particular attention paid to pain. Mood disturbances, such as depression, should also be aggressively managed.
The Institute of Medicine defined a good death as, “one that is free from avoidable distress and suffering for patients, families, and caregivers, in general accord with patients’ families’ wishes, and reasonably consistent with clinical, cultural, and ethical standards.”101 Providers must remember, however, that the definition of good death is highly individualized, culturally based, and changes over time. Dying with dignity is a major concern of elderly patients, which often goes unmet.
Cost
Resource allocation at the end of life has become more important with the passage of the Affordable Care Act, which has expanded provisions for palliative care and hospice. Of the $491 billion spent by Medicare in 2009, 27% ($132.5 billion) was spent on acute care services.102 The percentage of total Medicare payments for decedents in the last year of life fluctuates between 27% and 30%.103 While there are data demonstrating the improved value of palliative care and hospice at the end of life, none of the studies specifically involve GTPs.104 However, it is estimated that the costs associated with futile care in the GTP has a median cost of $87,391 compared with nonfutile care that had a median cost of $33,373.12 Attempting to predict who will or should receive quantitatively futile care is difficult. Attempting to address this issue, Nirula and Gentilello105 examined the National Trauma Data Bank to “identify injury and physiologic parameters that would indicate a high probability of futile resuscitation among geriatric patients.” Choosing a cutoff for 95% probability of death (5% chance of survival based on injury severity and physiology), they found that the charge for caring for one of these patients was $38,223, and the total for the group was $3,287,254. To save 1 life and get that patient to discharge would require treatment of 20, at a total cost of $764,478.
Organ Donation
Donation of organs from seniors requires “expanded criteria” that are specific to the Organ Procurement Organization. From San Diego and Imperial Counties, patients older than 60 years without hypertension or a serum creatinine greater than 1.5 can be considered for donation. In the interval between 2009 and 2013, 11% to 14% of annual donors from the San Diego and Imperial County Organ Procurement Organization were older than 60 years. Thus, it seems reasonable to consider otherwise healthy seniors as suitable candidates for organ donation.
Research Agenda
Physiology of Aging
Much of what we understand about the physiology of aging is based on dated research. A contemporary analysis of the physiology of aging would help to elucidate the variation. Patients should be stratified by activity levels, medical comorbidities, and frailty indices, to determine whether specific functional deficits or medical issues predict worse outcomes. Neurocognitive deficits may differentially predispose patients to certain types of injuries compared with musculoskeletal defects, cardiopulmonary, metabolic, or other defects.
Magnitude of the Problem
Avalue analysis of the care of the GTP is warranted. The outcomes following hospitalization, extended care (i.e., in a SNF), and rehabilitation would inform the best allocation of resources.
Injury Prevention in GTPs
Data should be collected on the impact of injury prevention initiatives on the injured elderly, particularly in the area of fall prevention.
Outcomes of GTPs
GTPs have disparate outcomes compared with younger adults.106 An updated analysis including cutoff points for the age after which outcomes decline would help inform resource allocation and care protocols. Predictors of the GTP physiologic response to injury assist risk and outcome assessment. Lastly, disparities in access and care delivery should be studied for their impact on the GTP outcomes.
Discharge Disposition
It is also important to understand outcomes beyond hospital discharge. Much of the literature focuses on in-hospital outcomes, but many deaths occur well after discharge.12 Outcomes of trauma should not be limited to in-hospital or even long-term survival but should include behavioral health (incidence of posttraumatic stress disorder, delirium, depression, etc.) and functional quality-of-life self-assessments.
Who Should Care for GTPs?
Our current understanding of who is best able to care for the GTP is limited by the quality of data. Do GTPs receive better care at designated trauma centers, and if so, at what trauma center level? Do GTPs benefit from the involvement of geriatricians or internists? Further research is required to answer these questions.
How Can We Improve Care for GTPs?
Studies are needed to update and refine concepts such as the appropriateness of age alone as a trigger for prehospital triage or hospital trauma activation; the optimal resuscitation strategy for the injured elderly; the role for β-blockers or statins in the injured elderly; whether surgical indications differ between elderly and younger adult patients (i.e., cervical spine fixation); whether there are postdischarge interventions that can improve survival and functional outcomes; and whether we need a discrete performance improvement processes for the GTP population. Few data exist on effective and acceptable rehabilitation strategies for the older patient. Moreover, which interventions decrease the incidence of undesirable outcomes such as delirium, posttraumatic stress disorder, and depression in the geriatric trauma population is not well understood. Lastly, evidence-based guidelines and protocols to standardize care of the geriatric patient are needed, particularly in the area of anticoagulation reversal.
How to Proceed?
The current care of the injured geriatric patient has been outlined, with the identification of problems unique or specific to the elderly. Table 2 summarizes the Committee’s recommendations for potential solutions to these problem areas. It is clear that without targeted research on this vulnerable patient population, our efforts to improve care will be limited.
TABLE 2.
Problems in the Care of the GTP and Proposed Solutions
| Problem | Proposed Solution |
|---|---|
| Multiple definitions of the GTP | Age ≥ 65 y |
| Is hip fracture due to mechanical fall a TP? | Include hip fractures in the trauma data |
| LD 50 for GTP is much lower than YTP. | Research on stress response |
| LD 50 for GTP is much lower than YTP. | Useful frailty assessment tool (research) |
| Falls | Effective prevention strategies (research) |
| Elder abuse | Education and reporting |
| Undertriage | Reassess triage criteria for GTP |
| Trauma center vs. nontrauma center care | Research including value (outcome/cost) |
| Multiple care models | Research including value (outcome/cost) |
| Geriatric workforce: supply and demand | Expand geriatric workforce |
| Anticoagulants, antidepressants, antihypertensives | Medication management education |
| Mortality assessment | Transfer to hospice = death |
| Mortality assessment | Research: how long and in whom? |
| Mortality assessment | Consistent methodology on adjudication of deaths |
| Palliative care models | Research: transfer or stay on trauma |
| Palliative care models | Research on value (outcome/cost) |
| Poor long-term outcomes | Research: posthospital rehabilitation |
| Poor long-term outcomes | Improve quality of care at the SNFs |
LD 50, dose producing death in 50% of patients; TP, trauma patient; YTP, young trauma patient.
Footnotes
DISCLOSURE
The authors declare no conflicts of interest.
References
- 1.United States Population Projections: 2000 to 2050. Available at: www.census.gov/population/projections/files/analytical-document09.pdf.
- 2.Centers for Disease Control and Prevention. Injury Prevention & Control: Data & Statistics (WISQARSTM) Available at: www.cdc.gov/injury/wisqars/pdf/leading causes of death by age group 2012-a.pdf.
- 3.Gage AM, Traven N, Rivara FP, Jurkovich GJ, Arbabi S. Compliance with Centers for Disease Control and Prevention field triage guidelines in an established trauma system. J Am Coll Surg. 2012;215(1):146–148. doi: 10.1016/j.jamcollsurg.2012.02.025. [DOI] [PubMed] [Google Scholar]
- 4.Garwe T, Cowan LD, Neas BR, Sacra JC, Albrecht RM, Rich KM. A propensity score analysis of prehospital factors and directness of transport of major trauma patients to a level I trauma center. J Trauma. 2011;70(1):120–129. doi: 10.1097/TA.0b013e3181d89439. [DOI] [PubMed] [Google Scholar]
- 5.Mackersie RC. For the care of the underserved. J Trauma Acute Care Surg. 2014;77(5):653–659. doi: 10.1097/TA.0000000000000440. [DOI] [PubMed] [Google Scholar]
- 6.Zarzaur BL, Kozar Ra, Fabian TC, Coimbra R. A survey of American Association for the Surgery of Trauma member practices in the management of blunt splenic injury. J Trauma. 2011;70(5):1026–1031. doi: 10.1097/TA.0b013e318217080c. [DOI] [PubMed] [Google Scholar]
- 7.Calland JF, Ingraham AM, Martin N, Marshall GT, Schulman CI, Stapleton T, Barraco RD. Evaluation and management of geriatric trauma: an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg. 2012;73(5 Suppl 4):S345–S350. doi: 10.1097/TA.0b013e318270191f. [DOI] [PubMed] [Google Scholar]
- 8.Pandharipande P, Cotton BA, Shintani A, Thompson J, Pun BT, Morris JA, Jr, Dittus R, Ely EW. Prevalence and risk factors for development of delirium in surgical and trauma intensive care unit patients. J Trauma. 2008;65(1):34–41. doi: 10.1097/TA.0b013e31814b2c4d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Orlando A, Salottolo K, Uribe P, Howell PA. A 5-year review of a trauma-trained hospitalist program for trauma patients : a matched cohort study. Surgery. 2010;152(1):61–68. doi: 10.1016/j.surg.2012.01.004. [DOI] [PubMed] [Google Scholar]
- 10.Davidson GH, Hamlat CA, Rivara FP, Koepsell TD, Jurkovich GJ, Arbabi S. Long-term survival of adult trauma patients. JAMA. 2011;305(10):1001–1007. doi: 10.1001/jama.2011.259. [DOI] [PubMed] [Google Scholar]
- 11.Sise MJ, Sise CB, Thorndike JF, Kahl JE, Calvo RY, Shackford SR. Withdrawal of care: a 10-year perspective at a level I trauma center. J Trauma Acute Care Surg. 2012;72(5):1186–1193. doi: 10.1097/TA.0b013e31824d0e57. [DOI] [PubMed] [Google Scholar]
- 12.Fleischman RJ, Adams AL, Hedges JR, Ma OJ, Mullins RJ, Newgard CD. The optimum follow-up period for assessing mortality outcomes in injured older adults. J Am Geriatr Soc. 2010;58(10):1843–1849. doi: 10.1111/j.1532-5415.2010.03065.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Labib N, Nouh T, Winocour S, Deckelbaum D, Banici L, Fata P, Razek T, Khwaja K. Severely injured geriatric population: morbidity, mortality, and risk factors. J Trauma. 2011;71(6):1908–1914. doi: 10.1097/TA.0b013e31820989ed. [DOI] [PubMed] [Google Scholar]
- 14.Bergeron E, Clement J, Lavoie A, Ratte S, Bamvita JM, Aumont F, Clas D. A simple fall in the elderly: not so simple. J Trauma. 2006;60(2):268–273. doi: 10.1097/01.ta.0000197651.00482.c5. [DOI] [PubMed] [Google Scholar]
- 15.Taylor MD, Tracy JK, Meyer W, Pasquale M, Napolitano LM. Trauma in the elderly: intensive care unit resource use and outcome. 1997;53(3):407–414. doi: 10.1097/00005373-200209000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Adams SD, Cotton BA, McGuire MF, Dipasupil E, Podbielski JM, Zaharia A, Ware DN, Gill BS, Albarado R, Kozar RA, et al. Unique pattern of complications in elderly trauma patients at a Level I trauma center. J Trauma Acute Care Surg. 2012;72(1):112–118. doi: 10.1097/TA.0b013e318241f073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Clegg A, Trust DM. The frailty syndrome. Clin Med. 2011;11(1):72–75. doi: 10.7861/clinmedicine.11-1-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–M156. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 19.Syddall H, Roberts HC, Evandrou M, Cooper C, Bergman H, Sayer AA. Prevalence and correlates of frailty among community-dwelling older men and women: findings from the Hertfordshire Cohort Study. Age Ageing. 2009;39:197–203. doi: 10.1093/ageing/afp204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ensrud KE, Ewing SK, Taylor BC, Fink HA, Stone KL, Cauley JA, Tracy JK, Hochberg MC, Rodondi N, Cawthon PM. Frailty and risk of falls, fracture, and mortality in older women: the study of osteoporotic fractures. J Gerontol A Biol Sci Med Sci. 2007;62:744–751. doi: 10.1093/gerona/62.7.744. [DOI] [PubMed] [Google Scholar]
- 21.Joseph B, Pandit V, Zangbar B, Kulvatunyou N, Hashmi A, Green DJ, O’Keeffe T, Tang A, Vercruysse G, Fain MJ, et al. Superiority of frailty over age in predicting outcomes among geriatric trauma patients: a prospective analysis. JAMA Surg. 2014;149:766–772. doi: 10.1001/jamasurg.2014.296. [DOI] [PubMed] [Google Scholar]
- 22.Joseph B, Pandit V, Sadoun M, Zangbar B, Fain MJ, Friese RS, Rhee P. Frailty in surgery. J Trauma Acute Care Surg. 2014;76(4):1151–1156. doi: 10.1097/TA.0000000000000103. [DOI] [PubMed] [Google Scholar]
- 23.Rockwood K, Mitnitski A. Frailty in relation to the accumulation of deficits. J Gerontol A Biol Sci Med Sci. 2007;62:722–727. doi: 10.1093/gerona/62.7.722. [DOI] [PubMed] [Google Scholar]
- 24.Min L, Ubhayakar N, Saliba D, Kelley-Quon L, Morley E, Hiatt J, Cryer H, Tillou A. The vulnerable elders survey-13 predicts hospital complications and mortality in older adults with traumatic injury: a pilot study. J Am Geriatr Soc. 2011;59:1471–1476. doi: 10.1111/j.1532-5415.2011.03493.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Morley JE, Argiles JM, Evans WJ, Bhasin S, Cella D, Deutz NE, Doehner W, Fearon KC, Ferrucci L, Hellerstein MK, et al. Nutritional recommendations for the management of sarcopenia. J Am Med Dir Assoc. 2010;11(6):391–396. doi: 10.1016/j.jamda.2010.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moisey LL, Mourtzakis M, Cotton BA, Premji T, Heyland DK, Wade CE, Bulger E, Kozar RA. Skeletal muscle predicts ventilator-free days, ICU-free days, and mortality in elderly ICU patients. Crit Care. 2013;17(5):R206. doi: 10.1186/cc12901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grossman M, Scaff DW, Miller D, Reed J, Hoey B, Anderson HL. Functional outcomes in octogenarian trauma. J Trauma. 2003;55:26–32. doi: 10.1097/01.TA.0000072109.52351.0D. [DOI] [PubMed] [Google Scholar]
- 28.Grossman MD, Miller D, Scaff DW, Arcona S. When is an elder old? Effect of preexisting conditions on mortality in geriatric trauma. J Trauma. 2002;52:242–246. doi: 10.1097/00005373-200202000-00007. [DOI] [PubMed] [Google Scholar]
- 29.Richmond TS, Kauder D, Strumpf N, Meredith T. Characteristics and outcomes of serious traumatic injury in older adults. J Am Geriatr Soc. 2002;50:215–222. doi: 10.1046/j.1532-5415.2002.50051.x. [DOI] [PubMed] [Google Scholar]
- 30.Claridge JA, Leukhardt WH, Golob JF, McCoy AM, Malangoni MA. Moving beyond traditional measurement of mortality after injury: evaluation of risks for late death. J Am Coll Surg. 2010;210(5):788–794. 794–796. doi: 10.1016/j.jamcollsurg.2009.12.035. [DOI] [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention. Available at: www.cdc.gov/HomeandRecereationalSafety/Falls/adultfalls.html.
- 32.Friedman SM, Mendelson DA, Bingham KW, Kates SL. Impact of a comanaged Geriatric Fracture Center on short-term hip fracture outcomes. Arch Intern Med. 2009;169(18):1712–1717. doi: 10.1001/archinternmed.2009.321. [DOI] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention. Fatal Injury Reports. Available at: www.cdc.gov/injury/wisqars/fatal_injury_reports.html.
- 34.Available at: www.ircobi.org/downloads/irc12/pdf/pdf_files/14.pdf.
- 35.Intersection Crashes Among Drivers in Their 60s, 70s, and 80s. Available at: www.nhtsa.gov/staticfiles/nti/pdf/811495.pdf.
- 36.How to Understand & Influence Older Drivers. Available at: www.nhtsa.gov/people/injury/olddrive/UnderstandOlderDrivers.
- 37.Physician’s Guide to Assessing and Counseling Older Drivers. doi: 10.1016/j.annemergmed.2004.03.024. Available at: www.nhtsa.gov/staticfiles/nti/older_drivers/pdf/811298.pdf. [DOI] [PubMed]
- 38.Licensing Procedures for Older Drivers. Available at: www.nhtsa.gov/staticfiles/nti/pdf/811833.pdf.
- 39.Traffic Safety Facts 2010 Data. Available at: www-nrd.nhtsa.dot.gov/Pubs/811625.PDF.
- 40.NYC Department of Aging. Available at: www.nyc.gov/html/dfta/html/senior/pedestrian.shtml.
- 41.Centers for Disease Control and Prevention. Pedestrian Safety. Available at: www.cdc.gov/Motorvehiclesafety/Pedestrian_safety/index.html.
- 42.Available at: www.cdc.gov/ncipc/wisqars.
- 43.Rowe J, Conwell Y, Schulberg H, Bruce M. Social support and suicidal ideation in older adults using home healthcare services. Am J Geriatr Psychiatry. 2006;14:758–766. doi: 10.1097/01.JGP.0000218324.78202.25. [DOI] [PubMed] [Google Scholar]
- 44.Available at: www.apps.nimh.nih.gov/health/publications/suicide-in-the-us-statistics-and-prevention.shtml.
- 45.Centers for Disease Control and Prevention. Elder Abuse: Definitions. Available at: www.cdc.gov/violenceprevention/elderabuse/definitions.html.
- 46.Acierno R, Hernandez M, Amstadter A, Resnick HS, Steve K, Muzzy W, Kilpatrick DG. Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States; the National Elder Mistreatment Study. Am J Public Health. 2010;100:292–297. doi: 10.2105/AJPH.2009.163089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Centers for Disease Control and Prevention. Elder Abuse Prevention. Available at: www.cdc.gov/Features/ElderAbuse.
- 48.Anetzberger GJ. An update on the nature and scope of elder abuse. Generations. 2012;36(13):12–20. [Google Scholar]
- 49.Caregiving Resource Center. Available at: www.aarp.org/home-family/caregiving.
- 50.Lehmann R, Beekley A, Casey L, Salim A, Martin M. The impact of advanced age on trauma triage decisions and outcomes. Am J Surg. 2009;197:571–574. doi: 10.1016/j.amjsurg.2008.12.037. [DOI] [PubMed] [Google Scholar]
- 51.Sasser SM, Hunt RC, Faul M, Sugerman D, Pearson WS, Dulski T, Wald MM, Jurkovich GJ, Newgard CD, Lerner EB. Guidelines for field triage of injured patients: recommendations of the National Expert Panel on Field Triage, 2011. MMWR Recomm Rep. 2012;61(RR-1):1–20. [PubMed] [Google Scholar]
- 52.Chang DC, Bass RR, Cornwell EE, Mackenzie EJ. Undertriage of elderly trauma patients to state-designated trauma centers. Arch Surg. 2008;143(8):776–781. doi: 10.1001/archsurg.143.8.776. [DOI] [PubMed] [Google Scholar]
- 53.Lane P, Sorondo B, Kelly JJ. Geriatric trauma patients–are they receiving trauma center care? Acad Emerg Med. 2003;10(3):244–250. doi: 10.1197/aemj.10.3.244. [DOI] [PubMed] [Google Scholar]
- 54.Tepas JJ, 3rd, Veldenz HC, Lottenberg L, Romig LA, Pearman A, Hamilton B, Slevinski RS, Villani DJ. Elderly injury: a profile of trauma experience in the Sunshine (Retirement) State. J Trauma. 2000;48(4):581–586. doi: 10.1097/00005373-200004000-00001. [DOI] [PubMed] [Google Scholar]
- 55.Meldon SW, Reilly M, Drew B, Mancusco C, Fallon W. Trauma in the very elderly: a community-based study of outcomes at trauma and non-trauma centers. Acad Emerg Med. 2000;7(10):1166. [PubMed] [Google Scholar]
- 56.Demetriades D, Sava J, Alo K, et al. Old age as a criterion for trauma team activation. J Trauma. 2001;51(4):754–756. doi: 10.1097/00005373-200110000-00022. [DOI] [PubMed] [Google Scholar]
- 57.Goodmanson NW, Rosengart MR, Barnato AE, Sperry JL, Peitzman AB, Marshall GT. Defining geriatric trauma: when does age make a difference? Surgery. 2012;152(4):668–674. doi: 10.1016/j.surg.2012.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, Salkever DS, Scharfstein DO. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354(4):366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 59.Oyetunji T, Chang DC, Crompton JG, Greene WR, Efron DT, Haut ER, Cornwell EE, 3rd, Haider AH. Redfining hypotension in the elderly: normotension is not reassuring. Arch Surg. 2011;146:865–869. doi: 10.1001/archsurg.2011.154. [DOI] [PubMed] [Google Scholar]
- 60.Mion L, Odegard P, Resnick B, Segal-Galan F. Interdisciplinary care for older adults with complex needs: American Geriatrics Society position statement. J Am Geriatr Soc. 2006;54:849–851. doi: 10.1111/j.1532-5415.2006.00707.x. [DOI] [PubMed] [Google Scholar]
- 61.Group IA. Position statement on interdisciplinary care team training in geriatrics: an essential component of quality health care for older adults. J Am Geriatr Soc. 2014;62:961–965. doi: 10.1111/jgs.12822. [DOI] [PubMed] [Google Scholar]
- 62.Fallon WF, Jr, Rader E, Zyzanski S, Mancuso C, Martin B, Breedlove L, DeGolia P, Allen K, Campbell J. Geriatric outcomes are improved by a geriatric trauma consultation service. J Trauma. 2006;61(5):1040–1046. doi: 10.1097/01.ta.0000238652.48008.59. [DOI] [PubMed] [Google Scholar]
- 63.Mangram AJ, Mitchell CD, Shifflette VK, Lorenzo M, Truitt MS, Goel A, Lyons MA, Nichols DJ, Dunn EL. Geriatric trauma service: a one-year experience. J Trauma Acute Care Surg. 2012;72(1):119–122. doi: 10.1097/TA.0b013e318241f0ba. [DOI] [PubMed] [Google Scholar]
- 64.Lenartowicz M, Parkovnick M, McFarlan A, Haas B, Straus SE, Nathens AB, Wong CL. An evaluation of a proactive geriatric trauma consultation service. Ann Surg. 2012;256:1098–1101. doi: 10.1097/SLA.0b013e318270f27a. [DOI] [PubMed] [Google Scholar]
- 65.The John A. Hartford Foundation. Available at: www.jhartfound.org/images/upoads/resources/Business_Case_5-17_3.pdf.
- 66.Association of Directors of Geriatric Academic Programs. Fellows in geriatric medicine and geriatric psychiatry programs. Training and Practice Update. 2007;5(2):1–7. [Google Scholar]
- 67.Gawandi A. The way we age now: medicine has increased the ranks of the elderly. Can it make old age easier? New Yorker. 2007;30:50–59. [PubMed] [Google Scholar]
- 68.Cohn SM, Nathens AB, Moore FA, Rhee P, Puyana JC, Moore EE, Beilman GJ. Tissue oxygen saturation predicts the development of organ dysfunction during traumatic shock resuscitation. J Trauma. 2007;62(1):44–54. doi: 10.1097/TA.0b013e31802eb817. [DOI] [PubMed] [Google Scholar]
- 69.Davis J, Kaups K. Base deficit in the elderly: a marker of severe injury and death. J Trauma. 1998;45:873–877. doi: 10.1097/00005373-199811000-00005. [DOI] [PubMed] [Google Scholar]
- 70.Tsang T, Petty G, Barnes M, O’Fallon WM, Bailey KR, Wiebers DO, Sicks JD, Christianson TJ, Seward JB, Gersh BJ. The prevalence of atrial fibrillation in incident stroke cases and matched population controls in Rochester, Minnesota; changes over three decades. J Am Coll Cardiol. 2003;42:93–100. doi: 10.1016/s0735-1097(03)00500-x. [DOI] [PubMed] [Google Scholar]
- 71.Lakshminarayan K, Anderson D, Herzog C, Quershi A. Clinical epidemiology and related cardiovascular events in the United States. Neurologist. 2008;14:143–150. doi: 10.1097/NRL.0b013e31815cffae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Mant J, Hobbs F, Fletcher K, Roalfe A, Fitzmaurice D, Lip GY, Murray E. Warfarin versus aspirin for stroke prevention in an elderly community population with atrial fibrillation: a randomized controlled trial. Lancet. 2007;370:493–503. doi: 10.1016/S0140-6736(07)61233-1. [DOI] [PubMed] [Google Scholar]
- 73.Franko J, Kish KJ, O’Connell BG, Subramanian S, Yuschak JV. Advanced age and preinjury warfarin anticoagulation increase the risk of mortality after head trauma. J Trauma. 2006;61(1):107–110. doi: 10.1097/01.ta.0000224220.89528.fc. [DOI] [PubMed] [Google Scholar]
- 74.Grandhi R, Duane TM, Dechert T, Malhotra AK, Aboutanos MB, Wolfe LG, Ivatury RR. Anticoagulation and the elderly head injured patient. Am Surg. 2008;74:802–805. doi: 10.1177/000313480807400905. [DOI] [PubMed] [Google Scholar]
- 75.Tran A, Cheng-Lai A. Dabigatran etexilate: the first oral anticoagulant available in the United States since warfarin. Cardiol Rev. 2011;19:154–161. doi: 10.1097/CRD.0b013e3182137758. [DOI] [PubMed] [Google Scholar]
- 76.Ivascu FA, Howells GA, Junn FS, Bair HA, Bendick PJ, Janczyk RJ. Rapid warfarin reversal in anticoagulated patients with traumatic intracranial hemorrhage reduces hemorrhage progression and mortality. J Trauma. 2005;59(5):1131–1139. doi: 10.1097/01.ta.0000189067.16368.83. [DOI] [PubMed] [Google Scholar]
- 77.Thachil J, Gatt a, Martlew V. Management of surgical patients receiving anticoagulation and antiplatelet agents. Br J Surg. 2008;95(12):1437–1448. doi: 10.1002/bjs.6381. [DOI] [PubMed] [Google Scholar]
- 78.Jacobs DG. Special considerations in geriatric injury. Curr Opin Crit Care. 2003;9(6):535–539. doi: 10.1097/00075198-200312000-00012. [DOI] [PubMed] [Google Scholar]
- 79.Kim SW, Han HS, Jung HW, Kim KI, Hwang DW, Kang SB, Kim CH. Multidimensional frailty score for the prediction of postoperative mortality risk. JAMA Surg. 2014;149(7):633–640. doi: 10.1001/jamasurg.2014.241. [DOI] [PubMed] [Google Scholar]
- 80.Ely EW, Inouye SK, Bernard GR, Gordon S, Francis J, May L, Truman B, Speroff T, Gautam S, Margolin R, et al. Delerium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit. JAMA. 2001;286:2703–2710. doi: 10.1001/jama.286.21.2703. [DOI] [PubMed] [Google Scholar]
- 81.Milbrandt E, Deppen S, Harrison P, et al. Costs associated with delerium in mechanically ventilated patients. Crit Care Med. 2004;32:955–962. doi: 10.1097/01.ccm.0000119429.16055.92. [DOI] [PubMed] [Google Scholar]
- 82.Alvarez Fernandez B, Formiga F, Gomez R. Delirium in hospitalized older patients: a review. J Nutr Heal Aging. 2008;12:246–251. doi: 10.1007/BF02982629. [DOI] [PubMed] [Google Scholar]
- 83.Todd SR, McNally MM, Holcomb JB, Kozar RA, Kao LS, Gonzalez EA, Cocanour CS, Vercruysse GA, Lygas MH, Brasseaux BK, et al. A multidisciplinary clinical pathway decreases rib fracture-associated infectious morbidity and mortality in high-risk trauma patients. Am J Surg. 2006;192(6):806–811. doi: 10.1016/j.amjsurg.2006.08.048. [DOI] [PubMed] [Google Scholar]
- 84.Gage A, Rivara F, Wang J, Jurkovich GJ, Arbabi S. The effect of epidural placement in patients after blunt thoracic trauma. J Trauma Acute Care Surg. 2014;76(1):36–39. doi: 10.1097/TA.0b013e3182ab1b08. [DOI] [PubMed] [Google Scholar]
- 85.Hanlon J, Schmader KE, Koronkowski MJ, Weinberger M, Landsman PB, Samsa GP, Lewis IK. Adverse drug events in high risk older out-patients. J Am Geriatr Soc Am Geriatrc. 1997;45:945. doi: 10.1111/j.1532-5415.1997.tb02964.x. [DOI] [PubMed] [Google Scholar]
- 86.Perry D. When medicine hurts instead of helps. Consultant Pharmacist. 1991;14:1326–1330. [Google Scholar]
- 87.Murray CJ, Atkinson C, Bhalla K, Birbeck G, Burstein R, Chou D, Dellavalle R, Danaei G, Ezzati M, Fahimi A, et al. The state of US heath, 1990–2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310:591–608. doi: 10.1001/jama.2013.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.The American Geriatrics Society. AGS Guidelines & Recommendations. Available at: www.americangeriatrics.org/health_care_professionals.
- 89.Kozar RA, Holcomb JB, Xiong W, Nathens AB. Are all deaths recorded equally? The impact of hospice care on risk-adjusted mortality. J Trauma Acute Care Surg. 2014;76(3):634–639. doi: 10.1097/TA.0000000000000130. [DOI] [PubMed] [Google Scholar]
- 90.Franklin GA, Cannon RW, Smith JW, Harbrecht BG, Miller FB, Richardson JD. Impact of withdrawal of care and futile care on trauma mortality. Surgery. 2011;150(4):854–860. doi: 10.1016/j.surg.2011.07.065. [DOI] [PubMed] [Google Scholar]
- 91.Kahl JE, Calvo RY, Sise MJ, Sise CB, Thorndike JF, Shackford SR. The changing nature of death on the trauma service. J Trauma Acute Care Surg. 2013;75(2):195–201. doi: 10.1097/TA.0b013e3182997865. [DOI] [PubMed] [Google Scholar]
- 92.Thompson HJ, Bourbonniere M. Traumatic injury in the older adult from head to toe. Crit Care Nurs Clin North Am. 2006;18(3):419–431. doi: 10.1016/j.ccell.2006.05.008. [DOI] [PubMed] [Google Scholar]
- 93.Trunkey DD, Cahn RM, Lenfesty B, Mullins RJ. Management of the geriatric trauma patient at risk of death: therapy withdrawal decision making. Arch Surg. 2001;136:165–168. doi: 10.1001/archsurg.135.1.34. [DOI] [PubMed] [Google Scholar]
- 94.Silviera M, Scott Y, Langa K. Advance directives and outcomes of surrogate decision making before death. N Engl J Med. 2010;362:1211–1218. doi: 10.1056/NEJMsa0907901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Available at: www.eperc.mcw.edu/EPERC/FastFactsIndex/ff_136.htm.
- 96.World Health Organization. Available at: www.who.org/programmes/cancer/palliative care.
- 97.Morrison S, Penrod J, Cassal J, Caust-Ellenbogen M, Spragens L, Meier D. Cost savings associated with US hospital palliative care consultation programs. Arch Intern Med. 2008;168:1783–1790. doi: 10.1001/archinte.168.16.1783. [DOI] [PubMed] [Google Scholar]
- 98.Jeraant AF, Azari RS, Nesbitt TS, Meyers FJ. The TLC model of palliative care in the elderly: preliminary application in the assisted living setting. Ann Fam Med. 2004;2:54–60. doi: 10.1370/afm.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ko FC, Morrison RS. Hip fracture: a trigger for palliative care in vulnerable older adults. JAMA Int Med. 2014;174(8):1281–1282. doi: 10.1001/jamainternmed.2014.999. [DOI] [PubMed] [Google Scholar]
- 100.Amella EJ. Geriatrics and palliative care: collaboration for quality of life until death. J Hosp Palliat Nurs. 2003;5(1):40–48. [Google Scholar]
- 101.Field M, Cassell C. Approaching D: Improving Care at End of Life (IOM Report) Washington, DC: National Academy Press; 1997. [Google Scholar]
- 102.Meier DE. Increased access to palliative care and hospice services: opportunities to improve value in health care. Milbank Q. 2011;89:343–380. doi: 10.1111/j.1468-0009.2011.00632.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Lubitz J, Beebe J, Baker C. Longevity and Medicare expenditures. N Engl J Med. 1995;332:999–1003. doi: 10.1056/NEJM199504133321506. [DOI] [PubMed] [Google Scholar]
- 104.Smith TJ, Cassel JB. Cost and non-clinical outcomes of palliative care. J Pain Symptom Manage. 2009;38(1):32–44. doi: 10.1016/j.jpainsymman.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 105.Nirula R, Gentilello LM. Futility of resuscitation criteria for the “young” old and the “old” old trauma patient: a National Trauma Data Bank analysis. J Trauma. 2004;57(1):37–41. doi: 10.1097/01.ta.0000128236.45043.6a. [DOI] [PubMed] [Google Scholar]
- 106.Taylor MD, Tracy JK, Meyer W, Pasquale M, Napolitano LM. Trauma in the elderly: intensive care unit resource use and outcome. J Trauma. 2002;53(3):407–414. doi: 10.1097/00005373-200209000-00001. [DOI] [PubMed] [Google Scholar]