Abstract
Acantholytic dyskeratosis (AD) is a histologic pattern seen in Darier's disease or dyskeratosis follicularis, warty dyskeratoma, and transient AD. This pattern is characterized by suprabasilar clefting, acantholysis, and formation of corps ronds and grains. We present a case of AD that is unique based on its genital location and cystic architecture. A 53-year-old woman presented with an otherwise asymptomatic cyst on her left vulva of uncertain duration. On microscopic examination, there were fragments of cystic epithelium with areas of hypergranulosis, acantholysis, corps ronds, and corps grains formation. These features are felt by the authors to be a unique presentation of a follicular adnexal neoplasm.
Keywords: Acantholytic dyskeratosis, cystic acantholytic dyskeratosis, dyskeratosis follicularis, wartydyskeratoma
INTRODUCTION
Acantholytic dyskeratosis (AD) is a histologic pattern characterized by hypergranulosis, acantholysis, suprabasilar clefting, and formation of corps ronds and grains. This can be seen in Darier's disease (DD) or dyskeratosis follicularis, transient acantholytic dyskeratosis (TAD) or Grover disease (GD), as well as in isolated lesions, such as warty dyskeratoma (WD), acantholytic dyskeratotic acanthoma, and as an incidental histopathologic finding of isolated AD.
DD, TAD, and WD are all papular dermatoses. DD is an autosomal dominant disease, whereas TAD and WD are nonhereditary. DD and TAD occur most commonly in seborrheic areas and WD most commonly in the head, neck, trunk, and extremities.[1,2,3] There have been rare cases of oral and genital involvement reported.[4,5,6,7,8] We present a case of acantholytic dyskeratosis that is unique based on its genital location and cystic architecture.
CASE REPORT
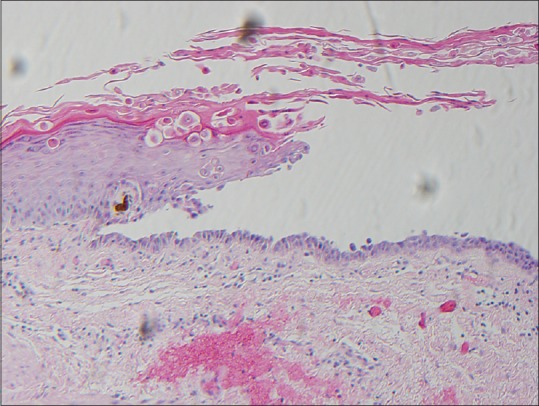
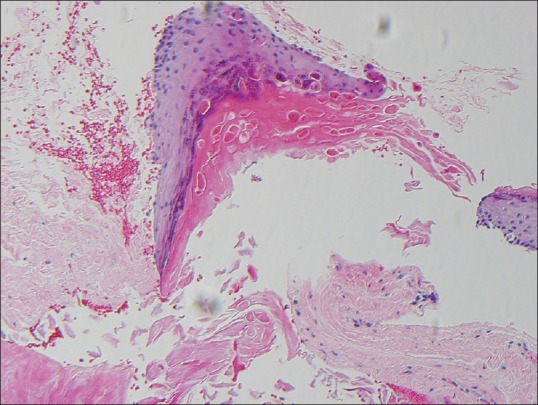
A 53-year-old woman presented with an otherwise asymptomatic cyst on her left vulva of uncertain duration. The initial clinical diagnosis was vulvar abscess. There was no known history of generalized skin conditions with similar histology and there were no associated lesions of the vulva or the cervix. The family history was negative for DD or other multiple dermatologic papules and nodules. The lesion was surgically removed and submitted for routine histologic processing and staining with hemotoxylin and eosin. On microscopic examination, there were fragments of cystic epithelium with areas of hypergranulosis, acantholysis, suprabasilar clefting, and corps ronds, and grains formation [Figures 1–3]. These features were felt to represent isolated dyskeratosis follicularis arising in the context of an infundibular cyst.
Figure 1.
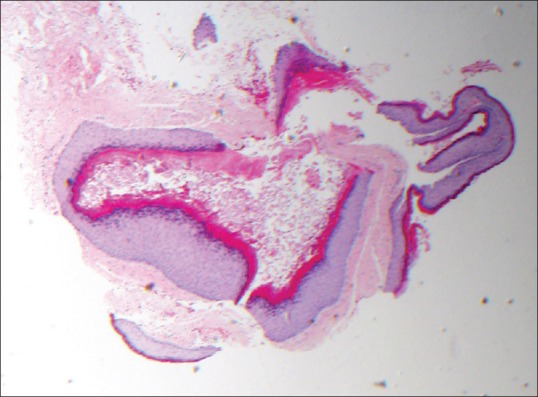
Fragments of cystic epithelium. Hematoxylin and eosin ×20
Figure 3.
Medium power view of cyst demonstrating corps ronds, grains, and suprabasal acantholysis. H and E ×100
Figure 2.
Medium power view of cystic lesion demonstrating hypergranulosis, acantholysis, and corps ronds formation. H and E ×100
DISCUSSION
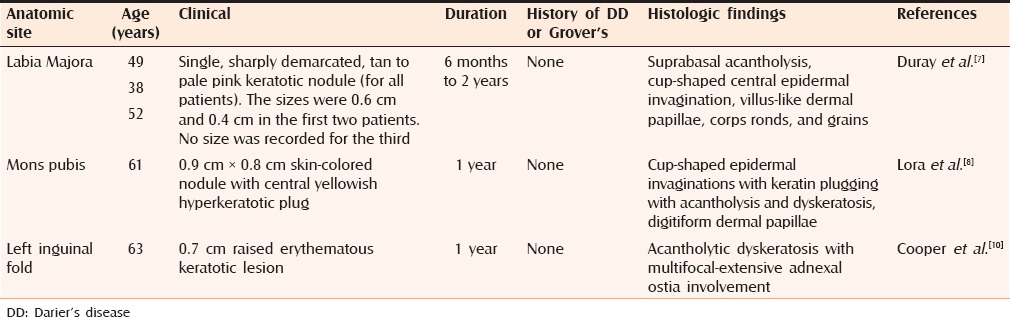
Changes of dyskeratosis follicularis are unusual in the genitalia but there have been cases of multiple papular lesions on the genital area reported under various terminology, including “papular acantholytic dyskeratosis”[9] and acantholytic dermatosis of the vulvocrural fold.[10] Solitary lesions of dyskeratosis follicularis have rarely been reported in this area. In fact, in a review of 28 cases of isolated dyskeratotic acanthoma, none occurred in the genital area.[11] We were able to identify three reports of solitary genital lesions of isolated AD[7,8,10] [Table 1]. One of the six vulvocrural cases described in the series by Cooper[10] exhibited cystic invaginations with multiple follicular connections and histologic features of Lora et al.'s[8] report of WD on the mons pubis also histologically showed a similar cup-shaped cystic invaginations involving multiple indundibulae. And of the three vulvar cases of WD reported by Duray et al.,[7] at least one appears to show a cystic invagination adjacent to or involving a pilosebaceous unit. However, none of these genital cases of AD demonstrated changes with a truly cystic architecture, as seen in our patient.
Table 1.
Cases of warty dyskeratoma located on the genital area
Our patient's lesion could be considered to represent an unusual presentation of WD. WD commonly presents as a solitary, keratotic papule or nodule on the sun-exposed areas in middle-aged males. Histologically, WD displays broad, well-circumscribed invagination of a hyperplastic epidermis with hypergranulosis and papillomatosis, suprabasilar acantholysis, villi formation of the dermal papillae, and presence of dyskeratotic squamous cells (corps ronds and grains). Histologic overlap of cystic, nodular, and cup-shaped patterns have been noted in a large clinicopathologic review of WD.[3] The cystic lesions are described as well-circumscribed nodules composed of one or several large infundibular cystic structures filled with masses of keratin material located in the papillary and upper reticular dermis. The cystic structures have a stratified squamous epithelial lining with foci of hypergranulosis and papillomatosis. A focal connection to the epidermis is sometimes observed.
Although it lacked the typical hyperplastic villous-like proliferations at the periphery seen in other cases of WD, this lesion presented herein otherwise exhibited hypergranulosis, dyskeratosis resulting in “iris” and “target” morphologic features of corps ronds, and suprabasilar acanthoysis, all of which are typical of WD. The cystic architecture described by Kaddu et al.[3] in other locations is reminiscent of our lesion, suggesting our lesion may lie on a spectrum of infundibular cyst and WD.[3] Contiguity with cystic infundibular structures described in the genital cases reported by Cooper[10] and Lora et al.[8] lends further support to the theory that WD is a distinctive follicular adnexal neoplasm. Kaddu et al.[3] show a clear-cut histologic connection of these lesions to rudimentary pilosebaceous units or at least were located adjacent to a pilosebaceous unit. In another retrospective study,[12] CK1 and CK10 were expressed in the suprabasal levels of the WD cases, whereas CK5 and CK17 were appreciated in the basal layer. This pattern of expression of cytokeratin markers further supports WD as an adnexal neoplasm with follicular differentiation. The term follicular dyskeratoma has been proposed to acknowledge the follicular infundibular origin of WD.[3] In keeping with this theory, we feel that the infundibular cystic features seen in our patient's lesion represent a spectrum of changes that can be seen in follicular dyskeratoma.
Vulvar WD with cystic configuration has never been reported [based on PubMed search], and to the best of our knowledge, our case is the first to describe such a lesion occurring on this site.
In addition to the various presentations of AD, the differential diagnosis of acantholysis on the vulva may include pemphigus vulgaris, herpes simplex virus, and Hailey–Hailey disease. These entities are excluded in the absence of positive immunofluorescence in pemphigus, presence of viral changes in herpes, and more prominent acantholysis and less dyskeratosis in Hailey–Hailey. Acantholytic squamous cell carcinoma (SCC) is differentiated by the absence of cytologic atypia in WD. Clinically, genital WD may resemble condylomata and bowenoid papulosis. These may easily be distinguished histopathologically.
Interestingly, cystic DD,[13] cystic SCC,[14,15] and keratoacanthoma with associated cystic sebaceous tumors in a Muir–Torre syndrome patient[16] have been reported. Although rare and reported to occur at nongenital sites, these entities should be considered as the most important differential diagnoses for cystic WD.
The definitive treatment for WD is surgical excision.[3] Topical tazarotenic acid gel was reported to be effective in one patient.[17]
In summary, we present a rare case of AD that is unusual in its cystic presentation and genital location. This is thought, by the authors, to be a unique presentation of a follicular adnexal neoplasm, lying on the spectrum of WD or follicular dyskeratoma.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Zeglaoui F, Zaraa I, Fazaa B, Houimli S, El Fekih N, Ezzine N, et al. Dyskeratosis follicularis disease: Case reports and review of the literature. J EurAcadDermatolVenereol. 2005;19:114–7. doi: 10.1111/j.1468-3083.2004.01096.x. [DOI] [PubMed] [Google Scholar]
- 2.Fernández-Figueras MT, Puig L, Cannata P, Cuatrecases M, Quer A, Ferrándiz C, et al. Grover disease: A reappraisal of histopathological diagnostic criteria in 120 cases. Am J Dermatopathol. 2010;32:541–9. doi: 10.1097/DAD.0b013e3181c80cf9. [DOI] [PubMed] [Google Scholar]
- 3.Kaddu S, Dong H, Mayer G, Kerl H, Cerroni L. Warty dyskeratoma--” follicular dyskeratoma”: Analysis of clinicopathologic features of a distinctive follicular adnexal neoplasm. J Am AcadDermatol. 2002;47:423–8. doi: 10.1067/mjd.2002.122756. [DOI] [PubMed] [Google Scholar]
- 4.Gorlin RJ, Peterson WC., Jr Warty dyskeratoma. A note concerning its occurrence in the oral mucosa. Arch Dermatol. 1967;95:292–3. doi: 10.1001/archderm.95.3.292. [DOI] [PubMed] [Google Scholar]
- 5.Pincus H, Mehregan AH. Guide to Dermatohistopathology. 2nd ed. New York: Appleton-Century-Crofts; 1976. p. 652. [Google Scholar]
- 6.Allon I, Buchner A. Warty dyskeratoma/focal acantholyticdyskeratosis—An update on a rare oral lesion. J Oral Pathol Med. 2012;41:261–7. doi: 10.1111/j.1600-0714.2011.01082.x. [DOI] [PubMed] [Google Scholar]
- 7.Duray PH, Merino MJ, Axiotis C. Warty dyskeratoma of the vulva. Int J GynecolPathol. 1983;2:286–93. doi: 10.1097/00004347-198303000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Lora V, Scarabello A, Cota C. Warty dyskeratoma as a cutaneous horn of the mons pubis. Am J Dermatopathol. 2015;37:802–4. doi: 10.1097/DAD.0000000000000262. [DOI] [PubMed] [Google Scholar]
- 9.Sáenz AM, Cirocco A, Avendaño M, González F, Sardi JR. Papularacantholyticdyskeratosis of the vulva. PediatrDermatol. 2005;22:237–9. doi: 10.1111/j.1525-1470.2005.22312.x. [DOI] [PubMed] [Google Scholar]
- 10.Cooper PH. Acantholyticdermatosis localized to the vulvocrural area. J CutanPathol. 1989;16:81–4. doi: 10.1111/j.1600-0560.1989.tb00015.x. [DOI] [PubMed] [Google Scholar]
- 11.Ko CJ, Barr RJ, Subtil A, McNiff JM. Acantholyticdyskeratoticacanthoma: A variant of a benign keratosis. J CutanPathol. 2008;35:298–301. doi: 10.1111/j.1600-0560.2007.00799.x. [DOI] [PubMed] [Google Scholar]
- 12.Diallo M, Cribier B, Scrivener Y. Warty dyskeratoma: Infundibularhistogenesis. Anatomoclinical study of 43 cases. Ann DermatolVenereol. 2007;134:633–6. doi: 10.1016/s0151-9638(07)91823-2. [DOI] [PubMed] [Google Scholar]
- 13.Matthews D, Perera LP, Irion LD, Carley F. Darier disease: Beware the cyst that smells. OphthalPlastReconstrSurg. 2010;26:207–7. doi: 10.1097/IOP.0b013e3181b8dd86. [DOI] [PubMed] [Google Scholar]
- 14.Dutta M, Kundu S, Ghosh B. Cystic squamous cell carcinoma of the neck: Could a second metastatic focus help? Otolaryngol Pol. 2014;68:338–41. doi: 10.1016/j.otpol.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 15.Skelton HG, Flax S, Chang L, Smith KJ. Squamous cell carcinoma arising from adnexal ductal cysts. Arch Pathol Lab Med. 2002;126:76–8. doi: 10.5858/2002-126-0076-SCCAFA. [DOI] [PubMed] [Google Scholar]
- 16.Lachiewicz AM, Wilkinson TM, Groben P, Ollila DW, Thomas NE. Muir-Torre syndrome. Am J ClinDermatol. 2007;8:315–9. doi: 10.2165/00128071-200708050-00008. [DOI] [PubMed] [Google Scholar]
- 17.Abramovits W, Abdelmalek N. Treatment of warty dyskeratoma with tazarotenic acid. J Am AcadDermatol. 2002;46(Suppl Case Reports):S4–17. doi: 10.1067/mjd.2002.104963. [DOI] [PubMed] [Google Scholar]


