Abstract
Cutaneous metastasis from visceral tumors is a rare entity with a reported incidence between 0.3% and 9.8%. These usually occur late in the course of the disease; the average time interval between the diagnosis of malignancy and presentation of cutaneous metastases has been reported to be 33 months. In rare instances (in about 0.8%–1.3% of patients), cutaneous metastases may be a pointer to an underlying undiagnosed malignancy. We report two patients presenting to us with soft, nodular, cutaneous lesions, which was the manifestation of metastatic signet cell carcinoma arising from the gut. We report these cases owing to their rarity.
Keywords: Cutaneous metastases, gastric carcinoma, signet ring cell carcinoma
INTRODUCTION
Cutaneous metastases from visceral tumors account for 2% of all cutaneous malignancies. Cutaneous metastases are usually a harbinger of advanced progression of the malignancy. Although cutaneous metastases usually occur late in the course of a malignancy, in rare instances, they may be a pointer to an underlying yet undiagnosed malignancy. We report the clinical diagnostic sequence of two patients who were diagnosed to have cutaneous metastatic lesions before the detection of carcinoma of the gut.
CASE REPORTS
Case report 1
A 35-year-old woman presented with rapidly progressing, asymptomatic skin lesions on the chest followed by similar nodules over the occipital and left parietal area of her scalp. She had a significant loss of weight of 6 kg over the last 6 months. General examination revealed a firm left supraclavicular lymph node. Cutaneous examination revealed the presence of multiple tender nodules with a soft, rubbery consistency with overlying superficial telangiectasia scattered on the scalp [Figure 1], face [Figure 2], upper chest [Figure 3], and lower back, varying in size from 0.5 cm × 0.5 cm to 2 cm × 2 cm.
Figure 1.

Nodule on the scalp
Figure 2.

Nodule on the forehead
Figure 3.

Nodule on the upper chest
The differential diagnoses considered based on her clinical presentation were cutaneous lymphoma, cutaneous metastases, and histiocytosis. Her blood investigations were within normal limits. A skin biopsy from one of the nodules showed hyperkeratosis with prominence of the granular layer. The dermis was infiltrated by a tumor composed predominantly of loose clusters of round cells with eccentrically placed, hyperchromatic nuclei, and abundant amounts of cytoplasm containing neutral mucin [Figures 4–6]. On immunohistochemistry, the cells were pancytokeratin positive. A diagnosis of metastatic poorly differentiated signet cell carcinoma was made based on the histopathological findings. A gastroscopy-guided biopsy done from the gastric mucosa showed poorly differentiated signet cell-type adenocarcinoma. A computed tomography scan and positron emission tomography scan done showed thickening of the cecal wall and omentum with enlarged para-aortic lymph nodes. An explorative laparotomy was done, which showed an obstructive growth in the short segment of the ascending colon with extensive nodal involvement. She was diagnosed to have a synchronous adenocarcinoma of the stomach and cecum. A palliative ileotransverse anastomosis was done. She was started on chemotherapy. She however did not show any response to first-, second-, and third-line of chemotherapeutic drugs. After 6 months of being on chemotherapy, her skin nodules were found to be increasing in size. A simultaneous computed tomography scan showed disease progression. She succumbed to her disease a year after diagnosis.
Figure 4.

Biopsy from the nodule on the chest showing tumor mass in the dermis (H and E, ×10)
Figure 6.

Signet ring cells with intracytoplasmic periodic acid-Schiff positive mucin (periodic acid-Schiff, ×40)
Figure 5.
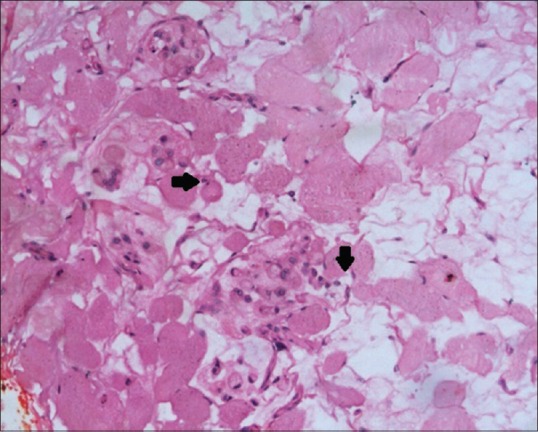
Loose clusters of round cells with eccentrically placed, hyperchromatic nuclei, and abundant amounts of cytoplasmic signet ring cells (arrows) (H and E, ×40)
Case report 2
A 33-year-old man presented with multiple, asymptomatic, gradually progressive swellings on the body for 4 months. He had recurrent episodes of epigastric burning and pain associated with passage of black, tarry stools for 4 months. He had lost about 4 kg in the last 1 year. General examination revealed pallor with an enlarged, firm left supraclavicular lymph node. Cutaneous examination revealed the presence of multiple soft, skin-colored and dull erythematous papules and nodules scattered on the face, trunk [Figure 7], and extremities [Figure 8]. The clinical differentials considered were cutaneous lymphomas, progressive nodular histiocytosis, and cutaneous metastases. Blood investigations showed anemia (hemoglobin: 5.3 g/dL) with microcytosis and anisocytosis. An ultrasonography done showed a mild thickening of the lesser curvature of the stomach. Gastroscopy showed an ulcer with irregular margins on the lesser curvature of the stomach from which a biopsy was taken. The skin biopsy was consistent with poorly differentiated metastatic adenocarcinoma (signet ring type). The biopsy from the gastric mucosa also showed signet ring cell carcinoma of the stomach.
Figure 7.

Nodules on the back
Figure 8.

Nodule on the left forearm
Palliative treatment with cisplatin was planned; however, he was lost to follow-up.
DISCUSSION
Cutaneous metastasis from visceral tumors is a rare entity with a reported incidence between 0.3% and 9.8%.[1] Cutaneous metastases of visceral malignancies usually occur late in the course of the disease, the average time interval between the diagnosis of malignancy and presentation of cutaneous metastases has been reported to be 33 months.[2] In rare instances (in about 0.8%–1.3% of patients), cutaneous metastases may be a pointer to an underlying undiagnosed malignancy.[2,3,4] Brownstein and Helwig had found that malignancies arising from the lung, kidney, and ovary are the most common type of cancers, which present with skin involvement as the first manifestation of the disease.[5] The clinical presentation of cutaneous metastases of visceral malignancies was classified by Brownstein and Helwig into nodular, inflammatory, fibrotic, and sclerodermoid types.[5] The other lesions that have been described in literature include indurated or infiltrated nodules, indurated plaques, papulosquamous lesions, bullae, ulcers, erysipelas-like erythema (carcinoma erysipeloides), large indurated plaques resembling a coat of armor (carcinoma en cuirasse), scarring alopecia (alopecia neoplastica), and zosteriform pattern of metastases.[6,7] The evolution of these skin lesions have been shown to correlate with the disease progression as in our first patient.[3]
Cutaneous metastases from gastrointestinal carcinoma commonly presents as solitary or multiple nodules, which are characteristically described as being firm in consistency. There is a single case report of metastatic nodules from a signet ring type of synchronous gastric, duodenal, and cecal carcinoma being described as soft nodules, as in one of our patients.[8] There are other reports of metastatic signet ring cell carcinoma of the gut presenting as firm nodules, indurated plaques, vegetative lesions, and carcinoma erysipeloides.[9,10] The typical site of location of metastatic lesions from the gastrointestinal tract is on the anterior abdominal wall.[3] Palpable, nodular lesions bulging into the umbilicus have been called “Sister Mary Joseph” nodules. Lesions have, however, been reported to appear on the head and neck area, axilla, chest, and the finger tip.[4] Both our patients had multiple lesions involving the scalp, face, upper chest, and lower back, which may be due to hematogenous spread of the tumor. The presence of cutaneous metastases indicates an advanced stage of the malignancy. There have been reports of these lesions responding to systemic or local chemotherapy, surgical excision, and/or radiotherapy. The size and number of lesions provide an easily accessible tool during follow-up visits for assessing the response of the tumor to treatment.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Mueller TJ, Wu H, Greenberg RE, Hudes G, Topham N, Lessin SR, et al. Cutaneous metastases from genitourinary malignancies. Urology. 2004;63:1021–6. doi: 10.1016/j.urology.2004.01.014. [DOI] [PubMed] [Google Scholar]
- 2.Saeed S, Keehn CA, Morgan MB. Cutaneous metastasis: A clinical, pathological, and immunohistochemical appraisal. J Cutan Pathol. 2004;31:419–30. doi: 10.1111/j.0303-6987.2004.00207.x. [DOI] [PubMed] [Google Scholar]
- 3.Nashan D, Müller ML, Braun-Falco M, Reichenberger S, Szeimies RM, Bruckner-Tuderman L. Cutaneous metastases of visceral tumours: A review. J Cancer Res Clin Oncol. 2009;135:1–14. doi: 10.1007/s00432-008-0432-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lookingbill DP, Spangler N, Helm KF. Cutaneous metastases in patients with metastatic carcinoma: A retrospective study of 4020 patients. J Am Acad Dermatol. 1993;29(2 Pt 1):228–36. doi: 10.1016/0190-9622(93)70173-q. [DOI] [PubMed] [Google Scholar]
- 5.Brownstein MH, Helwig EB. Patterns of cutaneous metastasis. Arch Dermatol. 1972;105:862–8. [PubMed] [Google Scholar]
- 6.Lifshitz OH, Berlin JM, Taylor JS, Bergfeld WF. Metastatic gastric adenocarcinoma presenting as an enlarging plaque on the scalp. Cutis. 2005;76:194–6. [PubMed] [Google Scholar]
- 7.Aneiros-Fernandez J, Husein-ElAhmed H, Arias-Santiago S, Escobar Gómez-Villalva F, Nicolae A, O'Valle Ravassa F, et al. Cutaneous metastasis as first clinical manifestation of signet ring cell gastric carcinoma. Dermatol Online J. 2010;16:9. [PubMed] [Google Scholar]
- 8.Ismaili Z, Dekhay S, Moussaoui A, Jahid A. Primary gastric, duodenal, and rectal signet ring cell carcinoma revealed by cutaneous metastasis. Endoscopy. 2011;43(Suppl 2):E209–10. doi: 10.1055/s-0030-1256399. [DOI] [PubMed] [Google Scholar]
- 9.Acikalin MF, Vardareli E, Tel N, Saricam T, Urer S. Erysipelas-like cutaneous metastasis from gastric signet ring cell carcinoma. J Eur Acad Dermatol Venereol. 2005;19:642–3. doi: 10.1111/j.1468-3083.2005.01214.x. [DOI] [PubMed] [Google Scholar]
- 10.Müller CS, Pföhler C, Reichrath J, Tilgen W. Gastric signet ring cell carcinoma presenting. An erysipelas-like cutaneous metastasis of the abdominal skin. Hautarzt. 2008;59:992–4. doi: 10.1007/s00105-008-1541-z. [DOI] [PubMed] [Google Scholar]


