Sir,
Postherpetic neuralgia (PHN) is the most common complication of herpes zoster (HZ), affecting approximately 50% of patients older than 60 years and 15% of all HZ patients.[1] Most of these patients complain of pain; which has been studied extensively. Itch is relatively under-reported and therefore, often, a neglected component of PHN. We, therefore, conducted a study on 100 consecutive patients of PHN to determine the burden of postherpetic pruritus (PHP) among them. We defined PHN as pain and/or pruritus persisting 1 month after the onset of zoster rash. Severity of pruritus was assessed on the visual analog scale and rated as mild (1-3), moderate (4-7), and severe (8-10).
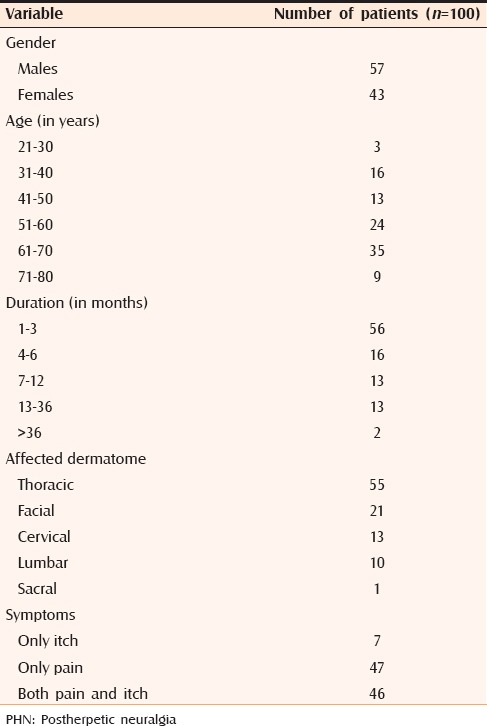
The study included 57 males and 43 females. Maximum number of patients belonged to the age group of 61–70 years. The mean duration of PHN was 7.7 months. The longest duration recorded was 7 years in one patient. Interestingly, this patient had only pruritus. Fifty-three out of 100 (53%) patients experienced PHP, of which 54.71%, 28.30%, and 16.94% cases had mild, moderate, and severe pruritus, respectively. Seven cases had only pruritus, whereas the rest had both pain and pruritus [Table 1]. It was noted that a higher proportion of patients with facial zoster had itching, seen in 15 out of 21 (71.4%) patients. Sixteen out of 53 (30.18%) patients also reported associated alloknesis.
Table 1.
Clinicoepidemiological features of patients with PHN
In different studies done on PHN, prevalence of PHP varies from 7% to 58%.[2] It is not surprising to see pruritus as a component of PHN because pain and itch are closely related. Itching accompanies pain in several disease states including HZ in its acute phase as well as in PHN. Histological studies of patients with acute HZ and PHN have revealed that cutaneous innervation density is decreased in the affected region[3] and the overall reduction appears more severe in patients who develop PHN. This might leave the affected dermatome relatively enriched in itch fibers extending from adjacent spared dermatomes, thus resulting in neuropathic itch.[2]
In our series, 54.71% of patients had mild itching, whereas 16.94% had severe itching. Severe itch can sometimes have devastating consequences. One of the classical examples include a patient with intractable PHP of the V1 dermatome who gradually and unintentionally went on scratching. This intractable painless scratching was probably a result of profound cutaneous denervation due to HZ, which resulted in loss of protective pain sensation. Severe scratching resulted in skull bone defect, subsequently leading to epidural abscess, hemiparesis, seizures, and personality changes due to frontal lobe injury.[4,5]
In conclusion, we experienced that a significant proportion of patients with PHN also suffer from itching, which is more likely in case of facial HZ. Most of these patients are fortunate enough to have mild-to-moderate itch, but few may have severe, disabling itch. Therefore, pruritus must be given adequate focus while managing a case of PHN. One must also remember that pain and itch may have to be treated differently, for example, opioids relieve neuropathic pain, but can cause or worsen itch.[5]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Niv D, Maltsman-Tseikhin A. Postherpetic neuralgia: The never-ending challenge. Pain Pract. 2005;5:327–40. doi: 10.1111/j.1533-2500.2005.00035.x. [DOI] [PubMed] [Google Scholar]
- 2.Oaklander AL, Bowsher D, Galer B, Haanpää M, Jensen MP. Herpes zoster itch: Preliminary epidemiologic data. J Pain. 2003;4:338–43. doi: 10.1016/s1526-5900(03)00637-0. [DOI] [PubMed] [Google Scholar]
- 3.Zografakis C, Tiniakos DG, Palaiologou M, Kouloukoussa M, Kittas C, Staurianeas N. Increased density of cutaneous nerve fibres in the affected dermatomes after herpes zoster therapy. Acta Derm Venereol. 2014;94:168–72. doi: 10.2340/00015555-1664. [DOI] [PubMed] [Google Scholar]
- 4.Oaklander AL, Cohen SP, Raju SV. Intractable postherpetic itch and cutaneous deafferentation after facial shingles. Pain. 2002;96:9–12. doi: 10.1016/s0304-3959(01)00400-6. [DOI] [PubMed] [Google Scholar]
- 5.Oaklander AL. Common neuropathic itch syndromes. Acta Derm Venereol. 2012;92:118–25. doi: 10.2340/00015555-1318. [DOI] [PubMed] [Google Scholar]


