Abstract
Systematic review of literature was made to assess the extent of accuracy of cone beam computed tomography (CBCT) as a tool for measurement of alveolar bone loss in periodontal defect. A systematic search of PubMed electronic database and a hand search of open access journals (from 2000 to 2015) yielded abstracts that were potentially relevant. The original articles were then retrieved and their references were hand searched for possible missing articles. Only articles that met the selection criteria were included and criticized. The initial screening revealed 47 potentially relevant articles, of which only 14 have met the selection criteria; their CBCT average measurements error ranged from 0.19 mm to 1.27 mm; however, no valid meta-analysis could be made due to the high heterogeneity between the included studies. Under the limitation of the number and strength of the available studies, we concluded that CBCT provides an assessment of alveolar bone loss in periodontal defect with a minimum reported mean measurements error of 0.19 ± 0.11 mm and a maximum reported mean measurements error of 1.27 ± 1.43 mm, and there is no agreement between the studies regarding the direction of the deviation whether over or underestimation. However, we should emphasize that the evidence to this data is not strong.
Key words: Accuracy, alveolar bone loss, cone beam computed tomography, review
INTRODUCTION
Alveolar bone loss in periodontal defects is a common dental problem. Accurate assessment of the true extension of the periodontal defect is essential for proper formulation of a suitable treatment plan; dental radiographs are a valuable noninvasive tool used as an adjunct to clinical examination for assessment of the periodontal conditions of the teeth.[1]
Periapical and bitewing radiographs are the most commonly used radiographic techniques in assessment of the periodontium of the teeth; however, unfortunately, these techniques provide two-dimensional (2D) images lacking any information about the third dimension which hinders a true distinction between buccal and lingual cortical plates and complicates the evaluation of the periodontal defects.[2,3]
Due to this drawback, there was a need for a more accurate imaging technique to be used in assessment of periodontal conditions, with special regards to the imaging of the three-dimensional (3D) structures such as infra-bony defects, buccal and lingual cortical plates, and furcation involvement. All that drew the attention to the use of computed tomography (CT) in diagnosing periodontal problems, and it yielded good results, but unfortunately, other important factors such as cost, accessibility, and radiation dose prevent its routine use in dental clinics.[4,5]
Cone beam CT (CBCT) has recently emerged in the dental field providing another 3D alternative to medical CT. It has the great advantage of a much more reduced radiation dose which favors its use for dental and maxillofacial structures imaging, and it also provides variable fields of view; therefore, an optimum field of view (FOV) can be selected for each patient based on the task, for which CBCT is used and the region of interest. Moreover, it provides a submillimeter isotropic voxel resolution which allow the nonorthogonal sectioning of the obtained data sets, for that it can be used as a supplementary imaging technique insituations where traditional 2D techniques are unable to provide sufficient reliable information for periodontal assessment and treatment.[6]
To our knowledge, there have been only four review articles (and not systematic reviews) discussing the role of CBCT in diagnosis of periodontal diseases. The first was performed by Mohan et al., and it discussed the principles and evolution of CBCT, the differences between it and medical CT, and its advantages and limitations, and finally, its application as a diagnostic tool in periodontology and implant site assessment. They concluded that “the merits of CBCT made it as a natural fit in periodontal imaging.”[7]
Furthermore, du Bois et al. have reviewed the imaging modalities used in diagnosis of periodontal problems including conventional and digital periapical radiographs with their limitations, panoramic radiographs, conventional CT, and finally, CBCT. They also discussed the use of CBCT in assessment of periodontal defects, furcation involvement, and periodontal regeneration, and they noted that “unless there is a sound clinical indication, CBCT should not be routinely used for assessment of periodontal problems.”[8]
Aljehani has reviewed the use of CBCT in periodontal diseases diagnosis. He addressed its use in: (1) Diagnosing furcation involvement, craters, and bony defects, (2) measuring periodontal bone levels, (3) visualization of periodontal ligament space, and (4) other periodontal applications such as detection of apical periodontitis and periapical pathology. He concluded that “the CBCT does not offer a significant advantage over conventional radiography in assessment of alveolar bone loss.”[9]
Acar and Kamburoglu have discussed the CBCT merits and limitations and its role in diagnosing periodontal conditions such as furcation involvement, periodontal ligament space, alveolar bone defects, soft-tissue assessment, and outcomes of regenerative periodontal therapy and bone graft. Finally, they concluded that “CBCT has obvious benefits in periodontology, but its use should be kept only when necessary to avoid radiation hazards.”[10]
The question of this research is how much accuracy could be provided by CBCT in measurements of alveolar bone loss in periodontal defects?
MATERIALS AND METHODS
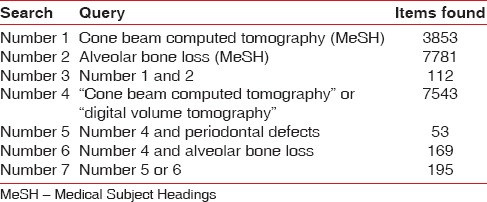
PubMed database was searched (from 2000 to 2015) to find potentially relevant articles for this review. On searching, we used two methods; the first by utilizing Medical Subject Headings search, in which we used the terms “cone beam computed tomography” and “alveolar bone loss,” and the second method by using the standard keywords (“cone beam computed tomography” or “CBCT” or “digital volume tomography”') and “alveolar bone loss” or “periodontal defects,” and then the results from the first and second search methods were combined and duplicates removed. Hand search of open access journals resulted in addition of two more articles: One from the Egyptian Journal of Oral and Maxillofacial Surgery and the other from the Egyptian Dental Journal [Table 1]. The last electronic search was made on April 14th2015.
Table 1.
The search strategy developed using PubMed database
The potentially relevant articles that were found using aforementioned search strategy were first screened by titles and irrelevant titles were excluded, then the remaining articles were considered for abstract evaluation based on the following inclusion criteria:
(1) The study should be a primary article not a review. (2) It should examine the CBCT accuracy in measuring the amount of alveolar bone loss in the periodontal defect by comparing CBCT measurements with the gold standard (GS) measurements of the defects (whether they were naturally occurring or artificially made). (3) Clinical studies and in vitro studies are included. (4) The study should examine accuracy of CBCT in assessment of periodontal not peri-implant defects as implants could affect the accuracy of measurements by introducing some sort of artifact due to its metallic nature, and that may affect the results and need to be examined as a separate problem.[11](5) The study should be in English.
If the title and abstract of an article did not provide sufficient information regarding the inclusion criteria to make a decision, the full text was obtained and examined. Further hand search was made including the bibliographies of all articles selected for full-text screening but it was not yielding.
For assessing the risk of bias both at study level and at outcome level and to ascertain the validity of the individual studies to be included in this review, we have used a checklist for assessing a diagnostic or predictive test developed by Leake[12] after modification. This was performed by two reviewers independently; finally, disagreements were resolved by discussion between the two reviewers; if no agreement could be reached, it was planned that a third author would decide. The following are the questions included in the checklist:
Was there a clear question for the study to address?
Did the study include different common presentations of the target disorder?
Were the exclusion and inclusion criteria mentioned?
Was the sample size sufficient?
Was the test clearly described?
Did the test report the technical parameters that may influence the results?
Was the test evaluated in a valid clinical setting?
Was the test measured against a valid GS?
Were the people assessing the results of the index diagnostic test blinded to the results of the reference standard?
Did the study describe the number and/or training and expertise of the persons executing and reading the index tests and the reference standard?
Did the results of the study clearly present the method error (minimally the mean and standard deviation values) of the index test compared to the GS?
RESULTS
The results of this search strategy are summarized in a flow diagram [Figure 1]. An electronic literature search revealed 195 articles from the PubMed database, of which 150 articles were excluded at the title stage and the remaining 45 studies full articles together with two articles obtained from hand searching were examined for the presence of the inclusion criteria. Only 14 articles were found fulfilling all the inclusion criteria and were included in the present analysis; they were published in a period ranging from 2005 to 2015.
Figure 1.
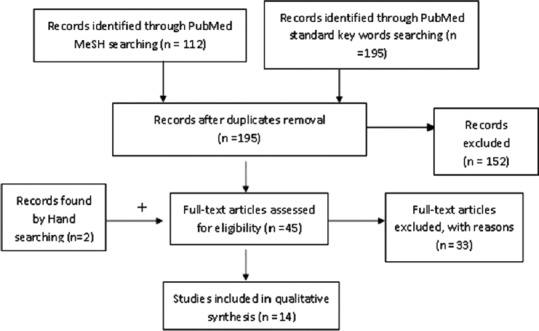
A flow diagram for the search strategy results
Meanwhile, 33 articles were excluded for missing one or more of the inclusion criteria as four articles were not primary articles,[7,8,9,10] three studies were in Chinese language,[13,14,15] eight studies were assessing peri-implant not periodontal defects,[16,17,18,19,20,21,22,23] sixteen studies were excluded because there was no comparison between CBCT and GS measurements of the defects,[23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39] and one study was excluded because the measurements were not made on periodontal defects but alveolar bone from alveolar crest (AC) to a marker anywhere on the alveolar bone.[40]
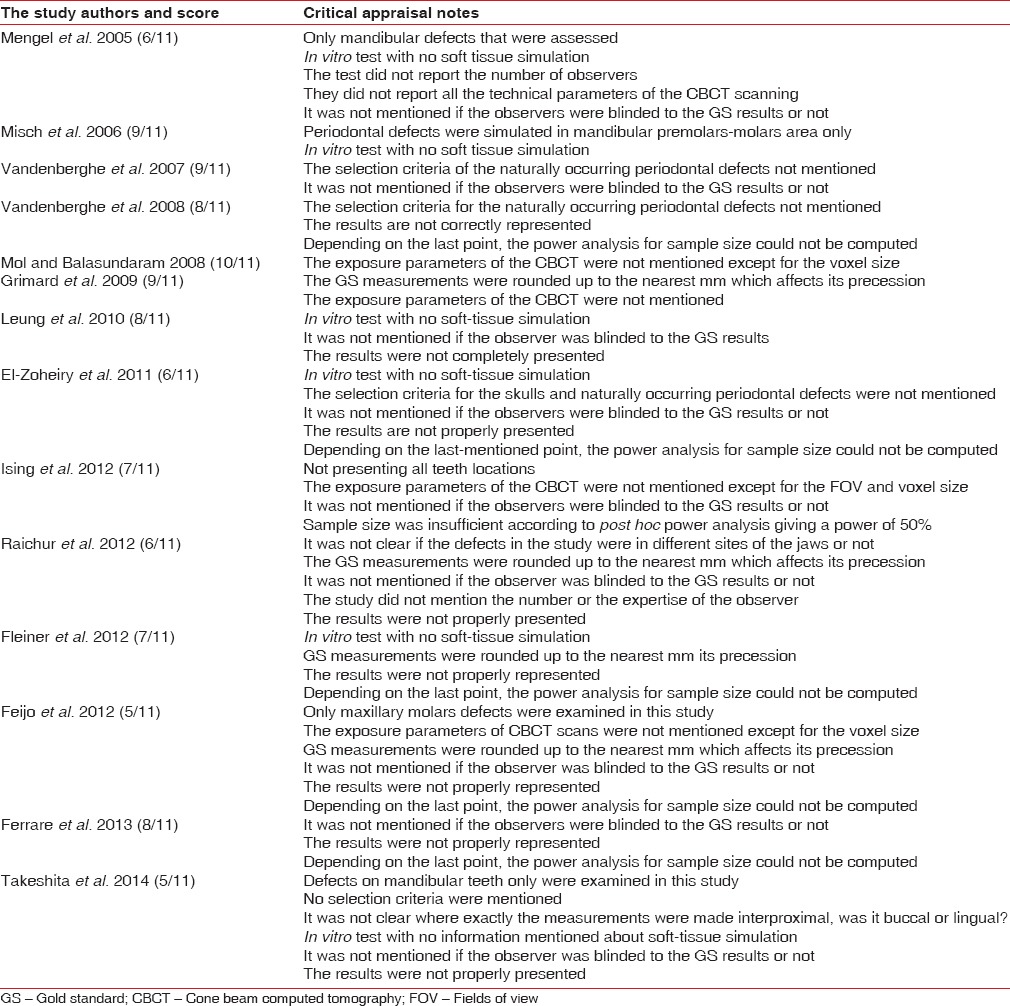
The data extraction from the 14 included studies were made [Table 2]. Then, these studies were criticized for risk of bias assessment and scored using the previously mentioned checklist [Table 3]. We have to mention that on appraising the sample size of the studies, if it was not determined and justified by a prior power analysis, we did a post hoc power analysis based on the primary outcome to evaluate it. Finally, the results of the criticism revealed that only two studies scored <l%, for that it was planned to include these studies only in the qualitative analysis while when it comes to the meta-analysis, they should be excluded to avoid bias in the results; however, at the end, we found that no meta-analysis for the collected data could be made due to the lack of complete and detailed statistical presentation of the deviation of the CBCT measurements from GS in most of the articles [Table 3].
Table 2.
Summary of the findings of the articles included in the study

Table 3.
Checklist scoring and critical appraisal notes of the included articles
On analyzing the data pooled from the studies included in this review, we have seen that they addressed the accuracy of CBCT in assessment of different types of periodontal defects as the study by Grimard et al. was made on vertical periodontal defects,[41] where the measurements were taken once at the initial surgery and once at the reentry surgery while Feijo et al. made their study on horizontal periodontal defects.[42]
Three studies have used CBCT in assessment of dehiscence, first of which was by Mengel et al. who assessed both the height and width of the dehiscence and they found that the average deviation from the “GS” measurements of the height of the dehiscence was 0.28 ± 0.20 mm, and for width it was 0.21 ± 0.15 mm.[43] Further, Ising et al. have assessed the height of the dehiscence defects,[44] whereas Leung et al. did not make any measurements on the dehiscence; they only reported the specificity and sensitivity of CBCT in detecting it with no measurements.[45]
In assessment of fenestration, two studies were found; the first was by Mengel et al. who found that the average deviation from the GS measurements of the height of the fenestration was 0.29 ± 0.21 mm, and for width, it was 0.05 ± 0.03[43] while the second was by Leung et al., but they did not report in their article the amount of deviation of CBCT measurements of fenestration from the GS.[45]
Vandenberghe et al. addressed the accuracy of CBCT in assessment of bony and/or infra-bony craters; they also examined the accuracy of CBCT in classifying furcation involvement and the topography of the craters.[46] Meanwhile, eight studies did not determine the type of the defects they assessed and only reported that they assessed the height of the defects whether naturally present or artificially made from the cementoenamel junction (CEJ) to the AC.[47,48,49,50,51,52,53,54]
There was no agreement between the included studies in the direction of the deviation (whether over or under estimation) as five studies reported that there was more tendency for underestimation; of them, three studies did not mention the percentage of which[41,45,49] while the other two studies did as Vandenberghe et al. reported a 53% underestimation[46] while El Zoheiry et al. reported 89% and 97% underestimation depending on the type of CBCT images used.[50] However, two studies reported a higher tendency for overestimation as Vandenberghe et al. reported a 52% and 63% overestimation depending on the type of CBCT images used[48] while Misch et al. did not mention the percentage of overestimation.[47] We can see that the same group of researchers who made two different studies in the same field has attained inconsistent results regarding the direction of the deviation. However, the remaining included seven studies ignored reporting the direction of the deviation.
DISCUSSION
In trying to find an answer for our research question, we found that the mean CBCT measurements error in the included studies ranged from 0.19 ± 0.11 mm.[43] to 1.27 ± 1.43 mm,[49] with the later exceeding the 0.5 mm value which is considered the clinically acceptable discrepancy in measurements.[2,3]
However, in the included studies, we tried to highlight, analyze, and compare the factors which were considered variables that may have an impact on the CBCT accuracy in assessment of periodontal defects, and we found that the reported accuracy of CBCT measurements is definitely dependent on the accuracy of the GS measurements as lack of accuracy in the GS will generate a bias in the results. We considered that for the GS to be valid, it should be recorded using a tool which provides measurements with submillimeter accuracy. Accordingly, we considered that GS recorded with a digital caliper directly on the defect in eight studies is a valid one.[44,45,46,47,48,49,50,54]
Moreover, two other different tools with submillimeter accuracy were used for GS measurements, the first was a reflecting stereomicroscope with measuring ocular tool and it was used by Mengel et al.;[43] the accuracy of this tool had been examined, especially for dental research purposes, and it was proved to be accurate with a high precession.[55,56] The second tool was micro-CT which was used by Ferrare et al.,[51] but being another imaging modality, it has its own error and deviation from the real measurements, as when examined by Kim et al., they found an error of 0.22 ± 0.635 mm.[57]
Meanwhile, the remaining four studies have utilized the manual periodontal probe with an accuracy of 1 mm to assess the GS measurements of the periodontal defects which were rounded up to the nearest millimeter.[41,42,52,53] The usage of both micro-CT and manual periodontal probe as a tool for GS measurements could introduce a bias in the results.
We also found that of the 14 selected studies, only three in vivo studies were found,[41,42,52] of them only the first one was a randomized clinical trial. While the greatest number of the studies was in vitro ones that were done in a more controlled environment under almost idealized conditions. For instance five studies of them used dry skulls and mandibles with no soft tissue simulation,[45,47,50,51,53] and eight studies utilized radio-opaque markers (Gutta-percha fragments or metallic balls) to facilitate identification of the CEJ.[43,44,46,47,48,49,50,54] And these could not be considered as valid clinical settings, for-that the reproducibility of the results of these studies is questionable and need to be assessed in vivo adequately, which could represent an inherent weakness of evidence.
Another factor that could have an impact on the accuracy of CBCT in measurements of periodontal defects is the tooth location, and we found two of the included studies were discussing this factor. The first was conducted by Mol and Balasundaram who found that the highest deviation from the GS measurements was at the lower anterior teeth with an average absolute error of 1.95 ± 1.89 mm which was significantly larger than for other teeth groups, whereas the lowest deviation was at the upper premolars teeth with an average absolute error of 0.91 ± 0.75 mm.[49]
The second study was by Ising et al. who found that the lowest average error was 0.33 mm for the incisors, and the highest average error was 0.74 mm for the premolars while for the canines, it was 0.62 mm; however, there was no statistically significant difference between them.[44] We can see that the results of the two studies are inconsistent; however, on revising the scoring and critical appraisal notes of both, we found that the sample size in the second study was not sufficient.
Not only the difference in tooth location but also the difference in surface location on the tooth could impact the reported accuracy of CBCT measurements as study by Feijo et al. compared the measurements error between mesial and distal aspects of the involved teeth; they were 0.75 ± 0.59 mm and 1.14 ± 0.88 mm, respectively, and the difference between them was not statistically significant (P = 0.063) while when they compared the measurements error between palatal and vestibular aspects for the same teeth, they found a statistically significant difference (P = 0.008) as the errors were 1.29 ± 1.04 mm and 0.58 ± 0.39 mm, respectively,[42] and that coincides with the results of Fleiner et al. who reported that there was a tendency toward better results of vestibular measurement sites compared to lingual or palatal sites.[53]
Three studies have been found comparing the accuracy of the CBCT measurements of the periodontal defects on different CBCT image types. The first was performed by Vandenberghe et al. who used panoramic reconstructed view with a default slice thickness of 5.2 mm and cross-sectional slices of 0.4 mm thickness, and the authors concluded that the cross-sectional images provide more accurate assessment of periodontal bone loss,[46] also El Zoheiry et al. utilized panoramic reconstructed view with slice thickness of 5.1 mm and cross-sectional slices of 0.32 mm, and they had the same conclusion as that of the previously mentioned study.[50]
Finally, Ising et al. compared the accuracy of CBCT measurements of periodontal defects on 3D surface rendering images and 2D multiplanar reformatted images and they found that the difference between them was not statistically significant; the authors concluded that both image types have a similar level of accuracy in assessment of periodontal dehiscence.[44]
Now after discussing the factors that were considered variables impacting the reported accuracy of CBCT in measurements of alveolar bone level, and on trial to link our search results with the clinical situations, we have to clarify the nonmentioned aspects about CBCT. As despite of its great merits, CBCT still suffer from some limitations; the most important one is the higher radiation dose it provides compared to the other radiographic techniques such as digital and conventional periapical and panoramic radiographs used in alveolar bone loss measurements.[6,58]
The effective dose from single intraoral radiography ranged from one to 20 µSv depending on the film/digital sensors used, collimation, focus skin distance, and tube voltage[59,60,61] while the effective doses reported in panoramic radiography were ranged from 4 to 30 µSv.[61,62] Whereas, for dental CBCT, the effective dose varied widely among the machines and depending on the size of the FOV used; however, when a limited FOV is used, the effective dose could be <l µSv.[58,60]
Depending on the previously mentioned facts and obeying as low as reasonably achievable concept, the CBCT should be the technique of choice only when it provide an important information that could not be supplied by other radiographic technique with a lower radiation dose, and this what was concluded by the previously made four review articles discussing role of CBCT in periodontology.[7,8,9,10] However, our review was a focused one aiming only to identify the degree of accuracy of CBCT in measurement of alveolar bone loss in periodontal defects. And answering this search question requires a valid meta-analysis for the data pooled from the studies discussing this point.
Unfortunately, many obstacles have been found on our trial to make a meta-analysis for the collected data, first of which is the statistical presentation of the results. As the descriptive analysis for numerical values such as method errors should include the minimum, maximum, mean, and standard deviation of the value, together with the precise P value,[63] and this was not present in most of the papers. In addition, almost one-half of included studies did not report whether their CBCT measurements errors were statistically significant or not, anyway the other half reported that they were not statistically significant.
Another great obstacle is the high heterogeneity between the studies which could be due to the difference between them in their purposes; hence, there were differences in the technical parameters used such as the voxel sizes of the scans, the type of the CBCT machine, and type of CBCT images used for measurements; there were also differences in the qualifications and the numbers of the observers who interpreted the radiographic data in the different studies. Another important point could be considered a source of heterogeneity is the inclusion of both in vivo and in vitro studies in our work due to the scarcity of articles discussing our search point.
Since no valid meta-analysis could be made, we could not reach a strong evidence-based answer for our search question. All we could reach is a wide range of the reported CBCT measurements error with its lower limit indicating very high accuracy of CBCT and encouraging its use when high precession in assessment of alveolar bone loss is needed, while the upper limit of this range indicating inadequate precession and accuracy based on what was considered by Mol 2004 and Brägger 2005 as a clinically acceptable discrepancy in measurements for alveolar bone loss assessment.
CONCLUSIONS
Under the limitation of the number and strength of the available studies, we can conclude that CBCT provides an assessment of alveolar bone loss in periodontal defect with a minimum reported mean measurements error of 0.19 ± 0.11 mm and maximum reported mean measurements error of 1.27 ± 1.43 mm, and there is no agreement between the studies regarding the direction of the deviation whether over- or under-estimation. However, we should emphasize that the evidence to this data is not strong. For that, we have no recommendation regarding the usefulness of CBCT in assessment of alveolar bone loss when high precession is needed, the only recommendations we have are that:
More clinical studies are required to establish the precession of the CBCT in assessment of alveolar bone loss in periodontal defects
The future studies should properly present their results with complete information on the minimum, maximum, mean, and standard deviation values of the measurement error and the precise P value, to facilitate the data pooling in a valid meta-analysis which could help other researchers to establish strong evidence.
Finally, we want to declare that there was no conflict of interest for any of the authors of this article.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Armitage GC. The complete periodontal examination. Periodontol 2000. 2004;34:22–33. doi: 10.1046/j.0906-6713.2002.003422.x. [DOI] [PubMed] [Google Scholar]
- 2.Brägger U. Radiographic parameters: Biological significance and clinical use. Periodontol 2000. 2005;39:73–90. doi: 10.1111/j.1600-0757.2005.00128.x. [DOI] [PubMed] [Google Scholar]
- 3.Mol A. Imaging methods in periodontology. Periodontol 2000. 2004;34:34–48. doi: 10.1046/j.0906-6713.2003.003423.x. [DOI] [PubMed] [Google Scholar]
- 4.Fuhrmann RA, Bücker A, Diedrich PR. Assessment of alveolar bone loss with high resolution computed tomography. J Periodontal Res. 1995;30:258–63. doi: 10.1111/j.1600-0765.1995.tb02131.x. [DOI] [PubMed] [Google Scholar]
- 5.Fuhrmann RA, Bücker A, Diedrich PR. Furcation involvement: Comparison of dental radiographs and HR-CT-slices in human specimens. J Periodontal Res. 1997;32:409–18. doi: 10.1111/j.1600-0765.1997.tb00553.x. [DOI] [PubMed] [Google Scholar]
- 6.Scarfe WC, Farman AG. What is cone-beam CT and how does it work? Dent Clin North Am. 2008;52:707–30, v. doi: 10.1016/j.cden.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 7.Mohan R, Singh A, Gundappa M. Three-dimensional imaging in periodontal diagnosis – Utilization of cone beam computed tomography. J Indian Soc Periodontol. 2011;15:11–7. doi: 10.4103/0972-124X.82256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.du Bois AH, Kardachi B, Bartold PM. Is there a role for the use of volumetric cone beam computed tomography in periodontics? Aust Dent J. 2012;57(Suppl 1):103–8. doi: 10.1111/j.1834-7819.2011.01659.x. [DOI] [PubMed] [Google Scholar]
- 9.Aljehani YA. Diagnostic applications of cone-beam CT for periodontal diseases. Int J Dent. 2014;2014:865079. doi: 10.1155/2014/865079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Acar B, Kamburoglu K. Use of cone beam computed tomography in periodontology. World J Radiol. 2014;6:139–47. doi: 10.4329/wjr.v6.i5.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Benic GI, Sancho-Puchades M, Jung RE, Deyhle H, Hämmerle CH. In vitro assessment of artifacts induced by titanium dental implants in cone beam computed tomography. Clin Oral Implants Res. 2013;24:378–83. doi: 10.1111/clr.12048. [DOI] [PubMed] [Google Scholar]
- 12.Leake JL. The Essentials. 3rd ed. Baltimore: Williams and Wilkins; 1996. [Last accessed on 2016 Jan 21]. Department of Biological and Diagnostic Sciences, Faculty of Dentistry, University of Toronto. “Unpublished Document”. Course Notes DENT 300Y; 2008. Fletcher RH, Fletcher SW, Wagner EH. Clinical Epidemiology. Sacket DL, Richardson SW, Rosenberg W, Haynes RB. Evidence-based Medicine: How to Practice and Tech. EBM. 2nd ed. New York: Churchill Livingston; 1997. Available from: https://www.dentistry.utoronto.ca/system/files/z2eblreport-2009.pdf. [Google Scholar]
- 13.Wang WF, Li ZH. Current research on alveolar bone dehiscences and fenestrations. Zhonghua Kou Qiang Yi Xue Za Zhi. 2013;48:570–2. [PubMed] [Google Scholar]
- 14.Zhao HJ, Wang HY, Pan YP. Evaluation of alveolar bone defect in chronic periodontitis by cone-beam computed tomography. Zhonghua Kou Qiang Yi Xue Za Zhi. 2013;48:7–11. [PubMed] [Google Scholar]
- 15.Deng Y, Wang C, Li T, Li A, Gou J. An application of cone-beam CT in the diagnosis of bone defects for chronic periodontitis. Zhonghua Kou Qiang Yi Xue Za Zhi. 2015;50:7–12. [PubMed] [Google Scholar]
- 16.Mengel R, Kruse B, Flores-de-Jacoby L. Digital volume tomography in the diagnosis of peri-implant defects: An in vitro study on native pig mandibles. J Periodontol. 2006;77:1234–41. doi: 10.1902/jop.2006.050424. [DOI] [PubMed] [Google Scholar]
- 17.Kehl M, Swierkot K, Mengel R. Three-dimensional measurement of bone loss at implants in patients with periodontal disease. J Periodontol. 2011;82:689–99. doi: 10.1902/jop.2010.100318. [DOI] [PubMed] [Google Scholar]
- 18.Corpas Ldos S, Jacobs R, Quirynen M, Huang Y, Naert I, Duyck J. Peri-implant bone tissue assessment by comparing the outcome of intra-oral radiograph and cone beam computed tomography analyses to the histological standard. Clin Oral Implants Res. 2011;22:492–9. doi: 10.1111/j.1600-0501.2010.02029.x. [DOI] [PubMed] [Google Scholar]
- 19.Fienitz T, Schwarz F, Ritter L, Dreiseidler T, Becker J, Rothamel D. Accuracy of cone beam computed tomography in assessing peri-implant bone defect regeneration: A histologically controlled study in dogs. Clin Oral Implants Res. 2012;23:882–7. doi: 10.1111/j.1600-0501.2011.02232.x. [DOI] [PubMed] [Google Scholar]
- 20.Vera C, De Kok IJ, Chen W, Reside G, Tyndall D, Cooper LF. Evaluation of post-implant buccal bone resorption using cone beam computed tomography: A clinical pilot study. Int J Oral Maxillofac Implants. 2012;27:1249–57. [PubMed] [Google Scholar]
- 21.Wang D, Künzel A, Golubovic V, Mihatovic I, John G, Chen Z, et al. Accuracy of peri-implant bone thickness and validity of assessing bone augmentation material using cone beam computed tomography. Clin Oral Investig. 2013;17:1601–9. doi: 10.1007/s00784-012-0841-y. [DOI] [PubMed] [Google Scholar]
- 22.Kamburoglu K, Murat S, Kiliç C, Yüksel S, Avsever H, Farman A, et al. Accuracy of CBCT images in the assessment of buccal marginal alveolar peri-implant defects: Effect of field of view. Dentomaxillofac Radiol. 2014;43:20130332. doi: 10.1259/dmfr.20130332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kaminaka A, Nakano T, Ono S, Kato T, Yatani H. Cone-beam computed tomography evaluation of horizontal and vertical dimensional changes in buccal peri-implant alveolar bone and soft tissue: A 1-year prospective clinical study. Clin Implant Dent Relat Res. 2015;17(Suppl 2):e576–85. doi: 10.1111/cid.12286. [DOI] [PubMed] [Google Scholar]
- 24.Naitoh M, Yamada S, Noguchi T, Ariji E, Nagao J, Mori K, et al. Three-dimensional display with quantitative analysis in alveolar bone resorption using cone-beam computerized tomography for dental use: A preliminary study. Int J Periodontics Restorative Dent. 2006;26:607–12. [PubMed] [Google Scholar]
- 25.Kasaj A, Willershausen B. Digital volume tomography for diagnostics in periodontology. Int J Comput Dent. 2007;10:155–68. [PubMed] [Google Scholar]
- 26.Noujeim M, Prihoda T, Langlais R, Nummikoski P. Evaluation of high-resolution cone beam computed tomography in the detection of simulated interradicular bone lesions. Dentomaxillofac Radiol. 2009;38:156–62. doi: 10.1259/dmfr/61676894. [DOI] [PubMed] [Google Scholar]
- 27.Gauthier C, Voyer R, Paquette M, Rompré P, Papadakis A. Periodontal effects of surgically assisted rapid palatal expansion evaluated clinically and with cone-beam computerized tomography: 6-month preliminary results. Am J Orthod Dentofacial Orthop. 2011;139(4 Suppl):S117–28. doi: 10.1016/j.ajodo.2010.06.022. [DOI] [PubMed] [Google Scholar]
- 28.Lund H, Gröndahl K, Gröndahl HG. Cone beam computed tomography evaluations of marginal alveolar bone before and after orthodontic treatment combined with premolar extractions. Eur J Oral Sci. 2012;120:201–11. doi: 10.1111/j.1600-0722.2012.00964.x. [DOI] [PubMed] [Google Scholar]
- 29.Chappuis V, Engel O, Reyes M, Shahim K, Nolte LP, Buser D. Ridge alterations post-extraction in the esthetic zone: A 3D analysis with CBCT. J Dent Res. 2013;92(12 Suppl):195S–201S. doi: 10.1177/0022034513506713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pangrazio-Kulbersh V, Jezdimir B, de Deus Haughey M, Kulbersh R, Wine P, Kaczynski R. CBCT assessment of alveolar buccal bone level after RME. Angle Orthod. 2013;83:110–6. doi: 10.2319/030712-198.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Brunetto M, Andriani Jda S, Ribeiro GL, Locks A, Correa M, Correa LR. Three-dimensional assessment of buccal alveolar bone after rapid and slow maxillary expansion: A clinical trial study. Am J Orthod Dentofacial Orthop. 2013;143:633–44. doi: 10.1016/j.ajodo.2012.12.008. [DOI] [PubMed] [Google Scholar]
- 32.Lombardo L, Bragazzi R, Perissinotto C, Mirabella D, Siciliani G. Cone-beam computed tomography evaluation of periodontal and bone support loss in extraction cases. Prog Orthod. 2013;14:29. doi: 10.1186/2196-1042-14-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kamburoglu K, Kolsuz E, Murat S, Eren H, Yüksel S, Paksoy CS. Assessment of buccal marginal alveolar peri-implant and periodontal defects using a cone beam CT system with and without the application of metal artefact reduction mode. Dentomaxillofac Radiol. 2013;42:20130176. doi: 10.1259/dmfr.20130176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Abdel-Rahim DF, Saleh HA, El-Ashiry SG. Diagnostic validity of cone beam computed tomography versus digital intraoral radiography for assessment of alveolar bone loss. Egypt Dent J. 2014;60:3389–99. [Google Scholar]
- 35.Ferreira PP, Torres M, Campos PS, Vogel CJ, de Araújo TM, Rebello IM. Evaluation of buccal bone coverage in the anterior region by cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2013;144:698–704. doi: 10.1016/j.ajodo.2013.07.010. [DOI] [PubMed] [Google Scholar]
- 36.Braun X, Ritter L, Jervøe-Storm PM, Frentzen M. Diagnostic accuracy of CBCT for periodontal lesions. Clin Oral Investig. 2014;18:1229–36. doi: 10.1007/s00784-013-1106-0. [DOI] [PubMed] [Google Scholar]
- 37.Songa VM, Jampani ND, Babu V, Buggapati L, Mittapally S. Accuracy of cone beam computed tomography in diagnosis and treatment planning of periodontal bone defects: A case report. J Clin Diagn Res. 2014;8:ZD23–5. doi: 10.7860/JCDR/2014/11165.5348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhao D, Zhang S, Chen X, Liu W, Sun N, Guo Y, et al. Evaluation of periodontitis and bone loss in patients undergoing hemodialysis. J Periodontol. 2014;85:1515–20. doi: 10.1902/jop.2014.140119. [DOI] [PubMed] [Google Scholar]
- 39.Zhao D, Chen X, Yue L, Liu W, Mo A, Yu H, et al. Assessment of residual alveolar bone volume in hemodialysis patients using CBCT. Clin Oral Investig. 2015;19:1619–24. doi: 10.1007/s00784-014-1393-0. [DOI] [PubMed] [Google Scholar]
- 40.Sun Z, Smith T, Kortam S, Kim DG, Tee BC, Fields H. Effect of bone thickness on alveolar bone-height measurements from cone-beam computed tomography images. Am J Orthod Dentofacial Orthop. 2011;139:e117–27. doi: 10.1016/j.ajodo.2010.08.016. [DOI] [PubMed] [Google Scholar]
- 41.Grimard BA, Hoidal MJ, Mills MP, Mellonig JT, Nummikoski PV, Mealey BL. Comparison of clinical, periapical radiograph, and cone-beam volume tomography measurement techniques for assessing bone level changes following regenerative periodontal therapy. J Periodontol. 2009;80:48–55. doi: 10.1902/jop.2009.080289. [DOI] [PubMed] [Google Scholar]
- 42.Feijo CV, Lucena JG, Kurita LM, Pereira SL. Evaluation of cone beam computed tomography in the detection of horizontal periodontal bone defects: An in vivo study. Int J Periodontics Restorative Dent. 2012;32:e162–8. [PubMed] [Google Scholar]
- 43.Mengel R, Candir M, Shiratori K, Flores-de-Jacoby L. Digital volume tomography in the diagnosis of periodontal defects: An in vitro study on native pig and human mandibles. J Periodontol. 2005;76:665–73. doi: 10.1902/jop.2005.76.5.665. [DOI] [PubMed] [Google Scholar]
- 44.Ising N, Kim KB, Araujo E, Buschang P. Evaluation of dehiscences using cone beam computed tomography. Angle Orthod. 2012;82:122–30. doi: 10.2319/020911-95.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Leung CC, Palomo L, Griffith R, Hans MG. Accuracy and reliability of cone-beam computed tomography for measuring alveolar bone height and detecting bony dehiscences and fenestrations. Am J Orthod Dentofacial Orthop. 2010;137(4 Suppl):S109–19. doi: 10.1016/j.ajodo.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 46.Vandenberghe B, Jacobs R, Yang J. Detection of periodontal bone loss using digital intraoral and cone beam computed tomography images: An in vitro assessment of bony and/or infrabony defects. Dentomaxillofac Radiol. 2008;37:252–60. doi: 10.1259/dmfr/57711133. [DOI] [PubMed] [Google Scholar]
- 47.Misch KA, Yi ES, Sarment DP. Accuracy of cone beam computed tomography for periodontal defect measurements. J Periodontol. 2006;77:1261–6. doi: 10.1902/jop.2006.050367. [DOI] [PubMed] [Google Scholar]
- 48.Vandenberghe B, Jacobs R, Yang J. Diagnostic validity (or acuity) of 2D CCD versus 3D CBCT-images for assessing periodontal breakdown. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:395–401. doi: 10.1016/j.tripleo.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 49.Mol A, Balasundaram A. In vitro cone beam computed tomography imaging of periodontal bone. Dentomaxillofac Radiol. 2008;37:319–24. doi: 10.1259/dmfr/26475758. [DOI] [PubMed] [Google Scholar]
- 50.El Zoheiry HS, Abou-Khalaf A, Farid MM. Assessment of periodontal defects using cone beam computed tomography. An in-vitro study. Egypt J Oral Maxillofac Surg. 2011;2:27–33. [Google Scholar]
- 51.Ferrare N, Leite AF, Caracas HC, de Azevedo RB, de Melo NS, de Souza Figueiredo PT. Cone-beam computed tomography and microtomography for alveolar bone measurements. Surg Radiol Anat. 2013;35:495–502. doi: 10.1007/s00276-013-1080-x. [DOI] [PubMed] [Google Scholar]
- 52.Raichur PS, Setty SB, Thakur SL, Naikmasur VG. Comparison of radiovisiography and digital volume tomography to direct surgical measurements in the detection of infrabony defects. J Clin Exp Dent. 2012;4:e43–7. doi: 10.4317/jced.50711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fleiner J, Hannig C, Schulze D, Stricker A, Jacobs R. Digital method for quantification of circumferential periodontal bone level using cone beam CT. Clin Oral Investig. 2013;17:389–96. doi: 10.1007/s00784-012-0715-3. [DOI] [PubMed] [Google Scholar]
- 54.Takeshita WM, Vessoni Iwaki LC, Da Silva MC, Tonin RH. Evaluation of diagnostic accuracy of conventional and digital periapical radiography, panoramic radiography, and cone-beam computed tomography in the assessment of alveolar bone loss. Contemp Clin Dent. 2014;5:318–23. doi: 10.4103/0976-237X.137930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.MacLarnon AM. Applications of the reflex instruments in quantitative morphology. Folia Primatol (Basel) 1989;53:33–49. doi: 10.1159/000156407. [DOI] [PubMed] [Google Scholar]
- 56.Speculand B, Butcher GW, Stephens CD. Three-dimensional measurement: The accuracy and precision of the reflex microscope. Br J Oral Maxillofac Surg. 1988;26:276–83. doi: 10.1016/0266-4356(88)90044-7. [DOI] [PubMed] [Google Scholar]
- 57.Kim I, Paik KS, Lee SP. Quantitative evaluation of the accuracy of micro-computed tomography in tooth measurement. Clin Anat. 2007;20:27–34. doi: 10.1002/ca.20265. [DOI] [PubMed] [Google Scholar]
- 58.Roberts JA, Drage NA, Davies J, Thomas DW. Effective dose from cone beam CT examinations in dentistry. Br J Radiol. 2009;82:35–40. doi: 10.1259/bjr/31419627. [DOI] [PubMed] [Google Scholar]
- 59.Gibbs SJ. Effective dose equivalent and effective dose: Comparison for common projections in oral and maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:538–45. doi: 10.1067/moe.2000.109189. [DOI] [PubMed] [Google Scholar]
- 60.Okano T, Sur J. Radiation dose and protection in dentistry (review article) Jpn Dent Sci Rev. 2010;46:112–21. [Google Scholar]
- 61.European Guidelines on Radiation Protection in Dental Radiology. Luxembourg: Office for Official Publications of the EC; 2004. [Last accessed on 2016 Jan 27]. European Commission. Radiation Protection 136. Available from: https://ec.europa.eu/energy/sites/ener/files/documents/136.pdf . [Google Scholar]
- 62.Danforth RA, Clark DE. Effective dose from radiation absorbed during a panoramic examination with a new generation machine. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:236–43. doi: 10.1067/moe.2000.103526. [DOI] [PubMed] [Google Scholar]
- 63.Hannigan A, Lynch CD. Statistical methodology in oral and dental research: Pitfalls and recommendations. J Dent. 2013;41:385–92. doi: 10.1016/j.jdent.2013.02.013. [DOI] [PubMed] [Google Scholar]


