Abstract
The role of periodontium in supporting the tooth structures is well-known. However, less is known about its contribution to the field of ophthalmology. Corneal diseases are among major causes of blindness affecting millions of people worldwide, for which synthetic keratoprosthesis was considered the last resort to restore vision. Yet, these synthetic keratoprosthesis suffered from serious limitations, especially the foreign body reactions invoked by them resulting in extrusion of the whole prosthesis from the eye. To overcome these shortcomings, an autologous osteo-odonto keratoprosthesis utilizing intraoral entities was introduced that could positively restore vision even in cases of severely damaged eyes. The successful functioning of this prosthesis, however, predominantly depended on the presence of a healthy periodontium for grafting. Therefore, the following short communication aims to acknowledge this lesser-known role of the periodontium and other oral structures in bestowing vision to the blind patients.
Key words: Eye surgery, ophthalmology, osteo-odonto keratoprosthesis, periodontal, tooth
INTRODUCTION
The regenerative potential of periodontium to fill up the alveolar bone defects and recession defects is well-known; yet, little has been documented in periodontics about its contribution to the field of ophthalmology. To restore vision to the patients whose corneas had been damaged, Strampelli in the early 1960s, introduced a complex two-stage corneal transplant technique employing osteo-odonto keratoprosthesis (OOKP), fabricated using oral entities,[1] which was then further modified by Falcinelli[2] Keratoprosthetic implant, a device that replaces damaged and opaque cornea, dates back more than 200 years to Pellier de Quengsy, a French ophthalmologist who proposed implanting a glass plate into an opaque cornea. Since then numerous attempts have been made to fabricate the ideal keratoprosthetic implant which would have an improved optical quality, with decreased aberrations and a specifiable power, excellent biointegration, resistant against infections, along with qualities similar to that of the cornea to last the lifetime of the patient. Though, the comparison between the various keratoprosthesis has been difficult since the published studies provide conflicting data and are often retrospective and uncontrolled, nonetheless, publications on OOKP provides the most extensive literature, with the most number of patients and the longest follow-up.[3] In this technique, autologous living human tissue, i.e., dentine, alveolar bone with its ligament and periosteum from an extracted tooth has to be auto-transplanted to replace the cornea. Though, autologous tissues are preferred, in certain cases OOKP allografts may be fashioned from a canine tooth donated by a human leukocyte antigen (HLA) matched living relative. In such cases, the patient is made aware of the higher risk of resorption of the lamina, and the need to be on lifelong immunosuppression even if the donor is HLA matched, to prevent graft rejection and prolong the life of the grafted OOKP lamina.[3]
OOKP Procedure – Indications, Contraindications & Complications
Patients indicated for OOKP surgery include those with bilateral corneal blindness resulting from severe end-stage Stevens–Johnson syndrome, ocular cicatricial pemphigoid, Lyell syndrome, chemical injury, physical injury, trachoma, loss of the lids, or multiple failed penetrating keratoplasty.[4] On the other hand, patients who are managing well with their level of vision, children under the age of 17, evidence of phthisis, eyes that have no perception of light, advanced glaucoma, or irreparable retinal detachment should be excluded.[3]
The first stage of the surgery, i.e., ocular surface reconstruction and fashioning of an osteo-odonto lamina and its optical cylinder involves covering the affected eye with the buccal mucosal membrane harvested from the oral cavity and subsequently fixing it to the conjunctiva with sutures after the globe of the eye has been prepared. This harvested buccal mucosa over a period of a couple of months acquires its own blood supply and forms a new ocular surface for receiving the OOKP. The first stage also includes fabrication of the osteo-odonto lamina wherein a single rooted tooth preferably maxillary canine along with its surrounding intact alveolar bone and periodontium is extracted, taking extreme caution to prevent any damage to the periosteum and periodontal ligament. Thereafter, it is carved and molded to prepare a plate which acts as a carrier for polymethyl methacrylate (PMMA) optical cylinder [Figure 1].[4] The resultant osteo-odonto lamina exposing dentine on one side and bone on the other along with the synthetic cylinder passing through it in the center is placed into a sub-muscular pocket under orbicularis oculi, usually in the lower lid of the fellow eye during the first stage surgery, in order to acquire a soft tissue covering.[5] The osteo-odonto lamina can also be inserted into the shoulder or the cheek. This last step is done so that the tooth-lens combination can grow tissue and form blood vessels.[6] Great care is taken while harvesting the grafts from the oral cavity to avoid any damage to the adjacent structures. Furthermore, after the graft has been procured the resultant alveolar defect is reconstructed following guided bone regeneration procedure. Thereafter, the second stage of the OOKP surgery which is performed 4–5 months after the first stage, fundamentally involves the retrieval of the osteo-odonto lamina from its sub-muscular pocket and implantation into the cornea of the affected eye after reflecting the buccal mucosa layer, with dentine facing the orbit and the bone towards the periorbital muscle [Figure 1].[5] A hole corresponding to the diameter of the PMMA optical cylinder (of osteo-odonto lamina) is trephined into the cornea of the affected eye to receive the posterior part of the cylinder, as well as into the buccal mucosa layer covering the affected eye to allow protrusion of the anterior part of the optical cylinder. Afterward, the mucosal flap is replaced into its position, and the eye is re-inflated. The vision is eventually restored after the second stage surgery when the light is allowed to transmit through the lens (of OOKP) to the retina of the patient's eye for clear vision. According to Professor Liu “Patients who have the surgery are often able to see immediately and the quality of sight can be extraordinarily good.”[7] Moreover, as the recovery time increase, vision increases. Some results of this procedure have been the ability to recognize faces; patient develops about 20/70 vision (at best even 20/40), and the ability to read newspaper print.[6]
Figure 1.
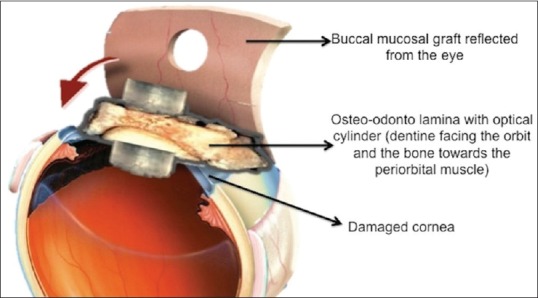
Osteo-nto lamina in position
This potential of OOKP in restoring vision has further been validated and well-established. Liu et al., in 2008 reported the long-term results of OOKP surgery in the visual rehabilitation of patients with corneal blindness from end-stage inflammatory ocular surface disease and revealed that out of the entire cohort, 83% patient had some improvement in vision, 78% achieved vision of 6/60 or better, and 53% achieved 6/12 or better.[8] Later, Tan et al., in 2012 systematically reviewed eight case series with sample sizes ranging from 4 to 181 eyes and found that anatomical survival rate of OOKP in all the studies was 87.8% (range: 67–100%) at 5 years with three studies exhibiting survival rates of 81.0% (range: 65–98%) even at 20 years; besides, the visual acuity was found to be more than 6/18 in 52% (range: 46–72%) of the eyes with OOKP surgery.[9] Thus, the authors concluded that of the available biological and synthetic keratoprosthesis, OOKP appears to be an excellent option for the treatment of end-stage corneal diseases.[9] Nevertheless, OOKP requires an interdisciplinary approach, involving a contribution from eye surgeons, dental surgeons, anesthesiologists, and other medical professionals for providing vision to the patients. The condition of the alveolar dental ligament plays a definitive role in the maintenance of the prosthesis and hence, the assessment of overall oral health with particular reference to oral hygiene and periodontal bone loss clinically as well as with the aid of orthopantomogram, and intraoral periapical radiographs is indispensable to ensure predictable results and avoid complications.[3] Since, if the harvested oral tissue undergoes necrosis as a consequence of an inflammatory disease, the implanted material behaves such as an allogeneic material and is eventually extruded from the recipient site (eye) as has been demonstrated by histological examination of the prosthesis removed 16 years after implantation in a patient.[10] Resorption of the bone may also be assessed radiologically using spiral computed tomography, magnetic resonance imaging or electron beam tomography, further aiding regular scanning of the OOKP lamina in all patients.[3]
Other complications associated with OOKP include necrosis of the buccal mucosal graft that may require additional grafting procedures, complications such as oromaxillary fistulas, fractures of the mandible, and damage to adjacent teeth and periodontium may also occur. Further, when the implant is in the subcutaneous pouch, absorption of the dentine, bone infection, or loosening of the optical cylinder can occur which should be then explanted and treated prior to continuation of the procedure or a second tooth should be harvested for implantation in the eye. Late postoperative complications include buccal membrane overgrowth over the optical cylinder or retroprosthetic membrane formation, requiring surgical removal. Serious sight-threatening complications include glaucoma, postoperative endophthalmitis, retinal detachment, etc.[9]
Nonetheless, osteo-odonto lamina plays an important role in making OOKP superior over other artificial corneal implants. Correspondingly, its success is essentially governed by the porosity of the bone that provides fixation of supporting tissues and by the suspensory periodontal ligament linking the bone to the cementum of the root dentine, that provides a barrier, preventing membrane encapsulation of the device and the downward migration of the mucosal epithelium, which may lead to separation of the optical cylinder from the osteo-odonto lamina. Furthermore, the shear and compressive forces on the supporting frame are well-absorbed by the periodontal ligament.[5]
CONCLUSION
Thus, this innovation acknowledges the contribution of periodontium and other oral structures in bestowing vision to the blind patients and further strengthens as well as presents a new dimension to the oral-systemic link, opening up gates for many newer exciting possibilities in the future promoting multidisciplinary research and teamwork for the welfare of general health of the people.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Strampelli B. Keratoprosthesis with osteodontal tissue. Am J Ophthalmol. 1963;89:1029–39. [Google Scholar]
- 2.Falcinelli G, Barogi G, Caselli M, Colliardod P, Taloni M. Personal changes and innovations in Strampelli's osteo-odonto-keratoprosthesis. An Inst Barraquer (Barc) 1999;28((s)):47–8. [Google Scholar]
- 3.Liu C, Paul B, Tandon R, Lee E, Fong K, Mavrikakis I, et al. The osteo-odonto-keratoprosthesis (OOKP) Semin Ophthalmol. 2005;20:113–28. doi: 10.1080/08820530590931386. [DOI] [PubMed] [Google Scholar]
- 4.Hille K, Grabner G, Liu C, Colliardo P, Falcinelli G, Taloni M, et al. Standards for modified osteoodontokeratoprosthesis (OOKP) surgery according to Strampelli and Falcinelli: The Rome-Vienna Protocol. Cornea. 2005;24:895–908. doi: 10.1097/01.ico.0000157401.81408.62. [DOI] [PubMed] [Google Scholar]
- 5.Viitala R, Franklin V, Green D, Liu C, Lloyd A, Tighe B. Towards a synthetic osteo-odonto-keratoprosthesis. Acta Biomater. 2009;5:438–52. doi: 10.1016/j.actbio.2008.07.008. [DOI] [PubMed] [Google Scholar]
- 6.Ausfresser G. Modified Osteo-OdontoKeratoprosthesis (MOOKP) [Last cited on 2015 Jan 05]. Available from: http://www.ele.uri.edu/Courses/bme281/F09/GabrielA_2.pdf .
- 7.Dailymail.com. Hodgekiss A. Blind Father Sees his Twin Sons’ Faces for First Time after Surgeon Restores his Sight Using one of his Teeth. [Last updated on 2013 Oct 03; Last cited on 2015 Jan 05]. Available from: http://www.dailymail.co.uk/health/article-2442404/Man-sight-restored-using-TEETH .
- 8.Liu C, Okera S, Tandon R, Herold J, Hull C, Thorp S. Visual rehabilitation in end-stage inflammatory ocular surface disease with the osteo-odonto-keratoprosthesis: Results from the UK. Br J Ophthalmol. 2008;92:1211–7. doi: 10.1136/bjo.2007.130567. [DOI] [PubMed] [Google Scholar]
- 9.Tan A, Tan DT, Tan XW, Mehta JS. Osteo-odonto keratoprosthesis: Systematic review of surgical outcomes and complication rates. Ocul Surf. 2012;10:15–25. doi: 10.1016/j.jtos.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 10.Ricci R, Pecorella I, Ciardi A, Della Rocca C, Di Tondo U, Marchi V. Strampelli's osteo-odonto-keratoprosthesis. Clinical and histological long-term features of three prostheses. Br J Ophthalmol. 1992;76:232–4. doi: 10.1136/bjo.76.4.232. [DOI] [PMC free article] [PubMed] [Google Scholar]


