Abstract
Background:
Open reduction and internal fixation with plate and screws are the gold standard for the surgical treatment of humeral shaft fractures, this study was to compare the mechanical properties of anteromedial, anterolateral, and posterior plating for humeral shaft fractures.
Methods:
A distal third humeral shaft fracture model was constructed using fourth-generation sawbones (#3404, composite bone). A total of 24 sawbones with a distal third humeral shaft fracture was randomly divided into three Groups: A, B, and C (n = 8 in each group) for anteromedial, anterolateral, and posterior plating, respectively. All sawbones were subjected to horizontal torsional fatigue tests, horizontal torsional and axial compressive fatigue tests, four-point bending fatigue tests in anteroposterior (AP) and mediolateral (ML) directions and horizontal torsional destructive tests.
Results:
In the horizontal torsional fatigue tests, the mean torsional angle amplitude in Groups A, B, and C were 6.12°, 6.53°, and 6.81°. In horizontal torsional and axial compressive fatigue tests, the mean torsional angle amplitude in Groups A, B, and C were 5.66°, 5.67°, and 6.36°. The mean plate displacement amplitude was 0.05 mm, 0.08 mm, and 0.10 mm. Group A was smaller than Group C (P < 0.05). In AP four-point bending fatigue tests, the mean plate displacement amplitude was 0.16 mm, 0.13 mm, and 0.20 mm. Group B was smaller than Group C (P < 0.05). In ML four-point bending fatigue tests, the mean plate displacement amplitude were 0.16 mm, 0.19 mm, and 0.17 mm. In horizontal torsional destructive tests, the mean torsional rigidity in Groups A, B, and C was 0.82, 0.75, and 0.76 N·m/deg. The yielding torsional angle was 24.50°, 25.70°, and 23.86°. The mean yielding torque was 18.46, 18.05, and 16.83 N·m, respectively.
Conclusions:
Anteromedial plating was superior to anterolateral or posterior plating in all mechanical tests except in AP four-point bending fatigue tests compared to the anterolateral plating group. We can suggest that anteromedial plating is a clinically safe and effective way for humeral shaft fractures.
Keywords: Anteromedial Plating, Biomechanics, Compressive Plate, Fracture Model, Humeral Shaft Fracture
INTRODUCTION
The humeral shaft fracture is one of the common types of orthopedic trauma, which account for approximately 1.2–3.0% of all fractures.[1,2,3,4] Currently, these fractures are primarily treated by surgery, resulting in good clinical outcomes.[5] Open reduction and fixation with plate and screws remain the gold standard for the treatment of humeral shaft fractures.[6,7,8,9] The treatment can be divided into three types based on the surgical approach: Anterolateral, posterior, and anteromedial. The former two are the most widely applied approaches in clinical practice.[10,11] However, during anterolateral plating, the radial nerve has to be isolated, placed on the surface of the plate or displaced since it moves along the radial nerve groove of the posterior humerus toward the inferior lateral humerus,[7] and this can cause iatrogenic radial nerve injury, with an incidence rate of 5.1–17.6%.[12,13,14] Moreover, damage to the muscular branches of the radial nerve is usually difficult to identify, but postoperative triceps muscle strength is often reduced. In addition, the radial nerve is frequently enveloped by a large number of calluses and large amounts of soft tissue scarring generated during fracture healing, which greatly increases the difficulty of plate removal and the incidence of iatrogenic radial nerve injury. Akan et al. found that anteromedial plating of humeral shaft fractures can markedly reduce the occurrence of iatrogenic radial nerve injury without increasing the incidence of the median nerve, brachial vein or ulnar nerve injury.[10] Furthermore, the anteromedial approach causes mild tissue injuries and no obvious local anatomical changes, and thus is associated with a lower incidence of iatrogenic injuries during plate removal.
According to the AO/ASIF (Arbeitsgemeinschaft für Osteosynthesefragen/Association for the Study of Internal Fixation) principles, in compressive stress states, the plate should be placed on the tension side of the fractured humerus, i.e., the lateral or posterior side. Nevertheless, the nonweight-bearing humerus is exposed to only low tensile stress, but also frequently to forces exerted by bending, twisting, body weight, and muscle traction. Therefore, anteromedial plating may be an alternative option for the treatment of humeral shaft fractures.[10] To date, the optimal plating approach remains an open question, which needs to be validated by biomechanical studies. We think that there is clinical value to compare the mechanical properties of anteromedial, anterolateral and posterior plating for humeral shaft fractures.
METHODS
Materials and instruments
A total of 24 fourth-generation sawbones (Item No: 3404, Pacific Research Laboratories, Inc., Vashon, WA, USA) were used as a synthetic left humerus model.
Testing instruments consisted of the following: Instron E10000 and E3000 electronic universal testing machines (Instron, High Wycombe, UK); Hand-made jigs; digital vernier caliper and digital height caliper (Prokit's Industries Co., Ltd., Taiwan, China); Ten-hole limited-contact plates (140 mm × 12.5 mm × 4.5 mm) and cortical screws (3.5 mm × 36 mm) (Tianjin ZhengTian Medical Instrument Co., Ltd., Tianjin, China); The ZX6350 series milling machine (Tengzhou Chenghai Inc., Shandong, China); Standard orthopedic internal fixation surgical instruments (Tianjin ZhengTian Medical Instrument Co., Ltd., Tianjin, China); Type II Class I self-curing denture powder and Type II Class I self-curing denture water (Shanghai New Century Dental Materials Company, Shanghai, China); Canon EOS 60D digital camera (Canon Corporation, Tokyo, Japan).
Preparation of fracture model
It is difficult to obtain reliable data in mechanical studies using cadaveric bones due to the rarity of the material and variations in physical properties and bone density. Synthetic humeri provide a good alternative because of their high degree of consistency in mechanical properties and physical size. In recent years, synthetic humeri have gradually become widely applied in mechanical studies.[15]
According to O’Toole method,[16] the measured width of the distal humerus condyle was 65.14 mm by the digital vernier caliper. A horizontal line was drawn at 65.14 mm away from the most distal humerus with a digital height caliper. The most distal end of the prebending plate was positioned strictly along the line, and the plate was attached to the bone surface in parallel to the long axis of the bone after shaping from the anteromedial, anterolateral, and posterior directions. The plate was held in place by a plate holder. Holes were drilled at the 1, 2, 3, 4, 7, 8, 9, and 10-hole positions on the proximal end of the plate according to the AO standard, followed by screw tapping. Two horizontal lines were drawn at 66.75 mm and 73.25 mm from the proximal end of the plate for use as fracture lines, and a 6.5-mm-long bone fracture was created with a ZX6350 series milling machine.[17] The plate was placed tightly along the fracture and screws were inserted into the existing holes by bicortical fixation. Our sequence of the fracture model preparation was to make sure the anatomical reductions were identical.
A total of 24 synthetic humerus sawbones #3404 were randomly divided into three groups (n = 8), and anteromedial, anterolateral, and posterior fracture models of AO classification of 12-C3 were created. The results showed that the plate in the anteromedial group was placed tightly without prebending, whereas the plate in the anterolateral and posterior groups was a poor fit against the bone and prebending was needed. Drilling and screw tapping were performed for the preparation of the fracture models. The anatomical reduction was observed in all specimens after fixation of the fractures with plates and screws [Figure 1].
Figure 1.

Anatomical reduction was observed in all specimens after fixation of the fractures with plates and screws.
Biomechanical testing
The hand-made jig had a central axis pin, which was inserted into the axis hole in the synthetic humerus sawbone (#3404) to ensure concentricity. Self-curing denture powder and water were precooled to 4° for 24 h. The jig, with the humerus proximal side down, was placed on the Instron E10000 system. The orientation of the specimen was adjusted, and the mixture of denture powder and water was poured into a hand-made mold. After it was completely cured, the jig and specimen were flipped, and the distal end of the specimen was poured as described from the proximal end. All surfaces of the jig were horizontal. All operations were performed by the same two technicians strictly following the same steps.
This study aimed to compare the biomechanical effects (capacity to resist bending and torsion) of the three plating approaches to provide a reliable reference for selection of the optimal surgical approach for the treatment of humeral shaft fractures.
Four biomechanical tests were selected for the assessment based on the literature[17] and on clinical experience during postoperative rehabilitation of humerus fractures, and performed as described below:
Horizontal torsional fatigue tests
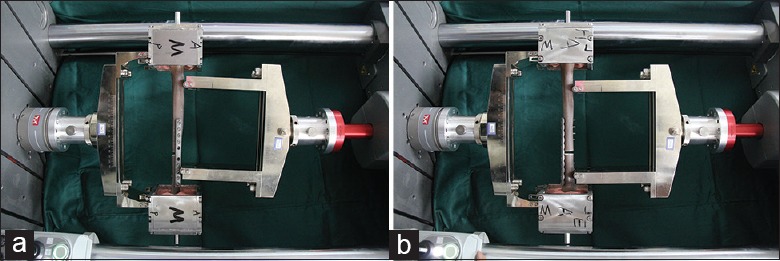
A total of 1500 horizontal torsional fatigue tests were performed using an Instron E10000 system with an axial retention pressure of 15 N, ±5 N·m cyclic torque capacity, and a frequency of 0.05 Hz. The torsional angle was automatically recorded by the device [Figure 2a–2c].
Figure 2.
(a) Horizontal torsional fatigue test of the anteromedial plating. (b) Horizontal torsional fatigue test of the anterolateral plating. (c) Horizontal torsional fatigue test of the posterior plating.
Horizontal torsional and axial compressive fatigue tests
After the completion of horizontal torsional fatigue tests, all specimens were examined to check for structural damage. Then, specimens were subjected to 1500 horizontal torsional and axial compressive fatigue tests using the E10000 system with an axial load of 50–500 N and ±5 N·m horizontal torque that were applied synchronously at a frequency of 0.05 Hz. The torsional angle and plate displacement amplitude were automatically recorded by the device.
Four-point bending fatigue tests
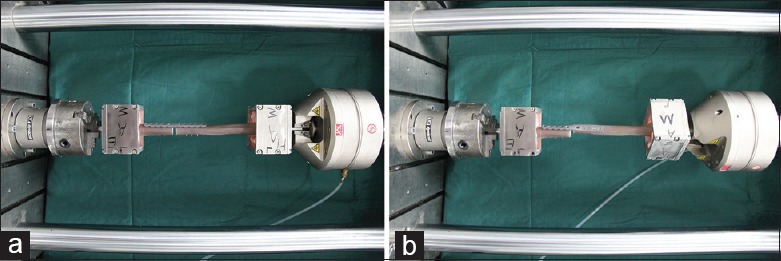
Specimens were then subjected to four-point bending fatigue tests as described previously.[17] Briefly, the plane passing through the line between the medial and lateral epicondyle of the humerus that was parallel to the ground was considered the horizontal plane of the humerus. The planes perpendicular to this horizontal plane were referred as the medial and lateral surfaces. A total of 1500 four-point bending fatigue tests were performed using an Instron E3000 system with a cyclic load of 24–240 N in anteroposterior (AP) and mediolateral (ML) directions, at a frequency of 0.5 Hz. The plate displacement amplitude was automatically recorded by the device [Figure 3a and 3b].
Figure 3.
(a) Antero-posterior four-point bending fatigue test. (b) Medio-lateral four-point bending fatigue test.
Horizontal torsional destructive tests
Specimens were subjected to horizontal torsional destructive tests using an Instron E10000 system with a pretest axial pressure of 15 N and a twist angle loading rate of 15°/min until the destruction of the subjects. The torsional rigidity (N·m/deg), yielding torsional angle (deg), and yielding torque (N·m) were recorded [Figure 4a and 4b].
Figure 4.
(a) The start of the horizontal torsional destructive test. (b) The end of the horizontal torsional destructive test.
Statistical analysis
Data were analyzed using SPSS 19.0 statistical software (IBM Corp., Armonk, NY, USA). A P < 0.05 was considered statistically significant. If P < 0.05, pair-wise comparison between groups was then performed.
RESULTS
All specimens in the three groups were intact after the completion of tests of horizontal torsional fatigue, horizontal torsional and axial compressive fatigue, and four-point bending fatigue, and were then subjected to horizontal torsional destructive testing. All corresponding data were recorded automatically by the device.
In the horizontal torsional fatigue tests, there was no significant difference in the amplitude of the mean torsional angle (6.12°, 6.53°, and 6.81° in Groups A, B and C, P > 0.05). In the horizontal torsional and axial compressive fatigue tests, variance analyses revealed significant differences in the mean displacement amplitude (0.05 mm, 0.08 mm, and 0.1 mm in Groups A, B, and C, respectively, P < 0.001). The further pair-wise comparison showed that there was a significant difference between Groups A and B (P < 0.001), Groups A and C (P < 0.001), and Groups B and C (P < 0.004). In the AP four-point bending fatigue tests, variance analyses revealed a significant difference in the mean displacement amplitude among the groups (0.16 mm, 0.13 mm, and 0.20 mm in Group A, B, and C respectively, P < 0.001). In further pair-wise comparisons, a significant difference was observed between Groups B and C (P < 0.013), but not between Groups A and B (P > 0.05), or Groups A and C (P > 0.05). In the ML four-point bending fatigue tests, there was no significant difference in the mean torsional displacement amplitude (0.16 mm, 0.17 mm, and 0.19 mm in Groups A, B, and C, respectively, P > 0.05). In the horizontal torsional destructive tests, there was no significant difference in the mean torsional rigidity (0.82, 0.75, and 0.76 N·m/deg in Groups A, B, and C, P > 0.05), yielding torsional angle (24.50°, 25.70°, and 23.86° in Groups A, B, and C, P > 0.05), or yielding torque (18.46, 18.05 and 16.83 N·m in Groups A, B, and C, P > 0.05). Details are summarized in Tables 1 and 2.
Table 1.
Comparison of the mean torsional angle amplitude, displacement amplitude, torsional rigidity, yielding torsional angle, and yielding torque of the three groups in different mechanical tests (Mean ± SD)
| Tests | A | B | C | P |
|---|---|---|---|---|
| Horizontal torsional fatigue test | ||||
| Torsional angle amplitude (°) | 6.12 ± 0.963 | 6.52 ± 0.741 | 6.81 ± 0.745 | 0.265 |
| Horizontal torsional and axial compressive fatigue test | ||||
| Torsional angle amplitude (°) | 5.66 ± 0.683 | 5.67 ± 0.478 | 6.36 ± 0.883 | 0.095 |
| Displacement amplitude (mm) | 0.05 ± 0.008 | 0.08 ± 0.008 | 0.10 ± 0.016 | <0.001 |
| Four-point bending fatigue test | ||||
| AP displacement amplitude (mm) | 0.16 ± 0.015 | 0.13 ± 0.017 | 0.200 ± 0.027 | <0.001 |
| ML displacement amplitude (mm) | 0.16 ± 0.025 | 0.19 ± 0.030 | 0.170 ± 0.024 | 0.094 |
| Horizontal torsional destructive test | ||||
| Torsional rigidity (N·m/deg) | 0.82 ± 0.090 | 0.75 ± 0.121 | 0.79 ± 0.080 | 0.386 |
| Yielding torsional angle (°) | 24.50 ± 2.419 | 25.70 ± 2.400 | 23.86 ± 4.113 | 0.492 |
| Yielding torque (N·m) | 18.46 ± 1.386 | 18.05 ± 0.922 | 16.83 ± 2.877 | 0.233 |
SD: Standard deviation; AP: Antero-posterior; ML: Medio-lateral.
Table 2.
P value of pair-wise comparisons of groups AB, BC, and AC
| Tests | AB | BC | AC |
|---|---|---|---|
| Horizontal torsional and axial compressive fatigue test | 0.001 | 0.004 | 0.001 |
| Four-point bending fatigue test | 0.170 | 0.013 | 0.105 |
AB: Groups A and B; BC: Groups B and C; AC: Groups A and C.
DISCUSSION
The goal of treatment for humeral shaft fractures is not only fracture healing but also, more importantly, the functional recovery of the limb. Surgery has long been the main treatment method for humeral shaft fractures.[5,18] As the gold standard method for the treatment of humeral shaft fractures, open reduction, and fixation with a plate and screws is well recognized.[6,7,8,9] Strong fixation with plate and screws can ensure early postoperative functional exercise and functional restoration of the limb.
Currently, anterolateral plating is the most widely applied surgical approach for humeral shaft fractures in clinical practice. In contrast, anteromedial plating of humeral shaft fractures has seldom been reported.
It was traditionally believed that iatrogenic injuries would rarely occur in anterolateral or posterior plating with the only complication involving interference of the radial nerve when compared with anteromedial plating, during which surgery might be complicated by the anatomical complexity of the inner side of the upper arm, especially the median nerve, brachial vein, and ulnar nerve. However, the reported incidence of iatrogenic radial nerve injury is 5.1–17.6%.[12,13,14] Moreover, plate removal may cause severe radial nerve injuries, leading to deformities including vertical fingers or wrist. Research for our study found that anteromedial plating was performed by inserting the plate from the rear side of the medial brachial intermuscular septum without splitting any muscle. Using this approach, the anteromedial surface of the humerus was easily exposed by pulling the median nerve and arteriovenous bundle forward and the ulnar nerve backward. We believe that operations carried out under direct vision are safer and have fewer potential risks compared with those performed without direct vision. Bichsel and Nyffeler,[19] and Livani and Belangero[20] have pointed out that a long incision is required for positive identification of the radial nerve area and, thus, to ensure the safety of the surgery. In a cadaveric study, Apivatthakakul et al.[21] suggested that 36.35–59.20% of the humerus, starting from the lateral epicondyle, is prone to damage and that 47.22–53.21% of the area is highly susceptible to damage. It is recommended to perform single-layer cortical fixation during screw insertion in this region to avoid any irritation of the radial nerve by the end of the screw, resulting in iatrogenic radial nerve injury. Detailed preoperative planning is essential for successful surgery. The anterior medial approach is performed with an incision from triceps and biceps brachii clearance to enter, to avoid splitting the brachialis muscle tissue, and reduce intra-operative bleeding. The anterior lateral approach may need to split the brachialis muscle. The posterior approach may need to split the triceps muscle to reveal the humeral shaft. Either of these approaches can cause increased bleeding. Anteromedial plating has little impact on nearby blood vessels and nerves and is conducive to postoperative recovery. In this study, we found that the plate in the anteromedial group could be placed tightly without prebending,[10] whereas in the anterolateral and posterior group, the plate fit poorly against the bone and prebending was needed, which increases operation time.
During rehabilitation of humeral shaft fractures after plate fixation, patients perform exercises including elbow flexion and extension, shoulder rotation, adduction, and abduction to restore limb functions. Unlike the weight-bearing tibia and femur, the humerus is usually exposed to only low tensile stress but also frequently to bending and twisting forces.[17] One of the main purposes of surgery for humeral shaft fractures is to ensure an early return to functional exercises by providing strong fixation.[22] According to the clinical experience, we assumed an optimal daily exercise regime of elbow flexion and extension (twenty times), upper limb rotation (twenty times), and adduction and abduction (twenty times), resulting in a total of 1000 repeats of each movement by day 50 after surgery. Assuming a safety factor of 1.5, 1500 repeats of each individual fatigue test were performed to simulate the actual clinical rehabilitation process.
In this study, fourth-generation sawbones (#3404) with uniform size and mechanical properties, and plates and screws from a single batch were used. All fracture models were created by the same two technicians strictly following the standard, and the anatomical reduction was achieved in nearly all specimens. In contrast, it is difficult to obtain reliable data in mechanical studies using cadaveric bones due to the rarity of the material and variations in physical properties and bone density.
In the horizontal torsional and axial compressive fatigue tests, variance analyses revealed significant differences in the mean displacement amplitude among the groups. Further pair-wise comparisons showed that the displacement amplitude in Group A was significantly lower than Groups B and C (P < 0.001), suggesting that the humeral shaft was primarily subjected to horizontal torsion and axial compressive force during the rehabilitation exercises, especially during shoulder rotation. Our results showed a larger displacement in anterolateral and posterior approaches due to the relatively lower stability of the plate, which might lead to delayed healing or nonunion of the fractures. Anterolateral and posterior plating are the most widely applied approaches for the treatment of humeral shaft fractures in clinical practice.[10,11] The mechanical properties of anteromedial plates were comparable to those of anterolateral and posterior plates in this study, suggesting that the fixation strength of an anteromedial plate meets the mechanical requirements of humeral shaft fracture surgery. The current study has provided a reliable mechanical basis for the widespread application of this approach for clinical practice. Furthermore, making the incision on the inner side of the upper arm during anteromedial plating not only meets the esthetic requirements of patients but is also suitable for special patients such as those with vascular injuries on the medial side of the upper arm and the lateral skin condition is not suitable for the operation, as well as obese patients and those suffering from nonunion.[23] We have done the relevant anatomical experiments, confirmed that the anterior medial approach is safe and effective, and the corresponding article is ready to be published.
Some clinical studies about minimally invasive anterior fixation of humeral shaft fracture have been reported.[24,25,26,27,28] Minimally invasive anterior fixation of humeral shaft fracture has its own advantages, for example, the minimally invasive plate osteosynthesis (MIPO) technique does offer a procedure with less stripping that can reduce the incidence of nonunion. A smaller incision, theoretically, causes less injury to the neurovascular structures.[24,25,26,27,28] The disadvantages are also obvious: Six disadvantages will be discussed. First, fracture reduction is difficult because it is a closed reduction. Complex humeral shaft fractures are difficult to achieve good reduction in operations, especially in correcting malrotation. Maintaining reduction is also very difficult.[24,25] There is the risk of injury to the radial nerve in the process of complex fracture reduction[26,28] and this may also increase the soft tissue injury around the fracture site. Second, during the operation, repeated C-arm X-ray monitoring was needed to monitor the position of the fracture and the placement of the plate and screw, and increases radiation hazard for medical staff and the patients.[27] Furthermore, the distal incision exposes the brachialis muscle and lateral traction to protect the radial nerve, which is a potential risk of iatrogenic radial nerve injury. Next, during this operation, it is possible to reduce the holding force of the screw because of repeated drilling and may cause internal fixation failure.[28] As well, the entire course of the muscle cutaneous nerve cannot be exposed and protected. There is increased the risk of injury in the process of drilling the screw into the bone. Finally, the postoperative skin scar was obvious because the scar is on the anterior side of the upper arm, compared to the MIPO technique.
Six advantages will be mentioned. First, the open reduction is relatively simple compared to the closed reduction, and also easier for maintaining the reduction before the plate was fixed. Second, there is no need for C-arm monitoring, no radiation hazard for the medical staff and the patients. Next, the radial nerve does not interfere during the operation. As well, for a satisfactory fracture reduction, the screw can be well controlled during the fixing of the plate to the bone. Furthermore, the muscle cutaneous nerve has no interference during the operation. Finally, the postoperative scar is concealed because the scar is on the medial side of the upper arm.
This study was performed only on artificial specimens, without removal of the muscles. The changes in fracture stability during the different recovery phases were not monitored. Furthermore, anteromedial plating is not suitable for humeral shaft fracture patients with concurrent radial nerve palsy or injury, which has a reported incidence rate of 2–17%,[29] since the central or distal radial nerve is not exposed during the operation. Surgical indication does not include the proximal humeral fracture because the anteromedial approach has not enough length for proximal fixation by the screws. This technique also requires clinicians to be familiar with the anatomy of the upper arm.[10]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Yi Cui
REFERENCES
- 1.Ekholm R, Adami J, Tidermark J, Hansson K, Törnkvist H, Ponzer S. Fractures of the shaft of the humerus. An epidemiological study of 401 fractures. J Bone Joint Surg Br. 2006;88:1469–73. doi: 10.1302/0301-620X.88B11.17634. doi: 10.1302/0301-620x.88b11.17634. [DOI] [PubMed] [Google Scholar]
- 2.Mahabier KC, Vogels LM, Punt BJ, Roukema GR, Patka P, Van Lieshout EM. Humeral shaft fractures: Retrospective results of non-operative and operative treatment of 186 patients. Injury. 2013;44:427–30. doi: 10.1016/j.injury.2012.08.003. doi: 10.1016/j.injury.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 3.Brunner A, Thormann S, Babst R. Minimally invasive percutaneous plating of proximal humeral shaft fractures with the proximal humerus internal locking system (PHILOS) J Shoulder Elbow Surg. 2012;21:1056–63. doi: 10.1016/j.jse.2011.05.016. doi: 10.1016/j.jse.2011.05.016. [DOI] [PubMed] [Google Scholar]
- 4.Volgas DA, Stannard JP, Alonso JE. Nonunions of the humerus. Clin Orthop Relat Res. 2004;419:46–50. doi: 10.1097/00003086-200402000-00008. doi: 10.1097/00003086-200402000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Denard A, Jr, Richards JE, Obremskey WT, Tucker MC, Floyd M, Herzog GA. Outcome of nonoperative vs operative treatment of humeral shaft fractures: A retrospective study of 213 patients. Orthopedics. 2010;33:552. doi: 10.3928/01477447-20100625-16. doi: 10.3928/01477447-20100625-16. [DOI] [PubMed] [Google Scholar]
- 6.Lee HJ, Oh CW, Oh JK, Apivatthakakul T, Kim JW, Yoon JP, et al. Minimally invasive plate osteosynthesis for humeral shaft fracture: A reproducible technique with the assistance of an external fixator. Arch Orthop Trauma Surg. 2013;133:649–57. doi: 10.1007/s00402-013-1708-7. doi: 10.1007/s00402-013-1708-7. [DOI] [PubMed] [Google Scholar]
- 7.Lee TJ, Kwon DG, Na SI, Cha SD. Modified combined approach for distal humerus shaft fracture: Anterolateral and lateral bimodal approach. Clin Orthop Surg. 2013;5:209–15. doi: 10.4055/cios.2013.5.3.209. doi: 10.4055/cios.2013.5.3.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lever JP, Aksenov SA, Zdero R, Ahn H, McKee MD, Schemitsch EH. Biomechanical analysis of plate osteosynthesis systems for proximal humerus fractures. J Orthop Trauma. 2008;22:23–9. doi: 10.1097/BOT.0b013e31815c89ce. doi: 10.1097/bot.0b013e31815c89ce. [DOI] [PubMed] [Google Scholar]
- 9.Spitzer AB, Davidovitch RI, Egol KA. Use of a “hybrid” locking plate for complex metaphyseal fractures and nonunions about the humerus. Injury. 2009;40:240–4. doi: 10.1016/j.injury.2008.07.019. doi: 10.1016/j.injury.2008.07.019. [DOI] [PubMed] [Google Scholar]
- 10.Akan B, Armangil M, Basarir K, Acar H, Bilgin S, Demirtas M. Clinical evaluation of an antero-medial approach for plate fixation of the proximal humeral shaft. Eur J Orthop Surg Traumatol. 2012;22:289–93. doi: 10.1007/s00590-011-0843-5. [Google Scholar]
- 11.Clavert P, Adam P, Bevort A, Bonnomet F, Kempf JF. Pitfalls and complications with locking plate for proximal humerus fracture. J Shoulder Elbow Surg. 2010;19:489–94. doi: 10.1016/j.jse.2009.09.005. doi: 10.1016/j.jse.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 12.Ricci FP, Barbosa RI, Elui VM, Barbieri CH, Mazzer N, Fonseca Mde C. Radial nerve injury associated with humeral shaft fracture: A retrospective study. Acta Ortop Bras. 2015;23:19–21. doi: 10.1590/1413-78522015230100823. doi: 10.1590/1413-78522015230100823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Claessen FM, Peters RM, Verbeek DO, Helfet DL, Ring D. Factors associated with radial nerve palsy after operative treatment of diaphyseal humeral shaft fractures. J Shoulder Elbow Surg. 2015;24:e307–11. doi: 10.1016/j.jse.2015.07.012. doi: 10.1016/j.jse.2015.07.012. [DOI] [PubMed] [Google Scholar]
- 14.Patra BP, Patra SK. Radial nerve palsy following plate osteosynthesis of shaft humerus in relation to posterior verses anterolateral approach. Int J Res Med Sci. 2016;4:913–9. doi: 10.18203/2320-6012.ijrms20160542. [Google Scholar]
- 15.Dunlap JT, Chong AC, Lucas GL, Cooke FW. Structural properties of a novel design of composite analogue humeri models. Ann Biomed Eng. 2008;36:1922–6. doi: 10.1007/s10439-008-9568-y. doi: 10.1007/s10439-008-9568-y. [DOI] [PubMed] [Google Scholar]
- 16.O'Toole RV, Andersen RC, Vesnovsky O, Alexander M, Topoleski LD, Nascone JW, et al. Are locking screws advantageous with plate fixation of humeral shaft fractures?A biomechanical analysis of synthetic and cadaveric bone. J Orthop Trauma. 2008;22:709–15. doi: 10.1097/BOT.0b013e31818df8cb. doi: 10.1097/bot.0b013e31818df8cb. [DOI] [PubMed] [Google Scholar]
- 17.Dunlap JT, Lucas GL, Chong AC, Cooke FW, Tiruvadi V. Biomechanical evaluation of locking plate fixation with hybrid screw constructs in analogue humeri. Am J Orthop (Belle Mead NJ) 2011;40:E20–5. [PubMed] [Google Scholar]
- 18.Singh AK, Narsaria N, Seth RR, Garg S. Plate osteosynthesis of fractures of the shaft of the humerus: Comparison of limited contact dynamic compression plates and locking compression plates. J Orthop Traumatol. 2014;15:117–22. doi: 10.1007/s10195-014-0290-2. doi: 10.1007/s10195-014-0290-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bichsel U, Nyffeler RW. Secondary radial nerve palsy after minimally invasive plate osteosynthesis of a distal humeral shaft fracture. Case Rep Orthop 2015. 2015:1–3. doi: 10.1155/2015/241968. doi: 10.1155/2015/241968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Livani B, Belangero WD. Bridging plate osteosynthesis of humeral shaft fractures. Injury. 2004;35:587–95. doi: 10.1016/j.injury.2003.12.003. doi: 10.1016/j.injury.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 21.Apivatthakakul T, Patiyasikan S, Luevitoonvechkit S. Danger zone for locking screw placement in minimally invasive plate osteosynthesis (MIPO) of humeral shaft fractures: A cadaveric study. Injury. 2010;41:169–72. doi: 10.1016/j.injury.2009.08.002. doi: 10.1016/j.injury.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 22.Scolaro JA, Hsu JE, Svach DJ, Mehta S. Plate selection for fixation of extra-articular distal humerus fractures: A biomechanical comparison of three different implants. Injury. 2014;45:2040–4. doi: 10.1016/j.injury.2014.08.036. doi: 10.1016/j.injury.2014.08.036. [DOI] [PubMed] [Google Scholar]
- 23.Jupiter JB. Complex non-union of the humeral diaphysis. Treatment with a medial approach, an anterior plate, and a vascularized fibular graft. J Bone Joint Surg Am. 1990;72:701–7. [PubMed] [Google Scholar]
- 24.Wang C, Li J, Li Y, Dai G, Wang M. Is minimally invasive plating osteosynthesis for humeral shaft fracture advantageous compared with the conventional open technique?J Shoulder Elbow Surg. 2015;24:1741–8. doi: 10.1016/j.jse.2015.07.032. doi: 10.1016/j.jse.2015.07.032. [DOI] [PubMed] [Google Scholar]
- 25.Zhiquan A, Bingfang Z, Yeming W, Chi Z, Peiyan H. Minimally invasive plating osteosynthesis (MIPO) of middle and distal third humeral shaft fractures. J Orthop Trauma. 2007;21:628–33. doi: 10.1097/BOT.0b013e31815928c2. doi: 10.1097/bot.0b013e31815928c2. [DOI] [PubMed] [Google Scholar]
- 26.Sanjeevayya C, Praneethreddy K. Minimally invasive plate osteosynthesis (mipo) in humeral shaft fractures – Biomechanics – Design – Clinical results. Int J Biol Med Res. 2016;7:5389–93. [Google Scholar]
- 27.Lian K, Wang L, Lin D, Chen Z. Minimally invasive plating osteosynthesis for mid-distal third humeral shaft fractures. Orthopedics. 2013;36:e1025–32. doi: 10.3928/01477447-20130724-18. doi: 10.3928/01477447-20130724-18. [DOI] [PubMed] [Google Scholar]
- 28.Pospula W, Abu Noor T. Percutaneous fixation of comminuted fractures of the humerus: Initial experience at Al Razi hospital, Kuwait. Med Princ Pract. 2006;15:423–6. doi: 10.1159/000095487. doi: 10.1159/000095487. [DOI] [PubMed] [Google Scholar]
- 29.Bumbasirevic M, Lesic A, Bumbasirevic V, Cobeljic G, Milosevic I, Atkinson HD. The management of humeral shaft fractures with associated radial nerve palsy: A review of 117 cases. Arch Orthop Trauma Surg. 2010;130:519–22. doi: 10.1007/s00402-009-0951-4. doi: 10.1007/s00402-009-0951-4. [DOI] [PubMed] [Google Scholar]



