Abstract
Background:
Migrations have been reported to be associated with the high risk of tuberculosis (TB), but there is no systematic analysis of the available data for TB among migrant in China. The aim of this study was to examine the notification rate of active and sputum smear-positive TB by a systematic review and meta-analysis.
Methods:
A systematic review and meta-analysis were performed to examine the notification rate of active and sputum smear-positive TB among migrants in China. Two reviewers searched the cross-sectional studies published in PubMed, EMBASE, SciFinder, and Web of Science in English and in CNKI and Wanfang databases in Chinese. Pooled estimates of notification rate of TB among migrants were calculated using a random effects model. Meta-regression analysis and subgroup analysis stratified by year, region were also performed.
Results:
Seventy eligible studies met the inclusion criteria for the final analysis. The overall notification rate of active TB and sputum smear-positive cases among migrants were 53.12 (95% confidence interval [CI]: 47.32–59.63) and 24.53 (95% CI: 22.01–27.34) per 100,000 populations, respectively. The notification rate of active TB significantly increased from 50.95 (95% CI: 41.11–63.14) per 100,000 populations in 2005 to 84.62 (95% CI: 78.00–91.80) per 100,000 populations in 2014 while that of smear-positive TB was constant during the study time (P = 0.79). The geographic difference was identified both for active and sputum smear-positive TB, with the higher notification rates mainly distributing along the eastern coastal areas.
Conclusions:
The pooled estimate of active TB and sputum smear-positive TB among migrants was lower than the national notification rate among general population, but the gap between our data and national notification rate among general population is narrowed down during 2005–2014.
Keywords: Meta-analysis, Migrants, Notification Rate, Systematic Review, Tuberculosis
INTRODUCTION
Tuberculosis (TB) remains a challenge among migrants despite a steady decrease in TB incidence among the general population in the last decade worldwide.[1,2,3,4,5] The WHO report shows that the notification rate of TB in immigrants is 82.9 per 100,000 population in countries where TB incidence fluctuates between 100 and 300 per 100,000 populations. The notification rate increases to 425.5 per 100,000 population in countries where TB incidence is <30 per 100,000 population, a low TB burden country defined by WHO.[6] However, there are no data on TB among migrants in countries where the incidence is between 30 and 100 per 100,000 population or above 300 per 100,000 population.[6]
China has 260 million internal migrants according to the China migration report,[7] but there was no national survey of TB among this risk population until 2010 when Liu et al. first reported the distribution of active TB patients at the provincial level by analyzing surveillance data.[8] Emergence of a large number of migrants in the last decade is one of the major reasons for inadequate knowledge about TB among this dynamic population. Lack of specific budget for TB surveillance among this high-risk population is another reason. The global fund was the first funding group to initiate a TB control project among migrants in six provinces in 2006.[9]
Limited local studies disclosed few features of TB situation among migrants, such as economic status and potential social stigma.[10,11,12] To address the TB problem among 260 million migrants, a systematic study on TB epidemic among migrant is needed to inform the decision by policymakers. We, therefore, performed this systematic review and meta-analysis to examine the overall notification rate of active and sputum smear-positive TB from 2005 to 2014.
METHODS
Search strategy and study selection
We designed a strategy to search for all published studies that reported notification rate of active or sputum smear-positive TB among migrants from January 2005 to October 15, 2015. The search was conducted in PubMed, EMBASE, SciFinder, and Web of Science in English and studies of in CNKI and Wanfang databases in Chinese. The search terms were “tuberculosis,” “Mycobacterium tuberculosis,” “tuberculosis, pulmonary,” and “migrant,” “migration,” “transient,” and “floating.” The details of the search strategy are available in the Supplementary Table.
Supplementary Table.
The search strategies
| Database | Search terms |
|---|---|
| Medline (PubMed) | #1 “Tuberculosis”[Mesh] OR tb OR tuberculosis #2 “Transients and Migrants”[Mesh] OR “Emigration and Immigration”[Mesh] OR immigrant*OR migrant* OR migrat* #1 AND #2 |
| SciFinder | #1 tb OR tuberculosis #2 Transients OR Migrants OR Emigration OR Immigration OR immigrant*OR migrant* OR migrat* #1 AND #2 |
| Web of Science | #1 tb OR tuberculosis #2 Transients OR Migrants OR Emigration OR Immigration OR immigrant*OR migrant* OR migrat* #1 AND #2 |
| WanFang | #1 jiehe #2 Liudong OR huji OR qianyi #1 AND #2 |
| CNKI | #1 jiehe #2 Liudong OR huji OR qianyi #1 AND #2 |
We excluded manuscripts such as (1) the diagnosis of TB was not made according to clinical, radiological or microbiological criteria, (2) which were duplicated, and (3) which were editorials, conference abstracts, and systematic reviews.
“Migrant” was defined nonlocal residents who had lived or planned to live in a certain area for more than 3 months.[9]
Data extraction and definitions
Two reviewers Yi-Xuan Sun and Lei Zhu independently screened all titles and abstracts identified in the database. The full text of articles accessed by either reviewers was obtained. To determine eligibility for inclusion, the first reviewer Yi-Xuan Sun assessed all full text articles and the second reviewer LZ repeated this assessment independently for a 10% random sample of full text articles. For excluded articles, two reviewers were required to reach complete agreement. Disagreements were resolved by the senior authors.
Two reviewers Yi-Xuan Sun and Lei Zhu independently extracted data from all included studies. Data extracted from selected studies included (1) paper title, authors, location of study (province level), study time session, published date; (2) migrant's population definition, migrants’ population origins, TB cases data origins, TB diagnosis methods applied; and (3) cases of migrants, cases of active TB, cases of sputum smear-positive TB, notification rate of active TB or notification rate of sputum smear-positive TB among migrants. The number of migrants was collected from statistical bureaus or public security.
We used the standard of the Agency for Healthcare Research and Quality to evaluate the quality of articles. Articles accessed with a score of 5 or above have been included in the analysis. Based on the heterogeneity test results, the random effect model was chosen to pool the rates of active TB or smear-positive TB across provinces, years, and the period of the Global Fund China Migrant (GFCM) TB control project.
Statistical analysis
A sputum smear-positive TB is defined as a case who meets one of the three sets of conditions: (1) two positive sputum smears by microscopy, (2) one positive sputum smear and 1 positive sputum culture, or (3) 1 positive sputum smear-positive with typical pathology of active TB on a chest X-ray.[13] An active TB is defined as a sputum smear-positive TB or a sputum smear-negative but diagnosed clinically.[11]
Subgroup analysis was done to explore the sources of heterogeneity, sensitivity analysis, and funnel plot to inquire into publication bias using R version 3.2.1 (R Core Team, Vienna, Austria) with Meta package (version 4.3-1). The trend Chi-square was used to analyze the temporal trend in notification rate of active TB or smear-positive TB rates over the years SPSS version 20.0 (SPSS, Inc., Chicago, IL, USA). Geographical thematic map was used to reveal spatial distribution of two rates with ArcGIS Desktop Version 9.3 (ESRI Redlands, USA).
We categorized the research regions into three regions: East (Beijing, Tianjin, Hebei, Liaoning, Shanghai, Jiangsu, Zhejiang, Fujian, Shandong, Guangdong, Hainan), Middle (Shanxi, Inner Mongolia, Jilin, Heilongjiang, Anhui, Jiangxi, He’nan, Hubei, Hu’nan, Guangxi), and West (Sichuan, Guizhou, Yunnan, Xizang, Shaanxi, Gansu, Qinghai, Ningxia, Xinjiang). Furthermore, we compared notification rate in different periods of the GFCM TB Control Project (year 2005–2006, year 2007–2011, year 2012–2014).
RESULTS
We identified a total of 10,451 studies, with seventy studies meeting the inclusion criteria to be included in the final analysis [Figure 1, Supplementary Figure 2 (671.3KB, tif) ]. The seventy studies reported 42,426 sputum smear-positive TB cases and 104,393 active TB cases, respectively, in 243,131,054 migrants across 13 provinces from 2005 to 2014 [Table 1].
Figure 1.
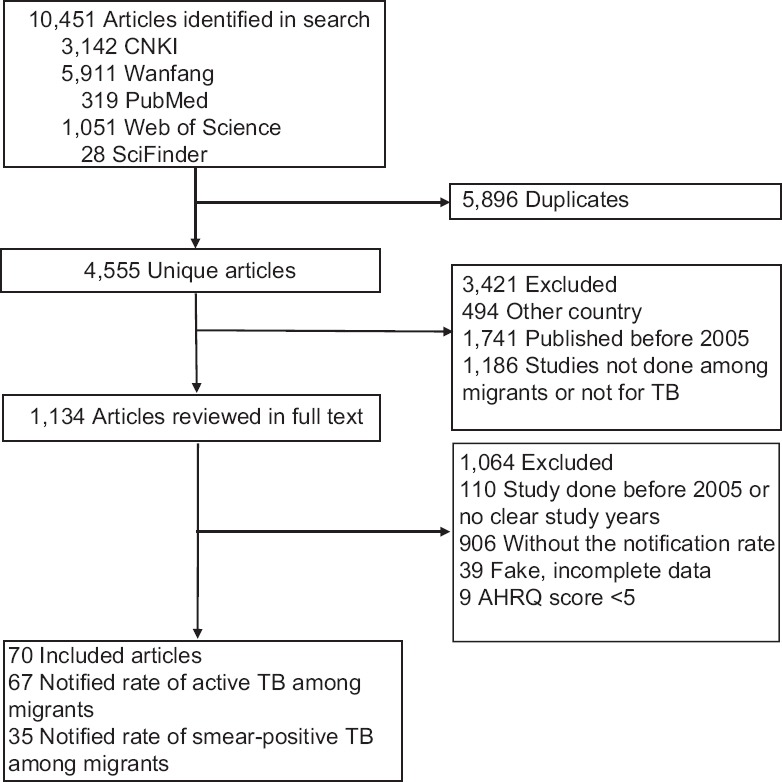
Flowchart of scanning. AHRQ: Agency for Healthcare Research and Quality.
Table 1.
Notification rate of active and positive TB among migrants during 2005–2014 by meta-analysis
| Years | Number of studies | Screened number | Case number | Notification rate (95% CI) | ||||
|---|---|---|---|---|---|---|---|---|
| Active | Positive | Active | Positive | Active | Positive | Active | Positive | |
| Overall | 67 | 35 | 189,713,880 | 156,230,594 | 104,393 | 42,426 | 56.91 (50.34–63.89) | 24.53 (22.01–27.34) |
| 2005 | 25 | 14 | 16,354,232 | 18,908,239 | 7341 | 4658 | 50.95 (41.11–63.14) | 25.82 (20.39–32.72) |
| 2006 | 34 | 20 | 36,129,661 | 36,330,792 | 14,339 | 8123 | 48.38 (40.19–58.25) | 23.48 (20.44–26.97) |
| 2007 | 39 | 26 | 21,103,953 | 25,247,139 | 11,589 | 7474 | 58.01 (48.63–69.22) | 24.83 (21.03–29.33) |
| 2008 | 36 | 24 | 20,129,364 | 27,428,193 | 11,809 | 8734 | 56.94 (49.25–65.83) | 26.80 (23.22–30.94) |
| 2009 | 36 | 24 | 21,117,925 | 14,759,550 | 12,769 | 4380 | 55.26 (46.94–65.06) | 26.52 (21.97–31.99) |
| 2010 | 30 | 21 | 18,011,447 | 15,581,322 | 11,592 | 4225 | 59.18 (48.02–72.93) | 24.57 (19.99–30.21) |
| 2011 | 21 | 13 | 15,806,101 | 12,818,979 | 9722 | 3371 | 56.61 (45.24–70.84) | 21.58 (16.79–27.74) |
| 2012 | 12 | 8 | 5,973,585 | 5,112,946 | 4695 | 1678 | 64.86 (50.76–82.89) | 22.84 (17.65–29.57) |
| 2013 | 4 | 2 | 938,227 | 406,734 | 998 | 76 | 70.12 (37.22–32.10) | 12.25 (2.48–60.47) |
| 2014 | 1 | 0 | 683,060 | – | 578 | – | 84.62 (78.00–91.80) | – |
| Preproject | 37 | 22 | 52,483,894 | 55,239,031 | 21,680 | 12,781 | 49.47 (43.12–56.75) | 24.64 (22.03–27.56) |
| Project | 52 | 34 | 96,332,512 | 95,835,183 | 57,560 | 28,184 | 57.14 (52.87–61.74) | 25.34 (23.54–27.26) |
| Postproject | 11 | 8 | 7,431,150 | 5,519,680 | 6192 | 1754 | 68.99 (55.64–85.54) | 21.08 (16.40–27.08) |
Preproject: 2005–2006; Project: 2007–2011; Postproject: 2012–2014; CI: Confidence interval; TB: Tuberculosis.
The notification rate during 2005–2013.
Notified rate on active TB (a) and smear-positive TB (b) among migrants by meta-analysis. TB: Tuberculosis.
Notification rate of active tuberculosis cases
The overall notification rate of active TB cases among migrants was 53.12 (95% confidence interval [CI]: 47.32–59.63) per 100,000 populations, with a significant increase from 50.95 (95% CI: 41.11–63.14) per 100,000 populations in 2005–84.62 (95% CI: 78.00–91.80) per 100,000 populations in 2014 [Table 1 and Figure 2].
Figure 2.
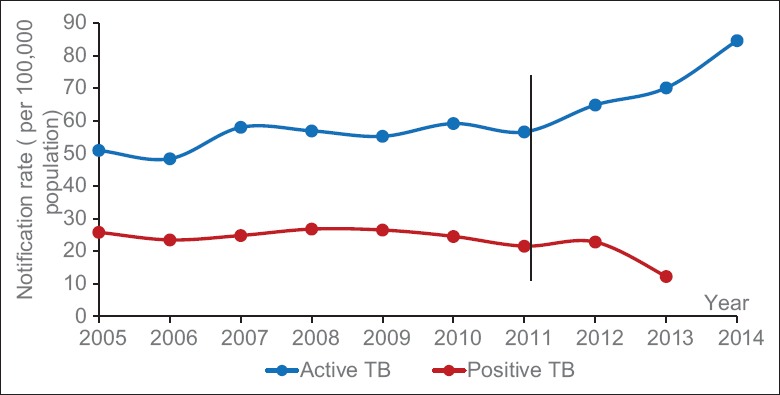
The trend of active TB and sputum smear-positive TB during 2004–2014. TB: Tuberculosis.
Geographic differences were also identified, 56.30 (95% CI: 49.71–63.30) per 100,000 in the eastern area, 57.11 (95% CI: 22.88–106.70) per 100,000 in the central, and 142.43 (95% CI: 118.27–168.83) per 100,000 in the west (P < 0.0001). By province, Xinjiang, Qinghai, Hubei, and Fujian showed relatively higher rate with 160.68 (95% CI: 115.29–213.58), 135.00 (95% CI: 107.22–165.98), 103.42 (95% CI: 67.81–146.51), and 81.14 (95% CI: 64.01–100.31) per 100,000 populations, respectively (P < 0.0001) [Table 2]. Heterogeneity was detected with a Chi-square of 22,368.17 (P < 0.0001) and I2 of 99.7%.
Table 2.
Notification rate among migrants by provinces and regions
| Provinces | Number of studies | Screened number | Case number | Notification rate (95% CI) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Active | Positive | Active | Positive | Active | Positive | Active | Positive | ||
| Overall | 67 | 35 | 189,713,880 | 156,230,594 | 104,393 | 42,426 | 56.91 (50.34–63.89) | 24.53 (22.01–27.34) | |
| Beijing | 3 | 1 | 11,636,107 | 7,896,096 | 3119 | 973 | 30.26 (25.70–35.18) | 12.32 (11.57–13.12) | |
| Shanghai | 18 | 9 | 32,520,591 | 14,750,865 | 14,619 | 2977 | 48.18 (41.18–55.39) | 18.72 (14.68–23.86) | |
| Jiangsu | 7 | 2 | 12,827,237 | 2,430,268 | 4914 | 578 | 44.87 (21.71–76.34) | 31.23 (13.51–72.20) | |
| Zhejiang | 16 | 10 | 45,151,513 | 36,779,062 | 26,352 | 8969 | 59.12 (50.65–68.24) | 23.08 (18.65–28.57) | |
| Fujian | 6 | 3 | 17,698,004 | 14,887,490 | 15,753 | 5873 | 81.14 (64.01–100.31) | 35.45 (30.21–41.60) | |
| Shandong | 4 | 2 | 7,488,467 | 5,029,158 | 5430 | 979 | 67.71 (60.66–75.14) | 28.56 (14.14–57.71) | |
| Guangdong | 11 | 6 | 58,889,304 | 73,714,595 | 31,845 | 20,924 | 65.43 (45.27–89.30) | 28.45 (23.36–34.64) | |
| Shanxi | 1 | 0 | 755,240 | – | 168 | – | 22.24 (19.01–25.74) | – | |
| Neimenggu | 1 | 0 | 47,018 | – | 19 | – | 40.41 (24.28–60.62) | – | |
| Anhui | 1 | 1 | 683,060 | 683,060 | 275 | 119 | 40.26 (35.64–45.16) | 17.42 (14.56–20.85) | |
| Hubei | 2 | 0 | 1,272,677 | – | 1453 | – | 103.42 (67.81–146.51) | – | |
| Qinghai | 1 | 1 | 60,000 | – | 81 | 55 | 135.00 (107.22–165.98) | 91.67 (70.39–119.38) | |
| Xinjiang | 1 | 0 | 25,516 | – | 41 | – | 160.68 (115.29–213.58) | – | |
| Eastern | 60 | 33 | 186,870,288 | 155,487,534 | 102,356 | 42,252 | 56.30 (49.71–63.30) | 23.92 (21.42–26.70) | |
| Central | 5 | 1 | 2,757,996 | 683,060 | 1915 | 119 | 57.11 (22.88–106.70) | 17.42 (14.56–20.85) | |
| Western | 2 | 1 | 85,516 | 60,000 | 122 | 55 | 142.43 (118.27–168.83) | 91.67 (70.39–119.38) | |
Eastern (Beijing, Tianjin, Hebei, Liaoning, Shanghai, Jiangsu, Zhejiang, Fujian, Shandong, Guangdong, Hainan); Central (Shanxi, Inner Mongolia, Jilin, Heilongjiang, Anhui, Jiangxi, He’nan, Hubei, Hu’nan, Guangxi); Western (Sichuan, Guizhou, Yunnan, Xizang, Shaanxi, Gansu, Qinghai, Ningxia, Xinjiang); CI: Confidence interval.
Notification rate of sputum smear-positive tuberculosis cases
The overall notification rate of sputum smear-positive TB cases was 24.53 (95% CI: 22.01–27.34) and maintained stable from 2005 to 2014 (P = 0.79) based on the analysis of 35 studies which reported sputum smear-positive TB [Table 1 and Figure 2]. Notification rate of smear-positive TB cases was 23.92 (95% CI: 21.42–26.70) per 100,000 population in the eastern area against 17.42 (95% CI: 14.56–20.85) per 100,000 population and 91.67 (95% CI: 70.39–119.38) per 100,000 population in the central and western areas, respectively (P < 0.0001). Qinghai also showed a higher rate of 91.67 (95% CI: 70.39–119.38) in comparison with other provinces (P < 0.01) [Table 2].
The rate among migrant showed a slight increase during the period of GFCM TB Control Project by 25.34 (95% CI: 23.54–27.26) in comparison with that of preproject by 24.64 (95% CI: 22.03–27.56) and of postproject by 21.08 (95% CI: 16.04–27.08) even without significant change (P = 0.38) [Table 1]. Heterogeneity was assessed with Chi-square of 3583.16 (P < 0.01) and I2 of 99.1% (P < 0.01) and I2 of 98.8%.
DISCUSSION
The present analysis is the first to report the notification rate of TB among migrants in China. The pooled estimate of the notification rate of active TB and sputum smear-positive TB among migrants were 56.91 (95% CI: 50.34–63.89) and 24.53 (95% CI: 22.01–27.34) per 100,000 populations, respectively. Based on global TB report,[14] the present analysis is also the first time to give data on TB situation for countries where the incidence of TB is between 30 and 100 per 100,000 population.[6]
The estimate of notification rate of smear-positive TB has been lower than the national data of 29.83, 36.92, 35.62, 35.32, 35.02, 36.17, 34.21, 29.82, and 25.72 in period of 2005–2012 with a slight decrease of 22.67 per 100,000 populations in 2013. The estimate of active TB is also lower than the national notification rate in the same time [Figure 2 and Supplementary Figure 1 (130.2KB, tif) ].[15] However, the gaps between our data and annually national notification rate narrowed down both for active and positive TB during 2005–2014 [Figure 2 and Supplementary Figure 1 (130.2KB, tif) ].[15]
This result can be attributed to several reasons. First, China initiated targeted TB control for migrants in 2006. There were no national data among migrants until 2010.[8] The number of migrants covered by surveillance is still expanding to date. It is difficult to quantify contribution of TB among migrants to the annual notification rate on TB under uncertain strategies. Second, the present analysis may underestimate the rate of TB among migrants because each rate involved in the study was calculated by dividing registered patients by the number of migrants in study setting [Table 2]. TB case finding is still passive in China.[16] TB patients could not be diagnosed until they consult a doctor and show TB symptoms. In addition, some migrant patients were not registered because of the cost for TB treatment; however, the number of migrants (denominator) for each study is usually the total migrants registered in a local official institute, such as public security. Third, meta-analysis may not represent real situation of TB among migrants because of publication bias detected in this study [Supplementary Figure 3 (213.6KB, tif) ].
Funnel plots of notified rate of active TB (a) and sputum smear-positive TB (b) among migrants TB: Tuberculosis.
Our study indicates an increase in active TB rate and a plateaus in smear-positive TB among migrants while the national notification rates among general population are decreasing [Figure 2 and Supplement Figure 1 (130.2KB, tif) ].[13] The most likely reason is that more and more benefit strategies of TB control covering migrant result in detection and finding of TB cases among migrants.[17] For example, China revised its administrative measures for prevention and control of TB in 2007.[18] The revised measures indicate that migrants should be provided with TB treatment in their respective residential areas when they are diagnosed as TB. Some areas subsequently provided free treatment for TB cases among migrants and further reduced delay of TB diagnosis by conducting entry examination for migrants.[19] Cheng et al. study showed that an increased proportion of TB cases was identified by physical examination among migrants in Shenzhen.[16] Increased funding on TB control project appeared to increase case finding which contributes to the higher notification rate. However, the intensified TB case finding does not imply an increased TB incidence among migrants [Table 1].
Geographic distribution patterns indicate that both active and sputum smear-positive TB are concentrated in the eastern coastal areas, which may be the result of migration from the rest of country.[20,21] The National Migrants Report 2011[21] indicated that 73.46% migrants have been flowing into Guangdong, Jiangsu, Zhejiang, and Shanghai. However, the high rate presented in Qinghai is most likely due to one reference which generally has publication bias resulted from authors.
The present analysis is subject to limitations. It only identifies notification rates of active and sputum smear-positive TB. There are insufficient data to investigate some risk factors, such as change of environment and socioeconomic stress, which have been proven to be related to immunity and might be closely associated with TB among migrants.[22] The present analysis would also have missed unreachable unpublished data. Moreover, the present analysis may be subject to publication bias as studies with more TB case among migrants may be less likely to be published. This may have led to over or underestimation of notification rate among migrants. However, the situation may be opposite.
While the present analysis indicates relatively low TB rates among migrants compared to the notification rates among general population issued by official annual reports, it is noteworthy that the present analysis is the first study to describe a pooled estimate of notification rate of TB among migrants in China. For the many factors that could not be detected by meta-analysis, a further investigation on TB among migrants is needed to better characterize and understand behavioral and biological risk factors related to TB among migrants in China.
Supplementary information is linked to the online version of the paper on the Chinese Medical Journal website.
Financial support and sponsorship
This work was supported by the National Nature Science Foundation (No. 61571001, 91546203).
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank Jin-Kou Zhao of the Global Fund in Geneva, and Allison Rhines for language assistance. We also thank Pei-Pei Ding of Beijing Normal University, for her help in searching literature and in spatial analysis.
Footnotes
Edited by: Yi Cui
REFERENCES
- 1.Massey PD, Durrheim DN, Stephens N, Christensen A. Local level epidemiological analysis of TB in people from a high incidence country of birth. BMC Public Health. 2013;13:62. doi: 10.1186/1471-2458-13-62. doi: 10.1186/1471-2458-13-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ormerod LP. Further evidence supporting programmatic screening for, and treatment of latent TB Infection (LTBI) in new entrants to the UK from high TB prevalence countries. Thorax. 2013;68:201. doi: 10.1136/thoraxjnl-2012-202184. doi: 10.1136/thoraxjnl-2012-202184. [DOI] [PubMed] [Google Scholar]
- 3.Mor Z, Pinsker G, Cedar N, Lidji M, Grotto I. Adult tuberculosis in Israel and migration: Trends and challenges between 1999 and 2010. Int J Tuberc Lung Dis. 2012;16:1613–8. doi: 10.5588/ijtld.12.0296. doi: 10.5588/ijtld.12.0296. [DOI] [PubMed] [Google Scholar]
- 4.Jensen M, Lau A, Langlois-Klassen D, Boffa J, Manfreda J, Long R. A population-based study of tuberculosis epidemiology and innovative service delivery in Canada. Int J Tuberc Lung Dis. 2012;16:43–9. doi: 10.5588/ijtld.11.0374. doi: 10.5588/ijtld.11.0374. [DOI] [PubMed] [Google Scholar]
- 5.Shen X, Xia Z, Li X, Wu J, Wang L, Li J, et al. Tuberculosis in an urban area in China: Differences between urban migrants and local residents. PLoS One. 2012;7:e51133. doi: 10.1371/journal.pone.0051133. doi: 10.1371/journal.pone.0051133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Geneva: World Health Organization; 2013. WHO. Systematic Screening for Active Tuberculosis: Principles and Recommendations. [PubMed] [Google Scholar]
- 7.National Health and Family Planning Commission of the People's Republic of China. China Development Report in Floating Population. 2015 [Google Scholar]
- 8.Liu X, Jiang S, Li X, Jia L, Du X, Zhang H, et al. Provincial distribution of active tuberculosis patients in floating population in China. [Last accessed on 2016 Jun 8];Dis Surveill 2010. 2013 28:521–7. Available form: http://www.jbjc.org/EN/abstract/abstract7822> . [Google Scholar]
- 9.Beijing: 2006. Bureau of Global Fund TB Project in China. Tuberculosis Prevention and Control in Floating Population Implementation; p. 1. [Google Scholar]
- 10.Jia ZW, Jia XW, Liu YX, Dye C, Chen F, Chen CS, et al. Spatial analysis of tuberculosis cases in migrants and permanent residents, Beijing, 2000-2006. Emerg Infect Dis. 2008;14:1413–9. doi: 10.3201/1409.071543. doi: 10.3201/eid1409.071543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lu H, Chen J, Wang W, Wu L, Shen X, Yuan Z, et al. Efforts to reduce the disparity between permanent residents and temporary migrants: Stop TB experiences in Shanghai, China. Trop Med Int Health. 2015;20:1033–40. doi: 10.1111/tmi.12512. doi: 10.1111/tmi.12512. [DOI] [PubMed] [Google Scholar]
- 12.Zhou C, Chu J, Geng H, Wang X, Xu L. Pulmonary tuberculosis among migrants in Shandong, China: Factors associated with treatment delay. BMJ Open. 2014;4:e005805. doi: 10.1136/bmjopen-2014-005805. doi: 10.1136/bmjopen-2014-005805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ministry of Health, PRC. Health Standards of the People's Republic of China. Diagnostic Criteria for Pulmonary Tuberculosis. WS288-2008. [Last accessed on 2016 Jun 08]. Available from: http://www.moh.gov.cn/zwgkzt/s9491/200801/38801/files/987acb0232964ca1a9dcf833ad126a31.pdf .
- 14.Geneva, Switzerland: World Health Organization; 2015. WHO. Global Tuberculosis Report 2015; pp. 15–47. [Google Scholar]
- 15.China CDC. Public Health Scientific Data [EB/OL] [Last accessed on 2016 Mar 18]. Available from: <http://www.phsciencedata.cn/Share/ky_sjml.jsp?id=f90892b6.c000.48fe.a73e.a4c6db172385> .
- 16.Cheng S, Chen W, Yang Y, Chu P, Liu X, Zhao M, et al. Effect of diagnostic and treatment delay on the risk of tuberculosis transmission in Shenzhen, China: An observational cohort study, 1993-2010. PLoS One. 2013;8:e67516. doi: 10.1371/journal.pone.0067516. doi: 10.1371/journal.pone.0067516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Beijing: 2006. Group of Global fund China TB Control Project. Plan of TB Control in Floating Population; p. 3. [Google Scholar]
- 18.National Health and Family Planning Commission of the People's Republic of China. Administrative Measures on Prevention and Control of Tuberculosis [No. 92] 2013. [Last accessed on 2016 Jun 08]. Available from: <http://www.moh.gov.cn/mohzcfgs/s3576/201303/727b973d5ee4403ead07e1a2a22928f6.shtml> .
- 19.Wei X, Zou G, Yin J, Walley J, Yang H, Kliner M, et al. Providing financial incentives to rural-to-urban tuberculosis migrants in Shanghai: An intervention study. Infect Dis Poverty. 2012;1:9. doi: 10.1186/2049-9957-1-9. doi: 10.1186/2049-9957-1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Beijing: China Statistics Press; 2010. Population Census Office under the State Council. Tabulation on the 2010 population census of the people's republic of china. [Google Scholar]
- 21.Beijing: China Statistics Press; 2010. Population Census Office under the State Council. Tabulation on the 2010 population census of the people's republic of china. [Google Scholar]
- 22.Lv L. Effect of family, life and economic status on tuberculosis in migrant workers. Pract Prev Med. 2009;2:388–9. doi: 10.3969/j.issn.1006-3110.2009.02.030. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The notification rate during 2005–2013.
Notified rate on active TB (a) and smear-positive TB (b) among migrants by meta-analysis. TB: Tuberculosis.
Funnel plots of notified rate of active TB (a) and sputum smear-positive TB (b) among migrants TB: Tuberculosis.


