Pituicytoma is a distinct low-grade glioma arising from pituicytes of the neurohypophysis and infundibulum. Due to the rarity of this tumor, most of the reported cases in the literature were originally misdiagnosed as pituitary adenoma, meningiomas, and craniopharyngioma. It is of vital importance to accurately identify this tumor because this tumor, unlike pituitary adenomas, is prone to heavy bleeding during the surgical resection.[1]
Previous reports mostly focused on plain and contrast-enhanced (CE) images of magnetic resonance imaging (MRI) and computed tomography (CT). However, these imaging features are thought to be nonspecific. To date, there is only one report that mentioned dynamic gadolinium-enhanced images of pituicytoma and demonstrated early homogeneous enhancement of the tumor,[2] rather than the gradual enhancement commonly seen with pituitary adenomas.[3] However, this report did not obtain signal intensity-time curve (SITC) pattern of the tumor and could not compare it with the SITC pattern of normal adenohypophysis.
The study presents one case of pituicytoma with plain MRIs, SITC of dynamic contrast-enhanced MRI (DCE-MRI), and delayed CE MRIs. In addition, a review of eighty previously published cases was performed. Based on all 81 cases, we made a comprehensive analysis aiming to identify specific neuroimaging features of this kind of tumor, which might provide insights into the preoperative diagnosis of this unusual neoplasm.
A 44-year-old woman presented with dizziness, headache, and progressive bitemporal hemianopsia for about 1 month. She had no galactorrhea and menstrual irregularities. The results of laboratory studies, including hypophyseal function, were normal.
Preoperative MRIs were obtained with a dynamic T1-weighted turbo spin sequence using a 1.5T MR scanner (Achieva, Philips Medical Systems, Amsterdam, The Netherlands). The sequence parameters were repetition time/echo time, 393 ms/10 ms; flip angle, 90°; matrix size, 208 × 140; section thickness, 3 mm; and field of view, 180 mm × 180 mm. Twenty phases of coronal dynamic images were acquired every 6.3 s for a total imaging time of 126 s after a bolus injection of 0.1 mmol/kg gadopentetate dimeglumine-diethylenetriaminepentaacetic acid (GD-DTPA; Beijing BeiLu Pharmaceutical Co., Ltd., China). MRIs showed a 2.1 cm × 2.4 cm × 2.0 cm oval mass in the suprasellar cistern, inseparable from the infundibulum. The normal pituitary gland located inferiorly to the tumor, but the normal pituitary stalk was not well visualized. The mass was isointense to gray matter on both T1-weighted image (T1-WI) and T2-WI. In addition, the “bright spot” of the neurohypophysis was not visible on sagittal T1-WI [Figure 1a and 1b]. The SITC of the tumor showed rapid and initial strong enhancement followed by a decline in signal intensity (SI). In addition, the SITC pattern of the tumor was compared with that of neurohypophysis and adenohypophysis. It was similar to that of neurohypophysis [Figure 1c and 1d] and different from adenohypophysis. Time to peak of the tumor was on the 2nd to 3rd phase whereas time to peak of adenohypophysis was on the 4th phase which was later than that of the tumor [Figure 1e and 1f]. On delayed phase, the SI of tumor was lower than that of adenohypophysis.
Figure 1.
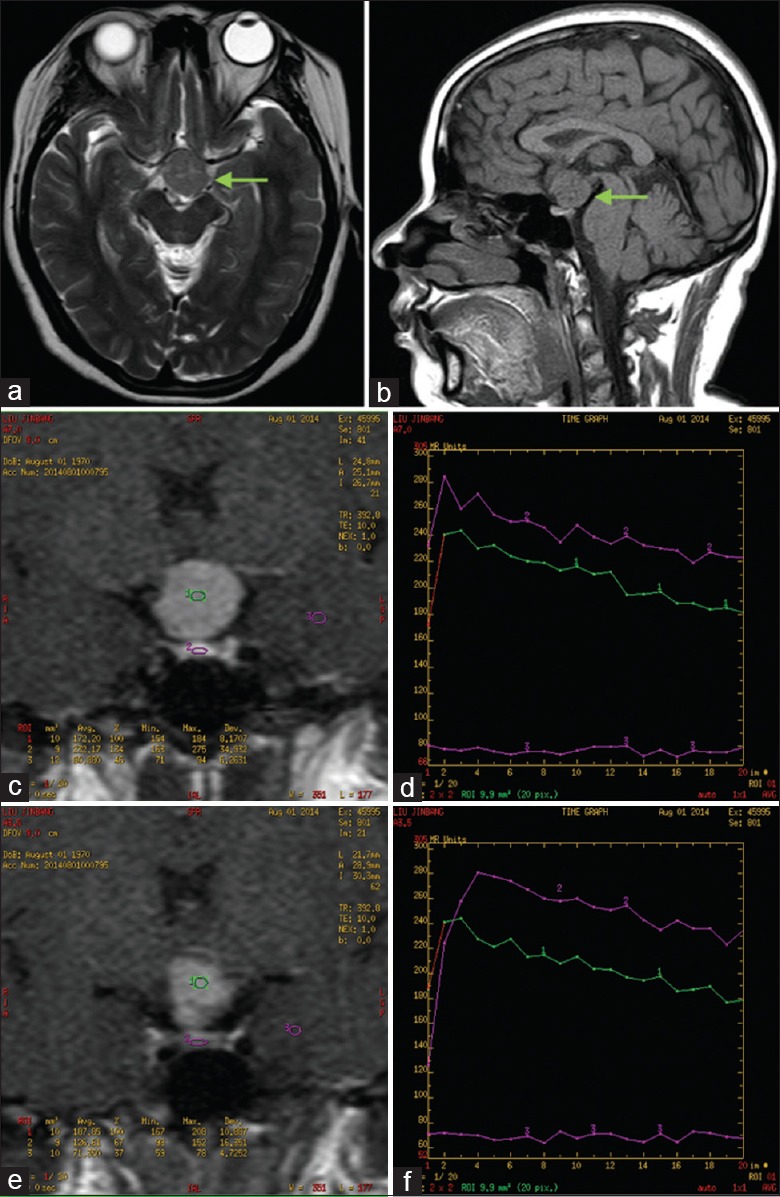
Plain scan magnetic resonance images (a and b) and SITC of pituicytoma (c-f). Axial T2-WI (a) and sagittal T1-WI (b) show an isointense, oval, well-demarcated mass in the suprasellar cistern (arrows). The “bright spot” of the neurohypophysis is absent. Coronal T1-WI on the slice of neurohypophysis (c) demonstrates three ROIs: 1 is tumor, 2 is neurohypophysis, and 3 is temporal lobe. (d) SITCs of three ROIs in (c): the SITC of the tumor is rapid and initial strong enhancement and it is similar to that of neurohypophysis. Coronal T1-WI on the slice of adenohypophysis (e) demonstrates three ROIs: 1 is the tumor, 2 is adenohypophysis, and 3 is temporal lobe. (f) SITCs of three ROIs in (c): Time to peak of the tumor is earlier than that of adenohypophysis. ROIs: Regions of interest; SITC: Signal intensity-time curve; T1-WI: T1-weighted image; T2-WI: T2-weighted image.
Solid tumor of suprasellar region was considered before operation. During the operation of transsphenoidal resection, a firm, pale-grayish, moderately vascular mass without obvious calcification was found attached to the pituitary stalk. A subtotal resection was performed to preserve the pituitary stalk. Histologically, the tumor cells showed a storiform-to-fascicular architecture. The shape of the tumor cells was short, spindle, or polygonal with eosinophilic cytoplasm [Figure 2a]. Immunohistochemically, the tumor cells were positive for vimentin, S-100 protein, thyroid transcription factor-1 [Figure 2b–2d], glial fibrillary acidic protein, epithelial membrane antigen, and estrogen receptor and negative for synaptophysin, chromogranin A, cytokeratin, and pituitary hormones. The Ki-67 labeling indices were about 1%. The final histopathological diagnosis was pituicytoma (WHO Grade I).
Figure 2.
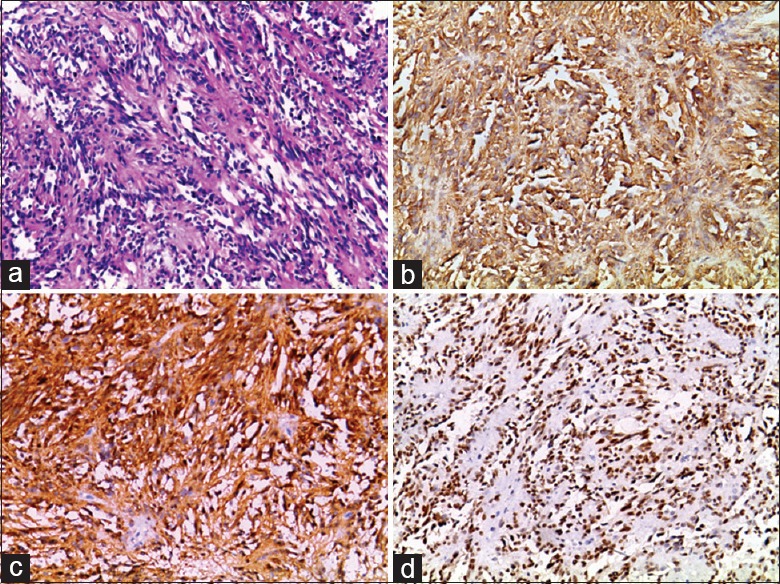
Histological and immunophenotypic features of pituicytoma in the present case. (a) A storiform-to-fascicular architecture (Hematoxylineosin staining, original magnification ×100). Tumor cells were positive for vimentin, S-100 protein, and thyroid transcription factor-1 (b-d, EnVasion, original magnification ×100).
A comprehensive PubMed search was performed using “pituicytoma” as a search term for the period between 1958 and March 2015. Based on this search, we identified a total of eighty cases.
The clinical presentation of this kind of tumors is typically chronic and progressive depending on the size and exact location of the lesions. Tumors were purely intrasellar in 12 cases (15%), purely suprasellar in 39 cases (49%), and mixed sellar/suprasellar in 29 cases (36%). Those located in the sella turcica typically mimic pituitary adenomas. Patients with suprasellar lesions usually presented with isolated visual symptoms, caused by the compression of the optic nerves.
Plain and CE imaging features of MRI and CT were reported in eighty cases. Among them, 16 cases performed CT scans and 74 performed MR scans. On CT and MRIs, the tumors appeared as solid, well-demarcated masses with rare calcifications and cystic component. Most of them demonstrated remarkable homogeneous enhancement after administration of contrast agent. In addition, the “bright spot” of the neurohypophysis was not visible on sagittal T1-WI in six cases.[1,4,5,6] Apart from this, one case mentioned dynamic gadolinium-enhanced images and demonstrated markedly homogeneous enhancement of the tumor on early phase by showing CE images of 30 s after contrast agent injection.[2] However, this report did not obtain SITC of the tumor due to insufficient temporal resolution.
In our patient, we also observed the absence of the high SI in the posterior pituitary lobe. In the vast majority of normal subjects, the posterior pituitary is seen as a hyperintense signal on sagittal T1-WI. This might be related to arginine vasopressin, which is transported from the hypothalamus through the neural component of the pituitary stalk, and stored in nerve terminals in the posterior pituitary.[7] This MRI finding of absence of “bright spot” in the neurohypophysis might be caused by stalk compression due to tumor growth. It suggests an infundibular or neurohypophyseal origin of the tumor, but not necessarily reflects neurohypophyseal dysfunction.[4]
This case reported on the SITC of pituicytoma using DCE-MRI rarely. In our case, the SITC pattern of the tumor is similar to that of neurohypophysis but different from adenohypophysis. Time to peak of the tumor is earlier than that of adenohypophysis. The difference in the SITC pattern between neurohypophysis and adenohypophysis lies in the way of the vascular supply: Pituitary has rich vascular supply and has no blood-brain barrier. The posterior pituitary lobe is supplied with blood predominantly by the inferior hypophyseal arteries. The median eminence and infundibulum are supplied with blood by the superior hypophyseal arteries. The main blood supply to the anterior lobe is through the portal venous system. Because the inferior hypophyseal arteries arise from the proximal portion of the internal carotid artery, the contrast agent will first reach the posterior pituitary lobe, then the infundibular stem, and finally the anterior pituitary lobe.[7] Therefore, pituicytomas which originate from neurohypophysis or pituitary stalk present earlier enhancement on SITC of DCE-MRI than pituitary adenomas which originate from adenohypophysis. This imaging feature is helpful to distinguish pituicytoma from pituitary adenoma if mass locates purely intrasellar or mixed sellar/suprasellar.
Differential diagnosis of pituicytoma includes pituitary macroadenoma, meningioma, craniopharyngioma, and other potential lesions of the hypothalamic-pituitary region. For a mass in the posterior aspect of the pituitary gland, clearly displacing the adenohypophysis forward and separating it from on MRI, pituicytoma could be considered prospectively. However, Covington et al.[8] noted that only 25% of pituicytomas were separable from the pituitary gland and the remainder appeared infiltrative of the underlying pituitary gland on MRI, which resulted in prospective diagnosis such as pituitary microadenomas or macroadenomas. In addition, it is also difficult to distinguish pituicytoma from pituitary macroadenomas for a mass occupying both sella turcica and suprasellar space. In these circumstances, SITC pattern of DCE-MRI will help differentiate pituicytomas from pituitary adenomas. Pituicytomas demonstrate rapid and early homogeneous enhancement, rather than the gradual enhancement commonly seen with pituitary adenomas. For a purely suprasellar enhancing solid lesion engulfing the infundibulum, both absence of posterior pituitary typical ’’bright spot’’ on sagittal MR T1-WI and absence of dural tail sign favor the diagnosis of pituicytoma.
In conclusion, this is a rare case report on the SITC pattern of pituicytoma. This specific imaging feature combined with plain and CE MRI and clinical presentation might help radiologists make accurate diagnosis before the operation, which can further surgeons setup appropriate preoperative treatment plan for patients.
Financial support and sponsorship
This work was supported by a grant from Yunnan Provincial applied basic research (Kunming Medical University combined special fund, No. 2013FB130).
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Peng Lyu
REFERENCES
- 1.Teti C, Castelletti L, Allegretti L, Talco M, Zona G, Minuto F, et al. Pituitary image: Pituicytoma. Pituitary. 2015;18:592–7. doi: 10.1007/s11102-014-0612-7. doi: 10.1007/s11102-014-0612-7. [DOI] [PubMed] [Google Scholar]
- 2.Katsuta T, Inoue T, Nakagaki H, Takeshita M, Morimoto K, Iwaki T. Distinctions between pituicytoma and ordinary pilocytic astrocytoma. Case report. J Neurosurg. 2003;98:404–6. doi: 10.3171/jns.2003.98.2.0404. [DOI] [PubMed] [Google Scholar]
- 3.Miki Y, Matsuo M, Nishizawa S, Kuroda Y, Keyaki A, Makita Y, et al. Pituitary adenomas and normal pituitary tissue: Enhancement patterns on gadopentetate-enhanced MR imaging. Radiology. 1990;177:35–8. doi: 10.1148/radiology.177.1.2399335. doi: 10.1148/radiology.177.1.2399335. [DOI] [PubMed] [Google Scholar]
- 4.Hammoud DA, Munter FM, Brat DJ, Pomper MG. Magnetic resonance imaging features of pituicytomas: Analysis of 10 cases. J Comput Assist Tomogr. 2010;34:757–61. doi: 10.1097/RCT.0b013e3181e289c0. doi: 10.1097/RCT.0b013e3181e289c0. [DOI] [PubMed] [Google Scholar]
- 5.Mao Z, Xiao W, Wang H, Li Z, Huang Q, He D, et al. Pituicytoma: Report of two cases. Oncol Lett. 2011;2:37–41. doi: 10.3892/ol.2010.209. doi: 10.3892/ol.2010.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chu J, Yang Z, Meng Q, Yang J. Pituicytoma: Case report and literature review. Br J Radiol. 2011;84:e55–7. doi: 10.1259/bjr/16529716. doi: 10.1259/bjr/16529716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maghnie M, Altobelli M, Di Iorgi N, Genovese E, Meloni G, Manca-Bitti ML, et al. Idiopathic central diabetes insipidus is associated with abnormal blood supply to the posterior pituitary gland caused by vascular impairment of the inferior hypophyseal artery system. J Clin Endocrinol Metab. 2004;89:1891–6. doi: 10.1210/jc.2003-031608. doi: 10.1210/jc.2003-031608. [DOI] [PubMed] [Google Scholar]
- 8.Covington MF, Chin SS, Osborn AG. Pituicytoma, spindle cell oncocytoma, and granular cell tumor: Clarification and meta-analysis of the world literature since 1893. AJNR Am J Neuroradiol. 2011;32:2067–72. doi: 10.3174/ajnr.A2717. doi: 10.3174/ajnr.A2717. [DOI] [PMC free article] [PubMed] [Google Scholar]


