Abstract
Air within the bladder wall, or bladder pneumatosis, is a very rare finding typically resulting from an infectious etiology, as in emphysematous cystitis (EC). However, there have been reports of bladder pneumatosis occurring without clear infectious origins. We present a case of a female patient found to have concurrent bladder and ileal pneumatosis secondary to a catastrophic vascular event. Prompt recognition of non-infectious etiologies of bladder pneumatosis is essential as this distinction may dramatically alter clinical decision-making.
Keywords: Bladder pneumatosis, Emphysematous cystitis
Introduction
Air within the bladder wall, or bladder pneumatosis, is a very rare finding typically resulting from an infectious etiology, as in emphysematous cystitis (EC). Major risk factors for EC include bladder dysfunction such as neurogenic bladder, and recurrent urinary tract infection (UTI). However, the strongest risk factor has been demonstrated to be diabetes mellitus (DM), seen in 2/3 of cases.1 There have been reports of bladder pneumatosis occurring without clear infectious origins.2 The pathogenesis of air within the bladder wall in these cases remains poorly understood but a process similar to pneumatosis intestinalis has been proposed.2 We present a case of bladder wall pneumatosis in a non-diabetic 73-year old woman.
Case presentation
A 73-year old woman presented to our emergency room from her nursing home with a chief complaint of three days of abdominal pain. On presentation, she denied nausea, vomiting, diarrhea, hematochezia, and melena. She had no prior history of abdominal surgery. She had not urinated since that morning, and a Foley catheter was placed which returned bloody urine. Of note, she had been recently hospitalized for non-ST elevation myocardial infarction (NSTEMI) and Takotsubo cardiomyopathy for which she underwent a coronary angiogram negative for occlusive disease. The procedure was completed via radial artery catheterization due to aorto-iliac occlusion. During that admission, she was treated with six days of broad-spectrum antibiotics for sepsis of unknown source and had a negative urine culture from her initial presentation.
The patient's past medical history included bipolar disorder, atrial fibrillation and aorto-iliac occlusive disease for which she was taking warfarin. There was no history of diabetes mellitus. On physical exam, she had a temperature of 97.7°F, a blood pressure of 138/66 mm Hg, and a heart rate of 124 beats per minute. The abdomen was soft and diffusely tender with no guarding. The bladder was not palpable and no masses were appreciated. The patient had cool bilateral lower extremities with no palpable pulses. She was alert, but not oriented.
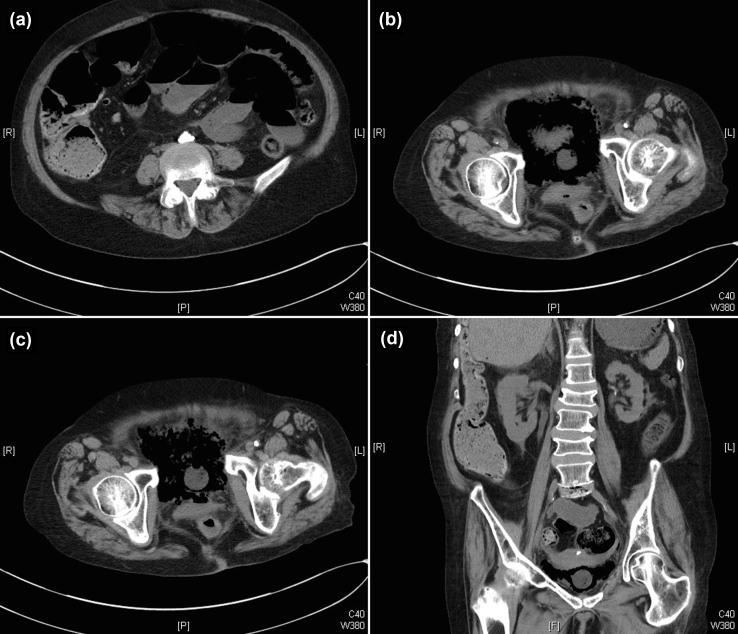
Laboratory evaluation showed a white blood cell count of 13.0 × 103/μL, a blood glucose of 136 mmol/L, a serum creatinine of 2.3 mg/dL and a blood urea nitrogen of 58 mg. Macroscopically, the urine was grossly bloody, and microscopic urinalysis was positive for nitrites, with 2+ leukocyte esterase. There was significant coagulopathy with PTT and INR >200 and >18, respectively. A computed tomography scan of the abdomen and pelvis without contrast was performed and was significant for diffusely dilated small bowel and ileal loops demonstrated pneumatosis. Severe atherosclerotic disease of the aorta and iliac arteries was noted, with stable chronic appearing occlusion of the distal aorta and iliac arteries. Additionally, there was diffuse bladder wall pneumatosis with a small amount of free air present peri-vesically (Fig. 1).
Figure 1.
Transverse and coronal views of the pelvis on CT imaging showing pneumatosis of the bladder wall as well as pneumatosis in ileal loops. (a) obstruction of aortic bifurcation, dilated bowel loops and ileal pneumatosis; (b, c) gas within bladder and bladder pneumatosis; (d) pneumatosis present in ascending colon.
The working diagnosis was a catastrophic vascular insult to multiple organs secondary to an arterial thromboembolic event with concordant multi-system organ failure. There was a family meeting and given the likely extent of intraabdominal injury, the patient was given comfort measures and transferred to inpatient hospice. She expired shortly thereafter and no autopsy was completed at the family request.
Discussion
EC is a rare condition of the urinary tract due to infection of the bladder with gas-forming bacteria. Reviews of reported cases have shown that cases are more common in elderly women (64% vs 36% in men) with a mean age of 66.3 The strongest risk factor for EC is DM.1 The clinical presentation can vary widely, but abdominal pain, irritative voiding symptoms, pneumaturia, and even an acute abdomen can be seen.3
However, this case did not appear to be a typical example of EC. Our patient was non-diabetic, and blood glucose measured at the time of the consult was only mildly elevated at 136 mmol/L. Furthermore, imaging revealed pneumatosis simultaneously in the wall of the ileum. Air appearing both in the bladder wall and in the ileum has not been reported in previously published reviews of EC.1, 3 The finding of intestinal pneumatosis on CT imaging is widely used as an indicator acute mesenteric ischemia.4 Alternatively, bladder wall pneumatosis has not been previously linked with ischemic disease of the bladder in our review of the literature.
In this patient, the constellation of multiple-organ pneumatosis in the absence of diabetes or other risk factors for EC suggests that vascular disease may be the causative factor in the development of bladder pneumatosis. Ischemia of the bladder may allow for increased translocation of bacteria into the bladder wall, by a similar mechanism to that seen in intestinal ischemia.5 Furthermore, our patient had atrial fibrillation, aorto-iliac occlusive disease, and had significantly coagulopathy at the time of presentation, increasing the concern for thromboembolic disease to multiple vascular beds. This case suggests that for patients with known vascular risk factors presenting with abdominal or urinary complaints, the finding of bladder pneumatosis may indicate diffuse vascular insult rather than EC.
Conclusion
Bladder wall pneumatosis is an uncommon clinical finding that is not always associated with an infectious etiology. The distinction between causative factors is important because management considerations for a presumed case of EC may be very different than those indicated for an underlying systemic vascular event as was seen in this patient. Clinicians should be aware of this distinction and should interpret the finding of air within the bladder wall in the context of the patient's overall clinical picture.
Disclosures
The authors report no relative financial disclosures. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
There was no conflict of interest for any of the authors included in this report.
References
- 1.Amano M., Shimizu T. Emphysematous cystitis: a review of the literature. Intern Med. 2014;53:79–82. doi: 10.2169/internalmedicine.53.1121. [DOI] [PubMed] [Google Scholar]
- 2.Medina-Polo J., Nunez-Sobrino J.A., Diaz-Gonzalez R. An unusual case of air within the bladder wall: bladder pneumatosis? Int J Urol. 2011;18:375–377. doi: 10.1111/j.1442-2042.2011.02748.x. [DOI] [PubMed] [Google Scholar]
- 3.Thomas A.A., Lane B.R., Thomas A.Z. Emphysematous cystitis: a review of 135 cases. BJU Int. 2007;100:17–20. doi: 10.1111/j.1464-410X.2007.06930.x. [DOI] [PubMed] [Google Scholar]
- 4.Aschoff A.J., Stuber G., Becker B.W. Evaluation of acute mesenteric ischemia: accuracy of biphasic mesenteric multi-detector CT angiography. Abdom Imaging. 2009;34:345–357. doi: 10.1007/s00261-008-9392-8. [DOI] [PubMed] [Google Scholar]
- 5.Renner P., Kienle K., Dahlke M.H. Intestinal ischemia: current treatment concepts. Langenbecks Arch Surg. 2011;396:3–11. doi: 10.1007/s00423-010-0726-y. [DOI] [PubMed] [Google Scholar]