Abstract
Hyponatremia with hyperkalemia in infancy is a rare presentation, but may be due to aldosterone deficiency or end organ resistance to its action. There are few cases associating this condition with urinary tract infections or anatomic abnormalities that predispose to infection. Clinicians should have a high index of suspicion in diagnosing secondary pseudohypoaldosteronism (PHA) due to its often atypical presentation. We describe ten month-old infant who presented with this condition and was found to have urinary tract infection complicating unilateral urinary tract anomaly, which may have strong association with renal tubular resistance to aldosterone.
Keywords: Hyponatremia, Hyperkalemia, Pseudohypoaldosteronism, Urinary tract infections, Urinary tract anomalies
Introduction
Hyponatremia with hyperkalemia is uncommon in infancy, but is a medical emergency that can cause life-threatening cardiac arrhythmias. These abnormalities may be due to congenital adrenal hyperplasia (CAH) that results from lack of 11- or 21-hydroxylase which are required for the synthesis of the mineralocorticoid, aldosterone. Other causes for impaired mineralocorticoid secretion or response may exist, particularly in infants one month of age or older. Such causes are PHA, congenital adrenal hypoplasia, isolated aldosterone deficiency and medication.1 PHA is classified into Type 1 and Type 2, which is characterized by hypertension and hyperkalemia. Type 1 is further sub-classified into primary and secondary (transient) PHA. The underlying pathology in Type 1 primary PHA is mutation in the amiloride-sensitive epithelial sodium channel gene or mineralocorticoid receptor mutation.1, 2 This causes end organ resistance to mineralocorticoids. Type 1 secondary (transient) PHA is strongly associated with urinary tract infections (UTI) complicating structural urinary tract anomalies.3, 4 We report an infant who presented with profound hyponatremia in the setting of urinary infection accompanied by structural abnormalities of the urinary tract. Subsequent to antibiotic therapy that cleared the infection, the electrolyte disturbances resolved, and required no ongoing therapy. We attribute these findings to Type 1 secondary (transient) PHA. The case demonstrates that the strongest predisposition for the development of aldosterone resistance or secondary PHA is the existence of severe urinary tract infection5 or more frequently urinary infection complicating structural urinary tract anomalies.
Case presentaion
A 10 month-old girl with an unremarkable birth history presented with failure to thrive. Investigation revealed a sodium of 103 mmol/L, potassium 6 mmol/L. She had a non-anionic gap, metabolic acidosis and her transtubular potassium gradient (TTKG) was < 3 (normal 8 – 9) indicating reduced urinary potassium excretion. The urine sodium was < 25 mmol/L. Infusion of 3% saline partially corrected the hyponatremia. With the addition of fludrocortisone her electrolytes normalized within 24 h.
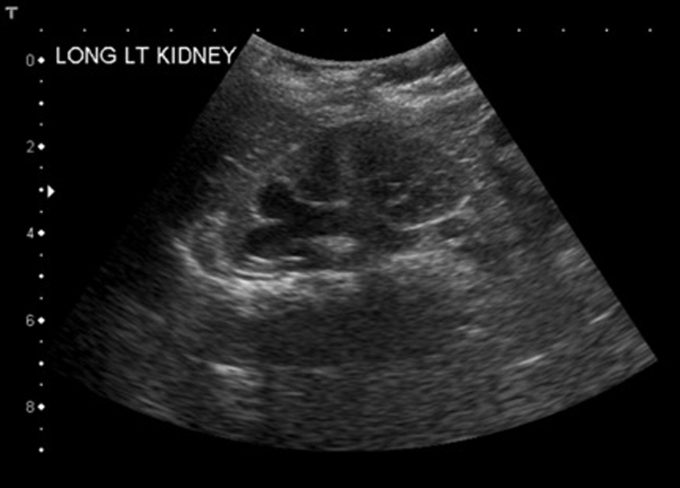
Urinalysis revealed leukocytes and nitrites. Escherichia coli was isolated from the urine culture. 21-hydroxylase and cortisol were normal. Aldosterone was elevated at 308.3 ng/dL (normal 5 – 80 ng/dL), implying tubular unresponsiveness. Renal imaging detected a duplicated left collecting system (Fig. 1) with an upper pole ectopic ureter that extended to the bladder neck and refluxed during voiding. Patient was treated with ceftriaxone for two days and discharged home on amoxicillin/clavulanate for two weeks. In the ensuing months, she tolerated weaning from fludrocortisone without recurrence of the electrolyte disturbances. Later, an upper pole nephroureterectomy was performed. Subsequent growth has been normal.
Figure 1.
Renal ultrasonography showing duplicated left collecting system.
Discussion
The primary function of aldosterone is reabsorption of sodium and water at the expense of potassium in the distal renal tubule. Deficiency of aldosterone or end organ resistance to its actions leads to hyponatremia, hypovolemia, hyperkalemia and metabolic acidosis. The key finding in Type 1 PHA is an elevated serum aldosterone level with hyponatremia and hyperkalemia. One should have a high index of suspicion for this diagnosis especially in infants. The least rare cause for Type I PHA is CAH due to 11- or 21-hydroxylase deficiency. Still rarer are congenital adrenal hypoplasia and isolated aldosterone deficiency. PHA can occur with nephrotoxic medications such as angiotensin converting enzyme inhibitors, non-steroidal anti-inflammatory drugs and beta-blockers.1, 4 Today almost all states include CAH in the newborn metabolic screen. Type 1 secondary (transient) PHA is strongly associated with urinary tract infections in the setting of urinary anomalies,3 which differentiates it from Type 1 (genetic) PHA. Our patient's UTI with renal anomaly, a unilateral defect, makes the finding of PHA especially surprising. There are, however, several reports of transient PHA in infancy, some of which also had unilateral disease. Nandagopal et al.,1 reported four infants with failure to thrive, hyponatremia, hyperkelemia and unilateral renal anomalies with urinary infections. These patients, like our patient, exhibited transient renal tubular resistance to mineralocorticoids. We speculate that severe renal inflammation may cause transient tubular resistance to aldosterone independent of structural anomaly.5 Also, the fact that addition of fludrocortisone in our patient causes rapid correction of electrolytes implies that high levels of mineralocorticoids may overcome transient tubular resistance.
Our patient demonstrated that renal tubular resistance to aldosterone can be caused by a urinary tract infection complicating congenital urinary tract anomalies. In the setting of an infant with hyponatremia, serum aldosterone, urine sodium, and urine cultures should be obtained. Renal imaging (ultrasound) is indicated in children under age six months with atypical UTI irrespective of type 1 PHA and in children over six months old who have a UTI and type 1 PHA.4
Conclusion
-
1)
Transient PHA should be considered in infants presenting with hyponatremia and hyperkalemia, even though genetic CAH has been excluded on newborn metabolic screening.
-
2)
Urinary tract infection may occur without fever.
-
3)
Evaluation of an infant with urinary tract infection should include serum electrolytes.
-
4)
Urinary tract imaging is indicated in children aged less than six months with atypical UTI irrespective of Type 1 PHA and in children over age six months with a UTI and Type 1 PHA.
Consent
Informed consent was obtained for publication.
Conflict of interest
The authors have no conflicts of interest.
References
- 1.Nandagopal R., Vaidyanathan P., Kaplowitz P. Transient pseudohypoaldosteronism due to urinary tract infection in infancy: a report of 4 cases. Int J Pediatr Endocrinol. 2009;2009:195728. doi: 10.1155/2009/195728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Geller D.S., Rodriguez-Soriano J., Vallo Boado A. Mutations in the mineralocorticoid receptor gene cause autosomal dominant pseudohypoaldosteronism type I. Nat Genet. 1998;19:279–281. doi: 10.1038/966. [DOI] [PubMed] [Google Scholar]
- 3.Melzi M.L., Guez S., Sersale G. Acute pyelonephritis as a cause of hyponatremia/hyperkalemia in young infants with urinary tract malformations. Pediatr Infect Dis J. 1995;14:56–59. doi: 10.1097/00006454-199501000-00012. [DOI] [PubMed] [Google Scholar]
- 4.Manikam L., Cornes M.P., Kalra D. Transient pseudohypoaldosteronism masquerading as congenital adrenal hyperplasia. Ann Clin Biochem. 2011;48:380–382. doi: 10.1258/acb.2011.010264. [DOI] [PubMed] [Google Scholar]
- 5.Gerigk M., Glanzmann R., Rascher W. Hyponatraemia and hyperkalaemia in acute pyelonephritis without urinary tract anomalies. Eur J Pediatr. 1995;154:582–584. doi: 10.1007/BF02074840. [DOI] [PubMed] [Google Scholar]