Abstract
Objective:
To assess a comprehensive multicomponent intervention against a low intensity intervention for promoting physical activity in chronic low back pain patients.
Design:
Randomised controlled trial.
Setting:
Inpatient rehabilitation and aftercare.
Subjects:
A total of 412 patients with chronic low back pain.
Interventions:
A multicomponent intervention (Movement Coaching) comprising of small group intervention (twice during inpatient rehabilitation), tailored telephone aftercare (twice after rehabilitation) and internet-based aftercare (web 2.0 platform) versus a low level intensity intervention (two general presentations on physical activity, download of the presentations).
Main measures:
Physical activity was measured using a questionnaire. Primary outcome was total physical activity; secondary outcomes were setting specific physical activity (transport, workplace, leisure time) and pain. Comparative group differences were evaluated six months after inpatient rehabilitation.
Results:
At six months follow-up, 92 participants in Movement Coaching (46 %) and 100 participants in the control group (47 %) completed the postal follow-up questionnaire. No significant differences between the two groups could be shown in total physical activity (P = 0.30). In addition to this, workplace (P = 0.53), transport (P = 0.68) and leisure time physical activity (P = 0.21) and pain (P = 0.43) did not differ significantly between the two groups. In both groups, physical activity decreased during the six months follow-up.
Conclusions:
The multicomponent intervention was no more effective than the low intensity intervention in promoting physical activity at six months follow-up. The decrease in physical activity in both groups is an unexpected outcome of the study and indicates the need for further research.
Keywords: Physical activity promotion, low back pain, rehabilitation
Introduction
The benefit of regular physical activity in primary and secondary prevention as well as in the rehabilitative treatment of several non-communicable diseases has been scientifically proven.1–4 Particularly those people with chronic health conditions are considered to be insufficiently, physically active.5,6 Physical activity is also an integral part of musculoskeletal rehabilitation in low back pain patients and is therefore widely recommended as a successful therapy for that patient group.7,8
However, studies have shown that it is a common problem for patients to adhere to self-directed exercise and to implement a health-enhancing physical activity into a daily routine following rehabilitation. Only a few patients integrate health-enhancing physical activity and/or sport activities into their lifestyles thus demonstrating the relevance of interventions that promote physical activity.9
Within the healthcare setting, different strategies have been used to promote physical activity. Strategies in physical activity promotion can be broadly separated into advice, behavioural-oriented counselling, providing written materials, exercise referral schemes, and disease specific rehabilitation programmes including exercise therapy.6,10,11 In addition to these, long-term interventions such as telephone-based and internet-based interventions, and mailed support have gained importance. Furthermore, current research discusses whether individually tailored interventions are more effective than standard interventions.12,13 Overall, independent of the chosen intervention strategy, it is recognized that the didactics of information delivery should be based on valid behaviour change methods (e.g., social cognitive theory and the transtheoretical model) which set clear and realistic goals and use simple and specific messages.2
At present, it is not known which method or strategy of physical activity promotion works best. 14,15 However, it seems that comprehensive and high-quality interventions, using additional exercise prescriptions and booster strategies, achieved the most significant long-term increases in physical activity behaviour.15 For this reason, further research is needed in order to identify the most effective strategies in physical activity promotion and to accumulate evidence on physical activity promotion in healthcare.
Within the scope of this study, two different strategies of physical activity promotion were compared within the rehabilitation setting. Owing to the high prevalence of chronic low back pain patients in inpatient orthopaedic rehabilitation in Germany, and due to the fact that the ultimate aim of exercise therapy is to lead patients into an active lifestyle,16,17 this indication was considered relevant for the study. The aim of the present study was to evaluate the effectiveness of a multicomponent approach in physical activity promotion (Movement Coaching) compared with a low intensity intervention six months after inpatient rehabilitation.
Methods
The study protocol for this research project has already been described elsewhere.18 Ethical approval was granted by German Sport University Ethics Committee and the study was conducted in compliance with the Helsinki Declaration.
Study design and study population
The present evaluation is based on a single centre randomised controlled trial with two measuring points: T0 = start of inpatient rehabilitation (baseline); T1 = six months follow-up. Participants were recruited from an inpatient medical rehabilitation centre.
Eligible patients were invited to an informational meeting and voluntary participation in the study was offered. Eligibility criteria included: (1) age 18 to 65 years; (2) starting an inpatient medical rehabilitation treatment due to low back pain. Exclusion criteria included: (1) cognitive disorders; (2) insufficient understanding of the German language; (3) previous surgery within the last three months; (4) posttraumatic conditions (e.g., LBP following an accident); (5) a current state-pension claim.
As far as possible, the study was conducted single-blinded. That is, we informed patients that we employed two different approaches which promote physical activity and these two interventions were labelled Movement Coaching A and Movement Coaching B. Thus, the patients did not know if they were randomised into the intervention group (Movement Coaching) or control group (low intensity intervention). However, the therapist conducted both interventions and was therefore not blinded.
Written informed consent forms were obtained by all participants. Patients were recruited from May 2013 to April 2014. The six-month follow up was completed in October 2014.
Intervention
The intervention (Movement Coaching) was designed as a multicomponent approach and comprised of three different components: face-to-face contact (small group intervention, twice during inpatient rehabilitation), a tailored telephone aftercare (8 weeks and 12 weeks after rehabilitation) and an Internet-based aftercare (web 2.0 platform; available up to six months after rehabilitation). For further information about the main objectives, the theoretical foundations of the intervention and differences between the two interventions, see Schaller et al.18
Control intervention
The control intervention was designed as a low intensity intervention merely comprising of two general presentations on physical activity during inpatient rehabilitation which could be downloaded from a homepage during aftercare. Differences and similarities of the two intervention strategies are presented in Table 1.
Table 1.
Similarities and differences of Movement Coaching and low intensity intervention.
| Commonalities | ||
|---|---|---|
| Main objective | Increasing physical activity after inpatient rehabilitation | |
| Indication | Chronic low back pain (inpatient rehabilitation) | |
| Coach | Same person conducting Movement Coaching and control intervention | |
| Differences | ||
| Low intensity intervention | Movement Coaching | |
| Inpatient rehabilitation | ||
| Methodology and didactics | Lecture | Interactive; solution-oriented coaching |
| Duration | 2 x 30 min | 2 x 60 min |
| Maximum group size | 30 patients | 8 patients |
| Aftercare | ||
| Homepage: Download of lectures | Tailored telephone intervention (at least twice) | |
| Interactive web 2.0 platform | ||
Outcomes
Patients answered a questionnaire on physical activity, sociodemographic and clinical variables. Following the informational meeting about the study, patients answered the baseline questionnaire at the beginning of inpatient rehabilitation. The outcome data at six months were collected using a postal questionnaire.
Physical activity was operationalized by the Global Physical Activity Questionnaire,19,20 which collects information on both physical activity during a typical week within three settings (workplace, transport and leisure time) as well as on sedentary behaviour. We chose total physical activity (MET-min/week) as our primary outcome because the Global Physical Activity Questionnaire measures leisure time and workplace physical activities with respect to their intensity by multiplying the minutes per week for each domain by their associated MET to give the MET-min scores. Activity specific scores are summed to give the total MET-min/week. Thereby, each minute of vigorous physical activity is multiplied by 8 METs and each minute of moderate physical activity by 4 METs. The metabolic equivalent (MET) is a physiological measure expressing the expended energy of physical activities. MET is defined as the ratio of the rate of energy consumption during a specific physical activity to a reference metabolic rate.
Bull et al.20 showed a moderate to strong positive relationship of the Global Physical Activity Questionnaire with the International Physical Activity Questionnaire (concurrent validity: Spearman’s rho 0.45 – 0.65), and the reliability was of moderate to substantial strength (kappa 0.67 to 0.73; Spearman’s rho 0.67 to 0.81) (20). Compared to the accelerometer data, the Global Physical Activity Questionnaire provided low-to-moderate validity and generally acceptable evidence of reliability.21
As secondary outcomes, leisure time (MET-min/week), workplace (MET-min/week) and transport physical activity (MET-min/week) as well as pain were evaluated. The intensity of pain during the last four weeks was measured via a question from the SF-36 questionnaire (“How much bodily pain have you had during the past 4 weeks?”; answering on a scale from 1 to 6).22
Further variables
Sociodemographic and indication-related variables include gender, age (in years), level of education (“lower secondary school”/“higher level of education than lower secondary school”), body mass index (BMI) and the duration of LBP at the beginning of inpatient rehabilitation (⩽12 months / >12 months).
Statistical analysis
In order to describe the sample, the means and standard deviations (SD) were calculated for continuous data, and frequency tables (n; %) for the categorical data. Due to the skewed distribution, the median, 25% quartile and 75% quartile were also presented for physical activity data. Differences in the baseline characteristics between the intervention group (Movement Coaching) and the control group (low intensity intervention) were tested using the Mann–Whitney U-test (age, BMI, and pain intensity, leisure time physical activity, workplace physical activity, transport physical activity, total physical activity) and the chi-squared test (gender, education level, and duration of low back pain).
To identify the differences between the patients who replied (reply to six month follow-up) and those patients who did not reply (non-reply to six month follow-up) to the postal six months follow-up questionnaires, both the sociodemographic and clinical variables as well as the setting specific baseline physical activity were included as independent variables in the equation of a binary logistic regression model for adjusted evaluation.
A base-case analysis was performed using data restricted to those patients who replied to the postal six month follow-up questionnaire. Here, compliance with the intervention was not considered.
To explore the robustness of the results, two intention-to-treat analyses were performed using two approaches to impute missing data. Since the effectiveness of physical activity promotion is considered controversial,10,14,23 we decided to take a conservative approach in the intention-to-treat analyses. The first intention-to-treat analysis (ITTLOCF) was performed assuming “last observation carried forward”: if six months follow-up data were missing, it was assumed that the physical activity and pain data were the same as at baseline. In the second intention-to-treat analysis (ITTworst), we assumed a “worst case” scenario for physical activity at six months follow-up (0 MET-min/week) and pain (“6”).
The Global Physical Activity Questionnaire data were checked for possible data entry errors by using the CleanRecode program provided by WHO. In comparison, the effectiveness of Movement Coaching and the low intensity intervention was evaluated by considering the total physical activity in both groups at six months follow-up.
Furthermore, the comparisons between group differences in the secondary outcomes (pain, leisure time physical activity, workplace physical activity, transport physical activity) and those between group differences over the course of time (Δ = six months follow-up (T1)- baseline (T0)) were tested using the Mann–Whitney U-test. The analysis also reported the means, standard deviations (SD), medians, the 25% quartiles and 75% quartiles.
Subject differences from baseline to six months follow up were tested using the Wilcoxon Test.
To calculate the sample size, we assumed a difference of 360 MET-min/week between the groups. This corresponds to 90 minutes physical activity with moderate intensity which, from the perspective of rehabilitation practitioners, is assumed to be a relevant difference in order to gain a health enhancing effect of physical activity.
We estimated the variance for the sample size calculation from the results of a survey of physical activity in the German population.24 Sample size was calculated based on a significance level of α = 0.05; power (1-β) = 0.80 and an estimated variance of 1.04. We increased the sample size by 5 % because of the high probability for applying a non-parametric test, and we estimated a total of 277 patients for the comparison of two independent groups. By estimating a loss to follow-up of 35 % during the twelve months period, we calculated a total sample size of 372 patients, 186 patients per group, respectively.
For all statistical tests, the significance level was set to P < 0.05. All analyses were run with IBM SPSS Statistics 20.
Results
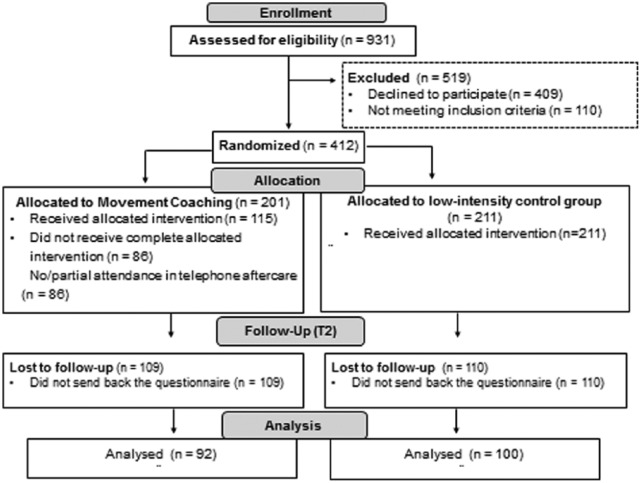
Informed consent and the baseline questionnaires were given by 412 patients who were assessed for eligibility (44 %). At six months follow-up, 46 % of the Movement Coaching and 47 % of the control groups completed the questionnaire. Overall, it was possible to analyse 192 questionnaires. Figure 1 shows the CONSORT flow diagram illustrating the progress through the phases of the present study.
Figure 1.
CONSORT flow-chart.
Sample description
The sample consisted of 286 men and 126 women. There were no significant differences between the control group and the intervention group (Movement Coaching) regarding either the sociodemographic and indication-related variables or the baseline physical activity. In both groups, workplace physical activity was higher than transport and leisure time physical activity. The initial characteristics of the patients are shown in Table 2.
Table 2.
Baseline characteristics of the sample.
| Movement Coaching (n = 201) | Control group (n = 211) | P | ||
|---|---|---|---|---|
| Age (years) (n = 406) | mean (SD) | 49.7 (±8.3) | 51.1 (±7.8) | 0.13a |
| Gender: men (n = 412) | n (%) | 143 (71.1 %) | 143 (67.8 %) | 0.32b |
| Body Mass Index (BMI) (n = 383) | mean (SD) | 28.9 (±5.3) | 29.8 (±5.9) | 0.08a |
| Highest level of education “lower secondary school” (n = 399) | n (%) | 101 (50.3 %) | 113 (53.5 %) | 0.62b |
| Duration of low back pain > 12 months (n = 400) | n (%) | 168 (83.6 %) | 175 (82.9 %) | 0.58b |
| Total physical activity (MET-min/week)c (n = 412) | mean (SD) | 7654 (±8527) | 6865 (±8779) | 0.30a |
| median [25%; 75%]- percentile | 3600 [480; 13260] | 2640 [480; 11880] | ||
| Workplace physical activity (MET-min/week)c (n = 412) | mean (SD) | 5903 (±7824) | 5330 (±8101) | 0.27a |
| median [25%; 75%]- percentile | 1800 [0; 10920] | 384 [0; 8640] | ||
| Leisure time physical activity (MET-min/week)c (n = 412) | mean (SD) | 985 (±2179) | 790 (±1519) | 0.99a |
| median [25%; 75%]- percentile | 0 [0; 1080] | 0 [0; 960] | ||
| Transport physical activity (MET-min/week)c (n = 412) | mean (SD) | 766 (±1516) | 743 (±1867) | 0.35a |
| median [25%; 75%]- percentile | 0 [0; 1020] | 0 [0; 600] | ||
| Intensity of pain during the last four weeks (minimum=1; maximum=6) (n = 378) | mean (SD) | 4.5 (±1.0) | 4.6 (±0.9) | 0.10a |
| median [25%; 75%]- percentile | 5.0 [4.0; 5.0] | 5.0 [4.0; 5.0] |
Mann-Whithney-U-Test; bPearson-Chi-Quadrat; cMET = metabolic equivalent; significance level P < 0.05.
The adjusted binary logistic regression model, including the baseline data, showed no significant differences between the patients that replied to the six month follow-up questionnaire and those patients who did not reply (see Table 3).
Table 3.
Differences between patients that replied to the six month follow-up questionnaire and the patients who did not reply in baseline data.
| Reply (n = 192) | Non-reply (n = 220) | P a | ||
|---|---|---|---|---|
| Group (Movement Coaching) | n (%) | 92 (48 %) | 109 (49 %) | 0.42 |
| Age (years) | mean (SD) | 51.3 (7.3) | 49.6 (8.6) | 0.08 |
| Gender: men | n (%) | 126 (66 %) | 160 (73 %) | 0.18 |
| Body Mass Index (BMI) | mean (SD) | 28.8 (5.0) | 29.8 (6.1) | 0.15 |
| Highest level of education “lower secondary school” | n (%) | 100 (53 %) | 114 (52 %) | 0.93 |
| Duration of low back pain > 12 months | n (%) | 25 (12 %) | 32 (15 %) | 0.83 |
| Intensity of pain during the last four weeks (minimum=1; maximum=6) | mean (SD) | 4.5 (±1.0) | 4.7 (±0.9) | 0.20 |
| Median [25%; 75%]- percentile | 5.0 [4.0; 5.0] | 5.0 [4.0; 5.0] | ||
| Workplace physical activity (MET-min/week)b | mean (SD) | 5105 (±7501) | 6050 (±8337) | 0.57 |
| Median [25%; 75%]- percentile | 1020 [0; 8400] | 432 [0; 10800] | ||
| Leisure time physical activity (MET-min/week)b | mean (SD) | 997 (±1855) | 788 (±1883) | 0.67 |
| Median [25%; 75%]- percentile | 360 [0; 960] | 0 [0; 960] | ||
| Transport physical activity (MET-min/week)b | mean (SD) | 826 (1662) | 692 (1739) | 0.43 |
| Median [25%; 75%]- percentile | 0 [0; 960] | 0 [0; 690] | ||
| Total physical activity (MET-min/week)b | mean (SD) | 6928 (±8089) | 7530 (±9131) | 0.70 |
| Median [25%; 75%]- percentile | 3420 [735; 11250] | 3024 [45; 13800] |
Adjusted binary logistic regression model; bMET = metabolic equivalent; *significant at the significance level < 0.05; R2 = 0.05.
Six months follow-up data
At the six months follow-up (Table 4), both base case (patients that replied to the six month follow-up questionnaire) as well as the two intention-to-treat scenarios showed no significant differences between the two groups regarding total physical activity.
Table 4.
Six months follow-up data.
| Movement Coaching | Control group | P a | ||
|---|---|---|---|---|
| Base case (patients that replied to the six month follow-up questionnaire) (n = 192) | (n = 92) | (n = 100) | ||
| Total physical activity (MET-min/week)d | mean (SD) | 2207 (±3613) | 2134 (±4124) | 0.30 |
| Median [25%; 75%]- percentile | 1260 [435; 2670] | 990 [285; 2518] | ||
| Workplace physical activity (MET-min/week)d | mean (SD) | 1559 (±3498) | 1583 (±3952) | 0.53 |
| Median [25%; 75%]- percentile | 480 [0; 1800] | 360 [0; 1673] | ||
| Leisure time physical activity (MET-min/week)d | mean (SD) | 342 (±419) | 266 (±291) | 0.21 |
| median [25%; 75%]- percentile | 270 [60; 428] | 180 [68; 360] | ||
| Transport physical activity (MET-min/week) | mean (SD) | 287 (±508) | 296 (±509) | 0.68 |
| median [25%; 75%]- percentile | 120 [0; 300] | 120 [0; 405] | ||
| Intensity of pain during the last four weeks (minimum 1; maximum: 6) | mean (SD) | 3.5 (1.3) | 3.7 (1.2) | 0.43 |
| median [25%; 75%]- percentile | 4.0 [2.0; 4.0] | 4.0 [3.0; 4.0] | ||
| ITTLOCFb (n=412) | (n = 201) | (n = 211) | ||
| Total physical activity (MET-min/week)d | mean (SD) | 4856 (±7150) | 5479 (±8321) | 0.96 |
| median [25%; 75%]- percentile | 1830 [360; 5760] | 1560 [260; 5940] | ||
| Workplace physical activity (MET-min/week)d | mean (SD) | 3719 (±6321) | 4350 (±7758) | 0.64 |
| median [25%; 75%]- percentile | 540 [0; 4260] | 330 [0; 3600] | ||
| Leisure time physical activity (MET-min/week)d | mean (SD) | 658 (±1799) | 497 (±987) | 0.53 |
| median [25%; 75%]- percentile | 180 [0; 540] | 120 [0; 480] | ||
| Transport physical activity (MET-min/week)d | mean (SD) | 467 (±1212) | 547 (±1450) | 0.47 |
| median [25%; 75%]- percentile | 0 [0; 415] | 60 [0; 420] | ||
| Intensity of pain during the last four weeks (minimum 1; maximum 6) | mean (SD) | 4.0 (±1.2) | 4.2 (±1.2) | 0.08 |
| median [25%; 75%]- percentile | 4.0 [3.0; 5.0] | 4.0 [4.0; 5.0] | ||
| ITTworstc (n=412) | (n = 201) | (n = 211) | ||
| Total physical activity (MET-min/week)d | mean (SD) | 944 (±2597) | 910 (±2886) | 0.90 |
| median [25%; 75%]- percentile | 0 [0; 960] | 0 [0; 720] | ||
| Workplace physical activity (MET-min/week)d | mean (SD) | 675 (±2421) | 690 (±2717) | 0.67 |
| median [25%; 75%]- percentile | 0 [0; 220] | 0 [0; 180] | ||
| Leisure time physical activity (MET-min/week)d | mean (SD) | 153 (±328) | 122 (±237) | 0.79 |
| median [25%; 75%]- percentile | 0 [0; 240] | 0 [0; 150] | ||
| Transport physical activity (MET-min/week)d | mean (SD) | 130 (±371) | 137 (±376) | 0.62 |
| median [25%; 75%]- percentile | 0 [0; 100] | 0 [0; 120] | ||
| Intensity of pain during the last four weeks (minimum 1; maximum 6) | mean (SD) | 4.9 (±1.5) | 4.9 (±1.4) | 0.71 |
| median [25%; 75%]- percentile | 6.0 [4.0; 6.0] | 6.0 [4.0; 6.0] | ||
Mann-Whithney-U-Test; significance level P < 0.05; bITTLOCF: if six months follow-up data were missing, it was assumed that the physical activity and pain data were the same as at baseline; cITTworst: if six months follow-up data were missing, 0 MET-min/week was assumed for physical activity, and “6” was assumed for pain; dMET = metabolic equivalent.
Again, regarding the secondary outcomes (setting specific physical activity and pain), no significant differences between the two groups were identified.
The Movement Coaching group tended to show higher workplace physical activity (base case: median 480 MET-min/week vs. 360 MET-min/week) and higher leisure time activity (MET-min/week) (base case: median 270 MET-min/week vs. 180 MET-min/week).
Both groups reported higher physical activity levels in workplace than leisure time or transportation. Figure 2 shows the boxplots of setting specific physical activity six months after inpatient rehabilitation.
Figure 2.
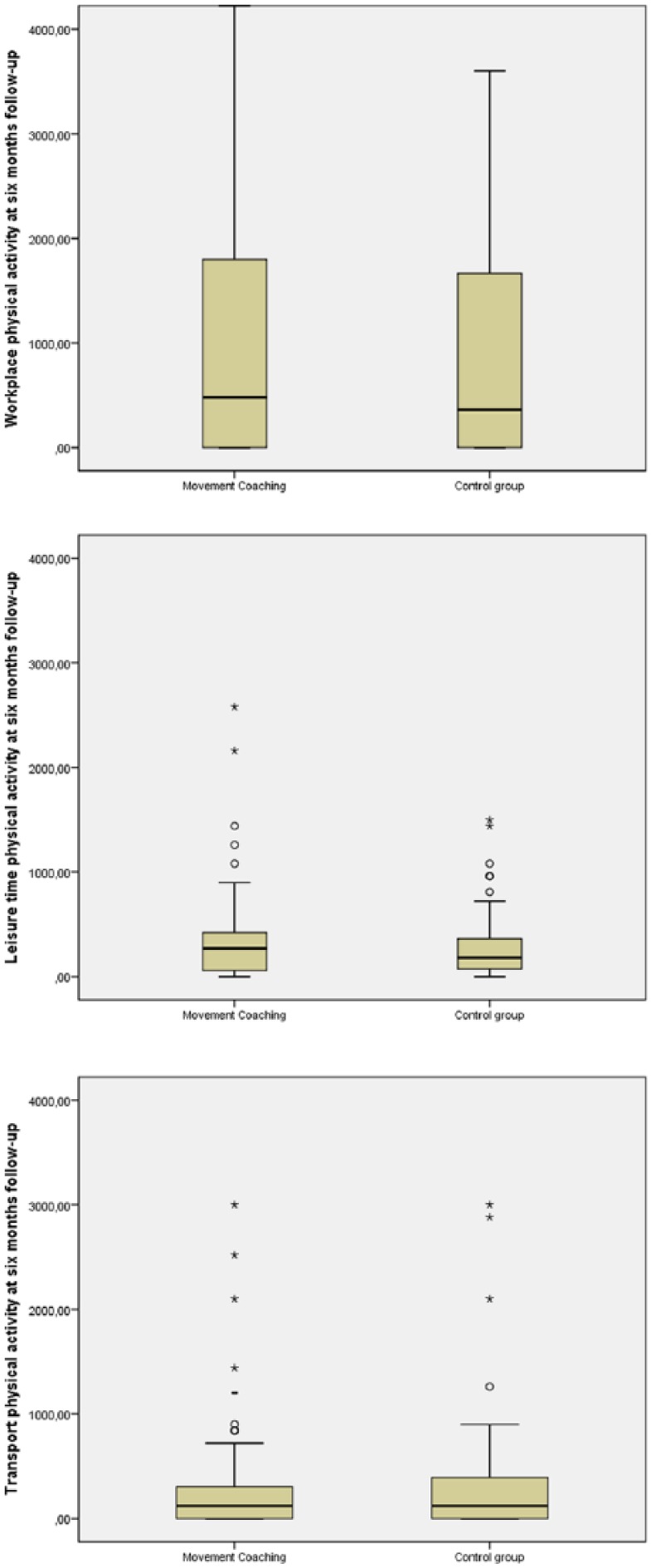
Boxplots of setting specific physical activities at six months follow-up.
Changes in physical activity from baseline to six months follow-up
From the beginning of inpatient rehabilitation (baseline) to six months follow up, both groups showed a significant decrease in pain. Furthermore, the results showed significant decreases in physical activity, except transport physical activity in the control group (P= 0.18). Compared to the control group, a significantly greater decrease in total physical activity (P < 0.01), transport (P = 0.02) and workplace physical activity (P = 0.03) in the Movement Coaching group was shown between the group differences (Table 5).
Table 5.
Between group and within subject differences (patients who replied to the postal six month follow-up questionnaire).
| Movement Coaching (n=92) | Control group (n=100) | P a | ||
|---|---|---|---|---|
| Total physical activity (∆ MET-min/week = T1-T0)c,d | mean (SD) | –6513 (±7236) | –3247 (±6018) | <0.01* |
| median [25%; 75%]- percentile | –4460 [–12045; –262] | –1110 [–4215; 124] | ||
| Pb | < 0.01* | < 0.01* | ||
| Workplace physical activity (∆ MET-min/week = T1-T0)c,d | mean (SD) | –5044 (±6944) | –2248 (±5121) | 0.03* |
| median [25%; 75%]- percentile | –720 [–9930; 0] | 0 [–3090; 0] | ||
| Pb | < 0.01* | < 0.01* | ||
| Leisure time physical activity (∆ MET-min/week = T1-T0)c,d | mean (SD) | –731 (±1817) | –614 (±1610) | 0.79 |
| median [25%; 75%]- percentile | –100 [–900; 158] | –155 [–840; 60] | ||
| Pb | < 0.01* | < 0.01* | ||
| Transport physical activity (∆ MET-min/week = T1-T0)c,d | mean (SD) | –659 (±1417) | –436 (±1828) | 0.02* |
| median [25%; 75%]- percentile | 0 [–1050; 0] | 0 [–294; 120] | ||
| Pb | < 0.01* | 0.18 | ||
| Intensity of pain during the last four weeks (minimum=1; maximum=6) (∆ = T1-T0)3 | mean (SD) | –0.94 (±1.24) | –0.81 (±1.2) | 0.46 |
| median [25%; 75%]- percentile | –1.0 [–2.0; 0.0] | –1.0 [–2.0; 0.0] | ||
| Pb | < 0.01* | < 0.01* |
Between group differences: Mann-Whitney-U-Test; bWithin subjects: Wilcoxon-Test; cT1 = six months follow-up; T0 = baseline: significance level P < 0.05; ** significant at the significance level P < 0.05; dDifferences between patients that replied to the six month follow-up questionnaire and the patients who did not reply in baseline data.
Discussion
In regard to physical activity and pain, the present study could not demonstrate superiority of a comprehensive multicomponent approach (Movement Coaching) over a low intensity intervention. Although the present results could not identify a superior intervention strategy or method in physical activity promotion, the study has several important implications for the future field of physical activity promotion in the healthcare setting. In particular, the decrease in physical activity in both groups over the six months period seems to be a noticeable aspect of the study and a major issue for further research on physical activity promotion.
Due to the clinical and statistical heterogeneity of studies on physical activity promotion (e.g., heterogeneity in the characteristics of the interventions, heterogeneity in the reported effects), the comparison with other studies is limited.14 Hence, the decrease in physical activity after an intervention aiming at promoting physical activity seems to contradict current research. A review of long-term effectiveness of interventions promoting physical activity in healthy adults showed evidence for increases in physical activity behaviour and physical fitness.15 Moreover, a review by Foster et al.14 suggests that physical activity interventions have a moderate effect on self-reported physical activity in sedentary adults.
One reason for the decrease in physical activity in the current study could be the target group of the intervention: since all patients suffered from chronic low back pain, a further deterioration of the patients’ health status cannot be excluded. Hence, the decrease in pain in the present results seems to contradict this assumption. Further research is needed to examine the relationship of health status and physical activity in low back pain patients.
Another reason for the decrease in physical activity might be the difficulties in measuring physical activity by a questionnaire. The literature shows a low correlation of objectively and subjectively measured physical activity.25,26 Moreover, a study from van Weering et al.27 showed that low back pain patients appear to have more problems in estimating their physical activity levels than healthy people. Patients probably overestimated their physical activity levels at the beginning of inpatient rehabilitation. The inpatient rehabilitation and each of the two different interventions employed here (Movement Coaching, low intensity control group), might have improved the patients’ self-estimation rather than their physical activity levels.
Comparing the decline in physical activity of the two different interventions, another interesting aspect is revealed: the decline in total physical activity in the Movement Coaching group is significantly greater than that in the control group. An improvement of self-assessment due to the comprehensive Movement Coaching intervention; including contact in the follow-up period, might be an explanation for this aspect. In this context, further studies are necessary on the correlation of subjective and objective physical activity before and after an intervention promoting physical activity.
The literature shows that comprehensive and high-quality interventions achieve the most significant long-term increases in physical behaviour.14,15 One reason that the present study could not underline the superiority of a comprehensive approach in physical activity promotion might be ascribed to the design of the present study. The comparison of two different intervention strategies might be a reason for the lack of differences in effectiveness. Several reviews could demonstrate that those interventions which were compared to an alternative intervention strategy, rather than to a minimal intervention or to no intervention at all, showed weaker effects.10,15,28
In line with the present results, Swinburn et al.29 could not show significant group differences between theory-based consultation on physical activity compared to solely oral advice, or at 6-weeks follow-up. Another randomised controlled trial, which compared a comprehensive high-intensity intervention (two supervised exercise a week, two hours education in physical activity and individual motivational counselling) with a low intensity control group (written information about the possibility of participating in exercise), showed significant improvement in physical activity in both groups but no significant group differences in effectiveness.30 Moreover, studies comparing phone and print intervention strategies in sedentary adults31 and studies evaluating differences between an individually tailored intervention and standardized intervention12,13 showed that the different strategies were equally effective.
The present study has several limitations. The low response rate was certainly the main weakness of the study. As a consequence, the generalization of the results on effectiveness is limited and the results should be interpreted very cautiously, taking into account the bias resulting from the non-reply to the postal six months follow-up questionnaire. To explore the robustness of the results, two ITT scenarios were also calculated.
A possible reason for the high loss to follow-up might be a lack of compliance with the interventions. To explore the feasibility and acceptance of the two approaches, a formative evaluation of the study results is planned. In a second step, this evaluation allows the possibility of identifying specific patients’ characteristics in order to gain knowledge about what intervention works for whom.
The methodological strength of the study is certainly the randomised controlled study design. However, this study design also faces several problems in rehabilitation practice: since the patients might recognise that they were receiving different types of treatment, the authors cannot completely exclude the possibility of bias resulting from the exchange of information between the patients.
A further limitation posing several challenges, which should be mentioned, is the measurement of physical activity using a questionnaire. The self-reported operationalization of physical activity may induce a reporting bias tending to overestimation.32,33 In addition to this, the Global Physical Activity Questionnaire, as a questionnaire recommended by the World Health Organization, is subject to concrete points of criticism and its validity is controversial.34,35
Apart from the limitations outlined above, this study includes a number of important strengths. Although most interventions on physical activity promotion consist of a combination of different intervention components, Movement Coaching is, as far as the authors are aware, the first multicomponent intervention combining face-to-face small group intervention, telephone aftercare and internet-based aftercare in the healthcare setting. Since it was already assumed that the promotion of physical activity exerts an influence, the study went further and compared two different approaches in a randomised controlled trial.
Clinical messages.
Six months after inpatient rehabilitation, the comprehensive multicomponent intervention does not seem to be more effective in promoting physical activity than the low intensity intervention.
The decrease in physical activity from baseline to follow-up is a noticeable aspect which should be examined further.
Acknowledgments
The authors would like to thank both the Aggertalklinik in Engelskirchen for their cooperation during the study and the patients for participating.
Footnotes
Conflict of interest: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study was funded by the German Statutory Pension Insurance Rhineland.
References
- 1. Warburton DE, Nicol CW, Bredin SS. Health benefits of physical activity: the evidence. CMAJ : Canadian Medical Association Journal 2006; 174: 801–809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Vuori IM, Lavie CJ, Blair SN. Physical activity promotion in the health care system. Mayo Clinic proceedings 2013; 88: 1446–1461. [DOI] [PubMed] [Google Scholar]
- 3. U.S. Department of Health and Human Services. Physical Activity and Health: A Report of the Surgeon General. Atlanta, GA: Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, 1996. [Google Scholar]
- 4. Körperliche Aktivität. Robert Koch-Institut (ed). Berlin: Robert-Koch-Inst, 2005. [Google Scholar]
- 5. World Health Organization (WHO). Global health risks: Mortality and burden of disease attributable to selected major risks. Geneva, Switzerland: World Health Organization, 2009. Available at: http://site.ebrary.com/lib/academiccompletetitles/home.action/http://site.ebrary.com/lib/alltitles/docDetail.action?docID=10363978/http://gbv.eblib.com/patron/FullRecord.aspx?p=476157. [Google Scholar]
- 6. Williams NH. Promoting physical activity in primary care. BMJ (Clinical research ed.) 2011; 343: d6615. [DOI] [PubMed] [Google Scholar]
- 7. German Medical Association, National Association of Statutory Health Insurance Physicians, Association of Scientific Medical Societies. National Disease Management Guideline Low back pain. Short version: 1st edition, 2011. Available at: http://www.leitlinien.de/nvl/kreuzschmerz.
- 8. Horst F, Adler B, Schulte-Frei B, Horst H. Orthopädisch-traumatologische Grudlagen. In: Froboese I, Wilke C, Nellessen-Martens G. (eds). Training in der Therapie: Grundlagen und Praxis. 3rd ed München: Elsevier Urban & Fischer, 2010. . [Google Scholar]
- 9. Haaf H. Findings on the Effectiveness of Rehabilitation 2005; 44: e1–e20. [DOI] [PubMed] [Google Scholar]
- 10. Orrow G, Kinmonth A, Sanderson S, Sutton S. Effectiveness of physical activity promotion based in primary care: systematic review and meta-analysis of randomised controlled trials. BMJ (Clinical research ed.) 2012; 344: e1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Brüggemann S, Sewöster D. Exercise therapy in the medical rehabilitation of the German Pension Insurance. B & G 2010; 26: 266–269. [Google Scholar]
- 12. Marcus BH, Lewis BA, Williams DM, Dunsiger S, Jakicic JM, Whiteley JA, et al. A comparison of Internet and print-based physical activity interventions. Archives of internal medicine 2007; 167: 944–949. [DOI] [PubMed] [Google Scholar]
- 13. Bock BC, Bess HM, Pinto BM, Forsyth LH. Maintenance of physical activity following an individualized motivationally tailored intervention. Ann Behav Med 2001; 23: 79–87. [DOI] [PubMed] [Google Scholar]
- 14. Foster C, Hillsdon M, Thorogood M, Kaur A, Wedatilake T. Interventions for promoting physical activity. The Cochrane database of systematic reviews 2005; (1): CD003180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Müller-Riemenschneider F, Reinhold T, Nocon M, Willich SN. Long-term effectiveness of interventions promoting physical activity: a systematic review. Preventive medicine 2008; 47: 354–368. [DOI] [PubMed] [Google Scholar]
- 16. Sudeck G, Pfeifer K. Bewegung in der Rehabilitation – ICF-Bezug, Kompetenzorientierung, Nachhaltigkeit. Public Health Forum 2013; 21: 14.e1–14.e4. [Google Scholar]
- 17. van Tulder M, Becker A, Bekkering T, Breen A, del Real, Maria Teresa Gil, Hutchinson A, et al. Chapter 3. European guidelines for the management of acute nonspecific low back pain in primary care. Eur Spine J 2006; 15 (Suppl 2): S169–S191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Schaller A, Froboese I. Movement coaching: study protocol of a randomized controlled trial evaluating effects on physical activity and participation in low back pain patients. BMC musculoskeletal disorders 2014; 15: 391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Armstrong T, Bull F. Development of the World Health Organization Global Physical Activity Questionnaire (GPAQ). J Public Health 2006; 14: 66–70. [Google Scholar]
- 20. Bull FC, Maslin TS, Armstrong T. Global Physical Activity Questionnaire (GPAQ): Nine Country Reliability and Validity Study. Journal of Physical Activity and Health 2009; 6:790–804. [DOI] [PubMed] [Google Scholar]
- 21. Herrmann SD, Heumann KJ, Der Ananian Cheryl A, Ainsworth BE. Validity and Reliability of the Global Physical Activity Questionnaire (GPAQ). Measurement in Physical Education and Exercise Science 2013; 17: 221–235. [Google Scholar]
- 22. Bullinger M, Kirchberger I, Ware J. Der deutsche SF-36 Health Survey: Übersetzung und psychometrische Testung eines krankheitstibergreifenden Instruments zur Erfassung der gesundheitsbezogenen Lebensqualität. Z. f. Gesundheitswiss 1995; 3: 21–36. [Google Scholar]
- 23. Lobelo F, Stoutenberg M, Hutber A. The Exercise is Medicine Global Health Initiative: a 2014 update. Br J Sports Med 2014; 48(22):1627–1633. [DOI] [PubMed] [Google Scholar]
- 24. Froboese I, Wallmann B. DKV-Report Wie gesund lebt Deutschland. 2012 https://www.dkv.com/downloads/DKV-Report-2012.pdf
- 25. Gaede-Illig C, Alfermann D, Zachariae S, Menzel C. Physical Activity Assessment - a Comparison between IPAQ-SF and SenseWearPro Armband. DZSM 2014; 65(6): 154–159. [Google Scholar]
- 26. Prince SA, Adamo KB, Hamel ME, Hardt J, Connor Gorber S, Tremblay M. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. The international journal of behavioral nutrition and physical activity 2008; 5: 56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. van Weering MGH, Vollenbroek-Hutten MMR, Hermens HJ. The relationship between objectively and subjectively measured activity levels in people with chronic low back pain. Clinical rehabilitation 2011; 25: 256–263. [DOI] [PubMed] [Google Scholar]
- 28. Williams NH, Hendry M, France B, Lewis R, Wilkinson C. Effectiveness of exercise-referral schemes to promote physical activity in adults: systematic review. The British journal of general practice : the journal of the Royal College of General Practitioners 2007; 57: 979–986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Swinburn BA, Walter LG, Arroll B, Murray WT, Russel DG. The Green Prescription Study: A Randomized Controlled Trial of Written Exercise Advice Provided by General Practitioners. American Journal of Public Health 1998; 88: 288–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Romé A, Persson U, Ekdahl C, Gard G. Physical activity on prescription (PAP): costs and consequences of a randomized, controlled trial in primary healthcare. Scandinavian journal of primary health care 2009; 27: 216–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sevick MA, Napolitano MA, Papandonatos GD, Gordon AJ, Reiser LM, Marcus BH. Cost-effectiveness of alternative approaches for motivating activity in sedentary adults: results of Project STRIDE. Preventive medicine 2007; 45: 54–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Slootmaker SM, Schuit AJ, Chinapaw MJ, Seidell JC, van Mechelen W. Disagreement in physical activity assessed by accelerometer and self-report in subgroups of age, gender, education and weight status. The international journal of behavioral nutrition and physical activity 2009; 6: 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Woll A. Assessment physical activity in adulthood. Zeitschrift für Sportpsychologie 2004; 11: 54–70. [Google Scholar]
- 34. Sitthipornvorakul E, Janwantanakul P, van der Beek, Allard J. Correlation between pedometer and the Global Physical Activity Questionnaire on physical activity measurement in office workers. BMC research notes 2014; 7: 280–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hoos T, Espinoza N, Marshal S, Arredondo EM. Validity of the Global Physical Activity Questionnaire(GPAQ) in Adult Latinas. J Phys Act Health 2012; 9: 698–705. [DOI] [PMC free article] [PubMed] [Google Scholar]