Abstract
Objectives
In patients with acute chest pain, we derived a cutpoint for ischaemia-modified albumin (IMA) and prospectively validated this cutpoint to predict 30-day major adverse cardiac events (MACEs).
Methods
We prospectively recruited a derivation cohort (18-month period) to establish a serum IMA cutpoint targeting 80% sensitivity. This was followed by a prospective validation cohort study of emergency department patients with acute chest pain at two university hospitals over a 3-month period. A MACE was defined as myocardial infarction, revascularisation or death at 30-day follow-up.
Results
In the derivation cohort of 151 patients, the IMA cutpoint that achieved 80% sensitivity for MACEs was 75 KU/litre. The sensitivity was prospectively validated in 171 patients consecutively enrolled, of whom 106 underwent multiple-biomarker analysis (19.8% MACE rate, 81% sensitivity of IMA). Furthermore, IMA by itself (81%, p<0.01) and in combination with initial highly sensitive cardiac troponin T (hsTnT) (90%, p<0.001) had significantly higher sensitivity than initial hsTnT (29%) for prediction of MACEs.
Conclusions
We prospectively validated the sensitive IMA cutpoint of 75 KU/litre with 80% sensitivity for MACEs in patients with acute chest pain. Our data suggest that IMA alone and in combination with initial hsTnT are more sensitive than the initial hsTnT for MACEs.
Chest pain accounts for >6 million emergency department (ED) visits annually in the United States.1 Of patients presenting with what is actually a myocardial infarction (MI), approximately 1%–5% are mistakenly discharged.1–3 Limitations of the clinical history4 and available risk scores5 emphasise the need for improvements in the routine assessment of acute chest pain to decrease the occurrence of “false-negative” ED workups that result in patients mistakenly discharged home. Highly sensitive risk-assessment tools would improve ED triage of patients with chest pain especially in low-risk populations.
Ischaemia-modified albumin (IMA) is an early sensitive biomarker of myocardial ischaemia. In the presence of myocardial ischaemia, structural changes in the N-terminus of serum albumin lower its natural affinity for cobalt binding.6,7 Use of a cobalt-binding assay to detect IMA has demonstrated differentiation between ischemic versus non-ischemic patients with chest pain,8 as well as prediction of inhospital acute coronary syndromes (ACSs)9–11 and mortality12 in patients with acute chest pain.
The objective of this study was to determine the 30-day prognostic sensitivity of IMA in patients with acute chest pain. We tested whether IMA can predict 30-day major adverse cardiac events (MACEs) for low- to moderate-risk patients with acute chest pain. We hypothesised that IMA would offer incremental benefit to the initial highly sensitive cardiac troponin T (hsTnT) for prediction of 30-day MACEs.
METHODS
Study setting and design
The study was designed as an observational cohort study of ED patients with acute chest pain to evaluate the test characteristics of IMA and the additive utility to that of initial hsTnT in this population. Patients were enrolled at two university, tertiary referral hospitals with >55 000 ED visits annually. Both institutions are staffed 24 hours a day with board-certified emergency doctors and cardiologists.
The study consisted of two phases: (a) convenience sampling during periods of research assistant availablility (consecutive patients on weekdays during business hours) at one hospital over 18 months (July 2004 to December 2005), which was used as a derivation data set to determine the optimal cutpoint for IMA, and (b) a prospectively enrolled study cohort at both hospitals (June–August 2006), which was used as a validation data set to independently validate the cutpoint for IMA. The study was approved by the institutional review boards at both study institutions.
Study population
For the derivation and validation cohorts, we defined the same enrolment criteria. We included adult (at least 21 years old) ED patients with the chief complaint of acute chest pain of any duration and onset within 24 h of ED presentation. We excluded patients with diagnostic ST elevation on electrocardiogram (ECG) who required rapid transfer to the cardiac catheterisation suite. Other exclusion criteria were refusal to the additional blood draw (required for IMA analysis) and discharge home or leaving the ED against medical advice without blood draw for cardiac biomarkers. All enrolled patients provided written informed consent.
Study protocol
Patients meeting the aforementioned study criteria during business hours (08:00–17:00) were approached by trained research assistants for enrolment. After providing written informed consent, a standardised data collection instrument was completed by a research assistant to assess baseline demographics (sex, age), traditional cardiac risk factors (current smoking, hypertension, dyslipidemia, diabetes mellitus and family history of coronary artery disease) and current medication use. Patients who agreed to have one additional blood draw for IMA were included in the multiple-biomarker analysis. Patients refusing the additional blood draw underwent routine data collection and follow-up but were not included in the multiple-biomarker analysis. Whole blood was drawn during the initial chest pain evaluation within 1 h of arrival to the ED. Details of the hospital course including results of laboratory tests, provocative testing, any procedural intervention and discharge summaries were prospectively collected from the electronic medical record.
Follow-up was achieved using review of clinic follow-up visits detailed in the electronic medical record, as well as telephone follow-up if no clinic follow-up was documented. We also reviewed social security death indices for patients without follow-up to assess for missed deaths within 30 days of the chest pain evaluation. If no follow-up was obtainable despite electronic records and death index review as well as five telephone calls from at least two investigators, then no further attempts were made, and these patients were deemed lost to follow-up.
Measurements
Initial troponin was measured using the hsTnT test (4th Generation Elecsys, Mannheim, Germany; detection limit 0.01 ng/ml, 10% imprecision) and was analysed with a cut-off ≥0.05 µg/l (99th percentile) considered positive. In all patients, initial hsTnT (Roche GmbH, Roche, Germany; cut-off 13 pg/ml, 99th percentile taken from 1500 apparently healthy participants (unpublished results), imprecision 10%) was followed by further serial standard troponin T or I measurements. No patients had undergone percutaneous coronary intervention immediately prior to initial hsTnT measurement; thus, no troponin elevations were considered iatrogenic.
Serum for IMA was immediately stored in 500-ml tubes at −20°C on site and consolidated to a −80°C freezer prior to analysis. Serum IMA (Roche Cobas Mira analysers; detection limit range <11–211 KU/litre, intra-assay coefficient of variation <10%) was measured off site using the albumin–cobaltbinding test, which is a colourimetric assay. The assay was run with test solutions from Inverness Medical (Louisville, Kentucky, USA) by collaborators who were blinded to the study hypothesis. Unlike results of initial hsTnT, IMA results were not available to treating doctors for clinical decision making.
Outcomes
The primary outcome was any MACE within 30 days of evaluation for acute chest pain. MACE was defined as any one of the following: MI (defined according to European Society of Cardiology–American College of Cardiology criteria),13 percutaneous coronary intervention, coronary artery bypass grafting, and all-cause mortality. The secondary outcome of inhospital non-ST elevation myocardial infarction (NSTEMI; defined according to European Society of Cardiology–American College of Cardiology13 criteria as the “detection of rise and/or fall of cardiac troponin with at least one value above the 99th percentile of the upper reference limit together with evidence of myocardial ischaemia with at least one of the following: (1) symptoms of ischaemia, (2) ECG changes indicative of new ischaemia (new ST T changes or new left bundle-branch block), (3) development of pathological Q waves in the ECG and (4) imaging evidence of new loss of viable myocardium or new regional wall motion abnormality”) was agreed upon by consensus of two study investigators.
Statistical analysis
We calculated sensitivities, odds ratios (ORs), and 95% confidence intervals (CIs). χ2 And Student t tests were used to compare categorical and continuous variables, respectively. Sensitivities of biomarkers were compared using McNemar test for correlated proportions. Based on the sensitivities of IMA (setting the cutpoint to that conferring 80% sensitivity for NSTEMI) and initial hsTnT (25% for MACEs) in the derivation cohort, we calculated the need to analyse the biomarkers of 110 patients in order to have 80% power to detect a difference in the sensitivity of each biomarker using McNemar test. Likelihood ratios (LRs) and 95% CIs were calculated using the estimated SE method with intercooled STATA V.8.2 software. All other calculations were performed with SPSS V.14 software.
RESULTS
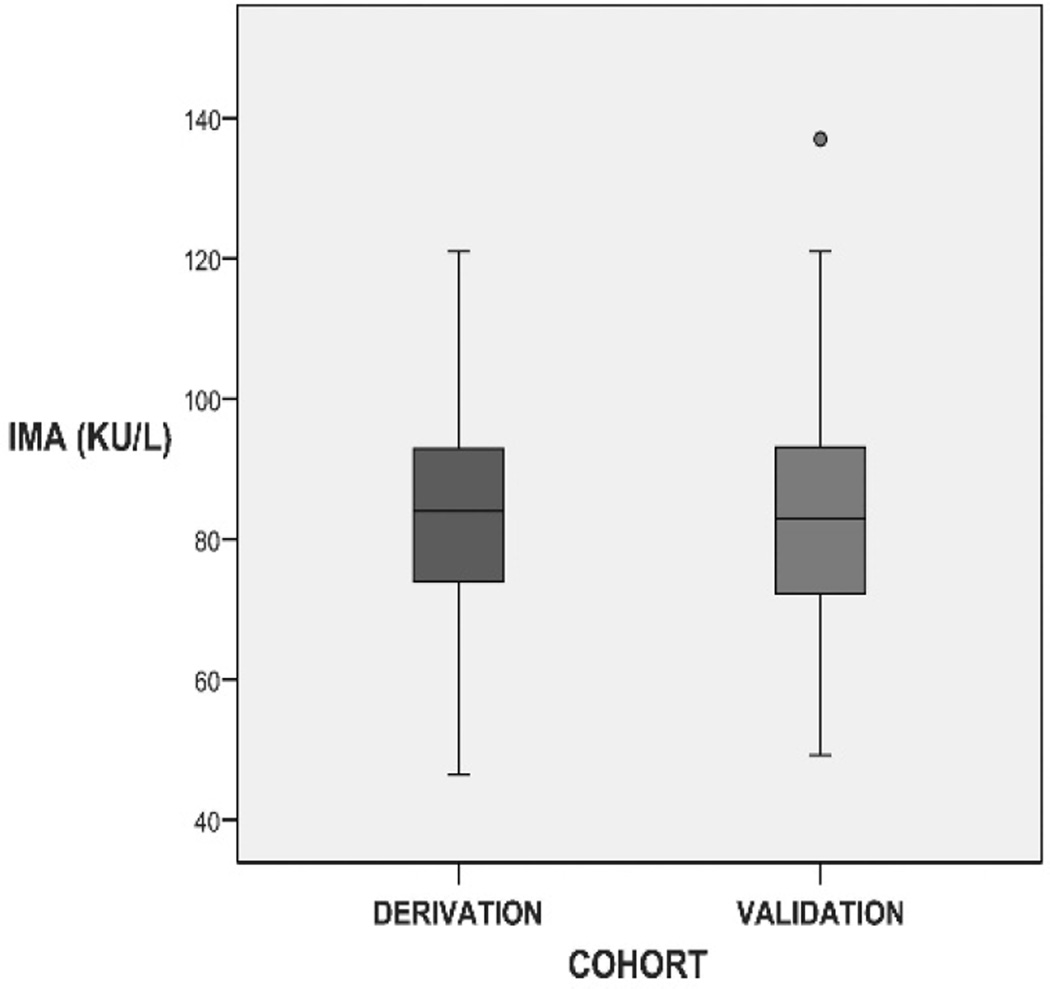
The baseline characteristics between the derivation and validation data sets were similar (table 1). Adverse event rates were generally higher in the consecutively sampled validation cohort than the derivation cohort (table 2). There was not a significant difference in the mean IMA serum concentration (t test p=0.6) between patients in each cohort.
Table 1.
Baseline characteristics of patients in the derivation and validation cohorts
| Characteristics | Derivation cohort | Validation cohort | p Value |
|---|---|---|---|
| Age (mean (SD)) | 55 (12) | 60 (14) | 0.20* |
| Male sex | 68 (45) | 57 (54) | 0.17† |
| Prior MI | 7 (5) | 26 (25) | <0.01† |
| Cardiac risk factors | |||
| Smoker | 22 (15) | 12 (11) | 0.45† |
| Hypertension | 72 (48) | 60 (57) | 0.16† |
| Hypercholesterolemia | 62 (41) | 58 (55) | 0.03† |
| Family history | 52 (34) | 27 (26) | 0.13† |
| Diabetes mellitus | 23 (15) | 22 (21) | 0.25† |
| Mean no (SD) risk factors | 1.9 (1.3) | 2.2 (1.3) | 0.04* |
| Total | 151 | 106 | 257 |
MI, myocardial infarction.
Values are presented as n (%), unless specified otherwise.
Mann—Whitney U test for continuous and ordinal variables.
χ2 Test for categorical variables.
Table 2.
Thirty-day outcomes and biomarker results for patients in the derivation and validation cohorts
| Outcome | Derivation sample (n=151) |
Validation sample (n=106) |
p Value |
|---|---|---|---|
| NSTEMI | 5 (3) | 14 (13) | <0.01* |
| IMA positive | 4 (80) | 10 (71) | 1.0* |
| Initial hsTnT positive | 0 (0) | 6 (43) | 0.13* |
| Both markers negative | 1 (20) | 2 (14) | 1.0* |
| Revascularisation | 6 (4) | 12 (11) | 0.02† |
| IMA positive | 3 (50) | 11 (92) | 0.08* |
| Initial hsTnT positive | 0 (0) | 3 (25) | 0.52* |
| Both markers negative | 3 (50) | 1 (8) | 0.08* |
| Death | 0 (0) | 2 (2) | 0.17* |
| IMA positive | 0 | 2 (100) | N/A |
| Initial hsTnT positive | 0 | 2 (100) | N/A |
| Both markers negative | 0 | 0 (0) | N/A |
| Any MACE‡ | 8 (5.3) | 21 (19.8) | <0.001† |
hsTnT, highly sensitive cardiac troponin T; IMA, ischaemia-modified albumin; MACE, major adverse cardiac event; NSTEMI, non-ST elevation myocardial infarction.
Values are presented as n (% in outcome category).
Significant p values are in bold font.
Fisher exact test for categorical variables.
χ2 Test for categorical variables.
Some patients had more than one adverse outcome.
Derivation cohort
We included 151 patients in the derivation cohort (mean IMA 84.4 (SD 22.1) KU/litre, range 11.4–211.0 KU/litre; see fig 1), of whom 8 (5%) developed 30-day MACEs. The baseline characteristics and specific outcomes of the derivation cohort are listed in tables 1 and 2, respectively. The IMA cutpoint that provided 80% sensitivity for 30-day NSTEMI was 75 KU/litre. Cutpoints of 60 and 90 KU/litre yielded sensitivities of 80% and 20%, respectively. Thus, the optimal cutpoint that maximised specificity while achieving 80% sensitivity was chosen to be 75 KU/litre. The sensitivity of initial hsTnT for 30-day MACEs in the derivation cohort was 25%.
Figure 1.
IMA results for derivation and validation cohorts. These box–whisker plots demonstrate the distribution of IMA biomarker results in the derivation and validation cohorts. (Midline = median, boxes = quartiles, vertical lines = range, dots = outliers.) IMA, ischaemia-modified albumin.
Validation cohort
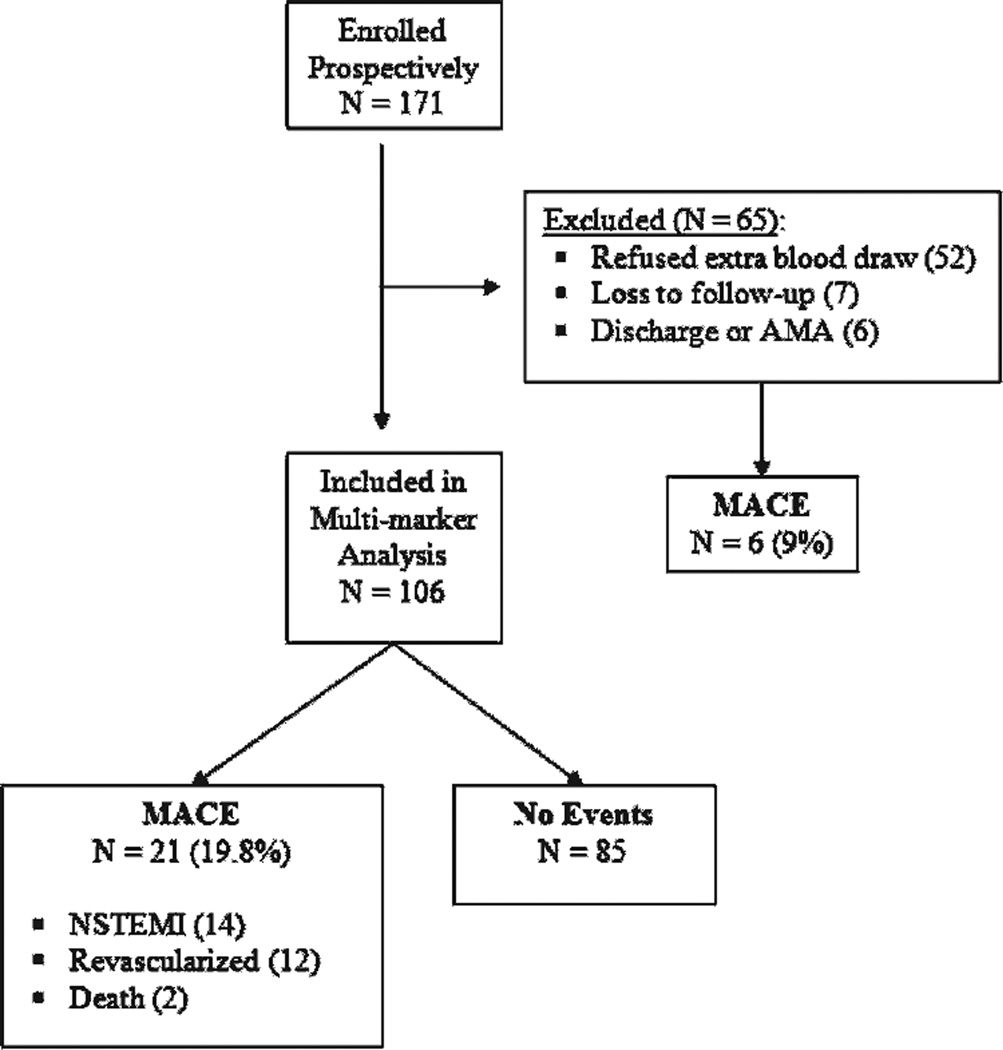
We prospectively enrolled 171 consecutive patients for the validation cohort, of which 65 were excluded from multiple-biomarker analysis because of refusal to additional blood draw (n=52), loss to follow-up (n=7), and ED discharge or leaving against medical advice without any hsTnT drawn (n=6). Of the remaining 106 patients available for multiple-biomarker analysis (mean IMA 86.1 (SD 30.4) KU/litre, range 14.8–211.0 KU/litre; see fig 1), 21 (19.8%) had MACEs within 30 days. A total of 71 (67%) of 106 patients had positive markers using the derived 75 KU/litre cutpoint. Study enrolment is summarised in fig 2.
Figure 2.
Flow chart for enrolment in the validation cohort. Flow chart outlining the prospective enrolment of 171 consecutive patients with acute chest pain for multibiomarker analysis in the validation data set. AMA, discharge against medical advice; MACE, major adverse cardiac event; NSTEMI, non-ST elevation myocardial infarction.
Multiple-biomarker analysis
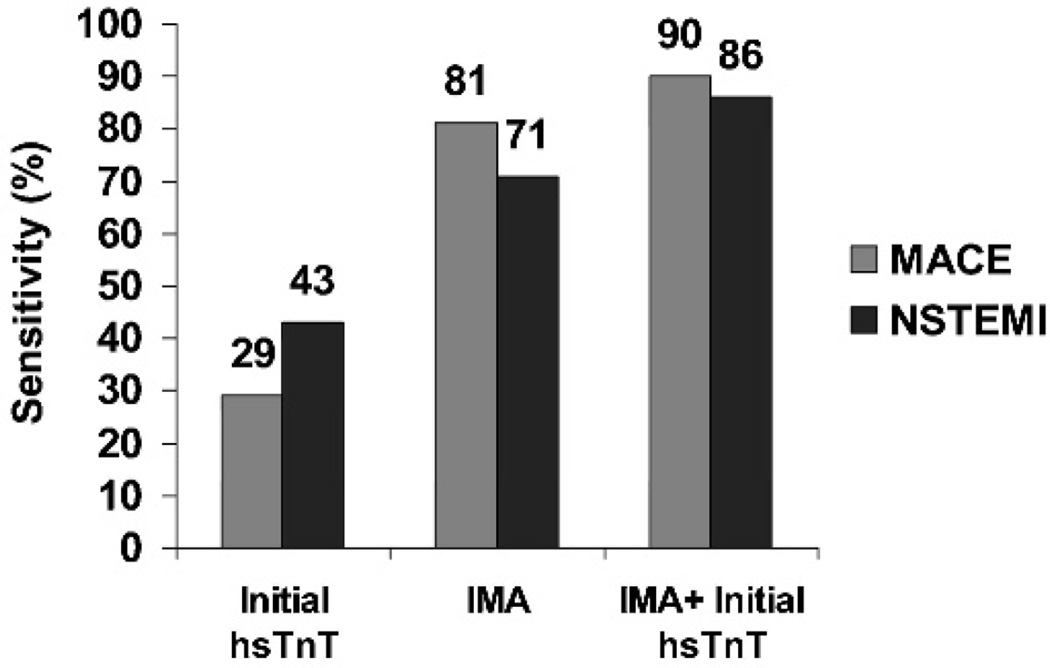
For each biomarker, 2×2 tables are depicted in table 3, and the sensitivities to predict NSTEMI and 30-day MACEs are summarised in table 4. The specificities of IMA for MACEs (36%) and NSTEMI (34%) were moderate. The sensitivity of IMA alone was significantly greater than the initial hsTnT to predict 30-day MACEs (p<0.01). Combining results of IMA with initial hsTnT incrementally improved the sensitivity to predict inhospital NSTEMI (p<0.05) and MACEs (p<0.001) over that of initial hsTnT alone. Graphical representations of the sensitivities of each biomarker for the MACEs and NSTEMI are summarised in fig 3.
Table 3.
Two-by-two table of IMA and MACEs in the validation sample (n = 106)
| MACEs | No MACEs | |
|---|---|---|
| IMA (≥75 KU/litre) | ||
| Yes | 17 | 54 |
| No | 4 | 31 |
| hsTnT (≥0.05 µg/l) | ||
| Yes | 6 | 0 |
| No | 15 | 85 |
hsTnT, highly sensitive cardiac troponin T test; IMA, ischaemia-modified albumin; MACEs, 30-day major adverse cardiac events.
Table 4.
Biomarkers in the validation cohort: test characteristics to predict 30-day NSTEMI and MACEs
| Cardiac biomarker | NSTEMI | MACEs | ||||
|---|---|---|---|---|---|---|
| Sensitivity | Specificity | OR | Sensitivity | Specificity | OR | |
| Initial hsTnT (≥0.05 µg/l) |
42.9% (CI 18% to 71%) |
100% (CI 96% to 100%) |
∞ | 28.6% (CI 11% to 52%) |
100% (CI 96% to 100%) |
∞ |
| IMA alone (≥75 KU/litre) |
71.4% (CI 42% to 92%) |
33.7% (CI 24% to 44%) |
1.3 (CI 0.4 to 4.4) |
81% (CI 58% to 95%) |
36.5% (CI 26% to 48%) |
2.4 (CI 0.8 to 7.9) |
| Combining IMA and initial hsTnT |
85.7% (CI 57% to 98%) |
33.7% (CI 24% to 44%) |
3.0 (CI 0.6 to 14.5) |
90.5% (CI 69% to 99%) |
36.5% (CI 26% to 48%) |
5.5 (CI 1.2 to 25.0) |
hsTnT, highly sensitive cardiac troponin T; IMA, ischaemia-modified albumin; MACEs, major adverse cardiac events; NSTEMI, non-ST elevation myocardial infarction.
Figure 3.
Sensitivity of biomarkers for cardiac outcomes (MACEs and NSTEMI). Sensitivities for MACEs and NSTEMI were compared with hsTnT using McNemar test. hsTnT, highly sensitive cardiac troponin T; IMA, ischaemia-modified albumin; MACEs, major adverse cardiac events; NSTEMI, non-ST elevation myocardial infarction. *p<0.05, ** p<0.01, ***p<0.001.
LR negatives (LR−) in decreasing order of utility (best listed first) were the following: combined hsTnT/IMA (LR− 0.26, 95% CI 0.07 to 1.01), IMA (LR− 0.52, 95% CI 0.21 to 1.32) and hsTnT (LR− 0.71, 95% CI 0.55 to 0.94). The LR positives (LR+) for each marker to predict MACEs in decreasing order of utility (best listed first) were the following: initial hsTnT (LR+ ∞), combined hsTnT/IMA (LR+1.42, 95% CI 1.15 to 1.76) and IMA (LR+1.27, 95% CI 0.98 to 1.66).
DISCUSSION
IMA cutpoint validation
We report an analysis of the 30-day prognostic utility of a commercially available IMA test applied to low- to intermediate-risk ED patients with acute chest pain. From a derivation data set, we derived an IMA cutpoint of 75 KU/litre that provides 80% sensitivity for 30-day NSTEMI. In a second step, we independently validated this cutpoint in a subsequent cohort study. In this validation group, a cutpoint of ≥75 KU/litre yielded a sensitivity of 71.4% (95% CI 42% to 92%) with an OR of 1.3 (95% CI 0.4 to 4.4) for NSTEMI and a sensitivity of 81% (95% CI 58% to 95%) with an OR of 2.4 (95% CI 0.8 to 7.9) for MACEs at 30 days. Intercohort sensitivity comparisons for NSTEMI were also validated using cutpoint of 60 KU/litre (80% derivation, 92.9% validation) and 90 KU/litre (20% derivation, 21.4% validation).
Incremental sensitivity of IMA
In addition, we demonstrated that IMA provides incremental sensitivity to initial hsTnT for prediction of 30-day MACEs (90%, p<0.001) and NSTEMI (86%, p<0.05). Sensitivity of initial hsTnT for NSTEMI (42.9%) and MACEs (28.6%) was extremely low, suggesting that patients in this cohort presented to the ED relatively early in the course of their symptoms. Thus, addition of IMA to the initial biomarker measurements may improve the sensitivity of the initial workup and potentially decrease the rate of mistaken discharges home from the ED. Although IMA was 100% sensitive for death at 30 days, the sensitivity of IMA for MACEs was too low (81% sensitive, 95% CI 58% to 95%) for use as a clinical decision-making tool on its own. Studies investigating the use of IMA in a diagnostic algorithm for acute chest pain are warranted.
LRs may provide an additional indicator as to the value of a diagnostic test. Clinically, the emergency doctor is most concerned about the negative predictive value of a test that allows an answer to the question, “Can I send this patient home if the test is negative?” Although this study was not powered specifically for LR calculation, we did find that the combination of IMA and hsTnT provided the lowest LR− (0.26); however, the 95% CIs were too wide to allow further recommendations on use of this parameter alone to decide whom to send home. Future studies of IMA should provide adequate power to help address this question.
Rationale for exclusion of STEMI
We excluded patients with diagnostic ST elevation on ECG who required rapid transfer to the cardiac catheterisation suite. The rationale for exclusion of STEMI patients was threefold: this study sought to enrol low- to intermediate-risk patients and STEMI patients are at high-risk for 30-day adverse outcomes14; STEMI patients are immediately rushed to the catheterisation suite at both institutions; therefore, to evaluate a biomarker that improves triage of these patients is irrelevant; and finally, research assistant interviews during STEMI patients’ brief time in the ED may be perceived as an impediment to expeditious clinical care (ie, rapid transfer to the catheterisation suite).
Context with prior IMA studies
Our data add significantly to the available knowledge regarding the utility of IMA for acute chest pain. Previously, non-commercially available IMA testing demonstrated excellent test characteristics in intermediate- and high-risk patients with chest pain for prediction of MI8 and ACSs.9,11 Aparci and colleagues12 analysed the prognostic utility of a non-commercially available IMA test in a coronary care unit population to predict 1-year mortality and found that the test characteristics were excellent. And finally, Sinha and colleagues10 analysed the sensitivity of a commercially available IMA test in a cohort of 208 high-risk ED patients with chest pain. IMA was more sensitive than either cardiac troponin or ECG analysis, but did not discriminate between ischemic patients with and without MI. In contrast to these studies, two investigations have reported limited potential of IMA to predict 72-h “serious cardiac outcomes,”15 8-h troponin I results (97.6% sensitivity in the PRIMA study)16 and inhospital acute MI17; however, these three latter studies suffered from lack of a clinically useful primary end point. A recent meta-analysis18 that evaluated a “triple prediction test” including non-diagnostic ECG, negative troponin, and negative IMA had a high negative predictive value (97.1%) for excluding ACS in the ED; however, the validity of unpublished data and heterogeneous quality of the studies evaluated may be called into question.
In contrast to the prior IMA studies outlined above, our results combine IMA and hsTnT to extend the utility of IMA beyond inhospital outcomes. Furthermore, our data suggest an improvement in the sensitivity to predict 30-day MACEs using IMA in addition to cardiac troponin. The utility of combining IMA, to maximise sensitivity, with hsTnT, to maximise specificity, may have synergistic diagnostic utility in the future.
Limitations
Analysis of this data set must take into consideration several limitations. The MACE rates were higher in the validation cohort than in the derivation cohort because of convenience sampling in the latter; however, the sensitivity of IMA for MACEs remained the same (~80%) in both cohorts. The characteristics of patients with broad inclusion criteria (ie, acute chest pain of any duration) in a tertiary-care setting may limit generalisability, but the 19.8% 30-day event rate in our study is comparable with other cohorts of low- to intermediate-risk patients with chest pain.3,19 The population may have been biased because of daytime enrolment; however, research assistants were not available after business hours, and to our knowledge, there are no data to suggest that after-business-hours MI rates are any different. The study was likely underpowered to demonstrate that IMA alone predicts 30-day MACEs; however, the analysis demonstrated a statistically significant improvement in sensitivity over that of initial hsTnT alone for prediction of inhospital NSTEMI and 30-day MACEs. We noticed a high sensitivity coupled with a low specificity for IMA and initial hsTnT, an inherent theme common to diagnostic testing in general; however, we feel that this was a minor limitation because the main clinical role of the biomarkers in this study was to test the sensitivity of each with the implicit goal to potentially save patients further unnecessary evaluation by use in future studies. In addition, the entry criteria of chest pain may lend itself to selection bias, at the expense of women, who present atypically with an ACS. Also, lack of information regarding the duration of chest pain and whether patients were chest pain-free while the marker was drawn is a subtle but important limitation to this data set; future studies should evaluate this relationship given that IMA is considered to be a rapidly rising and falling marker. And finally, our results await external validation in larger studies prior to widespread clinical application.
Conclusions
Our data suggest that analysis of serum IMA adds significantly to the sensitivity of the initial hsTnT in patients with acute chest pain. This improvement in the predictive value of ED biomarkers has the preliminary potential to decrease the rate of mistaken discharges home from the ED. The combination of IMA and hsTnT predicted a lower LR− for MACEs than either IMA or hsTnT alone; however, this was a statistically non-significant result. Further studies that incorporate IMA into diagnostic algorithms for patients with chest pain are warranted.
Acknowledgments
Funding: Cardiac Diagnostics Grant from Dade Behring (to JSB), Massachusetts General Hospital Departmental Award (to AFM) and in part by the National Institutes of Health (HL080053 to UH).
Footnotes
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
REFERENCES
- 1.Goldman L, Kirtane AJ. Triage of patients with acute chest pain and possible cardiac ischemia: the elusive search for diagnostic perfection. Ann Intern Med. 2003;139:987–995. doi: 10.7326/0003-4819-139-12-200312160-00008. [DOI] [PubMed] [Google Scholar]
- 2.Pope JH, Aufderheide TP, Ruthazer R, et al. Missed diagnoses of acute cardiac ischemia in the emergency department. N Engl J Med. 2000;342:1163–1170. doi: 10.1056/NEJM200004203421603. [DOI] [PubMed] [Google Scholar]
- 3.Christenson J, Innes G, McKnight D, et al. Safety and efficiency of emergency department assessment of chest discomfort. CMAJ. 2004;170:1803–1807. doi: 10.1503/cmaj.1031315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Swap C, Nagurney JT. Value and limitations of chest pain history in the evaluation of patients with suspected acute coronary syndromes. JAMA. 2005;294:2623–2629. doi: 10.1001/jama.294.20.2623. [DOI] [PubMed] [Google Scholar]
- 5.Manini AF, Dannemann N, Brown D, et al. Limitations of risk score models in patients with acute chest pain. Am J Emerg Med. 2009;27:43–48. doi: 10.1016/j.ajem.2008.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bar-Or D, Curtis G, Rao N, et al. Characterization of the Co(2+) and Ni(2+) binding amino-acid residues of the N-terminus of human albumin. An insight into the mechanism of a new assay for myocardial ischemia. Eur J Biochem. 2001;268:42–47. doi: 10.1046/j.1432-1327.2001.01846.x. [DOI] [PubMed] [Google Scholar]
- 7.Bar-Or D, Winkler JV, Vanbenthuysen K, et al. The cobalt–albumin binding assay: insights into its mode of action. Clin Chim Acta. 2008;387:120–127. doi: 10.1016/j.cca.2007.09.018. [DOI] [PubMed] [Google Scholar]
- 8.Bhagavan NV, Lai EM, Rios PA, et al. Evaluation of human serum albumin cobalt binding assay for the assessment of myocardial ischemia and myocardial infarction. Clin Chem. 2003;49:581–585. doi: 10.1373/49.4.581. [DOI] [PubMed] [Google Scholar]
- 9.Christenson RH, Duh SH, Sanhai WR, et al. Characteristics of an Albumin Cobalt Binding Test for assessment of acute coronary syndrome patients: a multicenter study. Clin Chem. 2001;47:464–470. [PubMed] [Google Scholar]
- 10.Sinha MK, Roy D, Gaze DC, et al. Role of “Ischemia modified albumin”, a new biochemical marker of myocardial ischaemia, in the early diagnosis of acute coronary syndromes. Emerg Med J. 2004;21:29–34. doi: 10.1136/emj.2003.006007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roy D, Quiles J, Aldama G, et al. Ischemia modified albumin for the assessment of patients presenting to the emergency department with acute chest pain but normal or non-diagnostic 12-lead electrocardiograms and negative cardiac troponin T. Int J Cardiol. 2004;97:297–301. doi: 10.1016/j.ijcard.2004.05.042. [DOI] [PubMed] [Google Scholar]
- 12.Aparci M, Kardesoglu E, Ozmen N, et al. Prognostic significance of ischemia-modified albumin in patients with acute coronary syndrome. Coron Artery Dis. 2007;18:367–373. doi: 10.1097/MCA.0b013e3281689a50. [DOI] [PubMed] [Google Scholar]
- 13.Thygesen K, Alpert JS, White HD Joint ESC/ACCF/AHA/WHF task force for the redefinition of myocardial infarction. Universal definition of myocardial infarction. Circulation. 2007;116:2634–2653. doi: 10.1161/CIRCULATIONAHA.107.187397. [DOI] [PubMed] [Google Scholar]
- 14.Antman EM, Anbe DT, Armstrong PW, et al. American College of Cardiology/American Heart Association task force on practice guidelines (writing committee to revise the 1999 guidelines for the management of patients with acute myocardial infarction) ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction—executive summary. Circulation. 2004;110:588–636. doi: 10.1161/01.CIR.0000134791.68010.FA. [DOI] [PubMed] [Google Scholar]
- 15.Worster A, Devereaux PJ, Heels-Ansdell D, et al. Capability of ischemia-modified albumin to predict serious cardiac outcomes in the short term among patients with potential acute coronary syndrome. CMAJ. 2005;172:1685–1690. doi: 10.1503/cmaj.045194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Keating L, Benger JR, Beetham R, et al. The PRIMA study: presentation ischaemia-modified albumin in the emergency department. Emerg Med J. 2006;23:764–768. doi: 10.1136/emj.2006.036269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Peacock F, Morris DL, Anwaruddin S, et al. Meta-analysis of ischemia-modified albumin to rule out acute coronary syndromes in the emergency department. Am Heart J. 2006;152:253–262. doi: 10.1016/j.ahj.2005.12.024. [DOI] [PubMed] [Google Scholar]
- 18.Collinson PO, Gaze DC, Bainbridge K, et al. Utility of admission cardiac troponin and “ischemia modified albumin” measurements for rapid evaluation and rule out of suspected acute myocardial infarction in the emergency department. Emerg Med J. 2006;23:256–261. doi: 10.1136/emj.2005.028241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Blomkalns AL, Lindsell CJ, Chandra A, et al. Can electrocardiographic criteria predict adverse cardiac events and positive cardiac markers? Acad Emerg Med. 2003;10:205–210. doi: 10.1111/j.1553-2712.2003.tb01991.x. [DOI] [PubMed] [Google Scholar]