Abstract
Background:
Recent evidence supports total hip arthroplasty (THA) as compared to hemiarthroplasty (HA) for the management of displaced femoral neck fractures in a significant subset of elderly patients. The purpose of this study was to examine trends in femoral neck fracture management over the last 12 years.
Methods:
Using the National Inpatient Sample database, we identified patients treated for femoral neck fractures between 1998 and 2010 with THA, HA, or internal fixation (IF). We examined treatment trends and demographic variables including patient age, gender, socioeconomic status, and payer and hospital characteristics.
Results:
We identified 362 127 femoral neck fracture patients treated between 1998 and 2010. Overall, there were statistically significant increases in rates of THA and HA, whereas rates of IF decreased. Total hip arthroplasty varied based on patient age, with significant increases occurring in age-groups 0 to 49 years, 50 to 59 years, 60 to 69 years, and 70 to 79 years. Utilization of THA varied significantly based on socioeconomic status and race. Patient sex, urban versus rural hospital location, and teaching versus nonteaching hospital status were not related to rates of THA.
Conclusion:
Rates of THA for femoral neck fractures increased between 1998 and 2010 in patients younger than 80 years, suggesting that surgeons are responding to clinical evidence supporting THA for the treatment of elderly femoral neck fractures. This is the first study to demonstrate this change and expose disparities in practice patterns over time in response to this evidence in the United States. Further research is indicated to explore the effect of socioeconomic status and race on femoral neck fracture management.
Keywords: hip, arthroplasty, femoral neck fracture, hip fracture, hemiarthroplasty, total hip arthroplasty
Introduction
Femoral neck fractures commonly occur in elderly patients, and the optimal management strategy remains uncertain. Nondisplaced and valgus impacted fractures are typically treated with internal fixation, whereas displaced fractures are treated with arthroplasty. Historically, these fractures were treated with hemiarthroplasty (HA), but there has been increasing interest in total hip arthroplasty (THA), with numerous contemporary studies demonstrating improved clinical outcomes at a lower overall cost.1–16 Total hip arthroplasty is now considered the optimal treatment for the active elderly hip fracture patient with limited comorbidities, whereas HA remains the mainstay treatment for low-demand patients, those with significant medical comorbid conditions, and patients with limited life expectancy. As the general population ages, the rate of femoral neck fractures in healthy active elderly patients is increasing. Several studies performed in the United States have demonstrated overall rates of THA as compared to HA have not increased significantly over time.17,18 Only very recently has a shift in treatment trends in the United States been identified.19 Recently published national registry data from Finland and Korea demonstrate an increasing utilization in THA over HA.20,21
Previous findings of little change in femoral neck fracture management strategies over time are likely multifactorial. It is possible that findings from recently published trials had not yet acted clinical practice. Some surgeons who are comfortable performing HA may not be comfortable performing THA as it is a more technically difficult operation. Appropriately so, surgeons may be reluctant to perform THA in the high-risk geriatric hip fracture population. We hypothesize that rates of THA for displaced geriatric femoral neck fractures will begin to rise in response to evidence supporting THA for the active healthy patient as the general population continues to age.
The goal of this study is to reexamine rates of internal fixation, HA, and THA for the treatment of femoral neck fractures in the United States between 1998 and 2010 with the hypothesis that there will have been an increase in rates of THA compared to HA. A secondary goal is to examine the influence of other patient-related, provider-related, geographic, and socioeconomic variables on utilization trends.
Materials and Methods
Data from the National Inpatient Sample (NIS) were used in this study. The NIS is the largest all-payer inpatient health-care database that is publicly available in the United States and is part of the Healthcare Cost and Utilization Project sponsored by the Agency for Healthcare Research and Quality. It contains deidentified discharge data for approximately 8 million hospital stays from more than 1000 hospitals every year. Sampled from 46 states that account for 97% of the US population, the NIS approximates a 20% stratified sample of US hospitals.
The NIS database contains information on patient diagnoses and procedures, listed as International Classification of Diseases, Ninth Edition, Clinical Modification (ICD-9-CM) codes. Each patient record contains up to 25 diagnosis codes (15 codes prior to 2009) and 15 procedure codes. For our cohort, we selected all patients with closed, transcervical femoral neck fractures (ICD-9-CM 820.0*) and closed fractures at unspecified parts of the femoral neck (820.8) in an effort to identify all patients with fracture patterns that could be appropriate for either arthroplasty or fixation. Fractures at the base of the femoral neck (820.03) were excluded, as fixation rather than arthroplasty is generally recommended for these injury patterns. We then further narrowed our cohort to look only at patients treated with THA (81.51), HA (81.52), or IF (78.55, 79.15, 79.35). Our final cohort included 362 127 patients.
The NIS also includes information about a number of patient and hospital variables that we included in our analysis. Patient characteristics include gender, race (white, black, Hispanic, Asian Pacific Islander, Native American, or other), age, and approximate income level. We defined age-groups from 0 to 49, 50 to 59, 60 to 69, 70 to 79, 80 to 89, and 90 to 119 years of age. The age-groups were intentionally allocated in this fashion. Lower and upper limits were set at 0 and 119 to ensure capture of all patients being treated for femoral neck fractures. More focused age-groups were then designated to evaluate trends in age-groups with the most clinically relevant cutoffs. To approximate patient income level, we used the NIS-provided median household income level of the patient’s home zip code. Hospital characteristics include ownership (public, private not-for-profit, or private investor-owned), teaching status (teaching or nonteaching), urban or rural location, and US region (northeast, midwest, south, or west). We also looked at the type of insurance used (Medicare, Medicaid, private, or self-pay) as well as the hospital case volumes for the 3 procedures.
To calculate hospital THA volume, we used the unique hospital identifiers in the data set to count how many THA cases were performed at each hospital, regardless of the patient diagnosis (ie, not only for femoral neck fractures). Hospitals were then categorized as having performed 0 THA cases, 1 to 50 cases, 51 to 100 cases, 100 to 200 cases, and more than 200 cases.
To test and describe changes in practice patterns, 2 statistical procedures were used. First, a test of independent proportions was used to evaluate whether the proportion of patients receiving a procedure in 1998 was different than the proportion of patients receiving the procedure in 2010. Second, a test of linear trend in proportions was conducted to evaluate whether the changes in practices were significantly increasing or decreasing across the study period. We repeated these procedures within strata of interest, such as gender and age groups, to explore the overall changes and trends obtained for particular patients. For all analyses, α of .05 was used. Analyses were conducted with SPSS and R statistical programs.
Results
Our cohort included 362 217 femoral neck fracture patients treated with 1 of the 3 procedures between 1998 and 2010. At all time points, HA was the most common management strategy (63.6% of patients), followed by IF (30.7%) and then THA (5.7%). We found a statistically significant increase in the rates of THA and HA and a statistically significant decrease in the rate of IF over this time period (Table 1). The proportion of patients treated with THA increased from 5.7% to 6.7% (P < .001), and the proportion treated with HA increased from 62.3% to 63.9% (P < .001). Conversely, the proportion of patients treated with IF decreased from 32.0% to 29.4% (P < .001).
Table 1.
Number of Patients (% of Patients) Undergoing Treatment for Displaced Femoral Neck Fractures with THA, HA, and IF per Year From 1998 to 2010.
| Procedure | 1998 | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | Trend P Values | Trend |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| THA | 1631 (5.8) | 1618 (5.7) | 1416 (5.5) | 1354 (4.9) | 1382 (4.9) | 1625 (5.7) | 1154 (5.5) | 1539 (5.4) | 1478 (5.3) | 1655 (5.9) | 1758 (6.1) | 1851 (6.8) | 1808 (6.7) | <.001 | Increasing |
| HA | 17 590 (62.3) | 17 665 (62.2) | 16 213 (63.5) | 17 746 (63.8) | 18 189 (64.1) | 18 044 (63.4) | 17 684 (63.1) | 18 248 (63.6) | 17 813 (64.3) | 17 786 (63.7) | 18 687 (64.9) | 17 338 (63.7) | 17 225 (63.9) | <.001 | Increasing |
| IF | 9032 (32) | 9130 (32.1) | 7913 (31) | 8714 (31.3) | 8825 (31.1) | 8781 (30.9) | 8796 (31.4) | 8883 (31) | 8413 (30.4) | 8477 (30.4) | 8009 (29.4) | 7912 (6.7) | 7912 (29.4) | <.001 | Decreasing |
Abbreviations: HA, hemiarthroplasty; IF, internal fixation; THA, total hip arthroplasty.
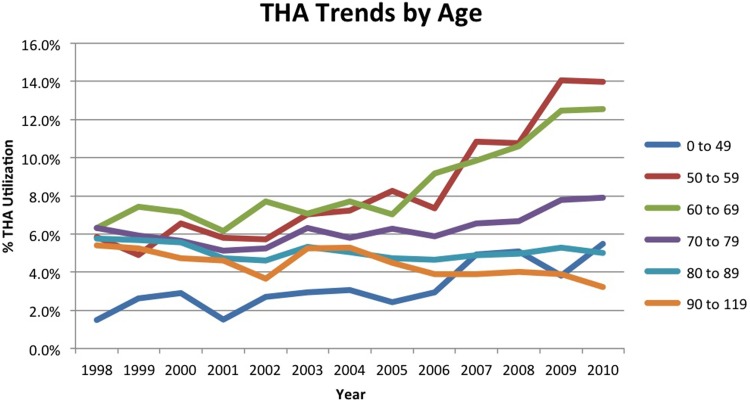
Stratifying the cohort by age revealed differences in management (Table 2). Across all years, a majority of patients in age-groups 0 to 49 years (86.4% of patients) and 50 to 59 years (55.6%) underwent IF, whereas most patients in groups 60 to 69 (54.2%), 70 to 79 (64.9%), 80 to 89 (69.4%), and 90 to 119 (71.2%) underwent HA. Additionally, utilization trends over time differed by age-group. Total hip arthroplasty utilization increased significantly in age-groups 0 to 49 (1.5%-5.5%), 50 to 59 (5.9%-14.0%), 60 to 69 (6.3%-12.6%), and 70 to 79 (6.3%-7.9%), and decreased significantly in age groups 80 to 89 (5.8%-5.0%) and 90 to 119 (5.4%-3.2%). Hemiarthroplasty utilization increased in age-groups 80 to 89 and 90 to 119 and decreased in the 60 to 69 group. Internal fixation utilization decreased in all age groups (Figure 1).
Table 2.
Procedure Performed by Age-Group for Displaced Femoral Neck Fractures per Year From 1998 to 2010.a
| Procedure by Age | 1998 | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | Trend P Values | Trend |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 to 49 | |||||||||||||||
| THA | 14 (1.5) | 27 (2.6) | 26 (2.9) | 14 (1.5) | 27 (2.7) | 29 (2.9) | 33 (3.1) | 25 (2.4) | 31 (2.9) | 48 (4.9) | 47 (5.1) | 33 (3.8) | 51 (5.5) | <.001 | Increasing |
| HA | 96 (10.3) | 92 (9.0) | 80 (8.9) | 85 (9.3) | 96 (9.6) | 111 (11.2) | 110 (10.2) | 120 (11.8) | 127 (12.1) | 93 (9.5) | 117 (12.6) | 95 (11.0) | 82 (8.8) | .084 | - |
| IF | 826 (88.2) | 908 (88.4) | 794 (88.2) | 814 (89.2) | 873 (87.7) | 849 (85.8) | 936 (86.7) | 876 (85.8) | 895 (85.0) | 835 (85.6) | 762 (82.3) | 738 (85.2) | 794 (85.7) | <.001 | Decreasing |
| 50 to 59 | |||||||||||||||
| THA | 55 (5.9) | 47 (4.9) | 60 (6.6) | 57 (5.8) | 64 (5.7) | 80 (7.0) | 90 (7.2) | 111 (8.3) | 99 (7.4) | 148 (10.8) | 152 (10.8) | 188 (14.1) | 199 (14.0) | <.001 | Increasing |
| HA | 306 (32.6) | 304 (31.7) | 345 (37.7) | 366 (37.3) | 417 (37.2) | 400 (35.1) | 456 (36.7) | 492 (36.6) | 508 (37.8) | 487 (35.7) | 511 (36.2) | 476 (35.6) | 484 (34.0) | .476 | - |
| IF | 579 (61.6) | 608 (63.4) | 510 (55.7) | 559 (56.9) | 641 (57.1) | 659 (57.9) | 697 (56.1) | 741 (55.1) | 737 (54.8) | 730 (53.5) | 750 (53.1) | 674 (50.4) | 742 (52.1) | <.001 | Decreasing |
| 60 to 69 | |||||||||||||||
| THA | 152 (6.3) | 174 (7.4) | 152 (7.1) | 137 (6.2) | 177 (7.7) | 172 (7.1) | 205 (7.7) | 187 (7.0) | 239 (9.2) | 268 (9.8) | 316 (10.6) | 365 (12.5) | 372 (12.6) | <.001 | Increasing |
| HA | 1367 (56.7) | 1283 (54.7) | 1202 (56.5) | 1238 (55.6) | 1259 (54.9) | 1320 (54.2) | 1442 (54.2) | 1435 (54.0) | 1460 (55.9) | 1480 (54.3) | 1594 (53.4) | 1531 (52.3) | 1487 (50.2) | <.001 | Decreasing |
| IF | 894 (37.0) | 889 (37.9) | 772 (36.3) | 850 (38.2) | 857 (37.4) | 943 (38.7) | 1014 (38.1) | 1036 (39.0) | 911 (34.9) | 978 (35.9) | 1073 (36.0) | 1030 (35.2) | 1104 (37.3) | .039 | Decreasing |
| 70 to 79 | |||||||||||||||
| THA | 506 (6.3) | 471 (5.9) | 399 (5.6) | 377 (5.1) | 398 (5.2) | 468 (6.3) | 412 (5.8) | 435 (6.3) | 392 (5.9) | 443 (6.6) | 454 (6.7) | 491 (7.8) | 485 (7.9) | <.001 | Increasing |
| HA | 5046 (63.1) | 5117 (64.3) | 4589 (64.8) | 4816 (65.4) | 5002 (65.8) | 4792 (64.8) | 4664 (65.7) | 4523 (65.2) | 4374 (65.7) | 4292 (63.7) | 4452 (65.6) | 4069 (64.4) | 3987 (65.0) | .104 | - |
| IF | 2449 (30.6) | 2375 (29.8) | 2098 (29.6) | 2174 (29.5) | 2203 (29.0) | 2135 (28.9) | 2022 (28.5) | 1983 (28.6) | 1891 (28.4) | 2007 (29.8) | 1878 (27.7) | 1754 (27.8) | 1666 (27.1) | <.001 | Decreasing |
| 80 to 89 | |||||||||||||||
| THA | 698 (5.7) | 695 (5.7) | 612 (5.6) | 584 (4.7) | 573 (4.6) | 669 (5.3) | 605 (5.1) | 596 (4.7) | 561 (4.7) | 589 (4.9) | 618 (5.0) | 612 (5.3) | 566 (5.0) | <.001 | Decreasing |
| HA | 8168 (67.3) | 8206 (67.2) | 7533 (68.5) | 8407 (68.2) | 8597 (69.0) | 8621 (68.9) | 8268 (69.0) | 8734 (69.5) | 8500 (70.6) | 8532 (70.7) | 8899 (71.6) | 8115 (70.0) | 8098 (71.5) | <.001 | Increasing |
| IF | 3275 (27.0) | 3317 (27.1) | 2845 (25.9) | 3328 (27.0) | 3296 (26.4) | 3226 (25.8) | 3105 (25.9) | 3243 (25.8) | 2979 (24.7) | 2954 (24.5) | 2904 (23.4) | 2868 (24.7) | 2666 (23.5) | <.001 | Decreasing |
| 90 to 119 | |||||||||||||||
| THA | 206 (5.4) | 204 (5.2) | 167 (4.7) | 185 (4.6) | 143 (3.7) | 207 (5.2) | 209 (5.3) | 185 (4.5) | 156 (3.9) | 157 (3.9) | 171 (4.0) | 162 (3.9) | 134 (3.2) | <.001 | Decreasing |
| HA | 2606 (68.2) | 2663 (68.3) | 2464 (69.9) | 2834 (70.7) | 2816 (71.9) | 2791 (70.6) | 2739 (69.2) | 2938 (71.3) | 2840 (71.2) | 2898 (72.2) | 3107 (73.3) | 3048 (73.6) | 3086 (74.3) | <.001 | Increasing |
| IF | 1009 (26.4) | 1032 (26.5) | 894 (25.4) | 989 (24.7) | 955 (24.4) | 953 (24.1) | 1011 (25.5) | 997 (24.2) | 991 (24.9) | 957 (23.9) | 962 (22.7) | 932 (22.5) | 936 (22.5) | <.001 | Decreasing |
Abbreviations: HA, hemiarthroplasty; IF, internal fixation; THA, total hip arthroplasty.
aValues are presented as number of patients (% of patients).
Figure 1.
Total hip arthroplasty (THA) utilization trends by age-group for displaced femoral neck fractures between 1998 and 2010.
Differences in socioeconomic status and race correlated with differences in patient management. When the cohort was stratified by income, there were no changes in the rates of THA in the lowest income group (US$1-US$24,999), whereas the rates of THA increased in all other groups. When stratified by race, we observed decreasing THA utilization over time in Hispanic patients, stable utilization in black, Native American, Asian, and other patients, and increasing utilization in white patients. We found no differences in utilization trends between males and females.
Hospital region and practice setting was also evaluated. The northeast, midwest, and west regions showed an increase in THA, whereas the south region did not. Rates of THA increased at both urban and rural hospitals. There were no differences in utilization trends between teaching and nonteaching hospitals. Total hip arthroplasty utilization at both public and private hospitals showed an increasing trend. Hospitals reporting a high volume of THA (100-200 and >200 per year) had a significant increase in THA for femoral neck fractures over this time period, whereas there was no difference in rates of THA for low-volume institutions (0-100 THA per year).
Discussion
We found increasing use of THA and decreasing use of IF for the treatment of femoral neck fractures between 1998 and 2010. Our findings suggest a response among surgeons in the United States to clinical evidence supporting the use of THA for the treatment of displaced femoral neck fractures in elderly patients. This shift comes on the heels of more than a decade of literature supporting THA over HA in the active healthy geriatric patient and several decades indicating the superiority of arthroplasty over IF. Importantly, we have identified striking disparities in the delivery of THA based on demographic, socioeconomic, and regional variables.
Several previous registry-based studies have analyzed trends in treatment patterns for these injuries in elderly patients in the United States and have not demonstrated the expected increased utilization of THA despite the supporting evidence.17,18,22 In 2008, Jain et al reported results of an analysis of the NIS, evaluating treatment trends from 1990 to 2001. They found an increased rate of HA over IF but a decrease in THA utilization over this time period. The authors concluded that the bulk of literature supporting THA over HA was published after 2000, explaining the apparent disparity between practice patterns and evidence, predicting there would be a shift in practice patterns in favor of THA in the future.17 In 2013, Miller et al published an analysis of data from the Medicare Part A database evaluating treatment trends from 1991 through 2008. Surprisingly, there were no significant changes in utilization of IF, HA, or THA over this time period. Hospital volume, regional variation, urban versus rural setting, and academic designation had no effect on treatment trends. The authors had several potential explanations for their findings, including the perception among community surgeons that the evidence supporting THA lacks generalizability to their practice, surgeon’s preference for a technically less demanding surgery, especially among those who do not routinely perform THA, and patient and family preference for a shorter and less complex procedure.18 Additional insight into surgeon decision-making comes from a 2006 survey distributed to the members of the American Association of Hip and Knee Surgeons to evaluate treatment preferences for displaced femoral neck fractures. At that time, 85% of responders routinely performed HA, while only 13% utilized THA and 2% IF despite 88% of responding surgeons being comfortable with performing THA. Dislocation risk and ambulatory status were cited as the most influential factors in decision-making.22 It is likely that the findings of the present study, with a more contemporary sample of patients, reflect the accumulation of clinical evidence over time.
There is recent evidence showing that practice patterns have started to change regionally in certain subsets of patients, as well as internationally. In Finland, the likelihood that a patient over the age of 50 with a displaced femoral neck fracture would be treated with THA nearly doubled between 2005 and 2011.20 Between 2006 and 2011 in South Korea, there was an increase in the number of THAs performed for femoral neck fractures in patients <65 years old.21 A recent study conducted by Hochfelder et al in New York state revealed a trend toward increasing utilization of THA among a subset of femoral neck fracture patients younger than 70 years of age but an overall unchanged rate of THA for femoral neck fracture over time.17 As in our study, THA was performed less frequently in the most elderly patients. It is likely that our large sample size allowed us to identify significant changes in management where this previous study did not.
Only very recently has a change in treatment patterns been identified in the United States.19 A query of the American Board of Orthopaedic Surgeons database demonstrated that among candidates applying for board certification between 1999 and 2011, utilization of THA for femoral neck fractures increased from 0.7% to 7.7%, with the most dramatic increase in THA use coming in younger patients. Those candidates declaring adult reconstruction as a subspecialty showed the most dramatic increase in use of THA for femoral neck fractures, from 4.3% in 1999 to 21.1% in 2011. Although the use of THA increased in all geographic locations, there was substantial variation among these. Practice patterns of established surgeons were not queried in this study.
Despite demonstrating statistically significant changes in treatment trends, the absolute number of patients undergoing THA rather that HA remains small, which brings into question the clinical relevance of these findings. This should be acknowledged when interpreting the results of this study. For example, in the 60- to 69-year age-group, there was a doubling in the proportion of patients undergoing THA, from 6.3% to 12.6% (P < .0001) over 12 years. Despite strong statistical significance, in 1998, 152 patients of 2413 underwent THA, and in 2010, 372 of 2963 underwent the same procedure in this age-group.
In the present study, demographic, geographic, and socioeconomic variables independently influenced trends in hip fracture management. Rates of THA did not increase in the poorest patients, while there was a significant increase across all other groups. Race had a significant effect on rates of THA. Caucasians were the only racial group to demonstrate an increase in THA. The rate of THA decreased significantly over this time period for Hispanics, and all other groups remained unchanged. Insurance type did not influence management strategies, with rates of THA increasing across all payer groups in this study. Interestingly, we found the most dramatic increase in THA use was in the self-payer group, increasing from 4.59% in 1998 to 10.69% in 2010. Hochfelder et al found that insurance status influenced treatment trends, as privately insured patients in their study were 41% more likely to undergo THA than those insured federally or self-pay. Race did not influence treatment in their study.23 It is concerning that some patients may be receiving suboptimal treatment based on race, geography, income, and insurance carrier, and further inquiry is warranted in this area.
There are limitations to this study. The use of a national database such as the NIS limits information available regarding factors that are likely to influence a surgeon’s preference for one treatment over the other. Although we were able to identify and include all patients treated surgically for a closed transcervical femoral neck fracture based on ICD-9 diagnosis and treatment codes, we were unable to account for the degree of displacement, other fracture characteristics, the degree of hip joint arthrosis, the functional status of the patient, and their medical comorbidities. Each one of these factors likely influences the treating surgeon’s decision for treatment independent of age, race, and socioeconomic status. As noted, although the findings are strongly statistically significant, the difference in absolute number of patients undergoing THA remains low.
Despite these limitations, this study provides a comprehensive quantitative analysis of treatment trends for displaced femoral neck fractures in the United States. Use of the NIS allows capture of patients in all age-groups, and accounts for all payer sources, allowing analysis of an accurate cross section of the US population having this injury.
This study demonstrates an increase in the utilization of THA for femoral neck fractures in the United States, confirming the hypothesis that surgeons nationwide are responding to evidence in support of THA. We found a trend toward decreased THA utilization in patients over 80 years, likely indicating surgeon reaction to decreased functional demand and increased medical comorbidities. There remains a disparity in treatment among various races, patients of differing socioeconomic status, and payer status. Further research should be focused on exploring the root causes of these disparities with the intention of identifying possible solutions for delivering equitable and optimal treatment to all patient groups.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Leonardsson O, Rolfson O, Hommel A, Garellick G, Åkesson K, Rogmark C. Patient-reported outcome after displaced femoral neck fracture: a national survey of 4467 patients. J Bone Joint Surg Am. 2013;95(18):1693–1699. [DOI] [PubMed] [Google Scholar]
- 2. Burgers PT, Van Geene AR, Van den Bekerom MP, et al. Total hip arthroplasty versus hemiarthroplasty for displaced femoral neck fractures in the healthy elderly: a meta-analysis and systematic review of randomized trials. Int Orthop. 2012;36(8):1549–1560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Liao L, Zhao J, Su W, Ding X, Chen L, Luo S. A meta-analysis of total hip arthroplasty and hemiarthroplasty outcomes for displaced femoral neck fractures. Arch Orthop Trauma Surg. 2012;132(7):1021–1029. [DOI] [PubMed] [Google Scholar]
- 4. Yu L, Wang Y, Chen J. Total hip arthroplasty versus hemiarthroplasty for displaced femoral neck fractures: meta-analysis of randomized trials. Clin Orthop Relat Res. 2012;470(8):2235–2243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zi-Sheng A, You-Shui G, Zhi-Zhen J, Ting Y, Chang-Qing Z. Hemiarthroplasty vs primary total hip arthroplasty for displaced fractures of the femoral neck in the elderly: a meta-analysis. J Arthroplasty. 2012;27(4):583–590. [DOI] [PubMed] [Google Scholar]
- 6. Avery PP, Baker RP, Walton MJ, et al. Total hip replacement and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck: a seven- to ten-year follow-up report of a prospective randomised controlled trial. J Bone Joint Surg Br. 2011;93(8):1045–1048. [DOI] [PubMed] [Google Scholar]
- 7. Hedbeck CJ, Enocson A, Lapidus G, et al. Comparison of bipolar hemiarthroplasty with total hip arthroplasty for displaced femoral neck fractures: a concise four-year follow-up of a randomized trial. J Bone Joint Surg Am. 2011;93(5):445–450. [DOI] [PubMed] [Google Scholar]
- 8. Goh SK, Samuel M, Su DH, Chan ES, Yeo SJ. Meta-analysis comparing total hip arthroplasty with hemiarthroplasty in the treatment of displaced neck of femur fracture. J Arthroplasty. 2009;24(3):400–406. [DOI] [PubMed] [Google Scholar]
- 9. Slover J, Hoffman MV, Malchau H, Tosteson AN, Koval KJ. A cost-effectiveness analysis of the arthroplasty options for displaced femoral neck fractures in the active, healthy, elderly population. J Arthroplasty. 2009;24(6):854–860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Macaulay W, Nellans KW, Iorio R, et al. Total hip arthroplasty is less painful at 12 months compared with hemiarthroplasty in treatment of displaced femoral neck fracture. HSS J. 2008;4(1):48–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Macaulay W, Nellans KW, Garvin KL, et al. Prospective randomized clinical trial comparing hemiarthroplasty to total hip arthroplasty in the treatment of displaced femoral neck fractures: winner of the Dorr Award. J Arthroplasty. 2008;23(6 suppl 1):2–8. [DOI] [PubMed] [Google Scholar]
- 12. Macaulay W. Total hip arthroplasty and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck. J Bone Joint Surg Am. 2007;89(5):1136; author reply 1136. [DOI] [PubMed] [Google Scholar]
- 13. Blomfeldt R, Törnkvist H, Eriksson K, Söderqvist A, Ponzer S, Tidermark J. A randomised controlled trial comparing bipolar hemiarthroplasty with total hip replacement for displaced intracapsular fractures of the femoral neck in elderly patients. J Bone Joint Surg Br. 2007;89(2):160–165. [DOI] [PubMed] [Google Scholar]
- 14. Macaulay W, Pagnotto MR, Iorio R, Mont MA, Saleh KJ. Displaced femoral neck fractures in the elderly: hemiarthroplasty versus total hip arthroplasty. J Am Acad Orthop Surg. 2006;14(5):287–293. [DOI] [PubMed] [Google Scholar]
- 15. Baker RP, Squires B, Gargan MF, Bannister GC. Total hip arthroplasty and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck. A randomized, controlled trial. J Bone Joint Surg Am. 2006;88(12):2583–2589. [DOI] [PubMed] [Google Scholar]
- 16. Healy WL, Iorio R. Total hip arthroplasty: optimal treatment for displaced femoral neck fractures in elderly patients. Clin Orthop Relat Res. 2004(429):43–48. [PubMed] [Google Scholar]
- 17. Jain NB, Losina E, Ward DM, Harris MB, Katz JN. Trends in surgical management of femoral neck fractures in the United States. Clin Orthop Relat Res. 2008;466(12):3116–3122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Miller BJ, Lu X, Cram P. The trends in treatment of femoral neck fractures in the Medicare population from 1991 to 2008. J Bone Joint Surg Am. 2013;95(18): e132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Miller BJ, Callaghan JJ, Cram P, Karam M, Marsh JL, Noiseux NO. Changing trends in the treatment of femoral neck fractures: a review of the American Board of Orthopaedic Surgery database. J Bone Joint Surg Am. 2014;96(17): e149. [DOI] [PubMed] [Google Scholar]
- 20. Hongisto MT, Pihlajamäki H, Niemi S, Nuotio M, Kannus P, Mattila VM. Surgical procedures in femoral neck fractures in Finland: a nationwide study between 1998 and 2011. Int Orthop. 2014;38(8):1685–1690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lee YK, Ha YC, Park C, Koo KH. Trends of surgical treatment in femoral neck fracture: a nationwide study based on claim registry. J Arthroplasty. 2013;28(10):1839–1841. [DOI] [PubMed] [Google Scholar]
- 22. Iorio R, Schwartz B, Macaulay W, Teeney SM, Healy WL, York S. Surgical treatment of displaced femoral neck fractures in the elderly: a survey of the American Association of Hip and Knee Surgeons. J Arthroplasty. 2006;21(8):1124–1133. [DOI] [PubMed] [Google Scholar]
- 23. Hochfelder JP, Khatib ON, Glait SA, Slover JD. Femoral neck fractures in New York State. Is the rate of THA increasing, and do race or payer influence decision making? J Orthop Trauma. 2014;28(7):422–426. [DOI] [PubMed] [Google Scholar]