Abstract
The poor prognosis of pancreatic cancer patients signifies a need for radically new therapeutic strategies. Tumor-targeted oncolytic viruses have emerged as attractive therapeutic candidates for cancer treatment due to their inherent ability to specifically target and lyse tumor cells as well as induce antitumor effects by multiple action mechanisms. Vaccinia virus has several inherent features that make it particularly suitable for use as an oncolytic agent. In this review, we will discuss the potential of vaccinia virus in the management of pancreatic cancer in light of our increased understanding of cellular and immunological mechanisms involved in the disease process as well as our extending knowledge in the biology of vaccinia virus.
Keywords: : immunotherapy, oncolytic virus, pancreatic cancer, vaccinia virus
Pancreatic cancer remains one of the most difficult cancers to diagnose and treat. It is the fifth most common cause of cancer death in the UK with 1 and 5 years survival of 20.8 and 3.3%, respectively. These figures have hardly improved since the early 1970s [1]. Complete surgical resection remains the only curative treatment. Unfortunately, less than 20% of pancreatic tumors are amenable to surgical excision at the time of diagnosis. However, even with complete surgical resection prognoses remains poor with 5 years survival around 20% [2,3]. Gemcitabine is the main chemotherapeutic agent approved for advanced pancreatic cancer. Despite being shown to improve life expectancy compared with 5-flurouracil, effect remains modest with median survival around 6 months [4]. Combining gemcitabin therapy with erlotinib led to minimal increase in life expectancy from 5.9 to 6.2 months [5]. Therefore, new treatment strategies are clearly imperative.
Vaccinia virus (VV) has played a prominent role in one of the greatest achievements in medical history: the eradication of smallpox (caused by Variola virus). Since then, VV has been developed as a vector for vaccines against infectious diseases such HIV, influenza, malaria and tuberculosis as well as in immunotherapies [6] and oncolytic therapies for cancer [7,8]. With regards to the latter, the earliest studies, which mainly used replication attenuated VV recombinants for fear of toxicity, were relatively disappointing in the clinic. Replication competent VVs retain their ability to lyse tumor cells and spread through tumor tissue. Recent advances in DNA recombinant technology enabling the rational manipulation of the viral backbone, coupled with the ever increasing knowledge gains in the fields of molecular virology and cancer cell biology have aided the development of safe and efficacious tumor-targeted oncolytic VVs. These are currently at the forefront of the most promising novel anticancer agents.
In this review, we will explore the potential of tumor-targeted oncolytic VV in the management of pancreatic cancer in light of our increased understanding of cellular and immunological mechanisms involved in the disease process as well as our extending knowledge in the biology of VV.
Tumor-targeted oncolytic viruses as a new class of cancer therapeutics
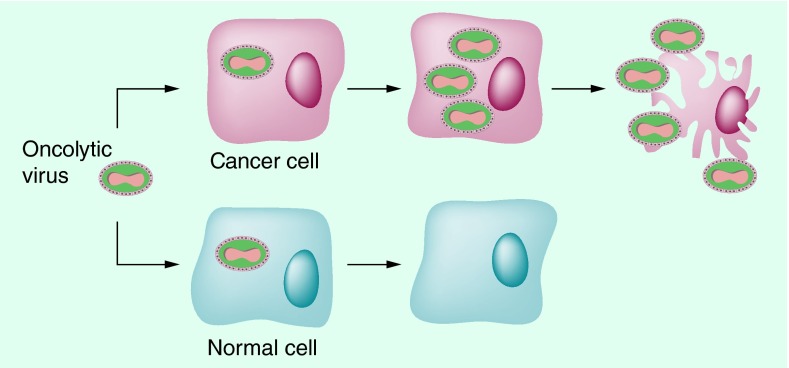
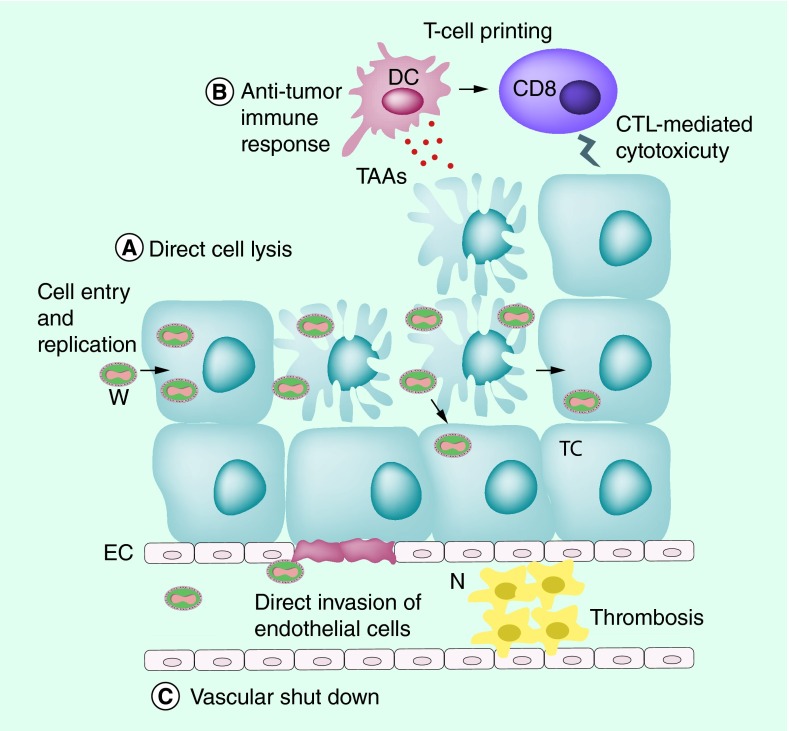
Targeted therapy of cancer using oncolytic viruses (OV) has generated much interest over the past decades in the light of the limited efficacy and the significant side effects of standard cancer therapeutics for advanced disease [9]. OVs have become an increasingly popular anticancer therapy platform due to their ability to selectively infect and lyse tumor cells (Figure 1). Cancer selectivity of OVs could be a result of natural tropism [10,11] or via genetic modification [9]. OVs can target multiple cellular pathways [12–14] minimizing the risk of tumor resistance and induce different modes of cell death [15–18]. In addition, OVs can break down the immunosuppressive tumor microenvironment and induce a long-lasting tumor-specific immunity [19,20] (Figure 2). OVs can specifically deliver therapeutic proteins into tumors at increasing levels following viral replication within the malignant cells. Furthermore, OVs can function in synergy with conventional cancer treatments of chemoradiotherapy [21–24]. Finally, OVs as a treatment platform are amenable to adjustment and development following our ever-increasing understanding of cancer cells, the virus and host immune responses to both tumor and virus.
Figure 1. . Tumor selectivity of oncolytic viruses.
Tumor-targeted oncolytic viruses can exploit defective cellular pathways in cancer cells (top). oncolytic viruses can infect and replicate in cancer cells leading to cell lysis and release of viral particles. These in turn infect neighbor tumor cells and so forth. In normal cells (bottom) cellular defense mechanisms prevents viral replications.
Figure 2. . Multiple modes of actions of tumor-targeted oncolytic viruses.
Oncolytic viruses (OV) can kill cancer cells via a variety of mechanisms. First, they directly infect, replicate and lyse tumor cells sparing normal cells. Released virions can infect neighbor tumor cells and so forth. Second, OVs can induce immunogenic cell death associated with the release of Pathogen-associated molecular patterns and Damage-associated molecular patterns. In addition viral infection results in the release of cytokine and chemokines deviating the immune response toward a cytotoxic profile. Dendritic cells can pick tumor-associated antigens released from lysed tumor cells and prime CD8+ T cells to induce a tumor-specific immune response. Third, OV infection can result in vascular shutdown caused by direct viral invasion of endothelial cells and thrombosis caused by cytokine-mediated neutrophils accumulation.
CD8: Cytotoxic T cell; DC: Dendritic cell; EC: Endothelial cell; N: Neutrophil; TAA: Tumor-associated antigen; TC: Tumor cell; VV: Vaccinia virus.
H101, an adenovirus with E1B 55K gene deletion (Oncorine; Shanghai Sunway Biotech, Shanghai, China) was licensed in China in 2005 as the world's first OV for treatment of head and neck cancer when combined with chemotherapy [25]. The similar virus, dl1520 (also known as, ONYX-015) has been administered by intratumoral injection under CT guidance into locally advanced primary tumors of pancreatic cancer patients in Phase I/II trials. The treatments were well tolerated, but no objective responses were seen in any of the patients with virus alone, and only 10% (2/21) patients showed objective response when gemcitabine was used in combination [26–28]. Another virus that entered clinical trials is HF10, a Herpes Simplex virus armed with granulocyte-macrophage colony-stimulating factor (GM-CSF). Phase I trial of intratumoral injection into nonresectable pancreatic tumors proved to be safe with some encouraging clinical results [29]. These early results warrant further investigation to seek more powerful agents for this cancer.
Favorable features of vaccinia virus for cancer treatment
VV is a member the poxvirus family. It is a double-stranded DNA virus ˜192 kbp in size. It can be stably accommodate up to 25 kbp of cloned exogenous DNA [30]. Structurally, it consists of a core region composed of viral DNA and a various viral enzymes including RNA polymerase and polyA polymerase encased in a lipoprotein core membrane. The outer layer of the virus consists of double lipid membrane envelope [31,32]. VV has two major forms of infectious virions; the intracellular mature virions, as described above, which is released upon cell lysis and the extracellular enveloped virion released from the cells via cell membrane fusion. The latter has an additional lipid bilayer membrane wrapped around the intracellular mature virion particle.
VV has many inherent characteristics that make it an ideal choice for oncolytic virotherapy. VV has a short life cycle of 8 h that takes place in its entirety in the cytoplasm eliminating the risk of genome integration. Replication usually starts 2 h after infection, at which time the host cell nucleic acid synthesis shuts down as all cellular resources are directed toward viral replication [33,34]. Cell lyses takes place between 12 and 48 h releasing packaged viral particles. Furthermore, the virus does not depend on host mechanisms for mRNA transcription making it less susceptible to biological changes of the host cell [33,35].
Unlike other OVs, VV does not have a specific surface receptor for cell entry allowing it to infect a wide range of cells unhindered by the lack of expression of said receptor. They depend on a number of membrane fusion pathways for cell entry [36,37].
The existence of various antigenically distinct forms of the mature virus allows it to evade host immune system. extracellular enveloped virion form of the virus is encapsulated in a host-derived envelope, with incorporated viral proteins, that contains several host complement control proteins [38–40]. In addition, VV infected cells secret Vaccinia complement control protein which binds an inactivate C4b and C3B inhibiting the classic and alternative complement activation pathways [41–43]. VV therefore can be disseminated relatively unharmed in the blood stream to reach distant tumors allowing systemic delivery of the virus [44], which is more suitable for the treatment of the advanced pancreatic cancer.
The hypoxic nature of pancreatic cancer contributes to its aggressive and treatment-resistant phenotype. In contrast to adenovirus [45], we have found that hypoxic conditions did not affect replication, viral proteins production, cytotoxicity and transgene expression of the Lister strain of VV [46]. These results suggest that VV could be suitable for management of pancreatic cancers and potentially other hypoxic tumors.
Finally, VV has a good safety track record following its use as a vaccine for over a century. Minor and less severe side effects include fever, rash and inadvertent inoculation. Moderate-to-severe side effects include eeczema vaccinatum, generalized vaccinia, progressive vaccinia and postvaccinial encephalitis [47]. Sides effects are rare with an incident of less than 1:10,000 and severe side effects in particular are extremely rare [48]. Genetically modified recombinant VV could be potentially safer due to their tumor selectivity. Recent clinical trial of JX-594 virus in hepatocellular carcinoma showed the treatment to be well tolerated with mainly flu-like symptoms in all patients and a single severe side effect [8].
How Vaccinia virus selectively kills cancer cells by multiple action mechanisms
VV has a natural tropism to cancer cells [49,50]. The virus can utilize activated molecular pathways in tumor cells to aid its replication [51–53]. In fact, many of the hallmarks of cancer [54] make tumor cells susceptible to viral replication including immune escape, sustained cell proliferation and resisting cell death. In the case of VV, the EGFR family [55], potentially plays an important role in tumor selectivity. The viral SPGF, an EGF-like growth factor carried by VV, can activate host cellular pathways leading to increased viral replication [56]. In addition, Ras–GTP-activating protein S3H domain-binding protein, overexpressed in most human cancers [57], plays a role in VV replication by complementing the activity of the VITF-2 [58].
Various approaches can be utilized to enhance tumor selectivity of OVs. The virus depends for its replication in normal cells on a set of genes that prepare the cell resources for viral replication and block apoptotic pathways. Deleting these genes will limit the virus ability to replicate in normal cells. However, these pathways are often disrupted in cancer cells allowing the mutant virus to replicate despite the defective genes. One such example is the disruption of the vaccinia thymidine kinase gene (TK gene) affecting the virus ability to synthesize deoxyribonucleotides [59,60]. Normal cells have a much smaller reserve of deoxyribonucleotides, compared with tumor cells, limiting the ability of VV to replicate. Another example is the deletion of the B18R gene encoding the secreted IFN-binding protein that blocks IFNα signaling [61]. In normal cells, this gene deletion attenuates viral replication due to IFN antiviral effect while cancer cells remain permissive to VV replication as IFN signaling is often disrupted [62,63]. In addition, altering the expression of crucial vaccinia viral gene by microRNA also enables tumor-specific viral replication, which is a potentially novel and versatile platform for engineering VVs for cancer virotherapy [64].
GLV-1h68 is a replication-competent VV targeted at tumor cells by mutation of J2R (encoding thymidine kinase) and A56R (encoding hemagglutinin) loci. This virus was shown to be effective against human pancreatic cancer cell line in vitro and in nude mice xenografts. Importantly this efficacy was enhanced when virus therapy was combined with gemcitabine and cisplatin [65]. GLV-1h151, a virus with similar gene deletions but different marker proteins transgenes [66], was found to be effective in vivo and in vitro against human pancreatic cancer cell lines. Combining the virus with radiotherapy resulted in a synergistic antitumor effect [67].
In addition to direct cell lysis, VV can utilize vascular shut down to kill noninfected tumor cells [44,68–69]. This is believed to be caused by accumulation of neutrophils in blood vessels, mediated by cytokines and chemokines, leading to intravascular thrombosis [69]. In addition, VV can infect and destroy tumor-associated endothelial cells further contributing to vascular collapse [62]. Although this process has not been specifically shown in pancreatic tumors, we believe it to play an important role in the multimechanistic antitumor effect of VV, as pancreatic cancers are often well-vascularised and high microvascular density correlates with poor outcome after surgical excision [70]. To further capitalize on this process we have rationally armed Lister strain VV with endostatin–angiostaten fusion gene, a well-documented angiogenesis inhibitor [71]. The resultant VVhAE virus proved to be tumor selective in vitro and in vivo. It resulted in suppression of angiogenesis and prolonged survival of mice bearing human pancreatic cancer xenografts [50].
Vaccinia virus as immunomodulatory agent
The ability of OVs to alter the immune composition of the, ordinarily, immune-suppressive tumor microenvironment led to a new line of thinking of their mechanism of action. Large body of evidence suggests that antitumor immunity, where the virus is acting as an oncotropic immunomodulator, is the key determinant of a successful onclytic virotherapy [72–74].
VV kills cancer cells via a combination of necrosis and immunogenic apoptosis resulting in the release of damage associated molecular patterns [75–78] and pathogen associated molecular patterns [79–81] as well as the release of viral antigens into the tumor. This process leads to a strong inflammatory response that can overcome the immune suppression within the tumor microenvironment. In addition, tumor cell lysis releases tumor-associated antigens (TAA) into this inflammatory environment. Dendritic cells recruited by the virus can in turn pick up these exposed TAAs and cross-prime CD8+ T-cells resulting in a potent antitumor adaptive immune response. It has been demonstrated that an oncolytic VV (JX549) could induce tumor-specific immunity in human cancer patients [82] and preclinical study [20]. Therefore, oncolytic virotherapy may be considered as a method of vaccination in situ, enabling the adaptive immune response to clear residual disease as well remote metastatic cancer cells and provide long-term surveillance against relapse.
In the context of vaccination, heterologous prime-boost immunization regimen using recombinant adenovirus prime and VV boost has been shown to enhance CD8+ T cell immunogenicity with protective efficacy against malaria in a mouse model [83,84]. So, it seems logical that combining two different OVs for cancer treatment may induce a stronger tumor-specific immunity. We have, for the first time, combined the use of oncolytic adenovirus and VV, in a prime-boost strategy, for treatment of established tumors in the hope to harness the host immune response to the infected tumor cells. We found that sequential treatment via intratumoral injection with oncolytic adenovirus followed by oncolytic VV resulted in complete eradication of subcutaneous pancreatic cancer grafts in Syrian hamsters. More importantly, the surviving animals developed a long-lasting tumor-specific immune response that protected them against tumor rechallenge. This process was shown to be T-cell dependent [20].
Arming VV with various cytokines and chemokines can further enhance its antitumor activity. IL-10, a cytokine produced by Th2 T cells, is a potent inhibitor of antiviral immune response [85]. We have found that arming VV with IL-10 dampened antiviral immune response resulting in prolonged viral persistence in pancreatic tumors. This led to stronger antitumor immunity and improved survival in both subcutaneous and transgenic pancreatic cancer mouse models [86].
Vaccinia virus as vaccine vector
The first use of a recombinant virus armed with an antigen from a different organism as a vaccine vector was reported over 30 years ago. VV armed with hepatitis B surface antigen gene was able to induce a protective immunity against hepatitis in chimpanzees [87,88]. Since then there has been a great progress in recombinant VV vaccines in the veterinary field [89,90]. Unfortunately this success did not extend to human infectious diseases vaccines, mainly due to the lengthy and more stringent process for human licensing, with only a handful of recombinant VV vectors in current clinical trials [91–94].
One of the significant challenges for cancer vaccination lies in developing strategies to improve the delivery of antigens to antigen-presenting cells in vivo, allowing effective antigen processing and presentation and activation of a potent immune response against a unique background of immune tolerance toward ‘self’ TAAs. Viral vectors have become attractive antigen delivery systems as they mimic a natural viral infection, resulting in induction of cytokines and co-stimulatory molecules that provide a powerful adjuvant effect and elicit potent cellular immunity [74,95].
Survivin is a member of the inhibitor of apoptosis family expressed in a variety of cancers. It plays a crucial role in tumor survival and drug resistance [96]. It is expressed during embryonic development but absent from differentiated cells [97]. Survivin is overexpressed in 70–80% of pancreatic cancers and is associated with resistance to chemoradiotherapy [98,99]. Vaccination with Vaccinia Ankara virus, a nonreplicating attenuated VV strain, armed with survivin induced survivin-specific CD8+ immune response resulting in a modest antitumor effect. When combined gemcitabine antitumor immunity and efficacy improved significantly. This is likely to be related to gemcitabine suppression of myeloid-derived suppressor cells [100].
The only VV-based cancer vaccine to enter clinical trials is PANVAC-V, a VV expressing carcinoembryonic antigen and mucin-1, both highly expressed in pancreatic cancers. The two antigens were packaged with three costimulatory molecules: B7.1 (cluster of differentiation 80), ICAM-1 (intracellular adhesion molecule one) and LFA-3 (leukocyte function-associated antigen-3) known collectively as TRICOM. To further enhance the immune response, the vaccination was delivered as a heterologous prime/boost regimen using a nonreplicating fowlpox vector expressing the same antigens and costimulatory molecules (PANVAC-F) [101]. GM-CSF was administered at the injection site as an adjuvant to enhance local antigen processing and presentation. In a Phase I clinical trial, the vaccine was found to be safe and well tolerable. It generated an antigen-specific immune response toward carcinoembryonic antigen and mucin-1 which correlated with increased survival [102]. However, Phase III trial (NCT00088660) targeting patients with metastatic pancreatic cancer who failed gemcitabine treatment failed to meet its therapeutic targets and was terminated [103]. The vaccine is currently under investigation for direct intratumoral injection under endoscopic ultrasound guidance with encouraging results of Phase I trial [104].
Future perspective
There has been a great interest in VV in recent years. Its safety, cancer tropism, amenability to genetic modification and ability to target solid tumors via a variety of mechanism of actions have made it a near-perfect onclytic virus to target pancreatic cancers. Nevertheless, as with any new therapeutic agents VV therapy need to overcome many hurdles and challenges before it enters routine clinical practice.
The first challenge is the selection of the right VV strain. The nonvaccine strain Western Reserve (WR) VV is widely used in the lab. JX-963, a GM-CSF armed mutant of WR VV with deletion of both the Thymidine Kinase and the Viral Growth Factor gene, has been reported as the most potent tumor-targeted oncolytic VV [52]. Other strains, such as the European vaccine Lister strain, are largely untested. We recently evaluated the antitumor potency and biodistribution of different VV strains using in vitro and in vivo models of cancer, including pancreatic cancer models. The Lister strain virus with Thymidine Kinase gene deletion (VVΔTK) demonstrated superior antitumor potency and cancer-selective replication in vitro and in vivo, compared with WRDD, especially in human cancer cell lines and immune-competent hosts. Further investigation of functional mechanisms revealed that Lister VVΔTK presented favorable viral biodistribution within the tumors, with lower levels of proinflammatory cytokines compared with WRDD, suggesting that Lister strain may induce a diminished host inflammatory response [105]. Our comprehensive study indicates that the Lister strain VV with TK deletion is a particularly promising VV strain for the development of the next generation of tumor-targeted oncolytic therapeutics. We anticipate that more and more people will use the Lister stain of VV as a backbone to develop new OVs for cancer treatment in the future.
Further genetic modifications of VV might enhance its oncolytic ability. Disruption of the N1L gene reduces virulence and inhibits VV replication in the brain reducing the risk postvaccinial encephalitis, a rare but significant complication of VV vaccination [106,107]. Our unpublished work on N1L-deleted VV suggests that N1L-deleted VV resulted in a superior antitumor efficacy compared with N1L-intact VV [ahmed, j. et al., unpublished data][query-q9: bryony amber(pe) to all(au)]please provide the first name initials for this author.[reply by: yaohe wang(au)]added[resolved by: bryony amber(pe)]. In addition, arming the new generation of VV with immune-modulatory genes or other therapeutic genes that enhance the antitumor immunity is a future for cancer treatment using tumor-targeted OVs.
Achieving the right immune response is of a paramount importance. Increasingly safer viruses permits the use of higher doses to maximize therapeutic effect [8], however higher viral load might deviate the immune response toward antiviral immunity resulting in rapid viral clearance and reduced antitumor immunity. Manipulating the immune system with cytokine-armed viruses is not without its risks including serious autoimmune side effects [108].
Systemic delivery of VV is particularly relevant in pancreatic cancer as most pancreatic tumors present with distant metastasis at the time of diagnosis. One such virus (JX594) has recently been shown to effectively target tumors after intravenous infusion, making it an ideal OV for treatment of inaccessible tumors such as pancreatic cancer [7]. To date, the systemic delivery of OVs has been shown to be safe but not efficacious mainly due to the rapid clearance of these agents by the immune system [109]. When designing new strategy to enhance the systemic delivery of VV lessons can be learnt from other OVs. Serotype exchange [110,111], engineering new serotypes [112] and the use of chemical shielding [113] have been successfully used with other OVs. In fact the latter strategy have been used to modify the nonreplicating Vaccinia Ankara vaccine vector to circumvent pre-existing anti-VV immunity [114]. Other approaches include pharmacologically modifying the immune response to reduce the neutralization of the systemically delivered OVs [115–117].
Combining oncolytic virotherapy with traditional cancer treatments is an area of great promise. Gemcitabine can suppress myloid-derived suppressor cells in the tumor microenvironment resulting in a stronger antitumor immune response [118]. On the other hand, gemcitabine is a nucleoside analogue that inhibits DNA synthesis including that of double-stranded DNA viruses [119]. Using these agents in a sequential rather than combination manner might be the key to effective therapy [120]. Similarly, combining OVs with immune checkpoints inhibitors is an area that requires more investigation and optimization. PD-1 and CTLA-4 inhibitors might enhance the OV-induced antitumor immunity by creating a favorable immune profile in the tumor microenvironment [121,122].
Despite the challenges, the field of oncolytic virotherapy is generating a great interest of both researchers and pharmaceutical companies alike. The recent US FDA approval of talimogene laherparapvec (T-VEC, an engineered herpes simplex virus-1 expressing GM-CSF), for the treatment of melanoma has given the field a much needed boost. As safety and efficacy data start to accumulate the process of licensing new OVs will get easier. We anticipate other cytokine- and chemokine-armed viruses to enter clinical practice within the next few years. In addition, combining OVs with immune checkpoint therapies, monoclonal antibodies and CAR-T therapies will be an area of major research interest in the near future. Combining immune checkpoint antibodies with other immune-stimulating agents such as conventional drugs, targeted agents and most of all OVs, may increase the tumor types and individual patient profiles in which a durable clinical benefit can be achieved. OVs are finally being recognized for their ability to stimulate antitumor immunity, and with anti-CTLA-4 and anti-PD-1 agents on the market, OVs may finally have met their perfect match. It has never been a more promising era for cancer immunotherapy and personalized medicine.
We believe at the current rate of development it will not be long before OVs are part of routine clinical practice.
Executive summary.
Pancreatic cancer is one of the most aggressive human cancers, without effective therapies.
Tumor-targeted oncolytic viruses is a new class of cancer therapeutic agents.
Oncolytic Vaccinia virus (VV) has distinctive features that make it ideal for treatment of pancreatic cancer.
The antitumor efficacy of oncolytic VV can be further improved by modification of viral genes and arming the virus with therapeutic genes.
Combination of oncolytic VV with other cancer therapies could be the future for treatment of pancreatic cancer.
Footnotes
Financial & competing interests disclosure
This project was funded by the Medical Research Council of the UK (MR/MD15696/1), Ministry of Sciences and Technology, China (2013DFG32080) and the UK Charity Pancreatic Cancer Research Fund as well Pancreatic Cancer Research UK. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
References
- 1.Cancer Research UK. Cancer Research UK; 2014. Pancreatic cancer key stats. [Google Scholar]
- 2.Allison DC, Piantadosi S, Hruban RH, et al. DNA content and other factors associated with ten-year survival after resection of pancreatic carcinoma. J. Surg. Oncol. 1998;67(3):151–159. doi: 10.1002/(sici)1096-9098(199803)67:3<151::aid-jso2>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 3.Garcea G, Dennison AR, Pattenden CJ, et al. Survival following curative resection for pancreatic ductal adenocarcinoma. A systematic review of the literature. JOP. 2008;9(2):99–132. [PubMed] [Google Scholar]
- 4.Burris HA, 3rd, Moore MJ, Andersen J, et al. Improvements in survival and clinical benefit with gemcitabine as first-line therapy for patients with advanced pancreas cancer: a randomized trial. J. Clin. Oncol. 1997;15(6):2403–2413. doi: 10.1200/JCO.1997.15.6.2403. [DOI] [PubMed] [Google Scholar]
- 5.Moore MJ, Goldstein D, Hamm J, et al. Erlotinib plus gemcitabine compared with gemcitabine alone in patients with advanced pancreatic cancer: a Phase iii trial of the national cancer institute of canada clinical trials group. J. Clin. Oncol. 2007;25(15):1960–1966. doi: 10.1200/JCO.2006.07.9525. [DOI] [PubMed] [Google Scholar]
- 6.Moss B. Reflections on the early development of poxvirus vectors. Vaccine. 2013;31(39):4220–4222. doi: 10.1016/j.vaccine.2013.03.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Breitbach CJ, Burke J, Jonker D, et al. Intravenous delivery of a multi-mechanistic cancer-targeted oncolytic poxvirus in humans. Nature. 2011;477(7362):99–102. doi: 10.1038/nature10358. [DOI] [PubMed] [Google Scholar]
- 8.Heo J, Reid T, Ruo L, et al. Randomized dose-finding clinical trial of oncolytic immunotherapeutic vaccinia jx-594 in liver cancer. Nat. Med. 2013;19(3):329–336. doi: 10.1038/nm.3089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wong HH, Lemoine NR, Wang Y. Oncolytic viruses for cancer therapy: overcoming the obstacles. Viruses. 2010;2(1):78–106. doi: 10.3390/v2010078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fiola C, Peeters B, Fournier P, et al. Tumor selective replication of newcastle disease virus: association with defects of tumor cells in antiviral defence. Int. J. Cancer. 2006;119(2):328–338. doi: 10.1002/ijc.21821. [DOI] [PubMed] [Google Scholar]
- 11.Krishnamurthy S, Takimoto T, Scroggs RA, Portner A. Differentially regulated interferon response determines the outcome of newcastle disease virus infection in normal and tumor cell lines. J. Virol. 2006;80(11):5145–5155. doi: 10.1128/JVI.02618-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu XY, Qiu SB, Zou WG, et al. Effective gene-virotherapy for complete eradication of tumor mediated by the combination of htrail (tnfsf10) and plasminogen k5. Mol. Ther. 2005;11(4):531–541. doi: 10.1016/j.ymthe.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 13.Zhang Y, Gu J, Zhao L, et al. Complete elimination of colorectal tumor xenograft by combined manganese superoxide dismutase with tumor necrosis factor-related apoptosis-inducing ligand gene virotherapy. Cancer Res. 2006;66(8):4291–4298. doi: 10.1158/0008-5472.CAN-05-1834. [DOI] [PubMed] [Google Scholar]
- 14.Freytag SO, Rogulski KR, Paielli DL, et al. A novel three-pronged approach to kill cancer cells selectively: concomitant viral, double suicide gene, and radiotherapy. Hum. Gene Ther. 1998;9(9):1323–1333. doi: 10.1089/hum.1998.9.9-1323. [DOI] [PubMed] [Google Scholar]
- 15.Diaconu I, Cerullo V, Hirvinen ML, et al. Immune response is an important aspect of the antitumor effect produced by a CD40L-encoding oncolytic adenovirus. Cancer Res. 2012;72(9):2327–2338. doi: 10.1158/0008-5472.CAN-11-2975. [DOI] [PubMed] [Google Scholar]
- 16.Miyamoto S, Inoue H, Nakamura T, et al. Coxsackievirus b3 is an oncolytic virus with immunostimulatory properties that is active against lung adenocarcinoma. Cancer Res. 2012;72(10):2609–2621. doi: 10.1158/0008-5472.CAN-11-3185. [DOI] [PubMed] [Google Scholar]
- 17.Donnelly OG, Errington-Mais F, Steele L, et al. Measles virus causes immunogenic cell death in human melanoma. Gene Ther. 2013;20(1):7–15. doi: 10.1038/gt.2011.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liikanen I, Ahtiainen L, Hirvinen ML, et al. Oncolytic adenovirus with temozolomide induces autophagy and antitumor immune responses in cancer patients. Mol. Ther. 2013;21(6):1212–1223. doi: 10.1038/mt.2013.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kaufman HL, Kim DW, Deraffele G, et al. Local and distant immunity induced by intralesional vaccination with an oncolytic herpes virus encoding gm-csf in patients with stage iiic and iv melanoma. Ann. Surg. Oncol. 2010;17(3):718–730. doi: 10.1245/s10434-009-0809-6. [DOI] [PubMed] [Google Scholar]
- 20.Tysome JR, Li X, Wang S, et al. A novel therapeutic regimen to eradicate established solid tumors with an effective induction of tumor-specific immunity. Clin. Cancer Res. 2012;18(24):6679–6689. doi: 10.1158/1078-0432.CCR-12-0979. [DOI] [PubMed] [Google Scholar]
- 21.Nishizaki M, Meyn RE, Levy LB, et al. Synergistic inhibition of human lung cancer cell growth by adenovirus-mediated wild-type p53 gene transfer in combination with docetaxel and radiation therapeutics in vitro and in vivo. Clin. Cancer Res. 2001;7(9):2887–2897. [PubMed] [Google Scholar]
- 22.Dai MH, Zamarin D, Gao SP, et al. Synergistic action of oncolytic herpes simplex virus and radiotherapy in pancreatic cancer cell lines. Br. J. Surg. 2010;97(9):1385–1394. doi: 10.1002/bjs.7124. [DOI] [PubMed] [Google Scholar]
- 23.Miranda E, Maya Pineda H, Oberg D, et al. Adenovirus-mediated sensitization to the cytotoxic drugs docetaxel and mitoxantrone is dependent on regulatory domains in the e1acr1 gene-region. PLoS ONE. 2012;7(10):e46617. doi: 10.1371/journal.pone.0046617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cherubini G, Kallin C, Mozetic A, et al. The oncolytic adenovirus addeltadelta enhances selective cancer cell killing in combination with DNA-damaging drugs in pancreatic cancer models. Gene Ther. 2011;18(12):1157–1165. doi: 10.1038/gt.2011.141. [DOI] [PubMed] [Google Scholar]
- 25.Garber K. China approves world's first oncolytic virus therapy for cancer treatment. J. Natl Cancer Inst. 2006;98(5):298–300. doi: 10.1093/jnci/djj111. [DOI] [PubMed] [Google Scholar]
- 26.Hecht JR, Bedford R, Abbruzzese JL, et al. A Phase i/ii trial of intratumoral endoscopic ultrasound injection of onyx-015 with intravenous gemcitabine in unresectable pancreatic carcinoma. Clin. Cancer Res. 2003;9(2):555–561. [PubMed] [Google Scholar]
- 27.Kirn D. Replication-selective oncolytic adenoviruses: virotherapy aimed at genetic targets in cancer. Oncogene. 2000;19(56):6660–6669. doi: 10.1038/sj.onc.1204094. [DOI] [PubMed] [Google Scholar]
- 28.Mulvihill S, Warren R, Venook A, et al. Safety and feasibility of injection with an e1b-55 kda gene-deleted, replication-selective adenovirus (onyx-015) into primary carcinomas of the pancreas: a Phase i trial. Gene Ther. 2001;8(4):308–315. doi: 10.1038/sj.gt.3301398. [DOI] [PubMed] [Google Scholar]
- 29.Nakao A, Kasuya H, Sahin TT, et al. A Phase I dose-escalation clinical trial of intraoperative direct intratumoral injection of HF10 oncolytic virus in non-resectable patients with advanced pancreatic cancer. Cancer Gene Ther. 2011;18(3):167–175. doi: 10.1038/cgt.2010.65. [DOI] [PubMed] [Google Scholar]
- 30.Smith GL, Moss B. Infectious poxvirus vectors have capacity for at least 25 000 base pairs of foreign DNA. Gene. 1983;25(1):21–28. doi: 10.1016/0378-1119(83)90163-4. [DOI] [PubMed] [Google Scholar]
- 31.Griffiths G, Roos N, Schleich S, Locker JK. Structure and assembly of intracellular mature vaccinia virus: thin-section analyses. J. Virol. 2001;75(22):11056–11070. doi: 10.1128/JVI.75.22.11056-11070.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Griffiths G, Wepf R, Wendt T, et al. Structure and assembly of intracellular mature vaccinia virus: isolated-particle analysis. J. Virol. 2001;75(22):11034–11055. doi: 10.1128/JVI.75.22.11034-11055.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Broyles SS. Vaccinia virus transcription. J. Gen. Virol. 2003;84(Pt 9):2293–2303. doi: 10.1099/vir.0.18942-0. [DOI] [PubMed] [Google Scholar]
- 34.Mallardo M, Leithe E, Schleich S, et al. Relationship between vaccinia virus intracellular cores, early mrnas, and DNA replication sites. J. Virol. 2002;76(10):5167–5183. doi: 10.1128/JVI.76.10.5167-5183.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Joklik WK. Vaccinia virus deoxyribonucleic acid: a genome replicating in the cytoplasm. Res. Publ. Assoc. Res. Nerv. Ment. Dis. 1968;44:87–101. [PubMed] [Google Scholar]
- 36.Mercer J, Knebel S, Schmidt FI, et al. Vaccinia virus strains use distinct forms of macropinocytosis for host-cell entry. Proc. Natl Acad. Sci. USA. 2010;107(20):9346–9351. doi: 10.1073/pnas.1004618107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Moss B. Poxvirus entry and membrane fusion. Virology. 2006;344(1):48–54. doi: 10.1016/j.virol.2005.09.037. [DOI] [PubMed] [Google Scholar]
- 38.Putz MM, Midgley CM, Law M, Smith GL. Quantification of antibody responses against multiple antigens of the two infectious forms of vaccinia virus provides a benchmark for smallpox vaccination. Nat. Med. 2006;12(11):1310–1315. doi: 10.1038/nm1457. [DOI] [PubMed] [Google Scholar]
- 39.Vanderplasschen A, Mathew E, Hollinshead M, et al. Extracellular enveloped vaccinia virus is resistant to complement because of incorporation of host complement control proteins into its envelope. Proc. Natl Acad. Sci. USA. 1998;95(13):7544–7549. doi: 10.1073/pnas.95.13.7544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vanderplasschen A, Hollinshead M, Smith GL. Antibodies against vaccinia virus do not neutralize extracellular enveloped virus but prevent virus release from infected cells and comet formation. J. Gen. Virol. 1997;78(Pt 8):2041–2048. doi: 10.1099/0022-1317-78-8-2041. [DOI] [PubMed] [Google Scholar]
- 41.Girgis NM, Dehaven BC, Fan X, et al. Cell surface expression of the vaccinia virus complement control protein is mediated by interaction with the viral a56 protein and protects infected cells from complement attack. J. Virol. 2008;82(9):4205–4214. doi: 10.1128/JVI.02426-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kotwal GJ, Isaacs SN, Mckenzie R, et al. Inhibition of the complement cascade by the major secretory protein of vaccinia virus. Science. 1990;250(4982):827–830. doi: 10.1126/science.2237434. [DOI] [PubMed] [Google Scholar]
- 43.Sahu A, Isaacs SN, Soulika AM, Lambris JD. Interaction of vaccinia virus complement control protein with human complement proteins: factor i-mediated degradation of C3B to IC3B1 inactivates the alternative complement pathway. J. Immunol. 1998;160(11):5596–5604. [PubMed] [Google Scholar]
- 44.Kirn DH, Wang Y, Liang W, Contag CH, Thorne SH. Enhancing poxvirus oncolytic effects through increased spread and immune evasion. Cancer Res. 2008;68(7):2071–2075. doi: 10.1158/0008-5472.CAN-07-6515. [DOI] [PubMed] [Google Scholar]
- 45.Pipiya T, Sauthoff H, Huang YQ, et al. Hypoxia reduces adenoviral replication in cancer cells by downregulation of viral protein expression. Gene Ther. 2005;12(11):911–917. doi: 10.1038/sj.gt.3302459. [DOI] [PubMed] [Google Scholar]
- 46.Hiley CT, Yuan M, Lemoine NR, Wang Y. Lister strain vaccinia virus, a potential therapeutic vector targeting hypoxic tumours. Gene Ther. 2010;17(2):281–287. doi: 10.1038/gt.2009.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Center for Disease Control and Prevention. Vaccinia (smallpox) vaccine: recommendations of the Advisory Committee On Immunization Practices (ACIP) MMWR. 2001;50:7–11. 2001 (RR-10) [PubMed] [Google Scholar]
- 48.Haim M, Gdalevich M, Mimouni D, et al. Adverse reactions to smallpox vaccine: the israel defense force experience, 1991 to 1996. A comparison with previous surveys. Mil. Med. 2000;165(4):287–289. [PubMed] [Google Scholar]
- 49.Zeh HJ, Bartlett DL. Development of a replication-selective, oncolytic poxvirus for the treatment of human cancers. Cancer Gene Ther. 2002;9(12):1001–1012. doi: 10.1038/sj.cgt.7700549. [DOI] [PubMed] [Google Scholar]
- 50.Tysome JR, Briat A, Alusi G, et al. Lister strain of vaccinia virus armed with endostatin-angiostatin fusion gene as a novel therapeutic agent for human pancreatic cancer. Gene Ther. 2009;16(10):1223–1233. doi: 10.1038/gt.2009.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Parato KA, Breitbach CJ, Le Boeuf F, et al. The oncolytic poxvirus jx-594 selectively replicates in and destroys cancer cells driven by genetic pathways commonly activated in cancers. Mol. Ther. 2012;20(4):749–758. doi: 10.1038/mt.2011.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Thorne SH, Hwang TH, O'Gorman WE, et al. Rational strain selection and engineering creates a broad-spectrum, systemically effective oncolytic poxvirus, jx-963. J. Clin. Invest. 2007;117(11):3350–3358. doi: 10.1172/JCI32727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yu YA, Shabahang S, Timiryasova TM, et al. Visualization of tumors and metastases in live animals with bacteria and vaccinia virus encoding light-emitting proteins. Nat. Biotechnol. 2004;22(3):313–320. doi: 10.1038/nbt937. [DOI] [PubMed] [Google Scholar]
- 54.Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 55.Yarden Y. The egfr family and its ligands in human cancer. Signalling mechanisms and therapeutic opportunities. Eur. J. Cancer. 2001;37(Suppl. 4):S3–S8. doi: 10.1016/s0959-8049(01)00230-1. [DOI] [PubMed] [Google Scholar]
- 56.Yang H, Kim SK, Kim M, et al. Antiviral chemotherapy facilitates control of poxvirus infections through inhibition of cellular signal transduction. J. Clin. Invest. 2005;115(2):379–387. doi: 10.1172/JCI23220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Guitard E, Parker F, Millon R, et al. G3bp is overexpressed in human tumors and promotes s Phase entry. Cancer Lett. 2001;162(2):213–221. doi: 10.1016/s0304-3835(00)00638-8. [DOI] [PubMed] [Google Scholar]
- 58.Katsafanas GC, Moss B. Vaccinia virus intermediate stage transcription is complemented by ras-gtpase-activating protein Sh3 domain-binding protein (g3bp) and cytoplasmic activation/proliferation-associated protein (p137) individually or as a heterodimer. J. Biol. Chem. 2004;279(50):52210–52217. doi: 10.1074/jbc.M411033200. [DOI] [PubMed] [Google Scholar]
- 59.Mccart JA, Ward JM, Lee J, et al. Systemic cancer therapy with a tumor-selective vaccinia virus mutant lacking thymidine kinase and vaccinia growth factor genes. Cancer Res. 2001;61(24):8751–8757. [PubMed] [Google Scholar]
- 60.Puhlmann M, Brown CK, Gnant M, et al. Vaccinia as a vector for tumor-directed gene therapy: biodistribution of a thymidine kinase-deleted mutant. Cancer Gene Ther. 2000;7(1):66–73. doi: 10.1038/sj.cgt.7700075. [DOI] [PubMed] [Google Scholar]
- 61.Colamonici OR, Domanski P, Sweitzer SM, et al. Vaccinia virus B18r gene encodes a type I interferon-binding protein that blocks interferon alpha transmembrane signaling. J. Biol. Chem. 1995;270(27):15974–15978. doi: 10.1074/jbc.270.27.15974. [DOI] [PubMed] [Google Scholar]
- 62.Kirn DH, Wang Y, Le Boeuf F, et al. Targeting of interferon-beta to produce a specific, multi-mechanistic oncolytic vaccinia virus. PLoS Med. 2007;4(12):e353. doi: 10.1371/journal.pmed.0040353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Luker KE, Hutchens M, Schultz T, et al. Bioluminescence imaging of vaccinia virus: effects of interferon on viral replication and spread. Virology. 2005;341(2):284–300. doi: 10.1016/j.virol.2005.06.049. [DOI] [PubMed] [Google Scholar]
- 64.Hikichi M, Kidokoro M, Haraguchi T, et al. MicroRNA regulation of glycoprotein B5r in oncolytic vaccinia virus reduces viral pathogenicity without impairing its antitumor efficacy. Mol. Ther. 2011;19(6):1107–1115. doi: 10.1038/mt.2011.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Yu YA, Galanis C, Woo Y, et al. Regression of human pancreatic tumor xenografts in mice after a single systemic injection of recombinant vaccinia virus GLV-1h68. Mol. Cancer Ther. 2009;8(1):141–151. doi: 10.1158/1535-7163.MCT-08-0533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Haddad D, Chen N, Zhang Q, et al. A novel genetically modified oncolytic vaccinia virus in experimental models is effective against a wide range of human cancers. Ann. Surg. Oncol. 2012;19(Suppl. 3):S665–S674. doi: 10.1245/s10434-011-2198-x. [DOI] [PubMed] [Google Scholar]
- 67.Dai MH, Liu SL, Chen NG, et al. Oncolytic vaccinia virus in combination with radiation shows synergistic antitumor efficacy in pancreatic cancer. Cancer Lett. 2014;344(2):282–290. doi: 10.1016/j.canlet.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 68.Liu TC, Hwang T, Park BH, et al. The targeted oncolytic poxvirus jx-594 demonstrates antitumoral, antivascular, and anti-HBV activities in patients with hepatocellular carcinoma. Mol. Ther. 2008;16(9):1637–1642. doi: 10.1038/mt.2008.143. [DOI] [PubMed] [Google Scholar]
- 69.Breitbach CJ, Paterson JM, Lemay CG, et al. Targeted inflammation during oncolytic virus therapy severely compromises tumor blood flow. Mol. Ther. 2007;15(9):1686–1693. doi: 10.1038/sj.mt.6300215. [DOI] [PubMed] [Google Scholar]
- 70.Ikeda N, Adachi M, Taki T, et al. Prognostic significance of angiogenesis in human pancreatic cancer. Br. J. Cancer. 1999;79(9–10):1553–1563. doi: 10.1038/sj.bjc.6690248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Scappaticci FA, Contreras A, Smith R, et al. Statin-AE: a novel angiostatin-endostatin fusion protein with enhanced antiangiogenic and antitumor activity. Angiogenesis. 2001;4(4):263–268. doi: 10.1023/a:1016067717433. [DOI] [PubMed] [Google Scholar]
- 72.Bell J, Mcfadden G. Viruses for tumor therapy. Cell Host Microbe. 2014;15(3):260–265. doi: 10.1016/j.chom.2014.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tong AW, Senzer N, Cerullo V, et al. Oncolytic viruses for induction of anti-tumor immunity. Curr. Pharm. Biotechnol. 2012;13(9):1750–1760. doi: 10.2174/138920112800958913. [DOI] [PubMed] [Google Scholar]
- 74.Bartlett DL, Liu Z, Sathaiah M, et al. Oncolytic viruses as therapeutic cancer vaccines. Mol. Cancer. 2013;12(1):103. doi: 10.1186/1476-4598-12-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Huang B, Sikorski R, Kirn DH, Thorne SH. Synergistic anti-tumor effects between oncolytic vaccinia virus and paclitaxel are mediated by the IFN response and Hmgb1. Gene Ther. 2011;18(2):164–172. doi: 10.1038/gt.2010.121. [DOI] [PubMed] [Google Scholar]
- 76.Guo ZS, Naik A, O'malley ME, et al. The enhanced tumor selectivity of an oncolytic vaccinia lacking the host range and antiapoptosis genes spi-1 and spi-2 . Cancer Res. 2005;65(21):9991–9998. doi: 10.1158/0008-5472.CAN-05-1630. [DOI] [PubMed] [Google Scholar]
- 77.John LB, Howland LJ, Flynn JK, et al. Oncolytic virus and anti-4–1BB combination therapy elicits strong antitumor immunity against established cancer. Cancer Res. 2012;72(7):1651–1660. doi: 10.1158/0008-5472.CAN-11-2788. [DOI] [PubMed] [Google Scholar]
- 78.Whilding LM, Archibald KM, Kulbe H, et al. Vaccinia virus induces programmed necrosis in ovarian cancer cells. Mol. Ther. 2013;21(11):2074–2086. doi: 10.1038/mt.2013.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zhu J, Martinez J, Huang X, Yang Y. Innate immunity against vaccinia virus is mediated by TLR2 and requires TLR-independent production of IFN-beta. Blood. 2007;109(2):619–625. doi: 10.1182/blood-2006-06-027136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Barbalat R, Lau L, Locksley RM, Barton GM. Toll-like receptor 2 on inflammatory monocytes induces type I interferon in response to viral but not bacterial ligands. Nat. Immunol. 2009;10(11):1200–1207. doi: 10.1038/ni.1792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Delaloye J, Roger T, Steiner-Tardivel QG, et al. Innate immune sensing of modified vaccinia virus ankara (MVA) is mediated by TLR2-TLR6, MDA-5 and the NALP3 inflammasome. PLoS Pathog. 2009;5(6):e1000480. doi: 10.1371/journal.ppat.1000480. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 82.Kim MK, Breitbach CJ, Moon A, et al. Oncolytic and immunotherapeutic vaccinia induces antibody-mediated complement-dependent cancer cell lysis in humans. Sci. Transl. Med. 2013;5(185):185ra163. doi: 10.1126/scitranslmed.3005361. [DOI] [PubMed] [Google Scholar]
- 83.Draper SJ, Moore AC, Goodman AL, et al. Effective induction of high-titer antibodies by viral vector vaccines. Nat. Med. 2008;14(8):819–821. doi: 10.1038/nm.1850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bruña-Romero O, González-Aseguinolaza G, Hafalla JC, et al. Complete, long-lasting protection against malaria of mice primed and boosted with two distinct viral vectors expressing the same plasmodial antigen. Proc. Natl Acad. Sci. USA. 2001;98(20):11491–11496. doi: 10.1073/pnas.191380898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Couper KN, Blount DG, Riley EM. Il-10: the master regulator of immunity to infection. J. Immunol. 2008;180(9):5771–5777. doi: 10.4049/jimmunol.180.9.5771. [DOI] [PubMed] [Google Scholar]
- 86.Chard LS, Maniati E, Wang P, et al. A vaccinia virus armed with interleukin-10 is a promising therapeutic agent for treatment of murine pancreatic cancer. Clin. Cancer Res. 2015;21(2):405–416. doi: 10.1158/1078-0432.CCR-14-0464. [DOI] [PubMed] [Google Scholar]
- 87.Smith GL, Mackett M, Moss B. Infectious vaccinia virus recombinants that express hepatitis B virus surface antigen. Nature. 1983;302(5908):490–495. doi: 10.1038/302490a0. [DOI] [PubMed] [Google Scholar]
- 88.Moss B, Smith GL, Gerin JL, Purcell RH. Live recombinant vaccinia virus protects chimpanzees against hepatitis B. Nature. 1984;311(5981):67–69. doi: 10.1038/311067a0. [DOI] [PubMed] [Google Scholar]
- 89.Meeusen EN, Walker J, Peters A, et al. Current status of veterinary vaccines. Clin. Microbiol. Rev. 2007;20(3):489–510. doi: 10.1128/CMR.00005-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Poulet H, Minke J, Pardo MC, et al. Development and registration of recombinant veterinary vaccines. The example of the canarypox vector platform. Vaccine. 2007;25(30):5606–5612. doi: 10.1016/j.vaccine.2006.11.066. [DOI] [PubMed] [Google Scholar]
- 91.Rerks-Ngarm S, Pitisuttithum P, Nitayaphan S, et al. Vaccination with Alvac and Aidsvax to prevent HIV-1 infection in Thailand. N. Engl. J. Med. 2009;361(23):2209–2220. doi: 10.1056/NEJMoa0908492. [DOI] [PubMed] [Google Scholar]
- 92.Sheehy SH, Duncan CJ, Elias SC, et al. Phase ia clinical evaluation of the safety and immunogenicity of the plasmodium falciparum blood-stage antigen ama1 in chad63 and mva vaccine vectors. PLoS ONE. 2012;7(2):e31208. doi: 10.1371/journal.pone.0031208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sheehy SH, Duncan CJ, Elias SC, et al. Phase ia clinical evaluation of the plasmodium falciparum blood-stage antigen MSP1 in CHAD63 and MVA vaccine vectors. Mol. Ther. 2011;19(12):2269–2276. doi: 10.1038/mt.2011.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Scriba TJ, Tameris M, Mansoor N, et al. Modified vaccinia ankara-expressing ag85a, a novel tuberculosis vaccine, is safe in adolescents and children, and induces polyfunctional CD4+ T cells. Eur. J. Immunol. 2010;40(1):279–290. doi: 10.1002/eji.200939754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Draper SJ, Heeney JL. Viruses as vaccine vectors for infectious diseases and cancer. Nat. Rev. Microbiol. 2010;8(1):62–73. doi: 10.1038/nrmicro2240. [DOI] [PubMed] [Google Scholar]
- 96.Singh N, Krishnakumar S, Kanwar RK, et al. Clinical aspects for survivin: a crucial molecule for targeting drug-resistant cancers. Drug Discov. Today. 2014;20(5):578–587. doi: 10.1016/j.drudis.2014.11.013. [DOI] [PubMed] [Google Scholar]
- 97.Adida C, Crotty PL, Mcgrath J, et al. Developmentally regulated expression of the novel cancer anti-apoptosis gene survivin in human and mouse differentiation. Am. J. Pathol. 1998;152(1):43–49. [PMC free article] [PubMed] [Google Scholar]
- 98.Sarela AI, Verbeke CS, Ramsdale J, et al. Expression of survivin, a novel inhibitor of apoptosis and cell cycle regulatory protein, in pancreatic adenocarcinoma. Br. J. Cancer. 2002;86(6):886–892. doi: 10.1038/sj.bjc.6600133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Kami K, Doi R, Koizumi M, et al. Downregulation of survivin by sirna diminishes radioresistance of pancreatic cancer cells. Surgery. 2005;138(2):299–305. doi: 10.1016/j.surg.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 100.Ishizaki H, Manuel ER, Song GY, et al. Modified vaccinia ankara expressing survivin combined with gemcitabine generates specific antitumor effects in a murine pancreatic carcinoma model. Cancer Immunol. Immunother. 2011;60(1):99–109. doi: 10.1007/s00262-010-0923-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Petrulio CA, Kaufman HL. Development of the panvac-vf vaccine for pancreatic cancer. Expert Rev. Vaccines. 2006;5(1):9–19. doi: 10.1586/14760584.5.1.9. [DOI] [PubMed] [Google Scholar]
- 102.Kaufman HL, Kim-Schulze S, Manson K, et al. Poxvirus-based vaccine therapy for patients with advanced pancreatic cancer. J. Transl. Med. 2007;5:60. doi: 10.1186/1479-5876-5-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Therion reports results of Phase 3 panvac-vf trial and announces plans for company sale. www.prnewswire.com/news-releases/therion-reports-results-of-phase-3-panvac-vf-trial-and-announces-plans-for-company-sale-56997582.html PR Newswire 28 June.
- 104.Riedmann EM. Human vaccines & immunotherapeutics: news. Hum. Vaccin. Immunother. 2014;10(7):1773–1777. doi: 10.4161/hv.36241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Hughes J, Wang P, Alusi G, et al. Lister strain vaccinia virus with thymidine kinase gene deletion is a tractable platform for development of a new generation of oncolytic virus. Gene Ther. 2015;22(6):476–84. doi: 10.1038/gt.2015.13. [DOI] [PubMed] [Google Scholar]
- 106.Billings B, Smith SA, Zhang Z, et al. Lack of n1l gene expression results in a significant decrease of vaccinia virus replication in mouse brain. Ann. NY Acad. Sci. 2004;1030:297–302. doi: 10.1196/annals.1329.037. [DOI] [PubMed] [Google Scholar]
- 107.Bartlett N, Symons JA, Tscharke DC, Smith GL. The vaccinia virus N1l protein is an intracellular homodimer that promotes virulence. J. Gen. Virol. 2002;83(Pt 8):1965–1976. doi: 10.1099/0022-1317-83-8-1965. [DOI] [PubMed] [Google Scholar]
- 108.Poutou J, Bunuales M, Gonzalez-Aparicio M, et al. Safety and antitumor effect of oncolytic and helper-dependent adenoviruses expressing interleukin-12 variants in a hamster pancreatic cancer model. Gene Ther. 2015;22(9):696–706. doi: 10.1038/gt.2015.45. [DOI] [PubMed] [Google Scholar]
- 109.Ferguson MS, Lemoine NR, Wang Y. Systemic delivery of oncolytic viruses: hopes and hurdles. Adv. Virol. 2012;2012:805629. doi: 10.1155/2012/805629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Roberts DM, Nanda A, Havenga MJ, et al. Hexon-chimaeric adenovirus serotype 5 vectors circumvent pre-existing anti-vector immunity. Nature. 2006;441(7090):239–243. doi: 10.1038/nature04721. [DOI] [PubMed] [Google Scholar]
- 111.Kuhlmann KF, Van Geer MA, Bakker CT, et al. Fiber-chimeric adenoviruses expressing fibers from serotype 16 and 50 improve gene transfer to human pancreatic adenocarcinoma. Cancer Gene Ther. 2009;16(7):585–597. doi: 10.1038/cgt.2009.4. [DOI] [PubMed] [Google Scholar]
- 112.Miest TS, Yaiw KC, Frenzke M, et al. Envelope-chimeric entry-targeted measles virus escapes neutralization and achieves oncolysis. Mol. Ther. 2011;19(10):1813–1820. doi: 10.1038/mt.2011.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Kim PH, Kim J, Kim TI, et al. Bioreducible polymer-conjugated oncolytic adenovirus for hepatoma-specific therapy via systemic administration. Biomaterials. 2011;32(35):9328–9342. doi: 10.1016/j.biomaterials.2011.08.066. [DOI] [PubMed] [Google Scholar]
- 114.Naito T, Kaneko Y, Kozbor D. Oral vaccination with modified vaccinia virus ankara attached covalently to TMPEG-modified cationic liposomes overcomes pre-existing poxvirus immunity from recombinant vaccinia immunization. J. Gen. Virol. 2007;88(Pt 1):61–70. doi: 10.1099/vir.0.82216-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Ikeda K, Ichikawa T, Wakimoto H, et al. Oncolytic virus therapy of multiple tumors in the brain requires suppression of innate and elicited antiviral responses. Nat. Med. 1999;5(8):881–887. doi: 10.1038/11320. [DOI] [PubMed] [Google Scholar]
- 116.Ikeda K, Wakimoto H, Ichikawa T, et al. Complement depletion facilitates the infection of multiple brain tumors by an intravascular, replication-conditional herpes simplex virus mutant. J. Virol. 2000;74(10):4765–4775. doi: 10.1128/jvi.74.10.4765-4775.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Kambara H, Saeki Y, Chiocca EA. Cyclophosphamide allows for in vivo dose reduction of a potent oncolytic virus. Cancer Res. 2005;65(24):11255–11258. doi: 10.1158/0008-5472.CAN-05-2278. [DOI] [PubMed] [Google Scholar]
- 118.Le HK, Graham L, Cha E, et al. Gemcitabine directly inhibits myeloid derived suppressor cells in balb/c mice bearing 4T1 mammary carcinoma and augments expansion of T cells from tumor-bearing mice. Int. Immunopharmacol. 2009;9(7–8):900–909. doi: 10.1016/j.intimp.2009.03.015. [DOI] [PubMed] [Google Scholar]
- 119.Watanabe I, Kasuya H, Nomura N, et al. Effects of tumor selective replication-competent herpes viruses in combination with gemcitabine on pancreatic cancer. Cancer Chemother. Pharmacol. 2008;61(5):875–882. doi: 10.1007/s00280-007-0567-8. [DOI] [PubMed] [Google Scholar]
- 120.Wennier ST, Liu J, Li S, et al. Myxoma virus sensitizes cancer cells to gemcitabine and is an effective oncolytic virotherapeutic in models of disseminated pancreatic cancer. Mol. Ther. 2012;20(4):759–768. doi: 10.1038/mt.2011.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Engeland CE, Grossardt C, Veinalde R, et al. CTLA-4 and PD-L1 checkpoint blockade enhances oncolytic measles virus therapy. Mol. Ther. 2014;22(11):1949–1959. doi: 10.1038/mt.2014.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Dias JD, Hemminki O, Diaconu I, et al. Targeted cancer immunotherapy with oncolytic adenovirus coding for a fully human monoclonal antibody specific for CTLA-4. Gene Ther. 2012;19(10):988–998. doi: 10.1038/gt.2011.176. [DOI] [PubMed] [Google Scholar]