SUMMARY
The aim of our study was to assess long-term results of radiofrequency volumetric tissue reduction of inferior turbinates (RVTR). We performed a prospective long-term longitudinal evaluation of 305 patients affected by rhinitis (114 allergic and 191 non-allergic) who were unresponsive to medical treatment and underwent RVTR (January 2004 - December 2010). Subjects were followed for a mean period of 39.70 ± 19.41 months (range 24-60). Patients completed the NOSE-scale questionnaire pre- and post-operatively after 1 month and yearly for 5-years. Recurrence was assumed if the post-operative total NOSE score increased by at least 75% during follow-up and the patient restarted medical treatments. Estimation of relapse over time was performed by Kaplan-Meyer analyses. We documented overall good satisfaction of patients regarding the procedure, with a good rate of pain control and a low rate of complications. Post-operatively there was a significant improvement in nasal stuffiness, nasal obstruction and mouth breathing (p < 0.05). We observed a worsening trend for symptoms after 36 months with progressive increasing rate of recurrences that were significantly higher in allergic than non-allergic patients (p < 0.05). We also observed a slight worsening trend of global satisfaction of patients. Our study confirms the minor discomfort and low risk of side effects of RVTR. Our data showed good efficacy of the procedure in the majority of patients for at least 36 months after surgery, and in fact in this time period the cumulative probability to remain relapse-free was up to 0.8. In the following 2 years, we observed a worse temporal trend in term of recurrence rate, and in particular in allergic patients with a significant difference vs non-allergic individuals (p < 0.05).
KEY WORDS: Non-allergic rhinitis, Allergic rhinitis, Inferior turbinate, Hypertrophy, Radiofrequency, Long-term results, Nasal obstruction, Mouth breathing, Local anaesthesia, Epistaxis, Relapse
RIASSUNTO
Lo scopo del nostro studio è stato quello di valutare i risultati a lungo termine della procedura di riduzione volumetrica dei turbinati inferiori mediante radiofrequenze (RVTR). Abbiamo eseguito una valutazione prospettica longitudinale a lungo termine di 305 pazienti affetti da rinite (114 allergici e 191 non allergici) refrattari alla terapia medica e sottoposti a intervento di RVTR (gennaio 2004 - dicembre 2010). I pazienti sono stati seguiti per un Follow-up medio di 39,70±19,41 mesi (minimo-24, massimo-60 mesi) e sono stati valutati mediante la somministrazione del questionario NOSE-scale prima e dopo l'intervento a distanza di un mese e successivamente ogni anno per 5 anni. I pazienti sono stati considerati affetti da recidiva durante il periodo di follow-up in caso di ricomparsa dei sintomi con un aumento del punteggio totale del NOSE scale di almeno il 75% e necessità di riassumere trattamenti medici. La ricorrenza è stata valutata mediante analisi di sopravvivenza con il metodo di Kaplan-Meyer. Complessivamente abbiamo documentato una buona soddisfazione dei pazienti per quanto riguarda la procedura, con un elevato controllo del dolore e poche complicanze. Nel post-operatorio abbiamo avuto un significativo miglioramento di ostruzione nasale e respirazione orale vicariante (p < 0,05). Dopo 36 mesi abbiamo osservato un peggioramento dei sintomi, in particolare, dopo 36 mesi con un progressivo crescente tasso di recidive significativamente più elevato nei pazienti allergici rispetto a quelli non-allergici (p < 0,05). Abbiamo anche osservato una leggera diminuizione della soddisfazione generale dei pazienti. Il nostro studio conferma la buona tollerabilità da parte dei pazienti della procedura di decongestione dei turbinati inferiori con radiofrequenze con un basso rischio di complicanze. I nostri dati confermano inoltre una buona efficacia a lungo termine nella maggior parte dei pazienti per almeno 36 mesi dopo l'intervento con una probabilità di rimanere liberi da recidiva in questo periodo sempre superiore a 0,8. Nei mesi successivi si assiste a una progressiva riduzione del beneficio clinico in particolare nei pazienti allergici, con una differenza statisticamente significativa rispetto ai pazienti non allergici (p < 0,05).
Introduction
Turbinate surgery is very common and has been reported as the eighth most common procedure performed by otolaryngologists 1 2. Bilateral inferior turbinate enlargement occurs in patients suffering from allergic seasonal or perennial rhinitis or vasomotor non-allergic rhinitis with more frequent hyperplasia of the head of the turbinate. Furthermore, chronic inflammatory condition may lead to hyperplasia of the mucosa and sub-mucosa, generally observed on the end of the turbinate, or morphologically presenting as polypoid formation of new tissue 3-5.
At least 13 surgical techniques have been used over the past 130 years 1. All authors agree that in modern functional nasal surgery there is no place for total or subtotal turbinectomy due to the risk of haemorrhage, postoperative pain and longterm complications, and especially atrophic rhinitis 6. All reduction techniques are successful, but vary significantly in terms of long-term efficacy and risk of complications. Nevertheless, no ideal standard technique has been developed to date, and in particular there is a lack of prospective and comparable long-term studies, which makes it difficult to recommend evidence-based surgical techniques 7-10.
The aim of our study was to assess the long-term results of radiofrequency volumetric tissue reduction (RFVTR) of the inferior turbinates in patients with nasal obstruction caused by turbinate hypertrophy.
Materials and methods
This single institution longitudinal prospective study was performed at the Department of Head and Neck Surgery Otorhinolaryngology of Catholic University of the Sacred Heart in Rome. The protocol was approved by our institutional board. All subjects gave written informed consent. From January 2004 to December 2010, 337 patients (205 males, 132 females), aged between 18-71 years, underwent RFVTR for treatment of simple bilateral hypertrophy of the turbinates that was not responsive to three-months of conservative therapy (intranasal sprays, antihistamines, systemic decongestants, mast cell stabilisers and allergic desensitisation) 10 11.
A total of 305 (133 female and 172 male) of 337 patients were included for statistical analyses and 32 were excluded because they were lost to follow-up. Of these, 37.37% (114/305) of patients were affected by allergic rhinitis and 62.63% (191/305) by non-allergic rhinitis. Subjects were followed for a mean period of 39.70 ± 19.41 months (range 24-60).
Pre-operative clinical evaluation included complete history and physical head and neck examination with nasal endoscopy, allergy testing through serum total IgE, allergometric skin testing for common inhalant allergens and determination of the levels of specific IgE in serum. In all patients we excluded chronic rhinosinusitis (according to the criteria of EPOS guidelines 8 for chronic rhinosinusitis), previous head and neck cancer, prior radiation therapy, rhinoplasty, active nasal infection, severe septal deformity, septal perforation, facial anomalies, connective tissue disorder and autoimmune disease, or nasal valve region deformity).
Patients were asked to complete a NOSE Scale questionnaire 9 pre-operatively, and then post-operatively at 1 month (Table I) and yearly for a maximum of 5 years. In the first month subjects were followed every week for 4 weeks to complete early evaluation of symptoms such as pain, rhinorrhoea, itching, sneezing, crusting and congestion scored by visual analogue scale (VAS) (range 0-10). The patient was asked to indicate on a VAS the answer to the question: "How troublesome are your symptoms?". Patients were told that 0 indicated 'nasal symptoms not at all bothersome' and that 10 indicated 'nasal symptoms extremely bothersome'. At 4 weeks after surgery patients were asked to formulate a final global evaluation of the procedure using a VAS scale (range 0-10). Successively, patients were followed-up for recurrence at yearly intervals for a maximum of 5 years. At every follow-up patients were asked about the need to restart medical treatment and the NOSE scale questionnaire was repeated. We obtained for every patient a total NOSE scale score from 0 to 20; then scaled to a total NOSE score from 0 to 100 multiplying the scores of the five items by 5. Recurrence was assumed if the post-operative total NOSE score increased by at least 75% during followup and the patient restarted medical treatments.
Table I.
NOSE scale questionnaire.
| NOSE scale | Over the past 1 month how much of a problem were the following conditions for you? Please mark the most correct response |
|||||
|---|---|---|---|---|---|---|
| Not a problem |
Very mild problem |
Moderate problem |
Fairly bad problem |
Severe problem |
||
| 1 | Nose obstruction and stuffiness | 0 | 1 | 2 | 3 | 4 |
| 2 | Nose blockage or obstruction | 0 | 1 | 2 | 3 | 4 |
| 3 | Trouble breathing through my nose or mouth breathing | 0 | 1 | 2 | 3 | 4 |
| 4 | Trouble sleeping | 0 | 1 | 2 | 3 | 4 |
| 5 | Unable to get enough air through my nose during exercise or exertion | 0 | 1 | 2 | 3 | 4 |
All procedures were performed in outpatient facilities with local anaesthesia using cotton strips with a 1:1 mixture of lidocaine and xylometazoline hydrochloride and conscious or deep sedation with midazolam or propofol. No premedication was given. Pain during the procedure was scored as none, mild, moderate and severe.
The surgery was performed using a radiofrequency system Celon Lab Precision (Olympus). Radiofrequency creates ionic agitation in tissue, inducing hypertermic sub-mucosal necrosis. The target temperature can be controlled from 60°C to 75°C to prevent surrounding tissue damage. It allows safe and gentle sub-mucosal volume reduction of hyperplastic nasal turbinate, developing predictably sized lesions in 4-10 sec. The resultant wound contraction and fibrosis of the sub-mucosa causes volume reduction of the inferior turbinate without damage to the overlying mucosa that adheres to the turbinate periosteum. This conservative procedure also damages sub-mucosal nerve fibres and the receptor nerve leading to denervation and hyporeactivity of turbinate mucosa. We never performed turbinate outfracture in combination with RFVTR 10-12.
Technically, the probe is introduced into the turbinate head under direct vision making 3-4 tunnels and maintaining a sufficient distance from the mucosa and bone. The process of ablation is accompanied by an acoustic tone that rises in pitch as the resistance of the tissue increases. No packing or antibiotic therapy was used after the operation.
For statistical analysis, we used Stata IC 12 software for MAC. The results are shown as mean and standard deviation(SD), median and interquartile range(IQR) or frequency relative percentages, as appropriate. With regards to outcome variables, comparisons between time 0 (PRE-intervention) and time 1 (4 weeks POST-intervention) were performed using a paired t-test. Kaplan-Meier analysis was used to estimate recurrence over time; the comparison between two relapse curves was made by the log-rank test. The results were considered statistically significant for p values < 0.05.
Results
During surgery we obtained a good rate of pain control that was considered absent in 225/305 patients (73.7%), mild in 40/305 (13.3%), moderate in 20/305 (6.5%) and severe in 20/305 (6.5%). A few patients (26/305; 8.5%) required prescription of analgesics after the procedure. The procedures were well tolerated as demonstrated by the early post-operative evaluation (1 week after surgery) using mean VAS values scores of symptoms such as nasal airway obstruction, crusting, sneezing, runny nose and itching (Table II).
Table II.
Post-operative mean VAS scores (range 0-10) and standard deviation of symptoms at early evaluation 1 week after surgery.
| VAS scale | Mean | SD |
|---|---|---|
| Nasal obstruction | 0.9 | 2.0 |
| Rhinorrhoea | 2.0 | 2.8 |
| Itching | 1.2 | 2.1 |
| Sneezing | 1.9 | 2.3 |
| Crusting | 2.6 | 2.8 |
| Intermittent Congestion | 4.7 | 3.1 |
| Persistent Congestion | 4.6 | 3.0 |
Results of anesthesiological questionnaires are shown in Table III. In the first months after surgery, the mean global evaluation score was of 7.3 ± 2.1, indicating good satisfaction of patients. No immediate complications such as major bleeding related to the treatment were observed after radiofrequency. Only 4 of 305 patients (1.3%) had postoperatively bleeding and nasal packing was needed. The most common complaints were transient side effects, including minor nasal discharge and post-procedural obstruction for up to 5-7 days. Subjects' estimation of symptoms by the NOSE scale was repeated at every follow-up evaluation. The mean baseline nose scale score and comparison to post-operative values at 1 month after the procedure are showed in Figure 1 and Table IV. We evaluated the temporal trend of the benefit obtained with surgery for the items of the NOSE scale that significantly improved as shown in Figure 2. We observed a worsening trend of the benefit obtained even though some patients experienced no change of benefit for extended periods. We also evaluated the temporal trend of global satisfaction of patients measured by VAS score (range 0-10) as shown in Figure 3.
Table III.
Anaesthesiologic questionnaire and results.
| Pain control during the procedure |
No pain 225/305 (73.7%) |
Mild pain 40/305 (12.9%) |
Moderate pain 20/305 (6.5%) |
Severe pain 20/305 (6.5%) |
| Anxiety during the procedure |
Yes 76/305 pts (24.91%) No 225/305 pts (73.7%) |
|||
| Recovery time |
Minutes 260/305 pts (85.24%) |
Hours 50/305 pts (16.39%) |
||
| Other problems (nausea, sickness, shiver etc.) |
Yes 70/305 pts (22.9%) No 120 pts (77.4%) |
|||
Fig. 1.
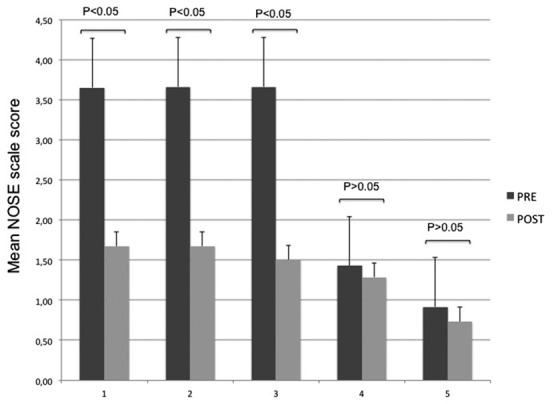
The figure shows differences respect to baseline of NOSE scale scores items comparing time 0 (PRE intervention) and time 1 values (4 week POST intervention). (1) Nose obstruction and stuffiness. (2) Nose blockage or obstruction. (3) Trouble breathing through my nose or mouth breathing. (4) Trouble sleeping. (5) Unable to get enough air through my nose during exercise or exertion.
Table IV.
Comparisons between time 0 (PRE intervention) and time 1 (4 week POST intervention) mean and median nose scale scores.
| Nose congestion or stuffiness p < 0.05 |
Nose blockage or obstruction p < 0.05 |
Trouble breathing through my nose or mouth breathing p < 0.05 |
Trouble sleeping p > 0.05 |
Unable to get enough air through my nose during exercise or exertion p > 0.05 |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| PRE | POST | PRE | POST | PRE | POST | PRE | POST | PRE | POST | |
| Mean | 3.6 | 1.7 | 3.7 | 1.8 | 3.7 | 1.6 | 1.5 | 1.3 | 1.1 | 0.7 |
| SD | 1.2 | 1.1 | 1.2 | 1.2 | 1.2 | 1.2 | 1.4 | 1.3 | 1.2 | 1.1 |
| Median | 4 | 2 | 4 | 2 | 4 | 2 | 1 | 1 | 1 | 0 |
| IQR | 1 | 2 | 1 | 2 | 1 | 1 | 3 | 2 | 2 | 1 |
Fig. 2.
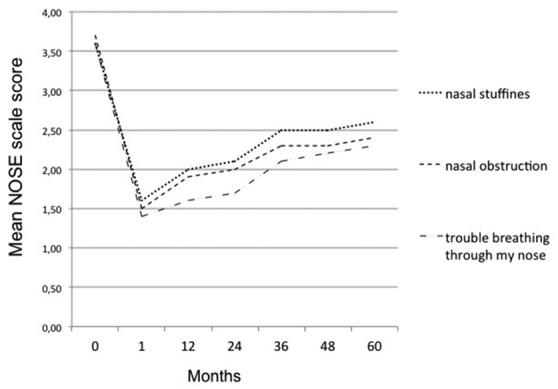
Temporal trend of the benefit obtained with surgery considering evolution during long-term follow-up of mean NOSE scores for items that significantly improved after surgery.
Fig. 3.
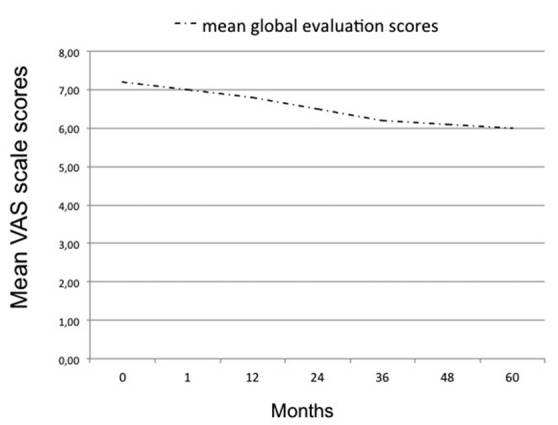
Temporal trend of global patient satisfaction evaluated during longterm follow-up by the VAS score (range 0-10). The indicator represents the mean VAS scores about global satisfaction at each follow-up visit.
Estimation of recurrence was performed in all patients by Kaplan Meyer analysis as shown in Figure 4. The cumulative probability to remain relapse-free was 0.848 at 36 months and 0.531 at 60 months after surgery as shown in Table V. In order to test if allergy could be a discriminating factor in the impact of intervention, the analysis of recurrence was stratified by the presence of allergy (Fig. 5). The analysis showed that allergic patients seemed to be worse in the post-intervention period compared to nonallergic patients, and in particular at long-term follow-up. In fact, cumulative probability to remain relapse-free in allergic and non-allergic patients was respectively 0.839 vs 0.807 at 36 months, and 0.616 vs 0.357 at 60 months (Table V). The log rank test revealed that the difference between curves was statistically significant (p < 0.05).
Fig. 4.
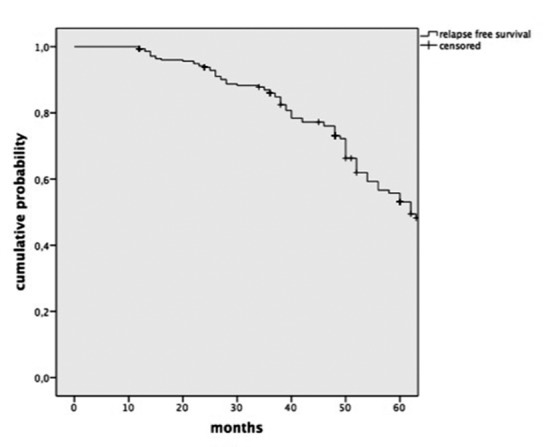
Estimation of recurrence over time by Kaplan-Meier analysis in all 305 patients enrolled.
Table V.
Cumulative probability to remain free of relapse obtained by Kaplan Meyer analyses in all patients and in allergic and non-allergic patients.
| Months of follow-up | |||||
|---|---|---|---|---|---|
| 12 | 24 | 36 | 48 | 60 | |
| All patients | 0.993 | 0.928 | 0.848 | 0.722 | 0.531 |
| Non-allergic patients | 0.989 | 0.930 | 0.839 | 0.729 | 0.616 |
| Allergic patients | 0.934 | 0.902 | 0.807 | 0.575 | 0.357 |
Fig. 5.
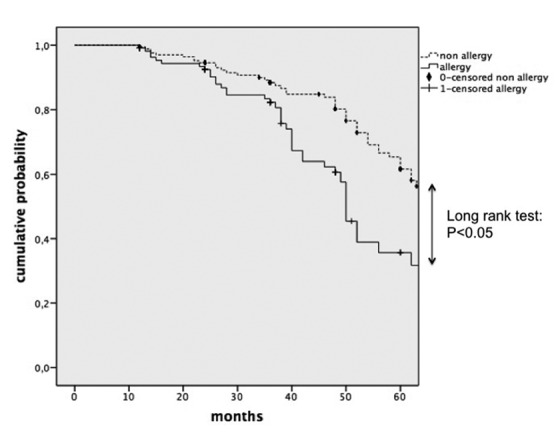
Estimation of relapse over time by Kaplan-Meier analysis in allergic patients (n = 114) and non-allergic patients (n = 191). The difference between curves was significant by log rank test.
Discussion
Reduction of the inferior turbinates can be performed using different surgical techniques including total or partial inferior turbinectomy (PIT), lateral outfracture, microdebrider submucosal resection, laser-assisted turbinate reduction, argon plasma surgery, cryosurgery, treatment with infrared light, vidian neurectomy, chemical or electrical coagulation and radiofrequency volume turbinate reduction (RFVTR) 12-14. The literature 12-15 provides considerable evidence for the efficacy of "hot surgery" in adults with symptomatic, inferior turbinate hypertrophy, with a significant increase in use of these techniques in the past decade. Important adverse effects of these techniques are likely the consequence of the heat generated by the power applied. Atrophic and metaplastic changes of mucosa, crusting and synechia may occur, and the incidence differs for the administered energy with various long-term results 16-21.
Several studies have shown 22-26 that RFVTR can be considered as a safe mini-invasive surgical procedure with only slight nasal mucosa damage, minor discomfort and a low risk of side effects. However, most published studies are observational and have a relatively short followup, while reports of long-term assessment of self reported benefits and patient satisfaction of treatment are insufficient. Porter et al. 27 in a small series showed that after two-years of follow-up there was no significant return of symptoms compared to evaluation at 6 months. Garzaro et al. 12 evaluated patients at 2 months and 2 years after the surgical procedure using the "Sniffin' Sticks" test battery and the NOSE scale. Long-term evaluation showed that radiofrequency treatment for allergic or non-allergic inferior turbinate hypertrophy appeared to provide improvement in olfaction, decrease in nasal resistance and had subjective benefits that were maintained at 2 years after the procedure. Cukurova et al. 10 demonstrated that most patients (82%) showed long-term (60 months) subjective and objective improvement after only one procedure. Safiruddin et al. 28 analysed the self-reported long-term effects of RFVTR treatment using a questionnaire sent to 441 patients who underwent RFA. They included a total of 142 patients. Subjective data retrieved through patient interviews showed a trend of beneficial effect of RFVTR on nasal breathing during daytime, with 60.7% of patients reporting long-term improvement after treatment.
Our data showed overall good satisfaction of patients with the procedure together with a good rate of pain control during surgery and a low rate of complications (1.3% bleeding). Post-operatively we observed (4 weeks after surgery) a significant improvement in nasal stuffiness, nasal obstruction and mouth breathing (Table IV, Fig. 1). We analysed the temporal trend of the benefit obtained with surgery and observed a worsening trend as shown in Figure 2. We also observed a mild worsening trend of global satisfaction of patients as shown in Figure 3. We followed patients over time for recurrence by the Kaplan Meyer method. At the early follow-up for at least 36 months the majority of patients maintained benefits achieved with surgery, and in this time period the cumulative probability to remain relapse free was up to 0.8 as shown in Table V. In the following years, we observed an increasing rate of recurrence with a decrease in cumulative relapse-free probability.
Taking into consideration the increasing prevalence of allergic rhinitis, its impact on individual quality of life and social costs, we investigated if allergy could be a discriminating factor in the impact of the intervention, and in particular on early exacerbations. Limited data are available in the literature on this topic because most published studies on RF turbinate surgery in patients with allergic rhinitis have a relatively short follow-up. Recently, some authors have suggested that urban residence and allergic rhinitis were significantly associated with lower long-term improvement after radiofrequency treatment 29. Furthermore, Linet al. 11 demonstrated that even though the outcome of RF turbinate reduction for patients with allergic rhinitis responding poorly to medical therapy decreases over time, it was still significant at 5 years after surgery. Herein, it was possible to stratify the analysis of recurrences by the presence of allergy, observing a worse temporal trend in allergic patients compared to non-allergic ones with a statistically significant difference (p < 0.05). Our data suggest that allergy affects results of surgery in terms of recurrence at long-term follow-up.
In conclusion, our data confirm that treatment of hyperplastic inferior nasal turbinates due to chronic allergic and nonallergic vasomotor rhinitis by minimally invasive nasal- RFA can be considered a safe procedure that alters nasal mucosa only slightly, while preserving physiologic function with minor discomfort and a low risk of side effects. In fact, the procedure is quick, easy, relatively painless and has the additional benefit of not requiring post-operative nasal packing, with satisfactory results. Furthermore, it appears to be a successful therapeutic option that offers very good results for at least 36 months. In the following 2 years, we observed a worse temporal trend in terms of recurrence rates, especially in allergic patients. Prediction of relapse after this procedure is a challenge for the future, and in particular to improve the success rate. In this regard, the severity and type of inflammation that causes turbinate hypertrophy is one of the factors that should be investigated. Several studies 30-35 have recently demonstrated that inflammation has a very important role in the pathogenesis of the swelling of nasal mucosa, not only in allergic rhinitis, but also in non-allergic rhinitis. Further studies should clarify whether the type and severity of inflammation correlate with the therapeutic success of this procedure.
References
- 1.Passàli D, Passàli FM, Damiani V, et al. Treatment of inferior turbinate hypertrophy: a randomized clinical trial. Ann Otol Rhinol Laryngol. 2003;112:683–688. doi: 10.1177/000348940311200806. [DOI] [PubMed] [Google Scholar]
- 2.Bhandarkar ND, Smith TL. Outcomes of surgery for inferior turbinate hypertrophy . Curr Opin Otolaryngol Head Neck Surg. 2010;18:49–53. doi: 10.1097/MOO.0b013e328334d974. [DOI] [PubMed] [Google Scholar]
- 3.Antunes MB, Gudis DA, Cohen NA. Epithelium, cilia and mucus: Their importance in chronic rhinosinusitis . Immunol Allergy Clin North Am. 2009;29:631–643. doi: 10.1016/j.iac.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 4.Chen XB, Lee HP, Chong VF, et al. Numerical simulation of thee ffects of inferior turbinate surgery on nasal airway heating capacity . Am J Rhinol Allergy. 2010;24:118–122. doi: 10.2500/ajra.2010.24.3511. [DOI] [PubMed] [Google Scholar]
- 5.Kojima Y, Tsuzuki K, Takebayashi H, et al. Therapeutic evaluation of outpatient submucosal inferior turbinate surgery for patients with severe allergic rhinitis . Allergol Int. 2013;62:479–485. doi: 10.2332/allergolint.12-OA-0533. [DOI] [PubMed] [Google Scholar]
- 6.Talmon Y, Samet A, Gilbey P. Total inferior turbinectomy: Operative results and technique . Ann Otol Rhinol Laryngol. 2000;109:1117–1119. doi: 10.1177/000348940010901206. [DOI] [PubMed] [Google Scholar]
- 7.Salzano FA, Mora R, Dellepiane M, et al. Radiofrequency, high-frequency, and electrocautery treatments vs partial inferior turbinotomy: microscopic and macroscopic effects on nasal mucosa . Arch Otolaryngol Head Neck Surg. 2009;135:752–758. doi: 10.1001/archoto.2009.87. [DOI] [PubMed] [Google Scholar]
- 8.Fokkens WJ, Lund VJ, Mullol J, et al. EPOS 2012: European position paper on rhinosinusitis and nasal polyps 2012. A summary for otorhinolaryngologists . Rhinology. 2012;50:1–12. doi: 10.4193/Rhino12.000. [DOI] [PubMed] [Google Scholar]
- 9.Kahveci OK, Miman MC, Yucel A, et al. The efficiency of Nose Obstruction Symptom Evaluation (NOSE) scale on patients with nasal septal deviation . Auris Nasus Larynx. 2012;39:275–279. doi: 10.1016/j.anl.2011.08.006. [DOI] [PubMed] [Google Scholar]
- 10.Cukurova I, Demirhan E, Cetinkaya EA, et al. Long-term clinical results of radiofrequency tissue volume reduction for inferior turbinate hypertrophy . J Laryngol Otol. 2011;125:1148–1151. doi: 10.1017/S0022215111001976. [DOI] [PubMed] [Google Scholar]
- 11.Lin HC, Lin PW, Friedman M, et al. Long-term results of radiofrequency turbinoplasty for allergic rhinitis refractory to medical therapy . Arch Otolaryngol Head Neck Surg. 2010;136:892–895. doi: 10.1001/archoto.2010.135. [DOI] [PubMed] [Google Scholar]
- 12.Garzaro M, Pezzoli M, Landolfo V, et al. Radiofrequency inferior turbinate reduction: long-term olfactory and functional outcomes . Otolaryngol Head Neck Surg. 2012;146:146–150. doi: 10.1177/0194599811423008. [DOI] [PubMed] [Google Scholar]
- 13.Garzaro M, Landolfo V, Pezzoli M, et al. Radiofrequency volume turbinate reduction versus partial turbinectomy: clinical and histological features . Am J Rhinol Allergy. 2012;26:321–325. doi: 10.2500/ajra.2012.26.3788. [DOI] [PubMed] [Google Scholar]
- 14.Chen YL, Tan CT, Huang HM. Long-term efficacy of microdebrider- assisted inferior turbinoplasty with lateralization for hypertrophic inferior turbinates in patients with perennial allergic rhinitis . Laryngoscope. 2008;118:1270–1274. doi: 10.1097/MLG.0b013e31816d728e. [DOI] [PubMed] [Google Scholar]
- 15.Willatt D. The evidence for reducing inferior turbinates . Rhinology. 2009;47:227–236. doi: 10.4193/Rhin09.017. [DOI] [PubMed] [Google Scholar]
- 16.Porter MW, Hales NW, Nease CJ, et al. Long-term results of inferior turbinate hypertrophy with radiofrequency treatment: a new standard of care? . Laryngoscope. 2006;116:554–557. doi: 10.1097/01.MLG.0000201986.82035.6F. [DOI] [PubMed] [Google Scholar]
- 17.Sroka R, Janda P, Killian T, et al. Comparison of long term results after Ho:YAG and diode laser treatment of hyperplastic inferior nasal turbinates . Lasers Surg Med. 2007;39:324–331. doi: 10.1002/lsm.20479. [DOI] [PubMed] [Google Scholar]
- 18.Gierek T, Jura-Szoltys E. Long-term results after argon plasma coagulation (APC) inferior turbinates reduction . Otolaryngol Pol. 2007;61:63–68. doi: 10.1016/S0030-6657(07)70385-2. [DOI] [PubMed] [Google Scholar]
- 19.Li KK, Powell NB, Riley RW, et al. Radiofrequency volumetric tissue reduction for treatment of turbinate hypertrophy: a pilot study . Otolaryngol Head Neck Surg. 1998;119:569–573. doi: 10.1016/S0194-5998(98)70013-0. [DOI] [PubMed] [Google Scholar]
- 20.Motta G, Salzano FA, Motta S. The treatment of allergic vasomotor rhinitis: diagnostic problems and local immunotherapy . Acta Otorhinolaryngol Ital. 1995;15(3 Suppl 48):1–24. [PubMed] [Google Scholar]
- 21.Gouveris H, Nousia C, Giatromanolaki A, et al. Immunohistological study of wound healing after submucosal radiofrequency tissue ablation of inferior nasal turbinate in a sheep model . Am J Rhinol Allergy. 2011;25:131–136. doi: 10.2500/ajra.2011.25.3576. [DOI] [PubMed] [Google Scholar]
- 22.Gindros G, Kantas I, Balatsouras DG, et al. Comparison of ultrasound turbinate reduction, radiofrequency tissue ablation and submucosal cauterization in inferior turbinate hypertrophy . Eur Arch Otorhinolaryngol. 2010;267:1727–1733. doi: 10.1007/s00405-010-1260-9. [DOI] [PubMed] [Google Scholar]
- 23.Bäck LJ, Hytönen ML, Malmberg HO, et al. Submucosal bipolar radiofrequency thermal ablation of inferior turbinates: a long-term follow-up with subjective and objective assessment . Laryngoscope. 2002;112:1806–1812. doi: 10.1097/00005537-200210000-00019. [DOI] [PubMed] [Google Scholar]
- 24.Hirunwiwatkul P, Udomchotphruet P. Efficacy study of nasal irrigation after radiofrequency tissue volume reduction for inferior turbinate hypertrophy: an equivalence randomized controlled trial . Am J Rhinol Allergy. 2012;26:497–503. doi: 10.2500/ajra.2012.26.3826. [DOI] [PubMed] [Google Scholar]
- 25.Brunworth J, Holmes J, Sindwani R. Inferior turbinate hypertrophy: review and graduated approach to surgical management . Am J Rhinol Allergy. 2013;27:411–415. doi: 10.2500/ajra.2013.27.3912. [DOI] [PubMed] [Google Scholar]
- 26.Manuele C, Giacomo C, Valeria F, et al. The potential role of hyaluronic acid in postoperative radiofrequency surgery for chronic inferior turbinate hypertrophy . Am J Rhinol Allergy. 2013;27:234–236. doi: 10.2500/ajra.2013.27.3869. [DOI] [PubMed] [Google Scholar]
- 27.Porter MW, Hales NW, Nease CJ, et al. Long-term results of inferior turbinate hypertrophy with radiofrequency treatment: a new standard of care? . Laryngoscope. 2006;116:554–557. doi: 10.1097/01.MLG.0000201986.82035.6F. [DOI] [PubMed] [Google Scholar]
- 28.Safiruddin F, Vroegop AV, Ravesloot MJ, et al. Long-term self-reported treatment effects and experience of radiofrequency- induced thermotherapy of the inferior turbinates performed under local anesthesia: a retrospective analysis. Eur Arch Otorhinolaryngol. 2013;270:1849–1853. doi: 10.1007/s00405-012-2302-2. [DOI] [PubMed] [Google Scholar]
- 29.Incandela C, Calamusa G, Massenti MF, et al. Long-term efficacy of radiofrequency treatment of turbinate hypertrophy: a patient based point of view . Indian J Otolaryngol Head Neck Surg. 2013;65(Suppl. 2):226–230. doi: 10.1007/s12070-011-0337-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Corso E, Battista M, Pandolfini M, et al. Role of inflammation in non-allergic rhinitis . Rhinology. 2014;52:142–149. doi: 10.4193/Rhino13.102. [DOI] [PubMed] [Google Scholar]
- 31.Passali GC1, Bellussi LM, Corso E, et al. The natural course of allergic rhinitis: a 32-year follow-up study. Acta Otolaryngol. 2013;133:1188–1195. doi: 10.3109/00016489.2013.815362. [DOI] [PubMed] [Google Scholar]
- 32.Corso E, Baroni S, Romitelli F, et al. Nasal lavage CCL24 levels correlate with eosinophils trafficking and symptoms in chronic sino-nasal eosinophilic inflammation . Rhinology. 2011;49:174–179. doi: 10.4193/Rhino10.133. [DOI] [PubMed] [Google Scholar]
- 33.Corso E, Baroni S, Battista M, et al. Nasal fluid release of eotaxin-3 and eotaxin-2 in persistent sinonasal eosinophilic inflammation . Int Forum Allergy Rhinol. 2014;4:617–624. doi: 10.1002/alr.21348. [DOI] [PubMed] [Google Scholar]
- 34.Passali D, Corso E, Platzgummer S, et al. Spa therapy of upper respiratory tract inflammations . Eur Arch Otorhinolaryngol. 2013;270:565–570. doi: 10.1007/s00405-012-2024-5. [DOI] [PubMed] [Google Scholar]
- 35.Corso E, Baroni S, Lucidi D, et al. Nasal lavage levels of granulocyte-macrophage colony-stimulating factor and chronic nasal hypereosinophilia . Int Forum Allergy Rhinol. 2015;5:557–562. doi: 10.1002/alr.21519. [DOI] [PubMed] [Google Scholar]


