Abstract
Introduction
Approximately 25.5 million pediatric patients are treated in Emergency Departments around the United States annually. Roughly 7% of these patients are transported by ambulance; of these, about 7% arrive in ambulances running red lights and sirens (RLS). Compared to those transporting without RLS, emergency vehicles employing RLS are involved in more accidents and are associated with more fatalities.
Objective
To characterize the use of RLS in pediatric transports and identify factors associated with unnecessary use of RLS.
Methods
As part of the Children’s Safety Initiative (CSI-EMS), a large, multi-phased National Institutes of Health-funded study, we conducted a medical record review of all pediatric RLS transports in an urban EMS system over a 4-year period (2008–2011). A standardized chart abstraction tool was adapted for the out-of-hospital setting and pilot tested. Charts were independently reviewed by physicians and paramedics, with disagreements arbitrated by a pediatric emergency physician. Reviewers were asked to judge whether RLS transport was necessary and to provide comments justifying their position. Descriptive statistics were used to measure the frequency of unnecessary transports and logistic regression analysis was employed to identify factors associated with unnecessary use of RLS.
Results
Of 490 RLS transports, experts identified 96 (19.6%) as unnecessary use of RLS. Necessary and unnecessary RLS transports had similar patient sex and duration of transport, though unnecessary use of RLS tended to increase with patient age. The call reasons that represented the largest proportion of unnecessary RLS transports were trauma (49.0%), respiratory distress (16.7%), and seizure/altered mental status (11.5%). Compared with necessary RLS transports, unnecessary RLS transports were less likely to require resuscitation, airway management, or medication administration. Univariate analysis revealed that patient vital signs within normal limits were associated with increased risk of unnecessary RLS transport, with the most pronounced effect seen in the normal GCS score group (odds ratio 7.74, p-value 0.001).
Conclusions
This analysis identified patient and transport characteristics associated with unnecessary use of RLS. Our results could help serve as the basis for designing and prospectively evaluating protocols for use of RLS, potentially mitigating the risk associated with transport in pediatric patients.
Introduction
About 25.5 million pediatric patients are treated in Emergency Departments around the United States every year (1). Approximately 7% of these patients are transported by ambulance; of these, about 7% arrive in ambulances running red lights and sirens (RLS), presumably those deemed to be the most ill and to require the most urgent care (2, 3). However, the ability of Emergency Medical Services (EMS) providers to accurately predict illness severity and need for admission is uncertain. Most existing data concern adult patients, with the sensitivity of paramedic prediction for hospital admission ranging from 61–81% (4–6). There is very limited information regarding EMS provider judgment in pediatric patients. One study examining pediatric trauma transports found a sensitivity of 50% for paramedic assessment of the need for trauma team activation, suggesting pediatric illness severity can be a difficult determination to make in the field (7).
Transporting patients with red lights and sirens carries significant risks. Compared to those transporting without RLS, emergency vehicles employing RLS are involved in more accidents, with more severe injuries, and more fatalities (8–10). A retrospective analysis of ambulance crashes over a 27-month period in San Francisco found injury rates of 1.5 per 100,000 runs without RLS compared to 22.2 per 100,000 with RLS (8). Data from the U.S. Department of Labor Bureau of Labor Statistics indicate that between 74% and 86% of EMS occupational fatalities are related to emergency vehicle transport (9, 11). Further, while several studies suggest that travel with RLS results in a modest reduction in transport time, it is not clear that this reduction is clinically significant (12–15). In the large majority of cases, patient outcomes appear to be similar for those transported with RLS and those without (14, 16). A large multicenter study published in 2010 examining 3656 trauma patients with unstable vital signs found no association between EMS activation, response, on-scene, transport or total time and patient mortality (17). In light of these considerations, several EMS agencies have instituted protocols designed to reduce the use of RLS (18–20). The majority, however, do not offer clearly articulated guidelines and depend solely on the discretion of the EMS provider.
While there is very little data pertaining to pediatric RLS transports generally, to our knowledge there is no literature concerning which factors influence caregivers’ determination of the necessity for RLS in pediatric patients. Previous studies have demonstrated that the most common reasons for all pediatric EMS transports are respiratory problems, neurologic symptoms, and traumatic injuries (2, 21, 22). However, many children with these clinical conditions do not require hospital admission; in particular, up to 90% of children brought in by ambulance with seizures are discharged home from the Emergency Department (3). Given this, the objective of this exploratory study is to identify patient and transport characteristics associated with unnecessary RLS transport, with the ultimate goal of identifying a subset of pediatric patients who are unlikely to benefit from that transport priority. We hypothesized that younger patients and those suffering from traumatic injuries or seizures would be more frequently transported with RLS unnecessarily.
Methods
Study design
The Children’s Safety Initiative Emergency Medical Services (CSI-EMS) is a large, multi-phased study funded by the National Institutes of Health (NICHD R01HD062478) designed to describe the epidemiology of preventable safety events in the out-of-hospital emergency care of children. As part of this project, we performed a retrospective observational study of all pediatric patients transported with RLS in an urban EMS system over a 4-year period (2008–2011). EMS charts were reviewed using a standardized chart abstraction tool adapted from the Harvard Medical Study “Retrospective Case Record Review” (23). The major domains analyzed for possible safety events included resuscitation, assessment, impression/diagnosis, clinical decision making, airway, fluids and medication, procedures, equipment, environment, and system. The adapted tool was revised through several rounds of pilot testing and administered using SurveyMonkey™.
The review panel was comprised of 13 paramedics and 7 physicians, all of whom underwent a 2-hour training session detailing use of the tool. Reviewers completed a test review case before and after the instructional session and received feedback on their application of the tool. A training manual addressing common questions was provided to each reviewer, and all reviewers received financial compensation per chart reviewed. Paramedics on the panel were not part of the agencies submitting charts, and physicians were emergency medicine, pediatric emergency medicine, or pediatric physicians working in tertiary care centers that provide online medical control.
Each chart was reviewed independently by a paramedic and a physician. All charts were also reviewed by one of two pediatric emergency physicians with experience in prehospital care, who arbitrated differences between the initial paramedic and physician reviewers (total of 3 reviews per chart). After the pediatric emergency physicians performed a review of their first 10 charts a kappa statistic was calculated for the presence of an error in the major domains of the review tool and was 0.615. All reviewers were blinded to agency, providers, patient, time frame, prior reviews, data analyses, and interim findings. The study was approved by the Institutional Review Board of Oregon Health & Science University (IRB00006942).
Study population and setting
We reviewed both fire and transport agencies’ medical records for all red lights and sirens transports in Multnomah County from 2008–2011 for patients less than 18 years of age. Multnomah County (population over 700,000) is a major urban area including the city of Portland, the largest city in Oregon. Private ambulance transports are staffed with advanced life support crews consisting of 2 paramedics, and fire units have 4–5 person crews with at least 1 paramedic in each unit. Both fire and transporting agencies respond to calls, though if not deemed necessary the fire crew may not provide care. Reviews included charts from the transporting agency, and when applicable, the fire response unit.
In the Multnomah county EMS system, priority of transport (i.e. whether to run RLS or not) is determined at the discretion of the transporting crew. Personnel are advised to use RLS in any patient with a ‘potential critical threat to life’; while this frequently applies to suspected cerebrovascular accidents, physiologic shock, ST-segment elevation myocardial infarction, and trauma system entries, there is no explicit rule, and what constitutes a ‘critical threat’ is left to the discretion of the transporting crew.
The pediatric experience of EMS personnel transporting patients in Multnomah county is naturally variable. At the time this study took place, the state of Oregon required 8 hours of “pediatric and obstetric” education per 2-year recertification cycle. The agencies included in this study additionally require paramedics to maintain PALS certification and all undergo pediatric airway training with patient simulators on an annual basis.
Variables and analysis
Within the chart review tool, each reviewer was asked to judge whether transport with RLS was necessary. No objective criteria were provided to reviewers with which to determine whether RLS was necessary; they were asked to simply make a subjective determination based on the information available in the chart. We collected data for both ‘Necessary RLS’ and ‘Unnecessary RLS’ transports including: patient characteristics (age, sex, vital signs, Glasgow coma scale score, EMS assessment) and transport characteristics (time of day, duration of transport, procedures performed, medications administered, and whether fire personnel remained on-scene and completed a chart). We used descriptive statistics to summarize patient characteristics and univariate analysis to identify characteristics associated with unnecessary RLS transport. The results of our univariate analysis were then used as predictors in a multivariable regression analysis, requiring a significance level of 0.3 to remain in the model. Odds ratios, confidence intervals, and p-values were calculated using logistic regression and both descriptive statistics and regression results were analyzed using SAS v9.4 (Cary, NC).
Results
From a total of 11,328 transports during the study period we identified 497 RLS transports (4.4% of all pediatric transports). We eliminated 2 cases due to missing data and 5 cases because a corresponding fire department chart was completed but could not be obtained. The final analysis therefore included 490 RLS transports. Patient characteristics are summarized in Table 1. Of note, a majority of all transported patients had initial heart rates, respiratory rates, and GCS scores in the normal range, while 67% had systolic blood pressures in the normal range (normal vital sign ranges were adjusted for patient age) (24).
Table 1.
Patient characteristics
| Patient Characteristics | RLS Necessary (%) [n=394] |
RLS Unnecessary (%) [n=96] |
% of Runs RLS Unnecessary |
|---|---|---|---|
| Age | |||
| Newborn, 0–28 days | 21 (5.3) | 2 (2.1) | 8.7% |
| Infant, 29 days-11 months | 56 (14.2) | 5 (5.2) | 8.2% |
| Toddler, 1–5 years | 138 (35.0) | 31 (32.3) | 18.3% |
| Kid, 6–11 years | 64 (16.2) | 20 (20.8) | 23.8% |
| Adolescent, 12–17 years | 115 (29.2) | 38 (39.6) | 24.8% |
| Sex | |||
| Female | 156 (39.6) | 39 (40.6) | 20.0% |
| Male | 237 (60.2) | 56 (58.3) | 19.1% |
| Initial VS in normal range (22) | |||
| HR*: | 197 (54.0) | 61 (67.0) | 23.6% |
| SBP*: | 133 (63.0) | 59 (77.6) | 30.7% |
| RR*: | 170 (49.0) | 57 (64.8) | 25.0% |
| GCS*: | 132 (50.4) | 55 (88.7) | 29.4% |
| Time of Transport | |||
| Morning: 0500–1059 | 65 (16.5) | 19 (19.8) | 22.6% |
| Afternoon: 1100–1659 | 144 (36.5) | 44 (45.8) | 23.4% |
| Evening: 1700–2259 | 134 (34.0) | 26 (27.1) | 16.3% |
| Overnight: 2300–0459 | 51 (12.9) | 7 (7.3) | 12.1% |
|
Transport Duration, mean mm:ss (sd) |
15:30 (8:29) | 16:29 (6:53) | |
| Fire Response-yes | 177 (44.9) | 28 (29.2) | 13.7% |
| Reason for Call | |||
| Cardiopulmonary Arrest | 35 (8.9) | 0 (0) | 0.0% |
| Trauma | 157 (39.9) | 47 (49.0) | 23.0% |
| Seizure or ALOC | 97 (24.6) | 11 (11.5) | 10.2% |
| Ingestion/Poisoning | 21 (5.3) | 8 (8.3) | 27.6% |
| Respiratory Distress | 63 (16.0) | 16 (16.7) | 20.3% |
| Allergic Reaction | 8 (2.0) | 4 (4.17) | 33.3% |
| Pain (non-trauma) | 6 (1.5) | 6 (6.3) | 50.0% |
| Other | 7 (1.78) | 4 (4.17) | 36..4% |
Due to missing data, percentages are calculated using cases with complete data
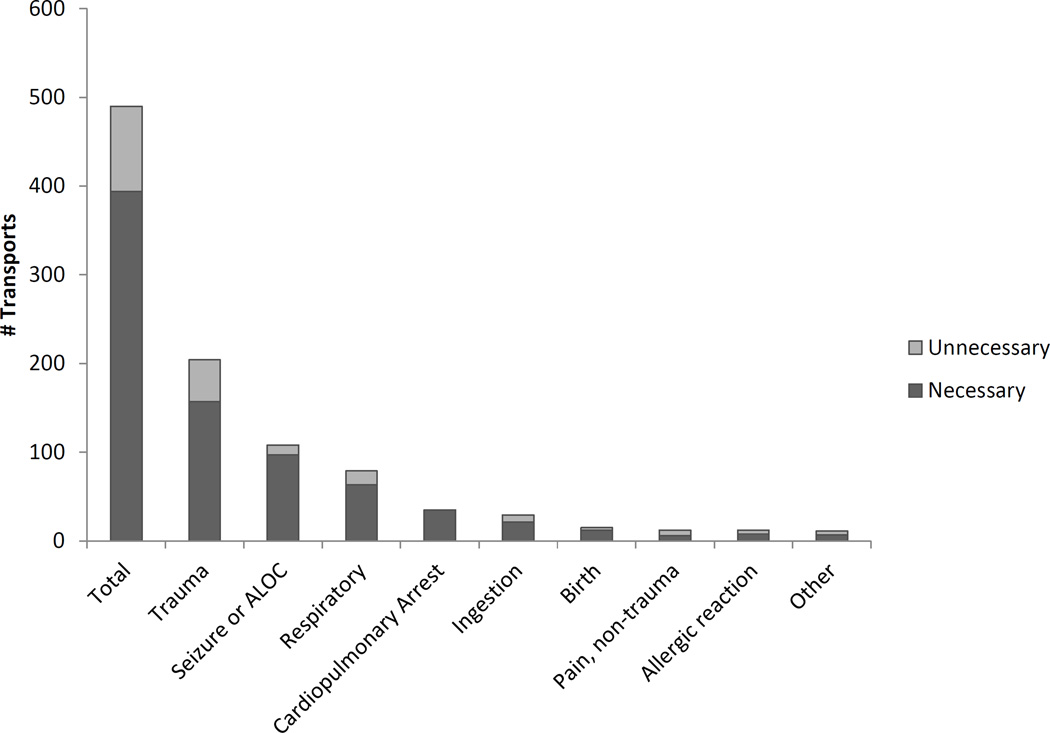
When evaluating unnecessary RLS transports, we found that roughly 1/5 of all RLS transports (19.6%) were determined to use RLS unnecessarily. When stratified by reason for transport, trauma, seizures or ALOC, and respiratory distress accounted for the majority (77.1%) of unnecessary RLS transports, with trauma accounting for almost 50% of the total. These data are represented in Figure 1.
Figure 1.
Proportion Unnecessary RLS by Reason for Transport
To better understand how reviewers determined whether use of RLS was necessary or unnecessary, we compared the characteristics of these two cohorts. Compared to cases in which RLS transport was felt to be necessary, those deemed unnecessary received fewer interventions (Table 2). Only 11.5% of patients transported unnecessarily required resuscitation, compared to 48.5% of those in whom RLS was deemed appropriate. Additionally, the large majority of resuscitation for these unnecessary transports came in the form of IV fluids, rather than cardiopulmonary resuscitation, cardioversion, airway interventions, or resuscitation medications. While over 30% of patients transported with RLS unnecessarily required airway management, only 2.1% of these patients required bag-valve-mask (BVM) ventilation and the remainder required only supplemental oxygen. This is in contrast to necessary RLS transports where 75% required airway intervention, with 19% requiring BVM ventilation and 12% needing advanced airway management including intubation. About 48% of necessary RLS transports received medications compared to 25% in the unnecessary RLS group. Amongst patients transported for seizures or ALOC, only 2 of 11 (18.2%) in the unnecessary RLS group received anti-seizure medications, while 67 of 96 (69.8%) in the necessary group were given medications to abort seizures. Lastly, procedures such as vascular access and cervical spine immobilization were more common in the group deemed to require RLS transport, while almost 30% of patients in the unnecessary RLS group received no intervention whatsoever.
Table 2.
Interventions according to transport type
| Intervention | Transport Priority | ||||
|---|---|---|---|---|---|
| RLS Appropriate | RLS Inappropriate | ||||
| n=394 | n=96 | ||||
| n | % | n | % | ||
| Any Resuscitation | 203 | 51.5 | 11 | 11.5 | |
| CPR | 40 | 10.2 | 0 | 0.0 | |
| IV fluids | 98 | 24.9 | 8 | 8.3 | |
| Cardioversion/Defibrillation | 3 | 0.8 | 0 | 0.0 | |
| Any Airway Management | 296 | 75.1 | 33 | 34.4 | |
| Oxygen | 270 | 68.5 | 32 | 33.3 | |
| BVM ventilation | 73 | 18.5 | 2 | 2.1 | |
| SGA or intubation | 46 | 11.8 | 0 | 0.0 | |
| Any Medication | 188 | 47.7 | 24 | 25.0 | |
| Sedative/Hypnotic | 14 | 3.6 | 0 | 0.0 | |
| Nausea | 24 | 6.1 | 8 | 8.3 | |
| Allergy/Anaphylaxis | 5 | 1.3 | 1 | 1.0 | |
| Antidote (e.g. naloxone) | 9 | 2.3 | 2 | 2.1 | |
| Anti-seizure | 67 | 17.0 | 2 | 2.1 | |
| Narcotic | 15 | 3.8 | 4 | 4.2 | |
| Respiratory | 40 | 10.2 | 8 | 8.3 | |
| RSI | 10 | 2.5 | 0 | 0.0 | |
| Cardiovascular | 31 | 7.9 | 0 | 0.0 | |
| Any Procedure | 301 | 76.4 | 49 | 51.0 | |
| Vascular access | 264 | 67.0 | 28 | 29.2 | |
| C-spine immobilization | 125 | 31.7 | 22 | 22.9 | |
We performed univariate logistic regression analysis to identify factors associated with unnecessary RLS transport. These results are included in Table 3. Notably, younger age was associated with decreased odds of unnecessary RLS transport. Initial vital signs within normal limits for age was associated with increased odds of unnecessary RLS transport, with the most pronounced effect seen in the normal GCS score group (odds ratio 7.74, p-value 0.001). A presenting complaint of seizures or altered level of consciousness was associated with reduced odds of unnecessary RLS transport, with an odds ratio of 0.38 (p-value 0.007). Utilizing these factors, we performed a multivariable regression analysis, summarized in Table 4. Cardiac arrest cases were excluded, as all cardiac arrest cases were determined to warrant use of RLS. In our final multivariable regression model, initial GCS score within normal limits remained a significant predictor of unnecessary use of RLS (OR 12.36, p-value 0.001).
Table 3.
Univariate analysis of factors associated with unnecessary RLS transport
| Patient Factors | OR (95% CI) | P-value | |
|---|---|---|---|
| Age Group (reference group: 12 – 17 years) | |||
| 0–28 days | 0.288 (0.065–1.287) | 0.1032 | |
| 29 days – 11 months | 0.27 (0.101–0.724) | 0.0093 | |
| 12 months – 5 years | 0.68 (0.398–1.161) | 0.1574 | |
| 6–11 years | 0.946 (0.508–1.761) | 0.8604 | |
| Sex (male reference) | 1.058 (0.671–1.669) | 0.8084 | |
| Initial Heart Rate w/in Normal Limits | 1.734 (1.07–2.811) | 0.0255 | |
| Initial Systolic BP w/in Normal Limits | 2.051 (1.117–3.766) | 0.0206 | |
| Initial Respiratory Rate w/in Normal Limits | 1.914 (1.178–3.111) | 0.0087 | |
| Initial GCS score w/in Normal Limits | 7.738 (3.398–17.621) | <.0001 | |
| Call Reason (Trauma reference) | |||
| Cardiopulmonary Arrest | <0.001 (<0.001– >∞) | 0.9605 | |
| Seizure or ALOC | 0.379 (0.187–0.766) | 0.0068 | |
| Ingestion/Poisoning | 1.273 (0.529–3.059) | 0.5902 | |
| Respiratory Distress | 0.848 (0.448–1.606) | 0.6135 | |
| Allergic Reaction | 1.67 (0.482–5.793) | 0.4189 | |
| Pain (non-trauma) | 3.34 (1.029–10.845) | 0.0447 | |
| Night (day reference) | 0.773 (0.429–1.394) | 0.3919 | |
| Fire chart (no fire chart reference) | 1.981 (1.222–3.21) | 0.0055 | |
| Transport time (1 minute increase) | 1.015 (0.988–1.043) | 0.2735 | |
Table 4.
Multivariable analysis of factors associated with unnecessary RLS transport
| Patient Factor | OR (95% CI) | P-value | |
|---|---|---|---|
| Call Reason (reference trauma) | |||
| Seizure or ALOC | 2.053 (0.443–9.508) | 0.3579 | |
| Ingestion/Poisoning | 1.896 (0.47 – 7.653) | 0.3691 | |
| Respiratory Distress | 2.593 (0.86–7.813) | 0.0905 | |
| Allergic Reaction | 16.384 (0.727 – 369.435) | 0.0786 | |
| Pain (non-trauma) | 3.809 (0.56–25.929) | 0.1718 | |
| Initial Systolic Blood Pressure w/in Normal Limits (reference initial sbp outside normal limits) |
1.92 (0.8–4.606) | 0.1439 | |
| Initial GCS Score w/in Normal Limits (reference initial gcs outside normal limits) |
12.36 (2.734–55.874) | 0.0011 | |
| Night (reference day) | 0.448 (0.166–1.211) | 0.1136 | |
Discussion
There are very few studies examining the use of RLS in pediatric transports, and ours is the first to identify factors employed by providers to distinguish necessary from unnecessary RLS use in pediatric patients. We found that approximately 20% of all RLS transports were judged to be unnecessary and that normal vital signs and normal GCS score were significantly associated with unnecessary use of red lights and sirens in our univariate analysis. We also found that patients in whom RLS transport was deemed unnecessary were much less likely to receive interventions of any kind, including resuscitation, airway management, medication, or procedural intervention.
When considering patients according to reason for transport, trauma represented the largest total number of unnecessary RLS transports. This is consistent with the existing epidemiologic literature on pediatric out-of-hospital care, with several large studies demonstrating over 40% of all pediatric EMS transports were due to trauma (2, 21, 22, 25–27). Seizures and ALOC, frequent reasons for RLS transport, had relatively low rates of unnecessary RLS use and were associated with reduced odds of unnecessary RLS (OR 0.40, p-value 0.008). This was an unexpected finding, in light of existing literature suggesting that up to 90% of children brought in by ambulance with seizures are discharged home from the Emergency Department (3). We did find that roughly 70% of patients in whom RLS was judged necessary received anti-seizure medications, compared with only 18% of patients in whom RLS was deemed unnecessary. This suggests that reviewers generally favored RLS transport for those who required abortive therapy for seizure control. While this approach is reasonable, it is generally accepted that seizures of short duration are benign. Furthermore, most children with first time seizures will cease seizing spontaneously, and the majority of patients who do require abortive medications will stop seizing after the first agent is administered (28–30). In our sample, only 24.3% of patients required more than one dose of benzodiazepine to abort the seizure. These considerations suggest a subset of these patients may have been transported safely without the use of RLS, even amongst those for whom RLS was deemed necessary by the reviewers in our study. Identifying which patients these are, however, remains a challenge and, given the risks of prolonged seizures and the potential for respiratory depression associated with treatment, clearly articulated guidelines for RLS use in these patients are essential.
The association between younger age and decreased risk for unnecessary RLS transport was unexpected. We hypothesized that providers would be less comfortable with the youngest pediatric patients and therefore more inclined to utilize RLS. However, closer examination of the data revealed that the reason for transport was not evenly distributed across groups. Compared to ages 6–18, cardiopulmonary arrest was more common in patients under 5 years (n of 6 and 29, respectively), as was seizure or ALOC (n of 42 and 65, respectively). This is in accordance with published data regarding pediatric EMS use, which consistently report that younger children are at higher risk for life-threatening reasons for transport (25, 26). Thus, the data suggests that younger patients are at lower risk for unnecessary RLS transport because they more frequently suffer from more severe medical conditions.
Given the risks of RLS transport and lack of clear benefit, it may be prudent to use a more systematic approach to the application of red lights and sirens. The American College of Emergency Physicians EMS committee adopted this position in a 2013 special report, wherein they advised that “the use of warning lights and sirens should be based on standardized protocols that take into account situational and patient problem assessments” (14). The results of our analysis may assist in the formulation of such guidelines. In pediatric trauma, for example, the major cause of morbidity and mortality is head injury (32, 33). This underscores the value of GCS score in the assessment of the pediatric trauma patient. Indeed, in our analysis, normal GCS was the factor most highly associated with unnecessary RLS transport. Thus, it may serve as a key criterion in deciding whether RLS are indicated for a given pediatric trauma patient. Similarly, for patients suffering from seizures, use of RLS may be predicated on a few key factors, such as whether the patient has compromised oxygenation or ventilation requiring positive pressure ventilation or has persistent seizures despite administration of a first dose of anti-seizure medication by EMS. Such an algorithm acknowledges the real potential for complications associated with prolonged seizures while encouraging judicious use of RLS. Additional algorithms incorporating patient and call characteristics could be elaborated for other common reasons for transport, such as respiratory distress. Such algorithms would need to be evaluated prospectively to monitor rates of RLS use and to ensure good patient outcomes.
Utilization of RLS in prehospital transport is a challenging issue, and the determination of when it is ‘necessary’ is difficult to operationalize. The line that EMS personnel must walk is a thin one, balancing the potential benefits of expedited transport against the risks inherent with RLS. In many systems, including the EMS system examined in this analysis, priority of transport is determined wholly at the discretion of the treating paramedics. While it is critical to retain a role for the judgement of the on-scene providers, given the potential complexity of the out-of-hospital environment, it is also important to recognize that general guidelines can simplify cognitively complex decisions. A small number of RLS transport algorithms based on common reasons for transport may serve to provide a rational foundation from which EMS providers may make their transport priority decisions. Deviations from such guidelines would certainly occur, but some standardization of this process would promote optimal safety practices.
Our study has a few notable strengths. First, it represents one of only a few efforts to identify pediatric patients transported with RLS in whom this method of transport was unnecessary—the last study investigating this topic was published in 1997, almost 20 years ago (22). Whereas the authors of that study considered as ‘inappropriate’ use of RLS in a ‘stable patient’, which they had defined a priori, another strength of our study is that we utilized the discretion of three blinded reviewers to operationalize necessary versus unnecessary use of RLS transport. We then performed post-hoc analysis of factors associated with unnecessary use of RLS. We feel this is the most suitable approach to identify the conditions that define ‘unnecessary’ use of RLS, given that there is no current gold standard for when use of RLS is appropriate in pediatric patients. Very likely, any reference standard for appropriateness of RLS transport will emerge from a consensus definition formulated by a panel of content experts; our results provide some groundwork for what such a definition might look like.
Our study has several limitations. Fundamentally, this study compares the judgment of the paramedics caring for the patient at the scene with the opinion of multiple providers reviewing chart data retrospectively and is subject to the limitations inherent in retrospective medical record reviews. It is possible that some factors not captured by the chart compelled EMS providers to transport the patient with RLS, and it is possible that more critically ill patients had less robust documentation, limiting the value of retrospective chart review. Another limitation is that we did not have associated ED or hospital data; it is feasible that a patient in whom RLS transport was deemed unnecessary in fact required significant intervention in the ED and beyond, suggesting that the patient was sicker than chart review may have indicated. A prospective study would better capture this data regarding patient dispositions. Lastly, this was a single EMS system in an urban area with several paramedics on scene for every call. Thus, these results may not be generalizable to other EMS systems where staffing is less robust or where customs for RLS transport differ.
In conclusion, this exploratory study describes pediatric patients who may have been transported with RLS unnecessarily and identifies factors employed by medical providers to distinguish necessary from unnecessary RLS use. The results of this study may help EMS researchers to more closely evaluate the conditions that influence transport priority determination. Ultimately, we hope such research will aid EMS leaders in developing policies and protocols to reduce unnecessary RLS transports in order to maximally safeguard the health of patients, EMS providers, and the public.
Contributor Information
Dr. Beech Burns, Email: burnsb@ohsu.edu, Oregon Health and Science University, Emergency Medicine, 3181 SW Sam Jackson Park Rd, Portland, 97239 United States, 3644 NE 20th Ave, Portland, 97212 United States.
Dr. Matthew L Hansen, Oregon Health & Science University, Emergency Medicine , CDW-EM 3181 SW Sam Jackson Pk. Road, CDW-EM 3181 SW Sam Jackson Pk. Road, Portland, 97239 United States.
Dr. Stacy Valenzuela, Oregon Health & Science University, Emergency Medicine , CDW-EM 3181 SW Sam Jackson Pk. Road, CDW-EM 3181 SW Sam Jackson Pk. Road, Portland, 97239 United States
Ms. Caitlin Summers, Oregon Health and Science University, Portland, United States
Mr. Joshua Van Otterloo, Oregon Health & Science University, Obstetrics & Gynecology, Portland, United States
Ms. Barbara Skarica, Oregon Health and Science University, Obstetrics and Gynecology, 3181 SW Sam Jackson Park Rd, Portland, 97239 United States
Dr. Craig Warden, Oregon Health & Science University, Emergency Medicine , CDW-EM 3181 SW Sam Jackson Pk. Road, CDW-EM 3181 SW Sam Jackson Pk. Road, Portland, 97239 United States, and Oregon Health & Science University, Portland, United States
Dr. Jeanne-Marie Guise, Oregon Health & Science University, Emergency Medicine , CDW-EM 3181 SW Sam Jackson Pk. Road, CDW-EM 3181 SW Sam Jackson Pk. Road, Portland, 97239 United States, and Oregon Health & Science University, Obstetrics & Gynecology, Portland, United States
References
- 1.Wier (Truven Health Analytics) LM, Hao (RAND) Y, Owens (AHRQ) P, Washington (AHRQ) R. Overview of Children in the Emergency Department, 2010. HCUP Statistical Brief #157. Rockville, MD: Agency for Healthcare Research and Quality; 2013. Jun, [Accessed March 7th, 2013]. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb157.pdf. [PubMed] [Google Scholar]
- 2.Shah MN, Cushman JT, Davis CO, Bazarian JJ, Auinger P, Friedman B. The Epidemiology of Emergency Medical Services Use by Children: An Analysis of the National Hospital Ambulatory Medical Care Survey. Prehospital Emergency Care. 2008;12(3):269–276. doi: 10.1080/10903120802100167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Richard J, Osmond MH, Nesbitt L, Stiell IG. Management and outcomes of pediatric patients transported by emergency medical services in a Canadian prehospital system. Canadian Journal of Emergency Medical Care. 2006 Jan;8(1):6–12. doi: 10.1017/s1481803500013312. [DOI] [PubMed] [Google Scholar]
- 4.Levine SD, Colwell CB, Pons PT, Gravitz C, Haukoos JS, McVaney KE. How well do paramedics predict admission to the hospital? A prospective study. Journal of Emergency Medicine. 2006;31(1):1–5. doi: 10.1016/j.jemermed.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 5.Cummins NM, Dixon M, Garavan C, Landymore E, Mulligan N, O’Donnell C. Can advanced paramedics in the field diagnose patients and predict hospital admission? Emergency Medicine Journal. 2013;30(12):1043–1047. doi: 10.1136/emermed-2012-201899. [DOI] [PubMed] [Google Scholar]
- 6.Richards JR, Ferral SJ. Triage Ability of Emergency Medical Services Providers and Patient Disposition: A Prospective Study. Prehospital and Disaster Medicine. 1999;14:174–179. [PubMed] [Google Scholar]
- 7.Qazi K, Kempf JA, Christopher NC, Gerson LW. Paramedic judgment of the need for trauma team activation for pediatric patients. Academic Emergency Medicine. 1998;5(10):1002–1007. doi: 10.1111/j.1553-2712.1998.tb02780.x. [DOI] [PubMed] [Google Scholar]
- 8.Saunders CE, Heye CJ. Ambulance collisions in an urban environment. Prehospital and Disaster Medicine. 1994;9(2):118–124. doi: 10.1017/s1049023x00041017. [DOI] [PubMed] [Google Scholar]
- 9.Maguire BJ, Hunting KL, Smith GS, Levick NR. Occupational fatalities in emergency medical services: a hidden crisis. Annals of Emergency Medicine. 2002;40(6):625–632. doi: 10.1067/mem.2002.128681. [DOI] [PubMed] [Google Scholar]
- 10.Custalow CB, Gravitz CS. Emergency medical vehicle collisions and potential for preventive intervention. Prehospital Emergency Care. 2004;8(2):175–184. doi: 10.1016/s1090-3127(03)00279-x. [DOI] [PubMed] [Google Scholar]
- 11.Maguire BJ, Smith S. Injuries and Fatalities among Emergency Medical Technicians and Paramedics in the United States. Prehospital and Disaster Medicine. 2013;28(4):376–382. doi: 10.1017/S1049023X13003555. [DOI] [PubMed] [Google Scholar]
- 12.Hunt RC, Brown LH, Cabinum ES, Whitley TW, Prasad NH, Owens CF, Jr, Mayo CE., Jr Is ambulance transport time with lights and siren faster than that without? Annals of Emergency Medicine. 1995;25(4):507–511. doi: 10.1016/s0196-0644(95)70267-9. [DOI] [PubMed] [Google Scholar]
- 13.Ho J, Casey B. Time saved with use of emergency warming lights and sirens during response to requests for emergency medical aid in an urban environment. Annals of Emergency Medicine. 1998;32(5):585–588. doi: 10.1016/s0196-0644(98)70037-x. [DOI] [PubMed] [Google Scholar]
- 14.Becker TK, Gausche-Hill M, Aswegan AL, Baker EF, Bookman KJ, Bradley RN, De Lorenzo RA, Schoenwetter DJ American College of Emergency Physicians EMS Committee. Ethical challenges in Emergency Medical Services: controversies and recommendations. Prehospital and Disaster Medicine. 2013;28(5):488–497. doi: 10.1017/S1049023X13008728. [DOI] [PubMed] [Google Scholar]
- 15.Fleischman RJ, Lundquist M, Jui J, Newgard CD, Warden C. Predicting ambulance time of arrival to the emergency department using global positioning system and Google maps. Prehospital Emergency Care. 2013;17(4):458–465. doi: 10.3109/10903127.2013.811562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marques-Baptista A, Ohman-Strickland P, Baldino KT, Prasto M, Merlin MA. Utilization of warning lights and siren based on hospital time-critical interventions. Prehospital and Disaster Medicine. 2010;25(4):335–339. doi: 10.1017/s1049023x0000830x. [DOI] [PubMed] [Google Scholar]
- 17.Newgard CD, Schmicker RH, Hedges JR, Trickett JP, Davis DP, Bulger EM, Aufderheide TP, Minei JP, Hata JS, Gubler KD, Brown TB, Yelle JD, Bardarson B, Nichol G Resuscitation Outcomes Consortium Investigators. Emergency medical services intervals and survival in trauma: assessment of the “golden hour” in a North American prospective cohort. Annals of Emergency Medicine. 2010;55(3):235–246. doi: 10.1016/j.annemergmed.2009.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Isenberg D, Cone DC, Stiell IG. A simple three-step dispatch rule may reduce lights and sirens responses to motor vehicle crashes. Emergency Medicine Journal. 2012;29(7):592–595. doi: 10.1136/emermed-2011-200133. [DOI] [PubMed] [Google Scholar]
- 19.Merlin MA, Baldino KT, Lehrfeld DP, Linger M, Lustiger E, Cascio A, Ohman-Strickland P, Dossantos F. Use of a limited lights and siren protocol in the prehospital setting vs standard usage. American Journal of Emergency Medicine. 2012;30(4):519–525. doi: 10.1016/j.ajem.2011.01.014. [DOI] [PubMed] [Google Scholar]
- 20.Olson GM. [Accessed March 7th, 2013];Enhancing safety during emergency medical responses. 2008 http://www.usfa.fema.gov/pdf/efop/efo41949.pdf.
- 21.Miller MK, Denise-Dowd M, Gratton MC, Cai J, Simon SD. Pediatric Out-of-hospital Emergency Medical Services Utilization in Kansas City, Missouri. Academic Emergency Medicine. 2009;16(6):526–531. doi: 10.1111/j.1553-2712.2009.00418.x. [DOI] [PubMed] [Google Scholar]
- 22.Lacher ME, Bausher JC. Lights and Siren in Pediatric 911 Ambulance Transports: Are They Being Misused? Annals of Emergency Medicine. 1997;29:223–227. doi: 10.1016/s0196-0644(97)70272-5. [DOI] [PubMed] [Google Scholar]
- 23.Brennan TA, Leape LL, Laird NM, Hebert L, Localio AR, Lawthers AG, Newhouse JP, Weiler PC, Hiatt HH. Incidence of adverse events and negligence in hospitalized patients: results of Harvard Medical Practice Study I. N Engl J M. 1991;324:370–376. doi: 10.1056/NEJM199102073240604. [DOI] [PubMed] [Google Scholar]
- 24.Pediatrics Fuchs S. In: Emergency Medical Services: Clinical Practice and Systems Oversight. Cone DC, O’Conner RE, Fowler R, editors. Vol. 1. National Association of EMS Physicians; 2009. p. 439. [Google Scholar]
- 25.Tsai A, Kallsen G. Epidemiology of pediatric prehospital care. Annals of Emergency Medicine. 1987;16:284–292. doi: 10.1016/s0196-0644(87)80173-7. [DOI] [PubMed] [Google Scholar]
- 26.Seidel JS, Henderson DP, Ward P, Wayland BW, Ness B. Pediatric prehospital care in urban and rural areas. Pediatrics. 1991;88:681–690. [PubMed] [Google Scholar]
- 27.Joyce SM, Brown DE, Nelson EA. Epidemiology of pediatric EMS practice: a multistate analysis. Prehospital and Disaster Medicine. 1996;11:180–187. doi: 10.1017/s1049023x00042928. [DOI] [PubMed] [Google Scholar]
- 28.Shinnar S, Berg AT, Moshe SL, Shinnar R. How long do new-onset seizures in children last? Annals of Neurology. 2001;49:659–664. [PubMed] [Google Scholar]
- 29.Warden CR, Frederick C. Midazolam and diazepam for pediatric seizures in the prehospital setting. Prehospital Emergency Care. 2006;10:463–467. doi: 10.1080/10903120600885126. [DOI] [PubMed] [Google Scholar]
- 30.Appleton R, Sweeney A, Choonara I, Robson J, Molyneux E. Lorazepam versus diazepam in the acute treatment of epileptic seizures and status epilepticus. Developmental Medicine and Child Neurology. 1995;37:682–688. doi: 10.1111/j.1469-8749.1995.tb15014.x. [DOI] [PubMed] [Google Scholar]
- 31.Kahn CA, Pirrallo RG, Kuhn EM. Characteristics of fatal ambulance crashes in the United States: an 11-year retrospective analysis. Prehospital Emergency Care. 2001;5:261–269. doi: 10.1080/10903120190939751. [DOI] [PubMed] [Google Scholar]
- 32.Tepas J, 3rd, DiScala C, Ramenofsky ML, Barlow B. Mortality and head injury: the pediatric perspective. Journal of Pediatric Surgery. 1990;25:92–96. doi: 10.1016/s0022-3468(05)80170-8. [DOI] [PubMed] [Google Scholar]
- 33.Cantais E, Paut O, Giorgi R, Viard L, Camboulives J. Evaluating the prognosis of multiple, severely traumatized children in the intensive care unit. Intensive Care Medicine. 2001;27:1511–1517. doi: 10.1007/s001340101039. [DOI] [PubMed] [Google Scholar]