Wide awake flexor tendon repair means no tourniquet and no sedation tendon repair under pure local lidocaine and epinephrine finger and hand anesthesia.
The 5 main advantages of doing the repair this way in the unsedated patient are as follows: (1) fewer postoperative ruptures happen because intraoperative testing of the tendon repair reveals gaps in 7% of cases that are repaired before skin closure.1 (2) These repairs get less tenolysis because intraoperative testing of the repair guides the surgeon to vent pulleys that impede full flexion or extension of the finger.2 (3) Surgeons educate the lucid patient during the surgery, so he understands how to avoid rupture and getting stuck.3 (4) Intraoperative flexor tendon repair testing guides the surgeon in the decision to maintain a superficialis repair or resect a superficialis slip.4 (5) Seeing full active flexion and extension with no gap during the surgery empowers the surgeon to allow up to half a fist of true active postoperative flexion (not place and hold) 3 to 5 days after surgery.5
LOCAL ANESTHESIA
Inject lidocaine with epinephrine (buffered 10:1 with 8.4% bicarbonate) everywhere you plan to dissect. Inject slowly from proximal to distal to decrease injection pain (See Video 1, Supplemental Digital Content 1, which displays a preoperative patient and local anesthetic injection. This video is available in the “Related Videos” section of the full-text article on PRSGlobalOpen.com or at http://links.lww.com/PRSGO/A212). Wait 30 minutes or more after the last injection to give time for maximal epinephrine vasoconstriction in the finger.
Video Graphic 1.
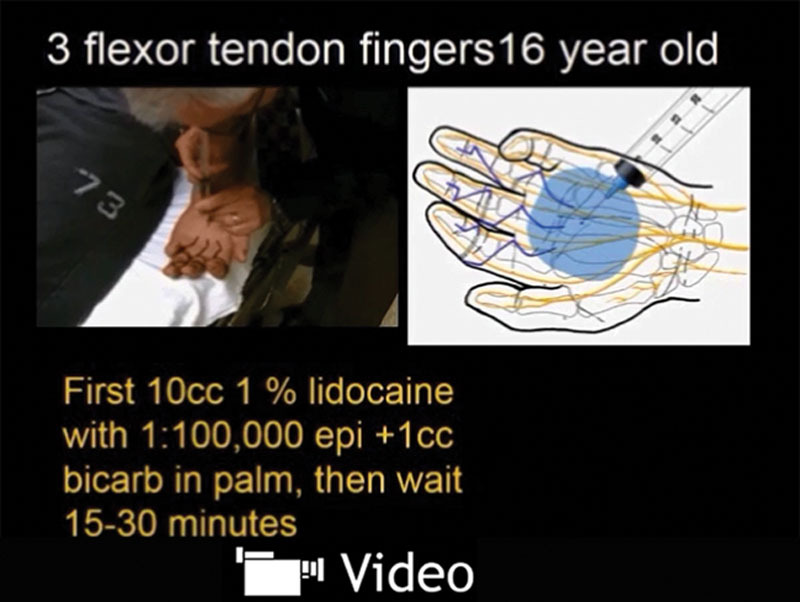
Preoperative patient and local anesthetic injection. See video, Supplemental Digital Content 1, which shows details of how to inject local anesthesia for wide awake flexor tendon repair. This video is available in the “Related Videos” section of the full-text article on PRSGlobalOpen.com or at http://links.lww.com/PRSGO/A212.
OPERATIVE TIPS
See Videos 2 to 4, Supplemental Digital Content 2, which demonstrates dissecting the skin flaps and exposing the sheath. This video is available in the “Related Videos” section of the full-text article on PRSGlobalOpen.com or at http://links.lww.com/PRSGO/A213). See video, Supplemental Digital Content 3, which demonstrates how to retrieve tendon ends. This video is available in the “Related Videos” section of the full-text article on PRSGlobalOpen.com or at http://links.lww.com/PRSGO/A214). See video, Supplemental Digital Content 4, which demonstrates how to suture the tendon and intraoperative patient education. This video is available in the “Related Videos” section of the full-text article on PRSGlobalOpen.com or at http://links.lww.com/PRSGO/A215).
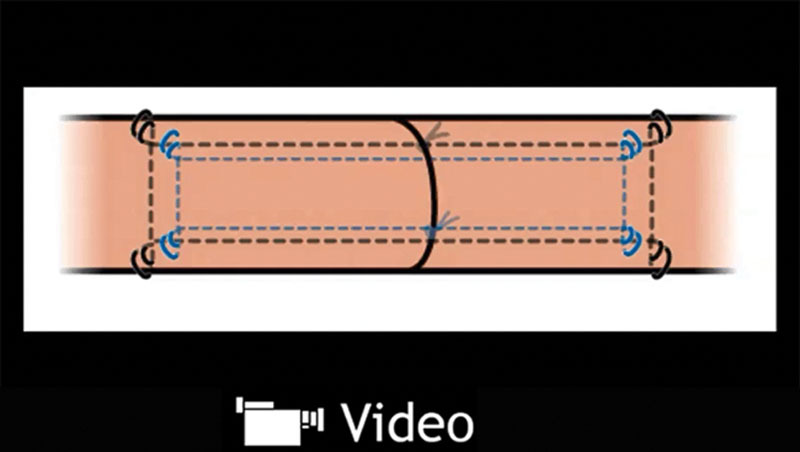
Video Graphic 2.

Dissecting the skin flaps and exposing the sheath. See video, Supplemental Digital Content 2, which shows the dissection of skin flaps and exposure of the sheath of the patient introduced in Video 1. This video is available in the “Related Videos” section of the full-text article on PRSGlobalOpen.com or at http://links.lww.com/PRSGO/A213.
Video Graphic 4.
Suture the tendon and intraoperative patient education. See video, Supplemental Digital Content 4, which observes the step by step suturing of the tendon through sheathotomies, venting of the A4 pulley, intraoperative testing of the repair, and patient education during the surgery. This video is available in the “Related Videos” section of the full-text article on PRSGlobalOpen.com or at http://links.lww.com/PRSGO/A215.
Repeatedly, test full active patient flexion and extension of the finger after each core and epitenon suture to make sure that there is no gap and that the repair fits through the pulleys. Repair any gaps and vent pulleys as required to get a full range of motion before skin closure. This is like testing blood flow in a vascular anastomosis to ensure function before skin closure.
Have the patients extend the finger if you feel them pull against you as you retrieve the tendon. Extension generates reflex relaxation of flexor muscles.
You do not need cautery. Bleeding stops by the time you sew back the skin flaps to expose the sheath.
Surgeons can repair tendons in minor procedure rooms outside the main operating room in daytime hours.
Involve hand therapists in patient teaching during surgery.
POSTOPERATIVE THERAPY
See Video 5, Supplemental Digital Content 5, which displays post operative therapy. This video is available in the “Related Videos” section of the full-text article on PRSGlobalOpen.com or at http://links.lww.com/PRSGO/A216.
Video Graphic 5.

Postoperative therapy. See video, Supplemental Digital Content 5, which displays the postoperative therapy, demonstrating early protected true active flexion and extension (as opposed to place and hold) and final result with patient of Videos 1 and 2. This video is available in the “Related Videos” section of the full-text article on PRSGlobalOpen.com or at http://links.lww.com/PRSGO/A216.
Video Graphic 3.
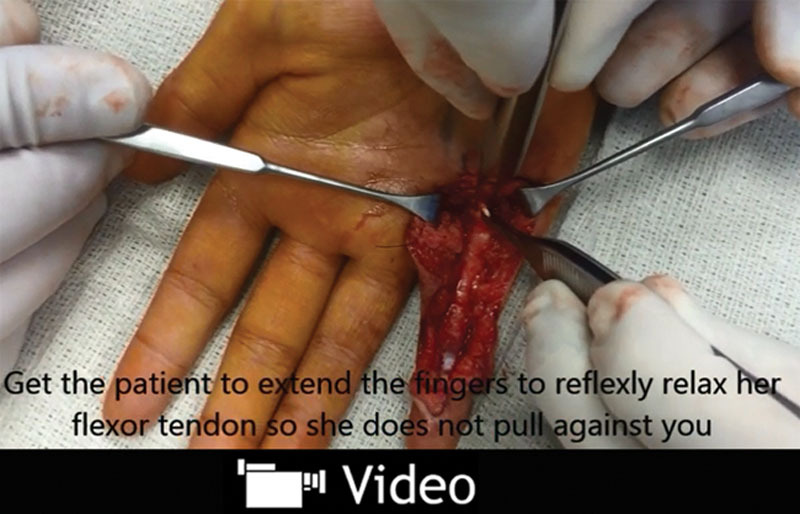
Retrieving the tendon ends. See video, Supplemental Digital Content 3, which demonstrates how the surgeon gets the patient to extend the finger to relax the flexor tendon and let it come distally in the sheath by pushing it with Adson forceps through sheathotomies. This video is available in the “Related Videos” section of the full-text article on PRSGlobalOpen.com or at http://links.lww.com/PRSGO/A214.
Immobilize and elevate the hand until swelling, friction, and work of flexion is gone (3–5 days).
Initiate up to half a fist of true active movement (not place and hold).
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge for this article was waived at the discretion of the Editor-in-Chief.
REFERENCES
- 1.Higgins A, Lalonde DH, Bell M, et al. Avoiding flexor tendon repair rupture with intraoperative total active movement examination. Plast Reconstr Surg. 2010;126:941–945. doi: 10.1097/PRS.0b013e3181e60489. [DOI] [PubMed] [Google Scholar]
- 2.Lalonde DH, Kozin S. Tendon disorders of the hand. Plast Reconstr Surg. 2011;128:1e–14e. doi: 10.1097/PRS.0b013e3182174593. [DOI] [PubMed] [Google Scholar]
- 3.Lalonde DH. How the wide awake approach is changing hand surgery and hand therapy: inaugural AAHS sponsored lecture at the ASHT meeting, San Diego, 2012. J Hand Therapy. 2013;26:175–178. doi: 10.1016/j.jht.2012.12.002. [DOI] [PubMed] [Google Scholar]
- 4.Lalonde DH. Wide Awake Hand Surgery. CRC Press; 2016. Finger flexor tendon repair. [Google Scholar]
- 5.Lalonde DH. Wide awake flexor tendon Repair and early mobilization in zones 1 and 2. In: Bo Tang J, Lee SK, editors. In: Hand Clinics Tendon Repair and Reconstruction. Elsevier Ltd; 2013. [DOI] [PubMed] [Google Scholar]


