Abstract
Background:
For the noncolonized wound, achieving tension-free, primary wound closure is ideal. Some surgeons advocate imbrication of deeper tissues rather than undermining, posing that imbrication preserves more dermal perfusion while still reducing tension at the wound edge. We sought to determine which technique most reliably reduced wound tension while preserving dermal wound perfusion.
Methods:
A total of 5 standardized, symmetrical pairs of full thickness wounds were created on Duroc swine. Wound tension was measured with a Tyrolean tensiometer before and after either method of closure, whereas a speckle contrast imager was used to assess dermal edge perfusion. Skin tension and dermal perfusion were evaluated for statistical significance via paired t tests and a multivariate analysis of variance.
Results:
There was a significant reduction in wound tension with undermining and imbrication relative to the raw wound tension (5 and 5.9 vs 7.1 N; P < 0.05) yet no significant difference between methods of closure (P > 0.05). There was a significant reduction in dermal perfusion between unwounded skin and the imbricated wound (222 perfusion units [PU] vs 48 PU; P < 0.05) and between the unwounded skin and the undermined wound (205 vs 63 PU; P < 0.05).
Conclusions:
We found no significant difference in wound tension between wound undermining or imbrication and a significant decrease in dermal perfusion after imbrication and undermining although the relative decrease in perfusion was greater with imbrication. Wound undermining reduces skin tension with greater relative dermal perfusion to the skin and should be selected over wound imbrication in standard primary wound closure.
“Accept that tension is the #1 enemy, but on occasion it can be maneuvered to act as a temporary friend” was quoted by Dr. Millard.1 Two commonly used maneuvers to reduce tension are undermining and deep tissue imbrication, but do these maneuvers reliably decrease tension and what is the effect on dermal perfusion? To date, no studies have reported the effects of undermining and imbrication on wound closure tension and dermal edge perfusion.
Purely “elastic” materials obey Hooke’s law and deform instantly when stressed and then return to their original state when that stress is removed. Deformation is directly and linearly proportional to the stress applied to it. A “plastic” material undergoes permanent deformation in response to a stress. The deformation of “viscous” materials depends on both the magnitude and duration of an applied stress. Mammalian skin typically behaves as a “viscoelastic” substance and as such exhibits both viscous and elastic characteristics when undergoing deformation by sutures. In the operating room, when a stress is applied for a matter of seconds to minutes, the skin exhibits elastic properties. However, if a stress is applied for days to weeks, its viscous properties dominate and it displays plastic properties, undergoing permanent deformation. “Stress relaxation” refers to the decrease in stress over time, whereas the deformation is held constant, as with the use of tissue expanders.2,3
Skin at nearly every point on the body has a resting tension caused by the elastic property of the dermis. Therefore, when it is disrupted surgically or traumatically, the skin recoils away from the wound because of unopposed tension. To reduce the size of the resultant defect, surgeons use sutures to counter the forces that would widen the wound. If skin were inanimate, the only limiting variables to primary wound closure would be suture strength and the skin’s ability to hold the suture. However, in vivo, the skin must be apposed while maintaining adequate perfusion.
The fibrous attachments between the dermis and subdermal tissues oppose the shearing forces generated when closing a wound. Undermining moves the origin of these shearing forces further away from the wound edge, allowing more skin elasticity to be recruited, essentially creating bilateral, random advancement flaps. The 2 major risks of this maneuver are the transection of perforating vessels and the creation of a potential space. In 1980, McGuire4 showed that wounds parallel to tension lines in swine benefit from undermining. This finding is consistent with the anisotropic property of mammalian skin, meaning that its elastic behavior varies in different directions. In 1982, Cox and Larrabee5 found that undermining large broadly based skin flaps in swine was not mechanically advantageous, whereas undermining narrow, thin flaps was beneficial.
Reducing wound tension improves perfusion, but do the maneuvers used reduce wound tension impair perfusion? Some surgeons advocate the imbrication of deep tissues rather than undermining, suggesting that imbrication preserves more dermal perfusion at the wound edge while reducing tension at the wound edge. The purpose of our study was to evaluate which technique, undermining or imbrication, most reliably reduced wound tension and what effect these techniques have on dermal perfusion at the wound edge. The study hypothesis was that imbrication will cause the greatest reduction in wound tension and have a negligible reduction in wound edge perfusion.
METHODS
All animal work described was reviewed and approved by the MedStar Health Research Institute’s Institutional Animal Care and Use Committee. Juvenile castrated male Duroc swine (30–55 kg) were received and handled according to facility standard operating procedures under an animal care and use program accredited by the Association for Assessment and Accreditation of Laboratory Animal Care International.
On the day of surgery, animals were anesthetized with a combination of ketamine and xylazine delivered intramuscularly. Animals were intubated, maintained on isoflurane, placed on a warming blanket, and ventilated, whereas heart rate, peripheral oxygen saturation, and core body temperature were continuously monitored by trained research staff. The body hair was clipped, and the skin was prepped with chlorhexidine gluconate scrub.
A total of 5 standardized, symmetrical pairs of wounds were created: 2 pairs on 2 swine and 1 pair on 1 swine. The wounds were created over the thigh/buttock region and the shoulders; these locations were defined by bony landmarks. Full-thickness fusiform wounds (6 × 3 cm) were created with a knife (Fig. 1). At each location, the orientation of the skin tension lines with respect to the y axis of the fusiform excision was recorded. Each excision was done at the same depth, just superficial to the panniculus carnosus (analogous to the deep investing fascia in humans). Hemostasis was achieved by Bovie electrosurgery (Bovie Medical Corp., Clearwater, Fla.). A single, simple interrupted 0-polypropylene suture was placed at the widest point of the wound, approximately 1 cm from the wound edges. No knots were thrown. The 2 suture tails were then pulled at an angle of 180 degrees to each other and tangential to the x axis of the wound until the wound edges were approximated. Wounds were then stapled, and suture tension was measured with a Tyrolean tensiometer (Pesola AG, Schindellegi, Switzerland; Fig. 1). The first measurement recorded for each wound was the raw wound tension. The wounds on 1 side were then undermined, whereas those on the other side were imbricated. Undermining was performed superficial to the panniculus carnosus in a subdermal plane. The undermined wounds were undermined by Bovie electrosurgery (Bovie Medical Corp.) at a distance of 4 cm from the wound edge circumferentially. The imbricated wounds were imbricated by placing figure of 8 sutures through the panniculus carnosus at the base of the wound with 0-polypropylene suture. After undermining or imbricating, wound tension was again measured with a Tyrolean tensiometer (Fig. 1). A speckle contrast imager (moorFLPI, Moor Instruments, Wilmington, Del.) was used to assess skin perfusion (Fig. 2). Images were captured before wounding and after undermining or imbrication. These data were then analyzed using the manufacture’s software (ImageJ). The speckle contrast imager shined a laser light on the wound producing a speckle image of varying contrasts where regions of high blood flow appeared as low contrast and regions without blood flow appeared as higher contrast. These contrasts were graded by intensity and color coded (Fig. 2).
Fig. 1.
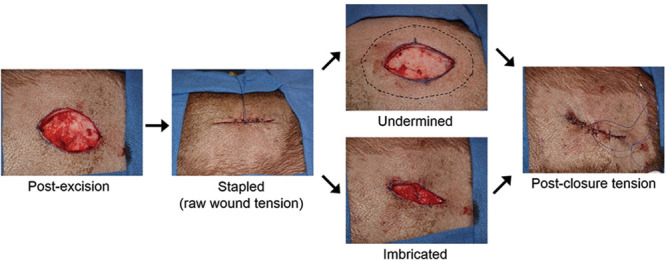
Schematic showing how wounds were measured in the study. Full-thickness wounds were excised in Duroc swine, and raw tension was measured after bringing the raw wound together, the wounds were then closed with either undermining or imbrication, and postclosure tension was measured with a Tyrolean tensiometer.
Fig. 2.

A speckle contrast imager was used to assess skin perfusion before and after wounding. The images reflect the perfusion after staple closure, undermining, and imbrication. The grid below the image indicates the intensity where red regions represent blood flow and blue regions represent areas without blood flow.
The raw, imbricated, and undermined skin tension values were evaluated for statistical significance via a paired two-tailed t test (VassarStats, ©1998–2011 Richard Lowry, Poughkeepsie, N.Y.). Dermal perfusions for undermined and imbricated wounds were assessed relative to raw wounds using paired two-tailed t tests. A multivariate analysis of variance was conducted across all major variable groups to assess statistical significance between groups (Microsoft Excel, Redmond, Wash.). A priori power analysis could not be performed because the magnitude of the difference was not known.
RESULTS
The mean raw tension was 7.1 N (range, 2.5–12 N), the mean undermined tension was 5 N (range, 1.5–14 N), and the mean imbricated tension was 5.9 (range, 1–14.5; Fig. 3; Table 1). Comparing the raw tension values with their respective undermined (4 cm) tension values showed a significant decrease in tension (P < 0.005). Comparing the raw tension values with their respective imbricated tension values also showed a significant decrease in tension (P < 0.05). Comparing the undermined tension values with their respective imbricated tension values showed no significant difference in tension (P = 0.17). Analysis of variance comparing the 3 groups revealed that the 3 groups were not significantly different (F = 1.44; P = 0.25; Table 2).
Fig. 3.
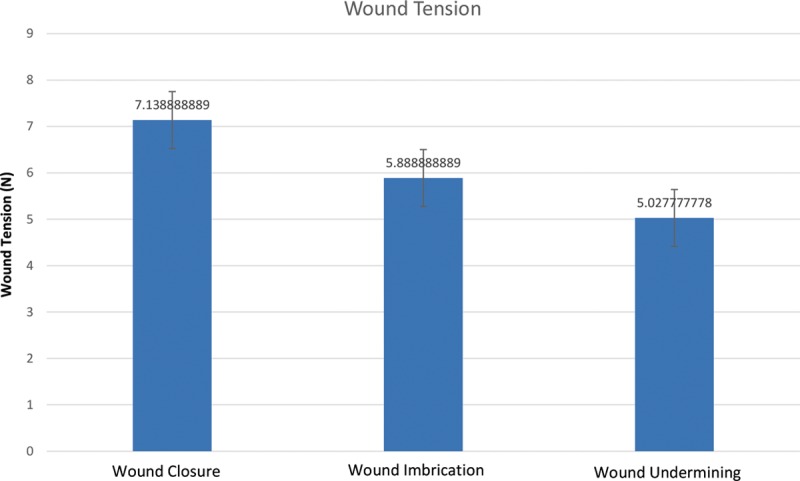
Raw, imbricated, and undermined wound tension values (N). There is a significant reduction in wound tension with either undermining or imbrication relative to the raw wound, but no significant reduction in tension exists between the methods of closure.
Table 1.
Tension and Perfusion Measurements for Wounds without Closure, with Deep Imbrication, and with Undermining

Table 2.
Analysis of Variance of the 3 Different Groups in the Study (Raw Wound, Imbricated Wound, and Undermined Wound) Showing No Significant Difference between the 3 Groups

Speckle contrast imaging showed a significant reduction in blood flow between unwounded skin (222 perfusion units [PU]; 95% confidence interval [CI], 187–257) and the imbricated wound (48.2 PU; 95% CI, 15–82; P< 0.05) and also showed a significant reduction in blood flow between the unwounded skin (205 PU; 95% CI, 134–277) and the undermined wound (63.4 PU; 95% CI, 24–103; P < 0.05). Relative to preexcision skin, perfusion in undermined wounds was greater than in imbricated wounds (30.7% vs 21.6%), but the difference was not significant (Figs. 4, 5).
Fig. 4.

Preexcision, raw, and undermined or imbricated wound perfusion values (PUs) using a speckle contrast imager. There is a significant decrease in wound perfusion with imbrication and undermining.
Fig. 5.

Relative dermal perfusion of both wound closure techniques relative to preexcision perfusion showing a greater relative perfusion with wound undermining relative to imbrication. The difference is not significant.
DISCUSSION
Wound closure is one of the most fundamental and important principles of surgery. Deep tissue imbrication and wound undermining are techniques used by surgeons for wound closure without objective evidence regarding which technique is superior. A Duroc swine model was used to conduct a prospective study comparing wound tension and dermal perfusion of wounds after deep tissue imbrication or wound undermining. When using a Tyrolean tensiometer to assess wound tension, both wound undermining and wound imbrication resulted in similar statistically significant reductions in wound tension. While using speckle contrast imaging to assess dermal perfusion, a significant decrease in wound perfusion was found when both wound imbrication and wound undermining were used relative to the unclosed wound. The relative wound edge perfusion (relative to unwounded skin) was greater for undermined wounds compared with imbricated wounds (30.7% vs 21.6%); however, this difference was not significant.
It is not surprising that both deep tissue imbrication and wound undermining significantly reduce wound tension. Both techniques have been in widespread use by surgeons for closed wounds, and many studies have confirmed their ability to reduce tension when closing defects.4–6 Few studies have examined the dermal perfusion of wounds when comparing wound closure techniques. This is the first prospective study to objectively compare both wound tension and dermal perfusion when comparing wound undermining with imbrication. There are a few possibilities as to why wound imbrication reduced dermal perfusion to a greater degree than wound undermining. Deep tissue imbrication and its deformation of deep tissues may cause pressure on perforating vessels, which could explain the reduction in wound edge perfusion seen with imbrication. Furthermore, deep tissue imbrication places foreign suture material in the wound, increasing the chances of infection leading to poor wound healing relative to wound undermining.
In a seminal study, McGuire4 found that the sequence in which the wounds are created at various locations has no apparent effect on force measurements. This study also found that undermining decreased the tension across all wounds in his model, except for wounds located in the dorsal posterior location that had their y axis oriented perpendicular to the lines of maximal tension. This suggested that tension was the greatest for wounds in which the y axis was oriented perpendicular to the lines of maximal tension. Our results are consistent with this finding where the tension for wounds oriented perpendicular to the line of maximal tension was higher than for wounds oriented parallel to this line. McGuire4 used intravenous fluorescein dye to evaluate the perfusion of undermined and nonundermined wounds, which were primarily closed under tension, and reported that all tissues appeared viable.
There are limitations to our study. We used a Duroc swine model to evaluate wound tension and wound perfusion, so the results of the study most directly apply to the swine. We used Duroc swine because the viscoelastic properties of the swine do resemble those of human skin making it one of the best available models for studying human physiology and pathophysiology.7
In our study, excisions were performed superior to the panniculus carnosus to allow for approximation of the superficial fascial system as described by Lockwood.8,9 Our study cannot speculate as to the tension or perfusion below the panniculus carnosus, and our perfusion assessment could not evaluate perfusion at this depth.
There are inherent flaws with using laser perfusion imaging to assess dermal perfusion. There is variability in its assessment related to the time after wounding, depth of penetration, and stochastic error because of the lack of units. The laser is only able to detect perfusion up to approximately 1.5 mm in depth; the dermal thickness of our wounds was on average 1.75 mm. It is possible that blood flow in the subdermal plexus was not detected causing a false negative result, suggesting that wound imbrication significantly reduces dermal perfusion. This is unlikely because this limitation would have also applied to the undermined wound, which did not show a significant decrease in perfusion. Also, it was not possible to blind the researcher performing the tension and perfusion assessments as to which wounds were undermined or imbricated as this can be easily discerned by looking at the wound before it is completely closed. When assessing the closed wounds, the researcher was blinded as to which wound was imbricated or undermined.
We plan to keep the swine alive to monitor wound healing over time with weekly biopsies. Other future directions of our research include performing intraoperative tension and perfusion measurements on human skin with the use of indocyanine green angiography.
CONCLUSIONS
Regarding wound edge tension, we found significance decreases in wound tension when using either deep imbrication or undermining relative to the unclosed wound. We found significant decreases in dermal perfusion with both imbrication and undermining, but the relative perfusion was higher with wound undermining. Wound undermining should be preferentially performed relative to deep imbrication to maximize dermal perfusion while reducing wound tension.
Footnotes
Disclosure: Funding for the study was received from the D.C. Firefighter Burn Foundation Fund. The article processing charge was paid by Dr. Stephen P. Davison of Da Vinci Plastic Surgery, Washington, D.C.
REFERENCES
- 1.Millard DR., Jr . Principlization of Plastic Surgery. 1st ed 1986. [Google Scholar]
- 2.Neligan PC. Plastic Surgery. (3rd ed) 2012;14–15(1):240–296. [Google Scholar]
- 3.Thorne CH. Grabb and Smith’s Plastic Surgery. 7th ed. 2013. pp. 1–38. [Google Scholar]
- 4.McGuire MF. Studies of the excisional wound: I. Biomechanical effects of undermining and wound orientation on closing tension and work. Plast Reconstr Surg. 1980;66:419–427. [PubMed] [Google Scholar]
- 5.Cox KW, Larrabee W., Jr A study of skin flap advancement as a function of undermining. Arch Otolaryngol. 1982;108:151–155. doi: 10.1001/archotol.1982.00790510023005. [DOI] [PubMed] [Google Scholar]
- 6.Clark JD, Baldwin RL, Bayne KA, et al. In: In: Guide for the Care and Use of Laboratory Animals. Grossblatt N, editor. Washington, DC: National Academy Press; 1996. [Google Scholar]
- 7.Travis TE, Mino MJ, Moffatt LT, et al. Biphasic presence of fibrocytes in a porcine hypertrophic scar model. J Burn Care Res. 2015;36:e125–e135. doi: 10.1097/BCR.0000000000000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lockwood TE. Fascial anchoring technique in medial thigh lifts. Plast Reconstr Surg. 1988;82:299–304. doi: 10.1097/00006534-198808000-00015. [DOI] [PubMed] [Google Scholar]
- 9.Lockwood TE. Superficial fascial system (SFS) of the trunk and extremities: a new concept. Plast Reconstr Surg. 1991;87:1009–1018. doi: 10.1097/00006534-199106000-00001. [DOI] [PubMed] [Google Scholar]


