Sir:
In reconstructive breast surgery, skin-flap quality is an important determinant of surgical outcome. Although the overall rate of complications is low in breast surgery,1 some patient cohorts may be associated with a significantly higher risk of wound complications.2,3 Lin et al2 found that breast reconstruction in irradiated wound beds has been associated with a greater than 3-fold increase in complications. In addition, many other factors have also been shown to increase the risk of subsequent wound complications in breast surgery, including elevated body mass index, smoking status, diabetes, steroid use, and even the location and type of incision.3 Given a higher rate of complications in some high-risk incisions in breast surgery, techniques to improve the strength of wound closure are of considerable interest.
The use of periincisional dermal deepithelialization to create extended wound apposition has previously been demonstrated to be a successful technique to close incisions in both perineal/sacral wounds4 and reduction mammoplasties.5 In 1 series of 9 patients undergoing sacral resections in previously irradiated tissue beds—a procedure that typically results in a high rate of dehiscence—the use of extended dermal apposition resulted in a satisfactory closure in all cases.4
In breast surgery, one commonly used technique to minimize the risk of incisional complications in higher risk wounds has been to excise the portions of the skin flap that seem nonviable on visual assessment. In an effort to use this potentially viable tissue, we propose the use of a simple technique to strengthen high-risk wounds in breast reconstruction by increasing dermal apposition through periincisional deepithelialization and the use of an extended dermal flap.
The technique is a modified version of that used by Hartzell et al.4 The inferior and superior edges of the incision are brought together with a gentle manual pincer grasp. An elliptical line is drawn around the incision approximating the point of superior and inferior dermal contact during the pincer grasp, typically 1 to 1.5 cm inferior and superior to the incision. The portion of the ellipse on the superior flap is deepithelialized (Fig. 1A). The superior dermal flap is then approximated with the inferior wound edge using interrupted, buried, absorbable deep dermal sutures (Fig. 1B). A subcuticular suture is used to complete the epidermal closure. The superior dermal flap should overlap significantly with the inferior edge’s dermis, allowing for adequate dermal seal.
Fig. 1.
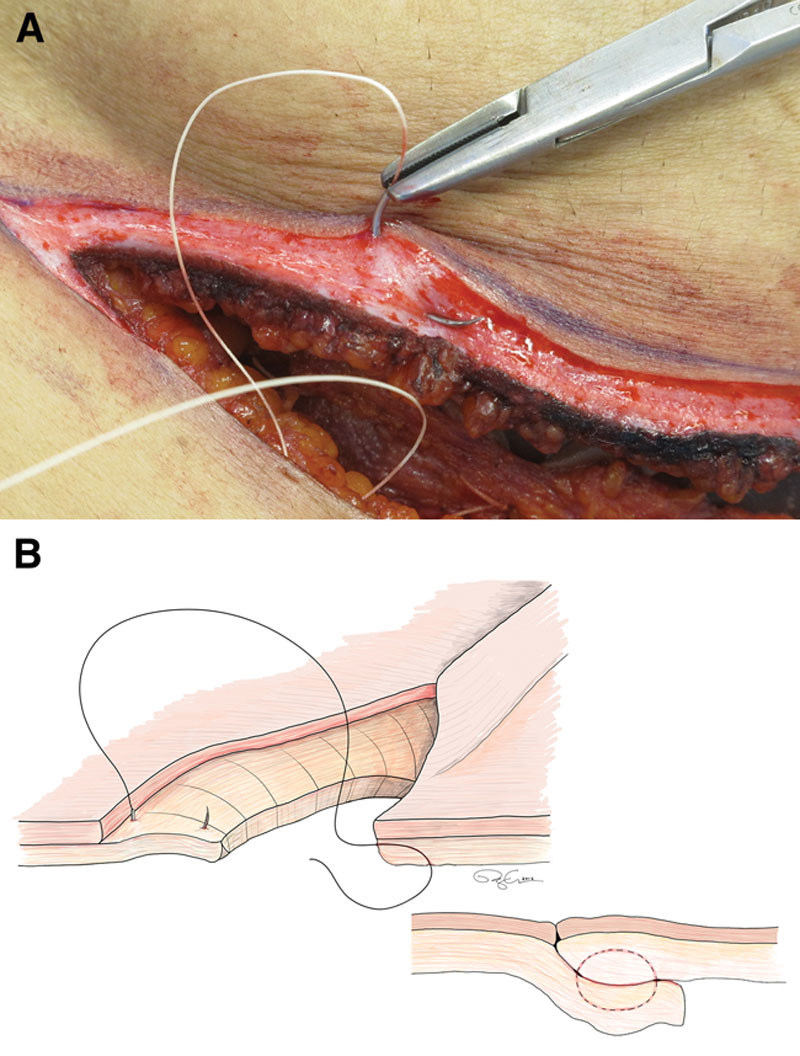
Deepithelialization incision closure technique. A, Photograph of the deepithelialized dermal flap on the superior aspect of a breast incision. A, A CT2 needle is placed going into and coming out on the deepithelialized dermal surface (right). B, Diagram of the suture technique going from the wound edge to the deepithelialized flap (left) to create an extended dermal apposition closure (right).
The use of extended dermal flaps to strengthen the wound closure in high-risk breast incisions is a valuable addition to the reconstructive breast surgeon’s armamentarium. The technique is quick and easy to perform, adds a strong dermal seal beneath the standard subcuticular closure, and uses tissue that is commonly discarded by the reconstructive surgeon. With minimal risk of using this technique, we think that it may be used for most high-risk wound closures in breast surgery, especially those associated with radiation exposure. Since the incorporation of this technique in our breast surgery practice, we have not experienced a wound dehiscence, even in high-risk cases.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid by the authors.
REFERENCES
- 1.Kjøller K, Hölmich LR, Jacobsen PH, et al. Epidemiological investigation of local complications after cosmetic breast implant surgery in Denmark. Ann Plast Surg. 2002;48:229–237. doi: 10.1097/00000637-200203000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Lin KY, Blechman AB, Brenin DR. Implant-based, two-stage breast reconstruction in the setting of radiation injury: an outcome study. Plast Reconstr Surg. 2012;129:817–823. doi: 10.1097/PRS.0b013e31824421d0. [DOI] [PubMed] [Google Scholar]
- 3.Ibrahim AM, Shuster M, Koolen PG, et al. Analysis of the National Surgical Quality Improvement Program database in 19,100 patients undergoing implant-based breast reconstruction: complication rates with acellular dermal matrix. Plast Reconstr Surg. 2013;132:1057–1066. doi: 10.1097/PRS.0b013e3182a3beec. [DOI] [PubMed] [Google Scholar]
- 4.Hartzell TL, Medina M, Hornicek FJ, et al. Extended dermal apposition: a simple technique for the closure of irradiated perineal and sacral wounds. Plast Reconstr Surg. 2011;127:170e–173e. doi: 10.1097/PRS.0b013e318213a3e2. [DOI] [PubMed] [Google Scholar]
- 5.Domergue S, Ziade M, Lefevre M, et al. Dermal flaps in breast reduction: prospective study in 100 breasts. J Plast Reconstr Aesthet Surg. 2014;67:e147–e150. doi: 10.1016/j.bjps.2014.02.004. [DOI] [PubMed] [Google Scholar]


