Abstract
Background:
Surgical cutting guides are used in mandibular reconstruction involving osteotomy of the mandible and fibula. Cutting guides produced using computer-aided design (CAD) and computer-aided manufacturing (CAM) technologies have been reported recently. These guides aim to increase the benefits to patients by improving the accuracy, shortening the operating time, and correcting occlusion. However, the availability of these advanced technologies is limited in some regions of the world. To test whether we could produce low-cost surgical cutting guides, we made surgical guides and investigated their accuracy.
Methods:
Using free CAD software, we designed surgical cutting guides for the mandible and fibula and used these to perform virtual mandibular segmental osteotomies and fibula transplants in 12 model surgeries. The cutting guides were printed on a 3-dimensional (3D) printer. The model surgeries were performed using 3D mandibular models and cutting guides to check their accuracy. Deviations between the virtually simulated plan and the actual model surgery were investigated.
Results:
CAD and CAM technologies were used to design and 3D print the cutting guides and models. The guided surgeries were performed. The deviations were about 1.3 mm for mandibular osteotomy, less than 1 mm for fibular osteotomy, and within 2.4 mm for reconstructions of the mandible.
Conclusions:
Without using expensive software or products, we were able to design surgical cutting guides for the mandible and fibula and used these to perform virtual simulation of mandibular segmental osteotomy and fibular reconstruction. Model surgeries using 3D-printed surgical guides showed that the accuracy of reconstruction was within a 3-mm deviation. In circumstances where commercial CAD/CAM guides are not available, it may be possible to use CAD/CAM surgical guides in the clinic if doctors are willing to volunteer their time for the design and printing.
The free fibular flap is one of the most common techniques used in mandibular reconstruction after resection of a malignant tumor in the head or neck. When a fibular flap is planned, it is very important to decide where the mandible should be osteotomized, where the fibula should be cut, and how accurately the surgery should be performed. These are often decided based on a presurgical plan to try to maximize good outcomes for patients.
Reconstruction techniques using surgical cutting guides to improve the accuracy of osteotomies have been reported. Computer-aided plans are thought to enable a more accurate osteotomy and reconstruction compared with conventional surgery.1 As part of the planning for reconstruction using computer-aided design (CAD) or computer-aided manufacturing (CAM) techniques, CAD software is used to design the surgical guides, and a 3-dimensional (3D) printer is used to print the designed guides. The software for these techniques, such as Mimics and 3-matic (Materialize, Leuven, Belgium), is expensive and is not available in some countries because of regulations. Experiences with such CAD software and surgical guides have been reported mainly in Europe and North America.2–5 However, these products are not available in our country.
The aim of this study was to explore whether we could produce low-cost surgical cutting guides without using expensive products. For this purpose, we made surgical guides for mandibular reconstruction using CAD technologies. In this report, we investigated the accuracy of the low-cost cutting guides.
MATERIALS AND METHODS
We used free public software, InVesalius (Technology of Information Renato Archer Centre of the Ministry of Science and Technology, Campinas, Brazil), to produce 3D stereolithography (STL) files of the mandibular and fibular bones from Digital Imaging and Communication in Medicine data for mandibles and fibulas. Artifact is deleted as possible. These STL files were imported to free CAD software Blender (The Blender Foundation, Amsterdam, the Netherlands). We designed the surgical cutting guides and manufactured them using the methods described below. Model surgeries and the measurement of reference points were performed for 12 cases of anonymous human mandibles and fibulas, for which the donors’ consent was obtained. Defect areas were randomly set (Fig. 1), but the condylion laterale (Cl) was not chosen. To improve the ease of the measurements, reference points such as Cl, gonion (Go), mental tubercle (T), menton (Me), and pogonion (Pog) were set in the virtual mandibles.
Fig. 1.
Defect areas are shown in black (n = 12).
1. Virtual osteotomy
Using Blender software, we planned the areas for a segmented osteotomy of the mandible using the 3D mandibular bone. The planes for the osteotomy were set to both edges of the osteotomized area. The areas of the osteotomy were set to have 1 or more reference points, such as Go or T. At the edges of the osteotomy, points were also set for measurements. For easier reproduction of these reference points, additional planes, such as the angle plane and tubercle plane, were usually added (Fig. 2).
Fig. 2.
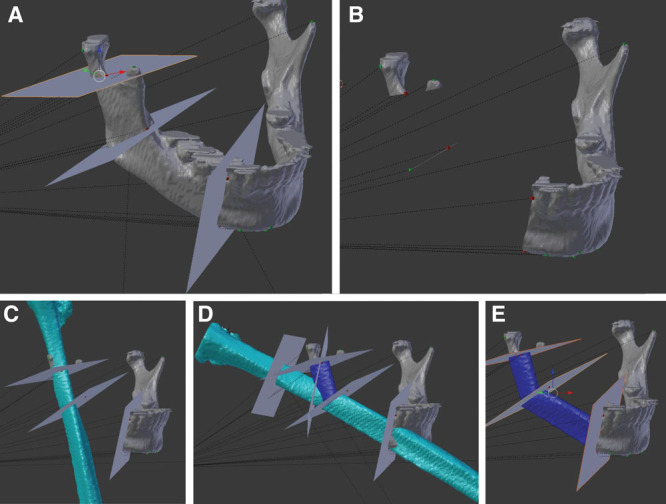
Virtual mandibular osteotomy and fibula inset. A, Two osteotomy planes are set near the condyle and right mental tubercle. Between these 2 planes, another plane, which includes the gonion, is set for later use in the osteotomy with the gonion. B, Mandibular osteotomy is performed virtually. C, The fibula transplant is set to reproduce the ramus of the mandible. D, After cutting of the fibula to fit the ramus to the gonion, the remaining fibula is rotated to fit to the body of the mandible. E, Two osteotomized fibular segments are placed.
After setting the planes for the osteotomy, resection of the bone was performed virtually. Then, the bone defect was defined, and the fibular STL file was imported to the bony defect. Fine tuning of the position of the fibula was necessary to reproduce the missing reference points. If the fibula had to be divided into 2 or 3 pieces, the osteotomy planes for the fibular divisions were set and cut virtually for each aspect. After division, the divided fibula was rotated and fit to the other defects. These simulations were planned to reproduce the reference points, such as Go and T. The curved shape of the body of the mandible was not included in the planning in this study. Our most serious concern was reproduction of Go and T. If a satisfactory virtual location of the transferred bone was not obtained, the simulation was repeated. In the cases of divided bone set at less than 2 cm, a new Go or T was shifted to increase the bone length to more than 2 cm for safer vascularization.
2. Guides design
Using these procedures, we produced mandibles and fibulas with the defects and osteotomy planes described.
In the mandible (Fig. 3), the osteotomy planes were thickened to 5 mm. The solid mandible was subtracted from this to create a thick osteotomy plane that could be fit to the outer surface of the mandible. In addition to this solid, a 2-cm wide outer surface plane of the mandible was thickened to 3 mm. If this solid was near a condyle, its width was shortened because 2 cm is considered too large to be inserted in actual surgery.
Fig. 3.
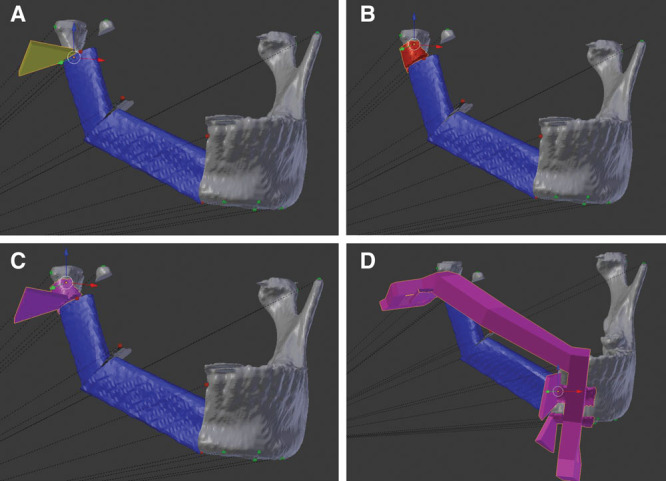
Designing the mandibular cutting guide. A, The osteotomy plane near the condyle is thickened to show the cutting plane. B, To make the guide fit to the mandible, the outer surface of the remaining ramus is thickened. C, The cutting plane solid and fitting surface solid are united. D, The cutting guides at both ends of the osteotomy are connected with pillars. This becomes the final cutting guide.
These procedures were performed at both edges of the osteotomies. After the 4 solids were united, a prop was used to connect each body; this was called the cutting guide. This guide was planned to include the planes for a segmental osteotomy, to connect the bones scheduled to remain after the osteotomy, and to maintain the relationships between the remaining bones, which acted as external fixators.
For the fibula (Fig. 4), because the osteotomy planes were set in even numbers, each pair of planes was connected to make a solid, and the fibular bone solid was subtracted from these solids. The remaining solids and a prop to connect them were united to make a fibular jig.
Fig. 4.
Designing the fibular cutting guide. A, The osteotomy planes are decided at the time the virtual fibula is inset into the mandible. B, The osteotomy planes are connected to make a solid. The box-shaped solid is made by subtracting the fibula solid. Each solid is connected with a pillar. C, Reverse view of the fibular guide.
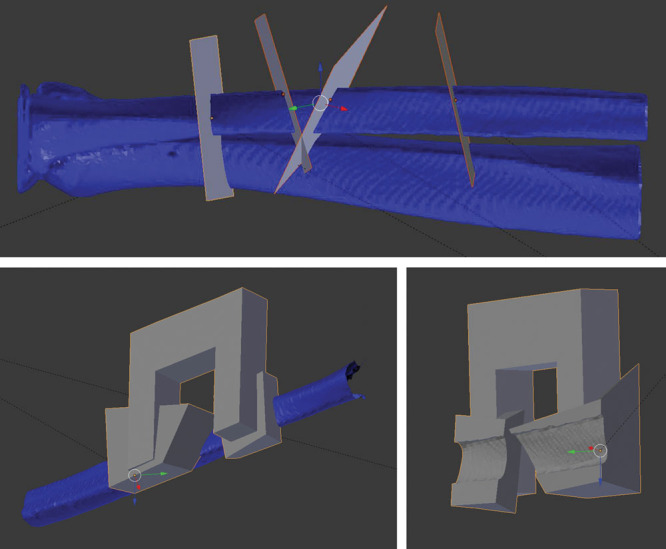
3. Manufacture of the surgical cutting guides (Fig. 5)
Fig. 5.
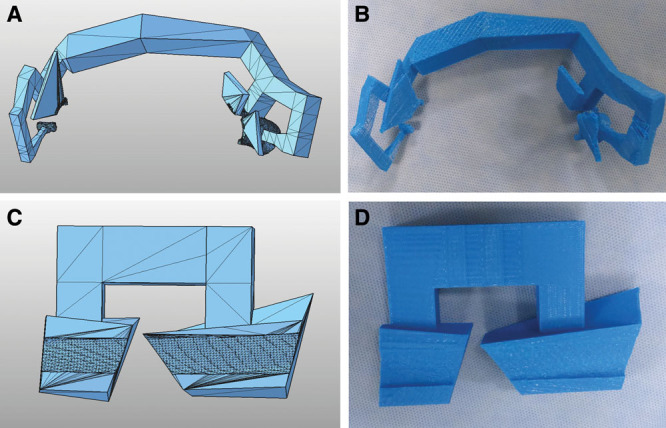
Three-dimensional printing of the design. A and B, The virtual mandibular guide and actual printed guide. C and D, The virtual fibular guide is also printed.
The virtual cutting guides for both the mandible and fibula were exported as STL files. These STL files were applied by using the 3D printer. In our laboratory, we use a fifth-generation MakerBot Replicator (MakerBot Industries, New York, N.Y.), which we purchased for about 3,000 USD. Polylactic acid was used as the material.
4. Model surgery (Fig. 6)
Fig. 6.
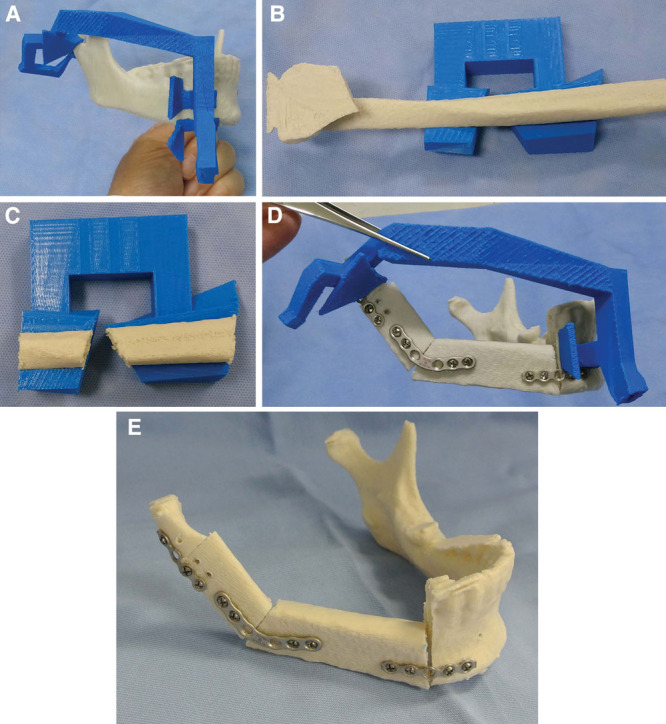
Model surgery. A, The printed mandibular cutting guide is fitted to the mandibular model. B, The fibular guide is placed in the fibular model. C, The osteotomies are performed on the model fibula. D, The fibular bone parts are transplanted to the model after the mandibular osteotomy, and the titanium plates are fixed. E, After removal of the mandibular guide.
The mandible, fibula, and guides were printed. The guides were fixed to bones with titanium screws (Synthes, West Chester, Pa.). The osteotomy was performed with a bone saw along the mandibular guide to create the bone defect model. The guide was also fixed to the fibula, and the fibula was osteotomized. The bone pieces were connected with titanium plates and then fixed to the mandible. Finally, the mandibular guide was removed. Model surgery was performed for each of the 12 cases.
5. Measurement (Fig. 7)
Fig. 7.
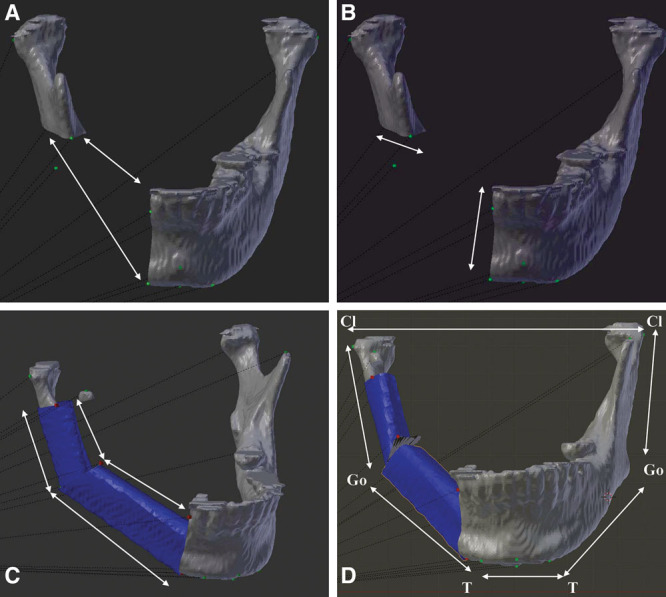
Measurements: the defect lengths (cranial and caudal, A), osteotomy lengths (mesial and distal, B), transplanted fibular lengths (cranial and caudal, C), and reference points, such as Cl-Cl, Cl-Go, and Go-T, are measured in both the virtual plan and model surgery (D).
To evaluate the accuracy of the osteotomies, the length of the osteotomies and the gaps of the remaining mandibular bones were calculated. For fibulas, both the cranial and caudal lengths of the divided fibular bones were calculated.
To evaluate the accuracy of the reconstructions, the distances between reference points (Cl-Cl, Cl-Go, Go-T, T-T, and so on) were calculated.
Measurements were made for both the actual model surgeries and virtual plans, and the results were compared. The virtual measurements were calculated using the same CAD software, and direct measurements were made in the model surgeries. The differences between the simulation plan and the actual model were calculated as deviations. Excel-Toukei 2010 software (SSRI, Tokyo, Japan) was used for statistical analysis.
RESULTS
Virtual osteotomies were possible using the free software. The changes and resetting of the osteotomy locations could be done at any time. The mandible osteotomy took several minutes to complete. The fibular arrangement took 5 minutes for a single osteotomy and 20 minutes for 3 divisions. The setting of reference points took 20 minutes, and the total time for the virtual osteotomy was within 50 minutes.
The jigs could be designed using free software. Subtractions, intersections, and unions of solids, which require Boolean operations, were also possible. Because the software we used was designed for purposes other than the production of surgical jigs, time and experience were needed to make the revisions for closing small holes or flipping the reverse planes.
In planning the mandibular guides, the areas in the surgical field in the actual surgery were limited for minimally invasive surgery, which meant that there were also limited sites for placement of the guides. In addition, the guide pillars had to be located so as not to disturb the ablative and reconstructive surgeries. Because the guides must be planned to obtain the correct fitting to the bones, a long time was needed to fulfill the specifications of these designs. At least 2 hours was necessary for designing the mandibular guide. By contrast, only 15 minutes was needed for the fibular guide because placement of a fibular guide is not limited.
3. The time needed to print 1 guide was about 5 hours. Occasionally, the printing failed. For failed printing, we revised the designs, and all guides were printed successfully.
4. In the model surgery, all printed guides were fit completely to the mandible and fibular models, and the model surgeries were possible in all cases.
5. The measured osteotomy gaps and lengths of the mandibles and fibulas are shown in Figure 8. For the mandibles, the average osteotomy length deviation was 0.66 mm (n = 18; 0.01–1.79 mm) and the average bone defect gap deviation was 1.33 mm (n = 24; 0.15–5.46 mm). In the fibulas, the average deviation of the segmented bones was 0.92 mm (n = 58; 0–6.18 mm).
Fig. 8.
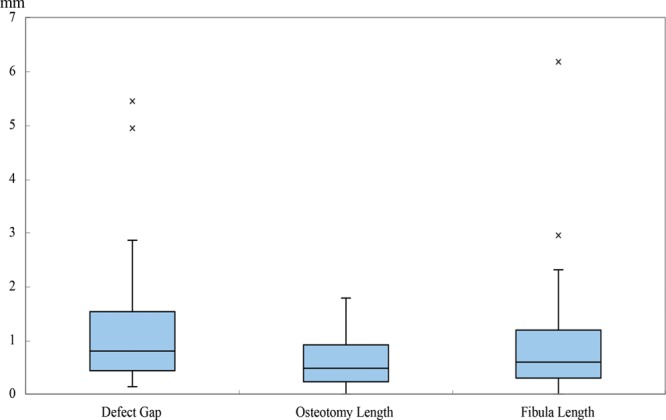
Results of the osteotomies. The average deviations between the plan and model are shown. The average distance deviations were 1.33 mm for the bone defect gap (n = 22; 0.15–5.46 mm; SD = 1.43), 0.66 mm for osteotomy length (n = 16; 0.01–1.79 mm; SD = 0.55), and 0.92 mm for fibular length (n = 54; 0–6.18 mm; SD = 1.00). The average error for the complete procedure was about 1 mm.
The distances between reference points after reconstruction are shown in Figure 9. The average deviation between the plan and the model was 2.34 mm (n = 12; 0–8.61 mm). The average deviations were 1.023 mm (n = 38) in the unreconstructed area and 1.43 mm (n = 16; 0.02–6.08 mm) in the reconstructed area. However, indirectly affected distances, such as Cl-Cl, were deviated by an average of 2.35 mm (n = 12; 0.02–6.34 mm).
Fig. 9.
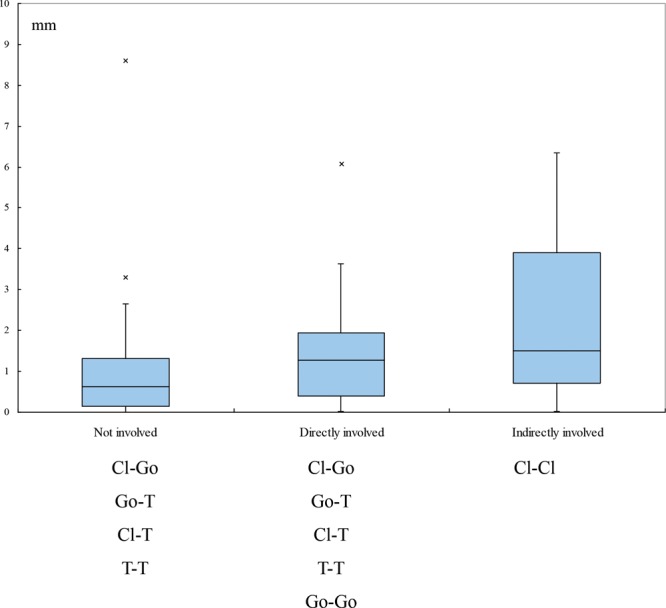
Results for reconstructed reference point discrepancies. The average deviation in distance between the reference points for points not involved in the reconstruction was 1.02 mm (n = 38; 0–8.61 mm; SD = 1.52) except for Cl-Cl. The average deviation between points directly involved in the reconstruction was 1.59 mm (n = 44; 0.02–6.08 mm; SD = 1.23). The most deviated point was the Cl-Cl distance, which was not directly involved in the reconstruction. The average deviation was 2.34 mm (n = 12; 0.02–6.34 mm; SD = 2.30).
DISCUSSION
Surgical cutting guides are now used in mandibular segmental osteotomies and reconstruction with a fibula. It is unclear whether this procedure is superior to traditional methods in terms of clinical outcomes. However, the theoretical superiority for calculating lengths and cutting angles of bones by computer is considered valuable. Although the advantages of computer-aided surgery include repeated simulations and accurate calculations, there are disadvantages, such as the cost and product delivery time.
In our country, commercially available surgical guide products are not available yet, and we cannot use these new computer-assisted products. Thus, we need to make computer-assisted surgical guides ourselves. Wilde et al4 noted a cost of 1,800 to 6,000 USD for commercial products. Producing the guides ourselves may help reduce costs. Thus, we used free software for CAD in this study. This free CAD software is not intended for use in mandibular reconstruction, and it was daunting to use this the first time without any reference books. However, once we became accustomed to it, we encountered no difficulties in using the software. We note that designing the product without disturbing the surgical field is essential but difficult.
Using this software enabled us to perform virtual osteotomies and to design surgical guides for free. For manufacturing the guides, 3,000 USD is a necessary initial investment for the 3D printer. The material cost for printing 1 guide is about 2 USD. If the initial investment is not affordable, entrusting printing to a commercial company is 1 option. We ordered 1 guide on trial, and its cost was 200 USD. Therefore, for mandibular reconstruction, a minimum of 400 USD is needed for printing mandibular and fibular guides. The cost of designing the guides is the time volunteered by the medical doctors.
Questions arise regarding the accuracy of this method and whether this low-cost CAD/CAM guide can ensure a precise osteotomy and accurate inset of the bone flap. Hanasono and Skoracki2 reported significant improvements in the accuracy in virtually simulated methods. Their comparison of pre- and postsurgical evaluations of bony landmarks found average deviations of 4.11 mm in the simulation group and 6.92 mm in the conventional group. Ayoub et al5 also reported a deviation of 6 mm using conventional methods, which was significantly improved to 1.5 mm in the computer-assisted group. Other reports have noted that computer-simulated methods produce deviations less than 2 or 3 mm from the preoperative plans for mandibular reconstruction.6–11 For osteotomies of the fibula, Hanasono and Skoracki2 reported that the divided fibular segments had an average 2.4-mm difference in length from the initial plans.
In our study, the average deviations from the osteotomy plan were 0.66 mm for mandibular osteotomies and 0.92 mm for fibular osteotomies. After reconstruction, the deviations were 1.33 mm for the gap of the bony defect and 2.35 mm for the reference points. Thus, in terms of accuracy, the osteotomies were performed within 1 mm of error. These results show that the low-cost design is not inferior to previous reports in osteotomies.
The deviation for the unreconstructed area (on average, 1.023 mm) is an error that may have been caused by a measurement error or a 3D-printing accuracy error. We could not avoid these in this study. The errors related to the guide design, stability, manual osteotomy, and fixation techniques are included in the errors for the reconstructed area.
To evaluate the reconstructed landmarks, the deviations in distances between adjacent reference points, such as Go-T or T-T, were measured, and these averaged 1.43 mm. However, the average deviation in distances between distant points, such as Cl-Cl (which is indirectly affected), was 2.35 mm (maximum of 6 mm). This means that the deviation of each segment may not be obvious, but the accumulation of errors can sometimes lead to obvious deviations. For example, if the Go-T-T-Go is removed, 3 separate fibular segments (Go-T, T-T, and T-Go) will be inserted in the reconstruction. Although neither Cl is directly involved in the operation, the final Cl-Cl distance can be indirectly influenced by the 4 connections of the 3 bone segments. Therefore, the errors should be counted for at least 3 connections.
To avoid these errors, several refinements should be made. First, the mandibular guide should be rigid enough, so that it does not bend during surgery. Second, the number of fibular segments should be reduced. Third, sockets can be made in which to place the fibular segment and to help decide on the appropriate lengths and angles.
During this study, we sometimes felt that the guides were frail when used with a thin body. The body of the guide should be thin enough, so that the operating field can be observed but thick enough to provide sufficient rigidity and stability. Reducing the bony parts may help to reduce errors, but this could lead to inaccurate bony reconstruction if the reference points, such as Go or T, are not reconstructed. After this study, we made sockets to improve the fitting, but this required complicated designs and extra time. A simpler design does not seem to improve the accuracy, and we are still looking for a point of compromise.
We expect that this technique will help reduce operating time. In this study, we counted time only for planning. Preoperative virtual planning took about 3 hours and 3D printing about 10 hours. In clinical studies that reported shortening of the operating time,2,12 we presume that considerable time for preoperative simulation was also needed. If outsourcing is possible, CAD technicians can help surgeons. Extra time was needed in our study because the surgeons performed the CAD/CAM themselves. The time required might be a voluntary contribution by the surgeon to reduce the cost.
CONCLUSIONS
Without using expensive software, virtual simulation of mandibular segmental osteotomy and fibular reconstruction and the design of surgical cutting guides for the mandible and fibula were possible. Model surgery using the 3D-printed surgical guides showed that guided surgery can be performed. The average deviation was about 1.3 mm for mandibular osteotomies, less than 1 mm for fibular osteotomies, and within 2.4 mm for reconstructions of mandibles. In circumstances where commercial CAD/CAM guides cannot be obtained, it might be possible to use CAD/CAM surgical guides in the clinic if doctors are willing to volunteer their time for the design and printing.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Tarsitano A, Del Corso G, Ciocca L, et al. Mandibular reconstructions using computer-aided design/computer-aided manufacturing: a systematic review of a defect-based reconstructive algorithm. J Craniomaxillofac Surg. 2015;43:1785–1791. doi: 10.1016/j.jcms.2015.08.006. [DOI] [PubMed] [Google Scholar]
- 2.Hanasono MM, Skoracki RJ. Computer-assisted design and rapid prototype modeling in microvascular mandible reconstruction. Laryngoscope. 2013;123:597–604. doi: 10.1002/lary.23717. [DOI] [PubMed] [Google Scholar]
- 3.Hirsch DL, Garfein ES, Christensen AM, et al. Use of computer-aided design and computer-aided manufacturing to produce orthognathically ideal surgical outcomes: a paradigm shift in head and neck reconstruction. J Oral Maxillofac Surg. 2009;67:2115–2122. doi: 10.1016/j.joms.2009.02.007. [DOI] [PubMed] [Google Scholar]
- 4.Wilde F, Hanken H, Probst F, et al. Multicenter study on the use of patient-specific CAD/CAM reconstruction plates for mandibular reconstruction. Int J Comput Assist Radiol Surg. 2015;10:2035–2051. doi: 10.1007/s11548-015-1193-2. [DOI] [PubMed] [Google Scholar]
- 5.Ayoub N, Ghassemi A, Rana M, et al. Evaluation of computer-assisted mandibular reconstruction with vascularized iliac crest bone graft compared to conventional surgery: a randomized prospective clinical trial. Trials. 2014;15:114. doi: 10.1186/1745-6215-15-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huang JW, Shan XF, Lu XG, et al. Preliminary clinic study on computer assisted mandibular reconstruction: the positive role of surgical navigation technique. Maxillofac Plast Reconstr Surg. 2015;37:20. doi: 10.1186/s40902-015-0017-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roser SM, Ramachandra S, Blair H, et al. The accuracy of virtual surgical planning in free fibula mandibular reconstruction: comparison of planned and final results. J Oral Maxillofac Surg. 2010;68:2824–2832. doi: 10.1016/j.joms.2010.06.177. [DOI] [PubMed] [Google Scholar]
- 8.Zheng GS, Su YX, Liao GQ, et al. Mandible reconstruction assisted by preoperative simulation and transferring templates: cadaveric study of accuracy. J Oral Maxillofac Surg. 2012;70:1480–1485. doi: 10.1016/j.joms.2011.05.015. [DOI] [PubMed] [Google Scholar]
- 9.Stirling Craig E, Yuhasz M, Shah A, et al. Simulated surgery and cutting guides enhance spatial positioning in free fibular mandibular reconstruction. Microsurgery. 2015;35:29–33. doi: 10.1002/micr.22229. [DOI] [PubMed] [Google Scholar]
- 10.Metzler P, Geiger EJ, Alcon A, et al. Three-dimensional virtual surgery accuracy for free fibula mandibular reconstruction: planned versus actual results. J Oral Maxillofac Surg. 2014;72:2601–2612. doi: 10.1016/j.joms.2014.07.024. [DOI] [PubMed] [Google Scholar]
- 11.Schepers RH, Raghoebar GM, Vissink A, et al. Accuracy of fibula reconstruction using patient-specific CAD/CAM reconstruction plates and dental implants: a new modality for functional reconstruction of mandibular defects. J Craniomaxillofac Surg. 2015;43:649–657. doi: 10.1016/j.jcms.2015.03.015. [DOI] [PubMed] [Google Scholar]
- 12.Toto JM, Chang EI, Agag R, et al. Improved operative efficiency of free fibula flap mandible reconstruction with patient-specific, computer-guided preoperative planning. Head Neck. 2015;37:1660–1664. doi: 10.1002/hed.23815. [DOI] [PubMed] [Google Scholar]


