Summary:
Although immediate postmastectomy breast reconstruction is favored over delayed reconstruction, it remains associated with high complication rates. Potential complications include seroma formation, dehiscence, infection, and tissue necrosis along incision edges. Closed incision negative pressure therapy (ciNPT; Prevena Incision Management System, KCI, an Acelity company, San Antonio, Tex.) has been reported to help hold incision edges together, protect incisions from external contamination, and remove fluid and infectious material. We investigated outcomes of applying ciNPT with a customizable dressing over closed incisions in 13 patients (25 breasts) who received immediate postmastectomy reconstruction as part of 2-stage expander/implant breast reconstruction. Nipple-sparing mastectomy was performed on 14 breasts, reduction-pattern mastectomy on 6 breasts, and skin-sparing mastectomy on 5 breasts. All breasts had ciNPT with a customizable dressing applied over the entire clean closed incision immediately after surgery at −125 mmHg for an average of 4.3 days. At 3-month follow-up, 24 of the 25 (96%) breasts had achieved healing. Delayed hematoma occurred on postoperative day 13 in 1 breast in the nipple-sparing mastectomy group and resolved. In the reduction-pattern mastectomy group, superficial dehiscence occurred on 3 breasts and resolved with local wound care. One breast in that group developed flap necrosis requiring surgical revision. Less drainage was observed in attached closed-suction drains, so time to drain removal was reduced from an estimated average of 12–14 days to 8.2 days. Based on the initial experience in this study, larger studies are warranted to evaluate the use of ciNPT with customizable or peel-and-place dressings after immediate postmastectomy breast reconstruction.
Immediate postmastectomy reconstruction as part of 2-stage expander/implant breast reconstruction provides better aesthetic outcomes1 and psychological benefits for patients2 but is associated with high complication rates. Seroma formation, infection, dehiscence, and tissue necrosis are possible problems after immediate reconstruction.3,4
Favorable results have been reported using closed incision negative pressure therapy (ciNPT; Prevena Incision Management System, KCI, an Acelity company, San Antonio, Tex.) over various incision types.5 Studies have shown that ciNPT helps hold incision edges together, removes fluid and infectious materials, and protects incisions from external contamination.5
We investigated outcomes of applying ciNPT with a customizable dressing over closed incisions on 13 patients (25 breasts) who received immediate postmastectomy breast reconstruction.
PATIENTS AND METHODS
Deidentified patient data were used in accordance with the principles outlined in the Declaration of Helsinki. A retrospective chart review collected data on patients who underwent two-stage expander/implant-based reconstruction with placement of expanders and incision management with ciNPT as part of immediate postmastectomy breast reconstruction.
Two breast surgeons and plastic surgeons were involved in this cohort. Reconstructive techniques utilized by both surgeons were the same. Nipple-sparing, reduction-pattern, or skin-sparing mastectomies were performed based on each patient’s oncological and reconstructive treatment goals.
All postmastectomy incisions were closed with our standard technique using absorbable sutures and managed with ciNPT, which was applied in the sterile field of the operating room. ciNPT consisted of a self-adhesive foam dressing and a battery-powered, portable therapy unit (PREVENA CUSTOMIZABLE Dressing—90 cm, PREVENA 125 Therapy Unit, KCI, an Acelity company, San Antonio, Tex.). The single-patient-use therapy unit provided continuous −125 mm Hg and contained a replaceable 45-mL exudate canister. Both customizable dressing and therapy unit were designed for placement up to 7 days. Surgical drains were used with ciNPT. Drain tubes were routed under the skin beyond the ciNPT dressing, and drains functioned independently of ciNPT. During ciNPT, the incision was protected by the sterile dressing placed in the operating room. After treatment, the dressings were carefully removed, and a skin adhesive closure (STERI-STRIP Skin Closure, 3M, St. Paul, Minn.) was applied over each incision.
Computed descriptive statistics included mean, SD, median, minimum, and maximum for continuous variables, and frequency and percentages for categorical variables. All analyses were performed using Statistical Analysis System version 9.3 (SAS software; SAS Institute Inc., Cary, N.C.).
RESULTS
Thirteen patients underwent mastectomy with immediate expander-based breast reconstruction. Mean patient age (SD) was 44.8 (9.7), and mean body mass index was 29.2 (7.2) kg/m2. Of 4 (30.8%) patients with comorbidities, 3 patients were obese, and one patient was diabetic with Hemoglobin A1c (HbA1c) of 9.7 (Table 1). Two patients had preoperative chemotherapy; none had preoperative radiation.
Table 1.
Patient Demographics/Comorbidities and Treatment Outcomes
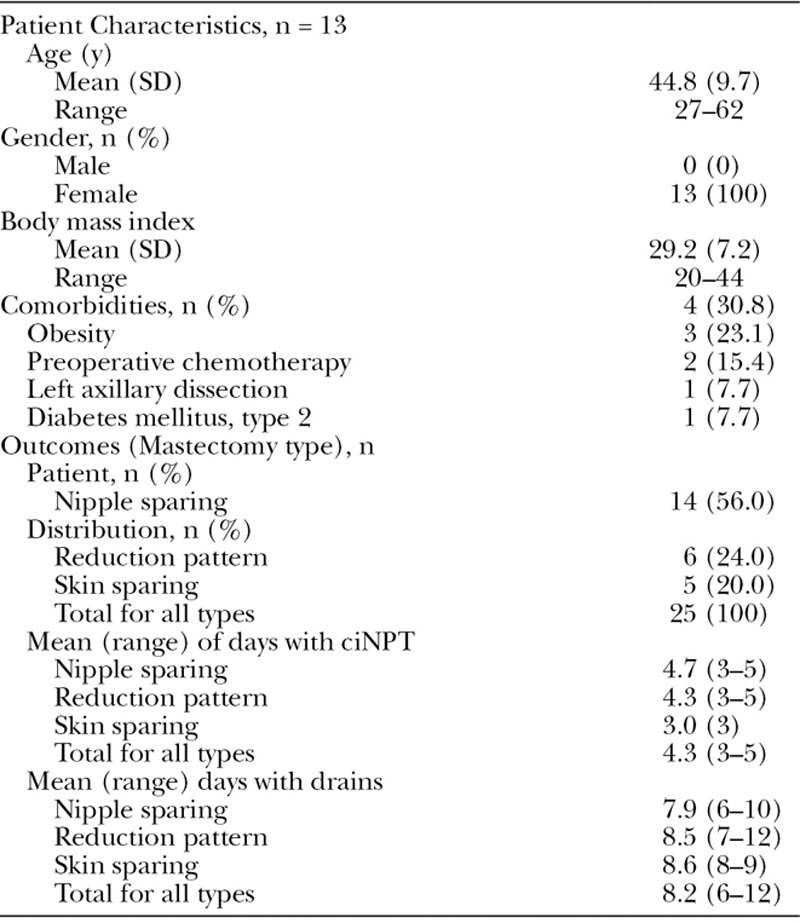
Twenty-five breasts underwent 1 of 3 types of mastectomies. The majority (56.0%) were treated with nipple-sparing mastectomies (Table 1). Overall mean ciNPT duration was 4.3 days (range, 3–5 days). Mean drain placement was 8.2 days (range, 6–12 days) (Table 1).
By 3-month follow-up, 24 of the 25 breasts (96%) achieved healing. Superficial dehiscence occurred on 3 of the 25 (12%) breasts, and flap necrosis occurred on 1 of the 25 (4%) breasts in the reduction-pattern group. A delayed hematoma developed on postoperative day 13 in 1 breast in the nipple-sparing group. No superficial dehiscences required surgical closure. Only flap necrosis in the breast of an obese, diabetic (HGBA1c, 9.7) patient required surgical revision. All other breasts healed and remained closed at 3-month follow-up.
Case Study
A 27-year-old woman with history of obesity, preoperative chemotherapy, and left breast axillary dissection (Fig. 1A) underwent reduction-pattern mastectomy on both breasts. After immediate breast reconstruction, ciNPT with a customizable dressing was applied over the entire incision (Fig. 1B). Superficial dehiscence in the left breast resolved with local wound care. Both incisions were intact at 4 weeks and remained intact at 2 months after mastectomy. The patient underwent breast reconstruction with good results at 12 months after reconstructive surgery (Fig. 1C).
Fig. 1.

Postmastectomy use of ciNPT. A, Patient before surgery. B, Application of ciNPT with customizable dressing after reduction-pattern mastectomy. C, At follow-up of 12 months after breast reconstruction with silicone implants, fat injections, and nipple reconstruction.
DISCUSSION
In this study of 13 patients who underwent immediate breast reconstruction, ciNPT with a customizable dressing was applied over entire clean incisions immediately after surgery on 25 breasts. At 3-month follow-up, all but one breast had healed.
Based on published literature and/or personal experience, we identified the risk factors associated with seroma formation, dehiscence, and delayed healing (Fig. 2). Patients with 1 or more factors received ciNPT.
Fig. 2.
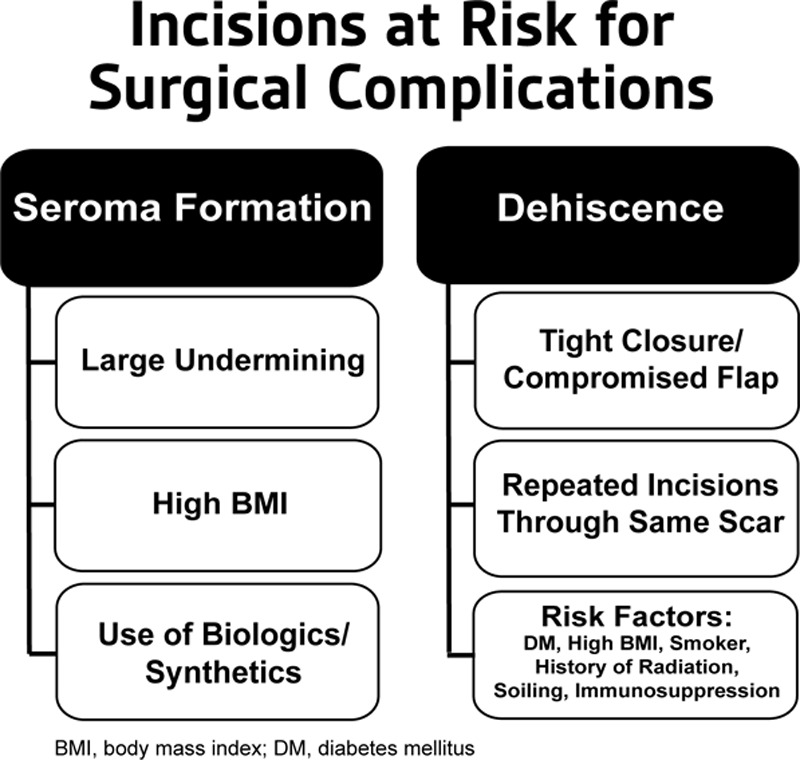
Checklist of potential risk factors for surgical complications.
Three patients whose breasts developed superficial dehiscences were obese with other risk factors (eg, diabetes mellitus, preoperative chemotherapy, and axillary dissection). All superficial dehiscences resolved without surgical closure. One patient developed a delayed hematoma, which resolved. A morbidly obese patient with type 2 diabetes developed flap necrosis in her left breast, which required surgical revision. Because complication rates up to 50% have been reported in immediate postmastectomy breast reconstruction studies,3 complication rates in this small study could be considered below average.
Based on previous negative pressure wound therapy experience, we speculated that ciNPT might reduce dead space. In a study of wounds with dead space created on the backs of pigs, ciNPT-treated incisions had significantly reduced drainage compared with gauze-treated incisions.6 Two comparative clinical studies of postoperative hip incisions reported reduced seroma development7 and volume,8 respectively, in ciNPT-treated incisions. Larger studies are needed to research the implications for breast reconstruction.
Initial experience using ciNPT over immediate postmastectomy breast reconstruction incisions raised some questions. Although ciNPT and the customizable dressing can be used for up to 7 days, concern about removing drains during ciNPT led to early ciNPT discontinuation. We have since become comfortable removing drains during ciNPT. Less drainage was also observed in attached closed-suction drains, which were removed in a mean of 8.2 days. We typically estimate 12–14 days of drain placement and may research this anecdotal observation. With recent availability of the 13-cm ciNPT peel-and-place dressing, ease of use has made dressing placement simpler.
Based on initial experience, ciNPT with customizable or peel-and-place dressings could be a viable option over closed incisions after immediate postmastectomy reconstruction as part of 2-stage expander/implant breast reconstruction. Larger observational and comparative studies are warranted.
ACKNOWLEDGMENT
We thank Leah Griffin (Acelity, San Antonio, Tex.) for statistical analysis support and Alice Goodwin (Acelity, San Antonio, Tex.) for medical writing support.
Footnotes
Presented at the Clinical Symposium on Advances in Skin and Wound Care, September 28, 2014, to October 1, 2014, Las Vegas, Nev.
Presented at the Symposium on Advanced Wound Care/Wound Healing Society, April 29, 2015, to May 3, 2015, San Antonio, Tex.
Disclosure: Drs. Gabriel, Sigalove, and Maxwell have consulting agreements with KCI, an Acelity. The Article Processing Charge was paid for by Acelity.
REFERENCES
- 1.Kroll SS, Coffey JA, Jr, Winn RJ, et al. A comparison of factors affecting aesthetic outcomes of TRAM flap breast reconstructions. Plast Reconstr Surg. 1995;96:860–864. doi: 10.1097/00006534-199509001-00015. [DOI] [PubMed] [Google Scholar]
- 2.Miller MJ, Rock CS, Robb GL. Aesthetic breast reconstruction using a combination of free transverse rectus abdominis musculocutaneous flaps and breast implants. Ann Plast Surg. 1996;37:258–264. doi: 10.1097/00000637-199609000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Sullivan SR, Fletcher DR, Isom CD, et al. True incidence of all complications following immediate and delayed breast reconstruction. Plast Reconstr Surg. 2008;122:19–28. doi: 10.1097/PRS.0b013e3181774267. [DOI] [PubMed] [Google Scholar]
- 4.Alderman AK, Wilkins EG, Kim HM, et al. Complications in postmastectomy breast reconstruction: two-year results of the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg. 2002;109:2265–2274. doi: 10.1097/00006534-200206000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Semsarzadeh NN, Tadisina KK, Maddox J, et al. Closed incision negative-pressure therapy is associated with decreased surgical-site infections: a meta-analysis. Plast Reconstr Surg. 2015;136:592–602. doi: 10.1097/PRS.0000000000001519. [DOI] [PubMed] [Google Scholar]
- 6.Suh H, Lee AY, Park EJ, et al. Negative pressure wound therapy on closed surgical wounds with dead space: animal study using a swine model. Ann Plast Surg. 2016;76:717–722. doi: 10.1097/SAP.0000000000000231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pachowsky M, Gusinde J, Klein A, et al. Negative pressure wound therapy to prevent seromas and treat surgical incisions after total hip arthroplasty. Int Orthop. 2012;36:719–722. doi: 10.1007/s00264-011-1321-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pauser J, Nordmeyer M, Biber R, et al. Incisional negative pressure wound therapy after hemiarthroplasty for femoral neck fractures - reduction of wound complications. Int Wound J. 2014 Aug 14; doi: 10.1111/iwj.12344. [Epub ahead of print.] [DOI] [PMC free article] [PubMed] [Google Scholar]


